Abstract
Purpose
We sought to investigate predictors of unfavorable tumor upgrading in very favorable intermediate-risk (IR) prostate cancer (PCa) patients treated with robot-assisted radical prostatectomy, in addition to evaluate how it may affect the risk of disease progression.
Methods
A very favorable subset of IR PCa patients presenting with prostate-specific antigen (PSA) < 10 ng/mL, percentage of biopsy positive cores (BPC) < 50%, and either International Society of Urological Pathology (ISUP) grade group 1 and clinical stage T2b or ISUP grade group 2 and clinical stage T1c-2b was identified. Unfavorable pathology at radical prostatectomy was defined as the presence of ISUP grade group > 2 (unfavorable tumor upgrading), extracapsular extension (ECE), and seminal vesicle invasion (SVI). Disease progression was defined as the event of biochemical recurrence and/or local recurrence and/or distant metastases. Associations were evaluated by Cox regression and logistic regression analyses.
Results
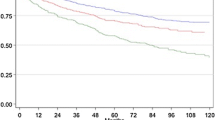
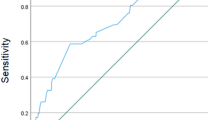
Overall, 210 patients were identified between January 2013 and October 2020. Unfavorable tumor upgrading was detected in 71 (33.8%) cases, and adverse tumor stage, including ECE or SVI in 18 (8.6%) and 11 (5.2%) patients, respectively. Median (interquartile range) follow-up was 38.5 (16–61) months. PCa progression occurred in 24 (11.4%) patients. Very favorable IR PCa patients with unfavorable tumor upgrading at final pathology showed a persistent risk of disease progression, which hold significance after adjustment for all factors (Hazard Ratio [HR]: 5.95, 95% Confidence Interval [CI]: 1.97–17.92, p = 0.002) of which PSA was an independent predictor (HR: 1.52, 95% CI 1.12–2.08, p = 0.008). Moreover, these subjects were more likely to belong to the biopsy ISUP grade group 2.
Conclusions
Very favorable IR PCa patients hiding unfavorable tumor upgrading were more likely to experience disease progression. Unfavorable tumor upgrading involved about one-third of cases and was less likely to occur in patients presenting with biopsy ISUP grade group 1. Tumor misclassification is an issue to discuss, when counseling this subset of patients for active surveillance because of the risk of delayed active treatment.

Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Further enquires can be directed to the corresponding author.
References
Mottet N, Cornford P, van den Bergh RCN et al (2022) EAU - EANM - ESTRO - ESUR - ISUP - SIOG Guidelines on Prostate Cancer. In: European Association of Urology. https://uroweb.org/guidelines/prostate-cancer. Accessed 5 Mar 2023
Schaeffer E, Srinivas S, An Y et al (2022) Prostate Cancer, Version 1.2023, NCCN Clinical Practice Guidelines in Oncology. In: National Comprehensive Cancer Network. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf. Accessed 5 Mar 2023
Moyer VA (2012) Screening for prostate cancer: U.S. preventive services task force recommendation statement. Ann Intern Med 157:120–134. https://doi.org/10.7326/0003-4819-157-2-201207170-00459
Shah N, Ioffe V, Huebner T, Hristova I (2018) prostate biopsy characteristics: a comparison between the pre- and post-2012 united states preventive services task force (USPSTF) prostate cancer screening guidelines. Rev Urol 20:77–83. https://doi.org/10.3909/riu0793
Jani C, Mouchati C, Abdallah N et al (2022) Trends in prostate cancer mortality in the United States of America, by state and race, from 1999 to 2019: estimates from the centers for disease control WONDER database. Prostate Cancer Prostatic Dis. https://doi.org/10.1038/S41391-022-00628-0
Artibani W, Porcaro AB, De Marco V et al (2018) Management of biochemical recurrence after primary curative treatment for prostate Cancer: a review. Urol Int 100:251–262. https://doi.org/10.1159/000481438
Gandaglia G, van den Bergh RCN, Tilki D et al (2018) How can we expand active surveillance criteria in patients with low- and intermediate-risk prostate cancer without increasing the risk of misclassification? development of a novel risk calculator. BJU Int 122:823–830. https://doi.org/10.1111/BJU.14391
Meissner VH, Woll M, Ankerst DP et al (2021) Long-term and pathological outcomes of low- and intermediate-risk prostate cancer after radical prostatectomy: implications for active surveillance. World J Urol 39:3763–3770. https://doi.org/10.1007/S00345-021-03717-2
Flammia RS, Hoeh B, Hohenhorst L et al (2022) Adverse upgrading and/or upstaging in contemporary low-risk prostate cancer patients. Int Urol Nephrol 54:2521–2528. https://doi.org/10.1007/s11255-022-03250-0
Porcaro AB, Panunzio A, Bianchi A et al (2022) Prognostic impact and clinical implications of unfavorable upgrading in low-risk prostate cancer after robot-assisted radical prostatectomy: results of a single tertiary referral center. Cancers (Basel). https://doi.org/10.3390/cancers14246055
Sorce G, Flammia RS, Hoeh B et al (2022) Grade and stage misclassification in intermediate unfavorable-risk prostate cancer radiotherapy candidates. Prostate 82:1040–1050. https://doi.org/10.1002/pros.24349
Awasthi S, Mahal BA, Park JY et al (2022) Substantial gleason reclassification in Black men with national comprehensive cancer network low-risk prostate cancer - a propensity score analysis. Prostate Cancer Prostatic Dis 25:547–552. https://doi.org/10.1038/s41391-022-00510-z
Perera M, Jibara G, Tin AL et al (2023) Outcomes of grade group 2 and 3 prostate cancer on initial versus confirmatory biopsy: implications for active surveillance. Eur Urol Focus 9:662–668. https://doi.org/10.1016/j.euf.2022.12.008
Wallis CJD, Zhao Z, Huang L-C et al (2022) Association of treatment modality, functional outcomes, and baseline characteristics with treatment-related regret among men with localized prostate cancer. JAMA Oncol 8:50. https://doi.org/10.1001/jamaoncol.2021.5160
Porcaro AB, Tafuri A, Sebben M et al (2019) Prostate volume index is able to differentiate between prostatic chronic inflammation and prostate cancer in patients with normal digital rectal examination and prostate-specific antigen values <10 ng/ml: results of 564 biopsy naïve cases. Urol Int 103:415–422. https://doi.org/10.1159/000502659
Porcaro AB, Rizzetto R, Bianchi A et al (2023) American Society of Anesthesiologists (ASA) physical status system predicts the risk of postoperative clavien-dindo complications greater than one at 90 days after robot-assisted radical prostatectomy: final results of a tertiary referral center. J Robot Surg 17:987–993. https://doi.org/10.1007/s11701-022-01505-7
Bock D, Nyberg M, Lantz A et al (2022) Learning curve for robot-assisted laparoscopic radical prostatectomy in a large prospective multicentre study. Scand J Urol 56:182–190. https://doi.org/10.1080/21681805.2022.2070274/SUPPL_FILE/ISJU_A_2070274_SM6703.ZIP
Sebben M, Tafuri A, Pirozzi M et al (2020) Open approach, extended pelvic lymph node dissection, and seminal vesicle invasion are independent predictors of hospital readmission after prostate cancer surgery: a large retrospective study. Minerva Urol Nefrol 72:72–81. https://doi.org/10.23736/S0393-2249.19.03586-0
Sebben M, Tafuri A, Shakir A et al (2020) The impact of extended pelvic lymph node dissection on the risk of hospital readmission within 180 days after robot assisted radical prostatectomy. World J Urol 38:2799–2809. https://doi.org/10.1007/s00345-020-03094-2
van der Kwast TH, Amin MB, Billis A et al (2011) International society of urological pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens working group 2: T2 substaging and prostate cancer volume. Modern Pathol. https://doi.org/10.1038/modpathol.2010.156
Sammon JD, Trinh QD, Sukumar S et al (2013) Risk factors for biochemical recurrence following radical perineal prostatectomy in a large contemporary series: a detailed assessment of margin extent and location. Urologic Oncol Semin Orig Investig 31:1470–1476. https://doi.org/10.1016/J.UROLONC.2012.03.013
Tafuri A, Sebben M, Pirozzi M et al (2020) Predictive factors of the risk of long-term hospital readmission after primary prostate surgery at a single tertiary referral center: preliminary report. Urol Int 104:465–475. https://doi.org/10.1159/000505409
Caster JM, Falchook AD, Hendrix LH, Chen RC (2015) Risk of pathologic upgrading or locally advanced disease in early prostate cancer patients based on biopsy gleason score and PSA: a population-based study of modern patients. Int J Radiat Oncol Biol Phys 92:244–251. https://doi.org/10.1016/J.IJROBP.2015.01.051
Epstein JI, Egevad L, Amin MB et al (2016) The 2014 international society of urological pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40:244–252. https://doi.org/10.1097/PAS.0000000000000530
Imnadze M, Sjoberg DD, Vickers AJ (2016) Adverse pathologic features at radical prostatectomy: effect of preoperative risk on oncologic outcomes. Eur Urol 69:143–148. https://doi.org/10.1016/J.EURURO.2015.03.044
Parry MG, Cowling TE, Sujenthiran A et al (2020) Risk stratification for prostate cancer management: value of the Cambridge Prognostic Group classification for assessing treatment allocation. BMC Med 18:114. https://doi.org/10.1186/s12916-020-01588-9
Patel HD, Gupta M, Tosoian JJ et al (2018) Subtyping the risk of intermediate risk prostate cancer for active surveillance based on adverse pathology at radical prostatectomy. J Urol 200:1068–1074. https://doi.org/10.1016/J.JURO.2018.04.058
van den Broeck T, van den Bergh RCN, Arfi N et al (2019) Prognostic value of biochemical recurrence following treatment with curative intent for prostate cancer: a systematic review. Eur Urol 75:967–987. https://doi.org/10.1016/J.EURURO.2018.10.011
Beauval JB, Cabarrou B, Gandaglia G et al (2017) External validation of a nomogram for identification of pathologically favorable disease in intermediate risk prostate cancer patients. Prostate 77:928–933. https://doi.org/10.1002/PROS.23348
Patel HD, Tosoian JJ, Carter HB, Epstein JI (2018) Adverse pathologic findings for men electing immediate radical prostatectomy: defining a favorable intermediate-risk group. JAMA Oncol 4:89–92. https://doi.org/10.1001/JAMAONCOL.2017.1879
Maggi M, Del Giudice F, Falagario UG et al (2021) Selectmdx and multiparametric magnetic resonance imaging of the prostate for men undergoing primary prostate biopsy: a prospective assessment in a multi-institutional study. Cancers (Basel). https://doi.org/10.3390/cancers13092047
Ferro M, Lucarelli G, Bruzzese D et al (2015) Improving the prediction of pathologic outcomes in patients undergoing radical prostatectomy: the value of prostate cancer antigen 3 (PCA3), prostate health index (phi) and sarcosine. Anticancer Res 35:1017–1023
Ferro M, Crocetto F, Bruzzese D et al (2021) Prostate health index and multiparametric mri: partners in crime fighting overdiagnosis and overtreatment in prostate cancer. Cancers (Basel). https://doi.org/10.3390/cancers13184723
Lucarelli G, Loizzo D, Ferro M et al (2019) Metabolomic profiling for the identification of novel diagnostic markers and therapeutic targets in prostate cancer: an update. Expert Rev Mol Diagn 19:377–387. https://doi.org/10.1080/14737159.2019.1604223
Weinstein IC, Wu X, Hill A et al (2023) Impact of magnetic resonance imaging targeting on pathologic upgrading and downgrading at prostatectomy: a systematic review and meta-analysis. Eur Urol Oncol 6:355–365. https://doi.org/10.1016/j.euo.2023.04.004
Noujeim J-P, Belahsen Y, Lefebvre Y et al (2023) Optimizing multiparametric magnetic resonance imaging-targeted biopsy and detection of clinically significant prostate cancer: the role of perilesional sampling. Prostate Cancer Prostatic Dis 26:575–580. https://doi.org/10.1038/s41391-022-00620-8
Funding
The authors declare they have not receive any financial support.
Author information
Authors and Affiliations
Contributions
A.B. PORCARO: project development, data analysis and interpretation, manuscript writing. A. Bianchi and A. Panunzio: data collection, manuscript writing. A. Bianchi, A. Panunzio, S. Gallina, E. Serafin, N. Trabacchin, R. Orlando, P.I. Ornaghi, G. Mazzucato, S. Vidiri, D. D’Aietti, F. Montanaro, D. Brusa, G. Marafioti Patuzzo, F. Artoni, and A. Baielli: data collection. A. Tafuri, F. Migliorini, V. De Marco, A. Veccia, M. Brunelli, S. Siracusano, M.A. Cerruto, and A. Antonelli: supervision and critical revision for important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest and did not receive any financial support.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by our Institutional Review Board. Data were collected prospectively but evaluated retrospectively as such Ethical Committee Approval was not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Porcaro, A.B., Bianchi, A., Panunzio, A. et al. Tumor upgrading among very favorable intermediate-risk prostate cancer patients treated with robot-assisted radical prostatectomy: how can it impact the clinical course?. Int Urol Nephrol (2024). https://doi.org/10.1007/s11255-024-04019-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11255-024-04019-3