Abstract
Background
Upgrading and/or upstaging in low-risk prostate cancer (PCa) patients may represent an indication for active treatment instead of active surveillance (AS). We addressed contemporary upgrading and/or upstaging rates in a large population based-cohort of low-risk PCa patients.
Materials and methods
Whitin the SEER database (2010–2015), NCCN low-risk PCa patients were identified across management modalities: radical prostatectomy (RP), radiotherapy (RT) and non-local treatment (NLT). In RP patients, upgrading and/or upstaging rates were assessed in logistic regression models.
Results
Overall, of 27,901 low-risk PCa patients, 38% underwent RP vs 28% RT vs 34% NLT. RP patients were the youngest and harbored the highest percentage of positive cores and a higher rate of cT2a than NLT. At RP, 46.2% were upgraded to GGG ≥ 2, 6.0% to GGG ≥ 3 and 10.5% harbored nonorgan-confined stage (NOC, pT3-4 or pN1). Of NOC patients, 1.6% harbored GGG ≥ 3, 6.3% harbored GGG2 and 2.6% harbored GGG1. Of pT2 patients, 4.4% harbored GGG ≥ 3, 33.9% harbored GGG2 and 51.3% harbored GGG1. Age, PSA, percentage of positive cores and number of positive cores independently predicted the presence of NOC and/or GGG ≥ 3, but with low accuracy (63.9%).
Conclusions
In low-risk PCa, critical changes between tumor grade and stage at biopsy vs RP may be expected in very few patients: NOC with GGG ≥ 3 in 1.6% and NOC with GGG2 in 6.3%. Other patients with upgrading and/or upstaging combinations will invariably harbor either pT2 or GGG1 that far less critically affect PCa prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
North American and European guidelines recommend active surveillance (AS) in low-risk prostate cancer (PCa) patients, based on comparable long-term oncologic outcomes relative to active treatment 1–4. However, these guidelines are based on findings of historical studies 5–8 when conservative management rates (active surveillance/active monitoring/watchful waiting) were substantially lower than currently 9,10. Moreover, grading of PCa might have not been the same, since in contemporary patients the combination of systemic and target biopsy has shown to significantly reduce upgrading rates 11–14. Similarly, contemporary use of MRI prior to prostate biopsy decreased the rate of clinically insignificant PCa diagnoses at initial biopsy 15–17. In consequences historical data may not be applicable to contemporary patients. To address this void, we tested most contemporary upgrading and/or upstaging rates with specific focus on critical upgrading and/or upstaging, respectively, defined as GGG ≥ 3 and/or nonorgan-confined stage. We hypothesized that contemporary upgrading and/or upstaging rates were substantially lower than historical rate.
Materials and methods
Study population
The Surveillance, Epidemiology and End Results (SEER) database samples 26% of the USA and approximates the USA in terms of geographic and demographic composition, as well as cancer incidence18. Within the SEER database spanning years 2010–2015, we identified all non-metastatic patients, aged between 40 and 75 years, with histologically confirmed adenocarcinoma of the prostate, diagnosed at biopsy (International Classification of Disease for Oncology [ICD-O-3] code 8140 site code C61.9), who fulfilled the NCCN low-risk criteria (cT1c-T2a and biopsy Gleason grade group I and/or PSA < 10 ng/ml).
We excluded patients with number of biopsy cores < 10 or > 14, as well as cases with missing information (PSA, clinical T stage, biopsy Gleason grade group, number of positive prostate biopsy cores). This resulted in a cohort of 27,901 patients exposed to any treatment modalities: radical prostatectomy (RP), radiotherapy (RT) and non-local treatment (NLT). The main study group in whom upgrading and/or upstaging rates were examined consisted of 9355 RP patients. Here, we excluded those individuals with missing information on pathologic T stage and Gleason grade group (GGG). This resulted in 9126 assessable patients.
Statistical analyses
In the first part of the analyses, patient characteristics were compared across treatment modalities (RP, RT, NLT). In the second part, we reported rates of upgrading and/or upstaging at RP. Upgrading was defined as change from GGG1 at biopsy to GGG ≥ 2 at RP. A stricter definition of upgrading relied on change from GGG1 at biopsy to GGG ≥ 3 at RP. Upstaging to nonorgan-confined stage (NOC) was defined as presence of extracapsular extension of the tumor (ECE, pT3a) or seminal vesicle invasion (SVI, pT3b) or pT4/pN1 stage at RP. Additionally, different combinations of upgrading and/or upstaging were computed and survival outcomes for these combinations were recorded. Moreover, we stratified upgrading and/or upstaging rates according to PSA (≤ 4.5 vs 4.5–5.8 vs > 5.8 ng/ml), percentage of positive cores (≤ 17 vs 17–33 vs > 33%), number of positive cores (≤ 2 vs 3–4 vs ≥ 5), age (< 60 vs > 60 years ) and race/ethnicity (Caucasians vs African-Americans vs Hispanic vs Asian vs others). Last, but not least, multivariable logistic regression models predicting two definitions of combined upgrading and/or upstaging were fitted and the accuracy of the models was calculated with previous methodology 19,20. All tests were two-sided with a level of significance set at p < 0.05 and R software environment for statistical computing and graphics (version 3.4.3) was used for all analyses.
Results
Baseline characteristics of the entire low-risk PCa patient cohort
Overall (Table 1), of 27,901 low-risk PCa patients 9,355 underwent RP (34%) vs 7820 underwent RT (28%) vs 10,726 underwent NLT (38%). RP patients were younger (59 vs 64 vs 63 years, p < 0.001), harbored higher median percentage of positive cores (25 vs 17 vs 14%, p < 0.001) and higher number of positive cores (3 vs 2 vs 2, p < 0.001) than RT or NLT counterparts. RP patients exhibited higher rates of cT2a than NLT (7.1 vs 5.4%), but not than RT patients (7.1 vs 7.1%). Finally, no differences in baseline PSA were recorded between RP vs RT vs NLT patients (5.1 vs 5.5 vs 5.4).
Upgrading and upstaging rates in low-risk prostate cancer patients
Overall (Table 2), 46.2% were upgraded to GGG ≥ 2 (4215/9126). Of those, 40.2% were GGG2 (3669/9126) vs 6.0% were GGG ≥ 3 (546/9126). Among those, 4.7% were GGG3 (433/9126) vs 1.3% were GGG4-5 (113/9126).
Overall (Table 2), 10.5% were upstaged to NOC (955/9126). Of those, 8.7% harbored ECE (796/9126) vs 1.5% harbored SVI (140/9126) vs 0.2% were upstaged to pT4 and/or pN1 (19/9126).
In GGG ≥ 3 patients (n = 149), 1.2% harbored ECE (108/9126), 0.4% harbored SVI (36/9126) and 0.06% were upstaged to T4 or pN1 (5/9126). In GGG2 patients (n = 573), 5.3% harbored ECE (480/9126), 0.9% harbored SVI (80/9126) and 0.1% were upstaged to T4 or pN1 (13/9126). In GGG1 patients (n = 233), 2.3% harbored ECE (208/9126), 0.3% harbored SVI (24/9126) and 0.01% were upstaged to T4 or pN1 (1/9126).
Among patients upstaged to NOC (n = 955), 1.6% harbored GGG ≥ 3 (149/9126), 6.3% harbored GGG2 (573/9126) vs 2.6% harbored GGG1 (233/9126). Conversely, of patients with organ-confined stage (pT2), 4.4% harbored GGG ≥ 3 (397/9126) vs 33.9% harbored GGG2 (3096/9126) and 51.3% harbored GGG1 (4678/9126). Different combinations of upgrading and/or upstaging were depicted in Fig. 1. Finally, detailed upgrading and/or upstaging rates according to patients characteristics are also tabulated (Supplementary Table 1).
Pie chart displaying rates of different combinations of upgrading and/or upstaging in low-risk prostate cancer patients treated with radical prostatectomy (n = 9126). Pathologic stage was defined as pT2 vs nonorgan confined (NOC, pT3a or pT3b or pT4 or pN1). Pathologic tumor grade was define as Gleason grade group (GGG) 1–2 vs 2 vs ≥ 3
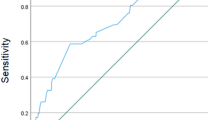
Model predicting upgrading and/or upstaging
For purpose of multivariable logistic regression modeling, we relied on two end points: (1) upgrading to GGG ≥ 2 and/or NOC stage at RP (48.7%; 4,448/9126); (2) upgrading to GGG ≥ 3 and/or NOC stage at RP (14.5%; 1,352/9126).
In model 1, age, PSA, clinical T stage, percentage of positive cores, number of positive cores, but not race/ethnicity were independent predictors of pT2 with GGG2 (Table 3). The accuracy of the model was 63.1% (95%CI 62.0–64.2%). In model 2, age, PSA, percentage of positive cores and number of positive cores, but not clinical T stage and race/ethnicity were independent predictors of NOC and/or GGG ≥ 3 (Table 3). The accuracy of the model was 63.9% (95%CI 62.3–65.6%).
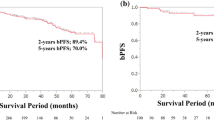
Survival differences in low-risk PCa patients according to pathologic stage and grade at RP
Overall, 12 deaths from PCa vs 139 deaths from other causes were recorded during 38,476 person-years of follow-up. After stratification according to different combinations of upgrading and/or upstaging definitions (NOC with GGG ≥ 3; NOC with GGG2; NOC with GGG1; pT2 with GGG ≥ 3; pT2 with GGG1–2), the following survival outcomes were recorded (Table 4).
In NOC with GGG ≥ 3 (n = 149), one death from PCa vs four deaths from other causes were recorded during 610 person-years of follow-up. This resulted in 1.6% person-time PCa-specific death rate per 1000 person-years. In NOC with GGG2 (n = 573), 1 death from PCa vs 11 deaths from other causes were recorded during 2404 person-years of follow-up. This resulted in 0.4% person-time PCa-specific death rate per 1000 person-years. In NOC with GGG1 (n = 233), one death from PCa vs four4 deaths from other causes were recorded during 1,018 person-years of follow-up. This resulted in 1.0% person-time PCa-specific death rate per 1000 person-years. In pT2 with GGG ≥ 3 (n = 397), one death from PCa vs three3 deaths from other causes were recorded during 1631 person-years of follow-up. This resulted in 0.6% person-time rates of PCa-specific deaths per 1000 person-years. Finally, in pT2 with GGG1–2 (n = 7774), 8 deaths from PCa vs 117 deaths from other causes were recorded during 32,814 person-years of follow-up. This resulted in 0.2% person-time PCa-specific death rate per 1000 person-years.
Discussion
We hypothesized that contemporary low-risk patients harbor lower rates of upgrading and/or upstaging than their historical counterparts due to important differences in diagnostics. We tested this hypothesis within a large contemporary cohort of low-risk PCa patients who underwent RP. Additionally we compared baseline characteristics of low-risk RP patients to their low-risk RT and NLT counterparts, to ensure absence of clinically meaningful differences.
First, regarding differences between low-risk RP vs RT vs NLT patients, RP patients harbored more aggressive PCa phenotype than their RT or NLT counterparts. Specifically, RP patients harbored a highest percentage of positive cores than RT and NLT patients (median, 25 vs 17 vs 14%, p < 0.001). Moreover, RP patients harbored a higher proportions of cT2a stage than NLT (7.1 vs 5.4%), but not RT (7.1 vs 7.1%) patients. In consequence, based on more unfavorable baseline PCa characteristics, it may be postulated that upgrading and/or upstaging rates recorded in RP patients, might be higher than those affecting RT or NLT patients. Unfortunately, this hypothesis cannot be formally tested since pathological staging only applied to RP patients and true PCa stage is unknown in those managed with RT and/or NLT.
Second, we identified low, albeit clinically meaningful rates of upgrading and/or upstaging. Upstaging from clinically favorable risk to pathologic NOC PCa represents the most important rate limiting factor, when conservative management strategy is implemented. Of 9126 low-risk PCa patients, 955 (10.5%) exhibited NOC stage. The largest subgroup consisted of pT3a (8.7%; 796/9126), substantially smaller subgroups harbored respectively pT3b (1.5%; 140/9126) and pT4 or pN1 (0.2%; 19/9126). Of those with NOC, 722 patients also harbored presence of Gleason pattern four or higher (GGG ≥ 2; 7.9%; 722/9126). Fortunately, most of those were GGG2 (6.3%; 573/9126) and of those, most had pT3a stage (5.3%; 480/9126) and only a minority harbored higher stage (1.0%; 93/9126). Conversely, only 149 of NOC patients harbored primary pattern 4 or higher (GGG ≥ 3, 1.6%, 149/9126) and within those a very marginal number were GGG4–5 (0.4%; 32/9126). Taken together, these observations indicate that contemporary low-risk PCa classification will critically misclassify 149 (1.6%; 149/9126) patients with NOC and primary Gleason pattern 4 or higher (GGG ≥ 3). Additional 573 (6.3%; 573/9126) individuals will be misclassified with less far-reaching implications, based on presence of exclusive secondary Gleason pattern 4 (GGG2) and NOC. This small patient group (1.6% plus 6.3%) represents the fatal flaw of low-risk group assignment based on PSA, clinical T stage and biopsy alone. This rate may possibly be reduced significantly with the use of MRI21,22.
Third, we tested whether upgrading and/or upstaging can be accurately predicted. Despite our best attempts and use of usual predictive modeling techniques the accuracy of predictions was low for both endpoints: 63.1% for NOC and/or GGG ≥ 2 and 63.9% for NOC and/or GGG ≥ 3. In consequence, observed rates of upgrading and/or upstaging cannot be accurately predicted using the available risk factors, at least in the current study. It may be argued that introduction of MRI findings may significantly increase the predictive ability of such a model. To the best of our knowledge, two nomograms relied on MRI findings in addition to clinical variables to predict NOC and/or GGG ≥ 3 in European19 and North American25 cohorts of low and intermediate risk PCa patients. All two nomograms exhibited an added benefit, when MRI findings were added to clinical variables. However, these results need to be replicated in external validation samples. Taken together, since the ability of MRI to improve prediction of upgrading and/or upstaging is still under debate26, other clinical tools, such as PSMA PET/CT scanning27, biomarkers28 (the prostate health index, urine PCA3, 4Kscore, TMPRSS2–ERG and ConfirmMDX) and IHC29 and genetic risk score30 may prove of value. However, large-scale contemporary testing of these tools have not been completed, especially in independent external validation samples that include sufficient numbers of low-risk patients31.
Fourth, we examined survival outcomes in the overall cohort of RP low-risk PCa patients with a median follow-up of 54 months. Expectedly, we recorded extremely low PCa mortality rates in these patients during 38,476 person-years of follow-up. Only 12 deaths were attributable to PCa. PCa-specific deaths ranged from 1 to 8, after stratification according to different combinations of upgrading and/or upstaging definitions. Based on person-time PCa-specific death rate per 1,000 person-years, only NOC with GGG ≥ 3 (1.6%) distinguished itself from values recorded for other combinations, including NOC with GGG2 (0.4%), NOC with GGG1 (1.0%), and pT2 with GGG ≥ 3 (0.6%). Nonetheless, all these combinations of upgrading and/or upstaging definitions invariably exhibited higher person-time PCa death rate for 1,000 person-years than pT2 GGG1–2 patients (0.2%) that represents the ideal candidate for AS. However, despite adequate median follow-up (54 month), the extremely low absolute number of PCa deaths undermined the ability to perform usual cancer-specific mortality rate comparisons. In consequence, consideration of person-years of follow-up and comparison of PCa person-time PCa death rates for 1,000 person-years is of essence. In agreement with our findings, Brooks et al. observed that adverse pathology (NOC and/or GGG ≥ 3) at the time of RP is highly associated with future development of distant metastasis and PCa-specific death among low and intermediate risk PCa patients from a single institutional prospectively maintained database (N = 428) with extensive follow-up (20 years)32.
The current study is not devoid limitations. The first and foremost limitation of the current study relates to the type of patients included in the analyses of upgrading and/or upstaging. Since biopsy required comparison to RP pathology, invariably such individuals represent RP patients. In consequence our findings are only directly applicable and mostly generalizable to similar patients. To address this limitation, we compared low-risk RP cohort to low-risk RT and NLT patients, with respect to age, race–ethnicity and clinical PCa characteristics. In those comparisons low-risk RP patients exhibited younger age and worse PCa characteristics. In consequence, RP low-risk PCa patients, at least in the current study, most likely reflect a less favorable phenotype of low-risk PCa. Second, an additional important limitation is lack of MRI data, since MRI represents a standard of care in the diagnostic workup of not only newly diagnosed PCa patients, but also of individuals at risk of PCa 2,4. Last but not least, SEER represents a retrospective data repository. Although, no prospective trial addressed the end points of the current study, several large institutional databases relied on prospective gathered data on biopsy and pathologic findings33. Such databases are undoubtedly better. However, they do not offer the same sample size of low-risk PCa patients as SEER.
Conclusions
In low-risk PCa patients, critical changes between tumor grade and stage at biopsy vs RP may be expected in few patients: NOC with GGG ≥ 3 in 1.6% and NOC with GGG2 in 6.3%. Others patients with upgrading and/or upstaging combinations will invariably harbor either pT2 or GGG1 that far less critically affect PCa prognosis.
Data availability statement
All data generated for this analysis were from the SEER database (https://seer.cancer.gov/data/). The code for the analyses will be made available upon request.
References
Schaeffer E, Srinivas S, Antonarakis ES et al (2021) Prostate cancer, version 1.2021: featured updates to the nccn guidelines. JNCCN J Natl Compr Cancer Netw 19(2):134–143. https://doi.org/10.6004/jnccn.2021.0008
Mottet N, van den Bergh RCN, Briers E et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur Urol 79(2):243–262. https://doi.org/10.1016/J.EURURO.2020.09.042
Sanda MG, Cadeddu JA, Kirkby E et al (2018) Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part II: recommended approaches and details of specific care options. J Urol 199(4):990–997. https://doi.org/10.1016/j.juro.2018.01.002
Sanda MG, Cadeddu JA, Kirkby E et al (2018) Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part I: risk stratification, shared decision making, and care options. J Urol 199(3):683–690. https://doi.org/10.1016/J.JURO.2017.11.095
Tosoian JJ, Mamawala M, Epstein JI et al (2015) Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J Clin Oncol 33(30):3379–3385. https://doi.org/10.1200/JCO.2015.62.5764
Klotz L, Vesprini D, Sethukavalan P et al (2015) Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol 33(3):272–277. https://doi.org/10.1200/JCO.2014.55.1192
Bill-Axelson A, Holmberg L, Garmo H et al (2018) Radical prostatectomy or watchful waiting in prostate cancer—29-year follow-up. N Engl J Med 379(24):2319–2329. https://doi.org/10.1056/NEJMOA1807801/SUPPL_FILE/NEJMOA1807801_DISCLOSURES.PDF
Hamdy FC, Donovan JL, Lane JA et al (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375(15):1415–1424. https://doi.org/10.1056/NEJMOA1606220
Mahal BA, Butler S, Franco I et al (2019) Use of active surveillance or watchful waiting for low-risk prostate cancer and management trends across risk groups in the United States, 2010–2015. J Urol 202(3):451–452. https://doi.org/10.1001/jama.2018.19941
Bandini M, Nazzani S, Marchioni M et al (2019) Increasing rate of noninterventional treatment management in localized prostate cancer candidates for active surveillance: a North American population-based study. Clin Genitourin Cancer 17(1):72-78.e4. https://doi.org/10.1016/J.CLGC.2018.09.011
Ahdoot M, Wilbur AR, Reese SE et al (2020) MRI-targeted, systematic, and combined biopsy for prostate cancer diagnosis. N Engl J Med 382(10):917–928. https://doi.org/10.1056/nejmoa1910038
Eklund M, Jäderling F, Discacciati A et al (2021) MRI-targeted or standard biopsy in prostate cancer screening. N Engl J Med 385(10):908–920. https://doi.org/10.1056/NEJMOA2100852/SUPPL_FILE/NEJMOA2100852_DATA-SHARING.PDF
Kaufmann B, Saba K, Schmidli TS et al (2022) Prostate cancer detection rate in men undergoing transperineal template-guided saturation and targeted prostate biopsy. Prostate 82(3):388–396. https://doi.org/10.1002/PROS.24286
Wenzel M, Preisser F, Wittler C et al (2021) Correlation of MRI-lesion targeted biopsy vs systematic biopsy gleason score with final pathological gleason score after radical prostatectomy. Diagn (Basel, Switz). https://doi.org/10.3390/DIAGNOSTICS11050882
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. https://doi.org/10.1056/NEJMOA1801993
Ahmed HU, El-Shater Bosaily A, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet (Lond, Engl) 389(10071):815–822. https://doi.org/10.1016/S0140-6736(16)32401-1
Venderbos LD, Luiting H, Hogenhout R, Roobol MJ (2021) Interaction of MRI and active surveillance in prostate cancer: time to re-evaluate the active surveillance inclusion criteria. Urol Oncol. https://doi.org/10.1016/j.urolonc.2021.08.008
About the SEER Program.
Flammia RS, Hoeh B, Sorce G et al (2022) Contemporary seminal vesicle invasion rates in NCCN high-risk prostate cancer patients. Prostate. https://doi.org/10.1002/PROS.24350
Wenzel M, Würnschimmel C, Chierigo F et al (2021) Nomogram predicting downgrading in national comprehensive cancer network high-risk prostate cancer patients treated with radical prostatectomy. Eur Urol Focus Published online. https://doi.org/10.1016/j.euf.2021.07.008
Amin A, Scheltema MJ, Shnier R et al (2020) The magnetic resonance imaging in active surveillance (MRIAS) trial: use of baseline multiparametric magnetic resonance imaging and saturation biopsy to reduce the frequency of surveillance prostate biopsies. J Urol 203(5):910–917. https://doi.org/10.1097/JU.0000000000000693
Klotz L, Pond G, Loblaw A et al (2020) Randomized study of systematic biopsy versus magnetic resonance imaging and targeted and systematic biopsy in men on active surveillance (ASIST): 2-year postbiopsy follow-up. Eur Urol 77(3):311–317. https://doi.org/10.1016/J.EURURO.2019.10.007
Gandaglia G, van den Bergh RCN, Tilki D et al (2018) How can we expand active surveillance criteria in patients with low- and intermediate-risk prostate cancer without increasing the risk of misclassification? Dev Novel Risk Calculator 122(5):823–830. https://doi.org/10.1111/BJU.14391
Luzzago S, de Cobelli O, Cozzi G et al (2020) A novel nomogram to identify candidates for active surveillance amongst patients with International Society of Urological Pathology (ISUP) Grade Group (GG) 1 or ISUP GG2 prostate cancer, according to multiparametric magnetic resonance imaging findings. BJU Int 126(1):104–113. https://doi.org/10.1111/BJU.15048
Lantz A, Falagario UG, Ratnani P et al (2020) Expanding active surveillance inclusion criteria: a novel nomogram including preoperative clinical parameters and magnetic resonance imaging findings. Eur Urol Oncol. https://doi.org/10.1016/J.EUO.2020.08.001
Schiavina R, Droghetti M, Novara G et al (2021) The role of multiparametric MRI in active surveillance for low-risk prostate cancer: the ROMAS randomized controlled trial. Urol Oncol Semin Orig Investig 39(7):433.e1-433.e7. https://doi.org/10.1016/j.urolonc.2020.10.018
Vlachostergios PJ, Niaz MJ, Thomas C et al (2022) Pilot study of the diagnostic utility of 89 Zr-df-IAB2M and 68 Ga-PSMA-11 PET imaging and multiparametric MRI in localized prostate cancer. Prostate. https://doi.org/10.1002/PROS.24294
Becerra MF, Atluri VS, Bhattu AS, Punnen S (2021) Serum and urine biomarkers for detecting clinically significant prostate cancer. Urol Oncol Semin Orig Investig 39(10):686–690. https://doi.org/10.1016/j.urolonc.2020.02.018
Mandel P, Wenzel M, Hoeh B et al (2021) Immunohistochemistry for prostate biopsy—impact on histological prostate cancer diagnoses and clinical decision making. Curr Oncol 28(3):2123–2133. https://doi.org/10.3390/curroncol28030197
Xu J, Isaacs WB, Mamawala M et al (2021) Association of prostate cancer polygenic risk score with number and laterality of tumor cores in active surveillance patients. Prostate 81(10):703–709. https://doi.org/10.1002/PROS.24140
Liu JL, Patel HD, Haney NM, Epstein JI, Partin AW (2021) Advances in the selection of patients with prostate cancer for active surveillance. Nat Rev Urol 18(4):197–208. https://doi.org/10.1038/S41585-021-00432-W
Brooks MA, Thomas L, Magi-Galluzzi C et al (2022) Validating the association of adverse pathology with distant metastasis and prostate cancer mortality 20-years after radical prostatectomy. Urol Oncol Semin Orig Investig 40(3):104.e1-104.e7. https://doi.org/10.1016/j.urolonc.2021.10.005
Würnschimmel C, Kachanov M, Wenzel M et al (2021) Twenty-year trends in prostate cancer stage and grade migration in a large contemporary german radical prostatectomy cohort. Prostate 81(12):849–856. https://doi.org/10.1002/pros.24181
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. The research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interests.
Ethics consent statement
All analyses and their reporting followed the SEER reporting guidelines. Due to the anonymously coded design of the SEER database, study-specific institutional review board ethics approval was not required.
Patient consent statement, permission to reproduce material from other sources and clinical trial registration
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Flammia, R.S., Hoeh, B., Hohenhorst, L. et al. Adverse upgrading and/or upstaging in contemporary low-risk prostate cancer patients. Int Urol Nephrol 54, 2521–2528 (2022). https://doi.org/10.1007/s11255-022-03250-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03250-0