Abstract
Purpose
Urolithiasis is a common urologic disease. Higher consumption of vinegar was associated with a lower risk of urolithiasis. Recent studies reported that disorder of gut microbiota and injury of the tight junction of renal tubular epithelial cells were associated with the formation of renal calcium oxalate (CaOx) stones. We aimed to explore the mechanism of vinegar reduced renal CaOx stone formation by regulating gut microbiota and the tight junction of renal tubular epithelial cells.
Methods
Thirty Sprague–Dawley rats were randomly allocated to control group, model group and vinegar group. Rats in control group got 2 ml/kg of sterile water by gavage. Model group rats were additionally supplied with drinking water with 1% (v/v) ethylene glycol (EG) every day. Rats in vinegar group had 1% (v/v) EG in drinking water and were gavaged with 2 ml/kg of vinegar (5% acetate) every day.
Results
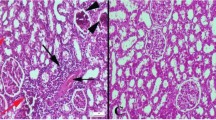
Vinegar reduced renal CaOx crystals and urinary oxalate. Vinegar increased the relative abundances of Ruminococcus gauvreauii, Ruminococcus torques, Ruminococcus-2, Moryella, Enterococcus, Alistipes, and Parabacteroides in the gut microbiota. Blood acetate increased in vinegar group. The renal tight junction occludin protein decreased in the model group and increased in the vinegar group. Studies in vitro verified that acetate could reverse the decline in occludin expression induced by CaOx crystals and inhibit CaOx crystal adhesion to cells.
Conclusion
Vinegar reduced renal CaOx stones by regulating gut microbiota and increasing blood acetate to restore renal tight junction and reduce CaOx crystal adhesion.





Similar content being viewed by others
References
Zeng G, Mai Z, Xia S, Wang Z, Zhang K, Wang L et al (2017) Prevalence of kidney stones in China: an ultrasonography based cross-sectional study. BJU Int 120:109–116. https://doi.org/10.1111/bju.13828
Liu Y, Chen Y, Liao B, Luo D, Wang K, Li H et al (2018) Epidemiology of urolithiasis in Asia. Asian J Urol 5:205–214. https://doi.org/10.1016/j.ajur.2018.08.007
Oehlschläger S, Fuessel S, Meye A, Herrmann J, Froehner M, Albrecht S et al (2009) Role of cellular oxalate in oxalate clearance of patients with calcium oxalate monohydrate stone formation and normal controls. Urology 73:480–483. https://doi.org/10.1016/j.urology.2008.11.028
Stitchantrakul W, Kochakarn W, Ruangraksa C, Domrongkitchaiporn S (2007) Urinary risk factors for recurrent calcium stone formation in Thai stone formers. J Med Assoc Thai 90:688–698
Peerapen P, Thongboonkerd V (2011) Effects of calcium oxalate monohydrate crystals on expression and function of tight junction of renal tubular epithelial cells. Lab Invest 91:97–105. https://doi.org/10.1038/labinvest.2010.167
Verkoelen CF (2006) Crystal retention in renal stone disease: a crucial role for the glycosaminoglycan hyaluronan? J Am Soc Nephrol 17:1673–1687. https://doi.org/10.1681/asn.2006010088
Tavasoli S, Alebouyeh M, Naji M, Shakiba Majd G, Shabani Nashtaei M, Broumandnia N et al (2020) Association of intestinal oxalate-degrading bacteria with recurrent calcium kidney stone formation and hyperoxaluria: a case–control study. BJU Int 125:133–143. https://doi.org/10.1111/bju.14840
Hatch M, Freel RW (2013) A human strain of Oxalobacter (HC-1) promotes enteric oxalate secretion in the small intestine of mice and reduces urinary oxalate excretion. Urolithiasis 41:379–384. https://doi.org/10.1007/s00240-013-0601-8
Stern JM, Moazami S, Qiu Y, Kurland I, Chen Z, Agalliu I et al (2016) Evidence for a distinct gut microbiome in kidney stone formers compared to non-stone formers. Urolithiasis 44:399–407. https://doi.org/10.1007/s00240-016-0882-9
Suryavanshi MV, Bhute SS, Jadhav SD, Bhatia MS, Gune RP, Shouche YS (2016) Hyperoxaluria leads to dysbiosis and drives selective enrichment of oxalate metabolizing bacterial species in recurrent kidney stone endures. Sci Rep 6:34712–34712. https://doi.org/10.1038/srep34712
Tang R, Jiang Y, Tan A, Ye J, Xian X, Xie Y et al (2018) 16S rRNA gene sequencing reveals altered composition of gut microbiota in individuals with kidney stones. Urolithiasis 46:503–514. https://doi.org/10.1007/s00240-018-1037-y
Ticinesi A, Milani C, Guerra A, Allegri F, Lauretani F, Nouvenne A et al (2018) Understanding the gut-kidney axis in nephrolithiasis: an analysis of the gut microbiota composition and functionality of stone formers. Gut 67:2097–2106. https://doi.org/10.1136/gutjnl-2017-315734
Suryavanshi MV, Bhute SS, Gune RP, Shouche YS (2018) Functional eubacteria species along with trans-domain gut inhabitants favour dysgenic diversity in oxalate stone disease. Sci Rep 8:16598–16598. https://doi.org/10.1038/s41598-018-33773-5
Zampini A, Nguyen AH, Rose E, Monga M, Miller AW (2019) Defining dysbiosis in patients with urolithiasis. Sci Rep 9:5425–5425. https://doi.org/10.1038/s41598-019-41977-6
Arvans D, Jung YC, Antonopoulos D, Koval J, Granja I, Bashir M et al (2017) Oxalobacter formigenes-derived bioactive factors stimulate oxalate transport by intestinal epithelial cells. J Am Soc Nephrol 28:876–887. https://doi.org/10.1681/asn.2016020132
Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F (2016) From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165:1332–1345. https://doi.org/10.1016/j.cell.2016.05.041
Xiang S, Zhou J, Li J, Wang Q, Zhang Q, Zhao Z et al (2015) Antilithic effects of extracts from different polarity fractions of Desmodium styracifolium on experimentally induced urolithiasis in rats. Urolithiasis 43:433–439. https://doi.org/10.1007/s00240-015-0795-z
Liu Y, Jin X, Hong HG, Xiang L, Jiang Q, Ma Y et al (2020) The relationship between gut microbiota and short chain fatty acids in the renal calcium oxalate stones disease. Faseb J. https://doi.org/10.1096/fj.202000786R
Schmittgen TD, Livak KJ (2008) Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc 3:1101–1108. https://doi.org/10.1038/nprot.2008.73
Guo WB, Huang ZH, Yang C, Lv XY, Xia H, Tian H et al (2020) Down regulating PHGDH affects the lactate production of sertoli cells in varicocele. Reprod Biol Endocrinol 18:70. https://doi.org/10.1186/s12958-020-00625-9
Hung TV, Suzuki T (2018) Short-chain fatty acids suppress inflammatory reactions in Caco-2 cells and mouse colons. 66:108–117. https://doi.org/10.1021/acs.jafc.7b04233
Zhu W, Liu Y, Lan Y, Li X, Luo L, Duan X et al (2019) Dietary vinegar prevents kidney stone recurrence via epigenetic regulations. EBioMedicine 45:231–250. https://doi.org/10.1016/j.ebiom.2019.06.004
Zhu W, Liu Y, Duan X, Xiao C, Lan Y, Luo L et al (2020) Alteration of the gut microbiota by vinegar is associated with amelioration of hyperoxaluria-induced kidney injury. Food Funct 11:2639–2653. https://doi.org/10.1039/c9fo02172h
Liu Y, Jin X, Ma Y, Jian Z, Wei Z, Xiang L, et al (2021): Short-Chain Fatty Acids Reduced Renal Calcium Oxalate Stones by Regulating the Expression of Intestinal Oxalate Transporter SLC26A6. mSystems, 6:e0104521. https://doi.org/10.1128/mSystems.01045-21
Peerapen P, Chaiyarit S, Thongboonkerd V (2018) Protein network analysis and functional studies of calcium oxalate crystal-induced cytotoxicity in renal tubular epithelial cells. Proteomics 18:e1800008. https://doi.org/10.1002/pmic.201800008
Liu Y, Chen Z, Dai J, Yang P, Xu W, Ai Q et al (2019) Sodium butyrate supplementation in high-soybean meal diets for turbot (Scophthalmus maximus L.): effects on inflammatory status, mucosal barriers and microbiota in the intestine. Fish Shellfish Immunol 88:65–75. https://doi.org/10.1016/j.fsi.2019.02.064
Fu J, Li G, Wu X, Zang B (2019) Sodium butyrate ameliorates intestinal injury and improves survival in a rat model of cecal ligation and puncture-induced sepsis. Inflammation 42:1276–1286. https://doi.org/10.1007/s10753-019-00987-2
Liu P, Wang Y, Yang G, Zhang Q, Meng L, Xin Y et al (2021) The role of short-chain fatty acids in intestinal barrier function, inflammation, oxidative stress, and colonic carcinogenesis. Pharmacol Res 165:105420. https://doi.org/10.1016/j.phrs.2021.105420
Denburg MR, Koepsell K, Lee JJ (2020) Perturbations of the gut microbiome and metabolome in children with calcium oxalate kidney stone disease. J Am Soc Nephrol 31:1358–1369. https://doi.org/10.1681/asn.2019101131
Milliner D, Hoppe B, Groothoff J (2018) A randomised phase II/III study to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Urolithiasis 46:313–323. https://doi.org/10.1007/s00240-017-0998-6
Hoppe B, Niaudet P, Salomon R, Harambat J, Hulton SA, Van’t Hoff W et al (2017) A randomised Phase I/II trial to evaluate the efficacy and safety of orally administered Oxalobacter formigenes to treat primary hyperoxaluria. Pediatr Nephrol 32:781–790. https://doi.org/10.1007/s00467-016-3553-8
Hoppe B, Groothoff JW, Hulton SA, Cochat P, Niaudet P, Kemper MJ et al (2011) Efficacy and safety of Oxalobacter formigenes to reduce urinary oxalate in primary hyperoxaluria. Nephrol Dial Transplant 26:3609–3615. https://doi.org/10.1093/ndt/gfr107
Hoppe B, Pellikka PA, Dehmel B, Banos A, Lindner E, Herberg U (2020) Effects of Oxalobacter formigenes in subjects with primary hyperoxaluria Type 1 and end-stage renal disease: a Phase II study. Nephrol Dial Transplant. https://doi.org/10.1093/ndt/gfaa135
Li X, Ellis ML, Dowell AE, Kumar R, Morrow CD, Schoeb TR et al (2016) Response of germ-free mice to colonization with O. formigenes and altered Schaedler flora. Appl Environ Microbiol 82:6952–6960. https://doi.org/10.1128/AEM.02381-16
Hatch M, Gjymishka A, Salido EC, Allison MJ, Freel RW (2011) Enteric oxalate elimination is induced and oxalate is normalized in a mouse model of primary hyperoxaluria following intestinal colonization with Oxalobacter. Am J Physiol Gastrointest Liver Physiol 300:G461–G469. https://doi.org/10.1152/ajpgi.00434.2010
Hatch M, Cornelius J, Allison M, Sidhu H, Peck A, Freel RW (2006) Oxalobacter sp. reduces urinary oxalate excretion by promoting enteric oxalate secretion. Kidney Int 69:691–698. https://doi.org/10.1038/sj.ki.5000162
Sidhu H, Allison MJ, Chow JM, Clark A, Peck AB (2001) Rapid reversal of hyperoxaluria in a rat model after probiotic administration of Oxalobacter formigenes. J Urol 166:1487–1491 ((PMID: 11547118))
Sadaf H, Raza SI, Hassan SW (2017) Role of gut microbiota against calcium oxalate. Microb Pathog 109:287–291. https://doi.org/10.1016/j.micpath.2017.06.009
de Almeida CV, Taddei A, Amedei A (2018) The controversial role of Enterococcus faecalis in colorectal cancer. Ther Adv Gastroenterol 11:1756284818783606–1756284818783606. https://doi.org/10.1177/1756284818783606
Choi EJ, Lee HJ, Kim WJ, Han KI, Iwasa M, Kobayashi K, et al (2019) Enterococcus faecalis EF-2001 protects DNBS-induced inflammatory bowel disease in mice model. 14:e0210854. https://doi.org/10.1371/journal.pone.0210854
Lengfelder I, Sava IG, Hansen JJ, Kleigrewe K, Herzog J, Neuhaus K et al (2019) Complex bacterial consortia reprogram the colitogenic activity of Enterococcus faecalis in a gnotobiotic mouse model of chronic, immune-mediated colitis. Front Immunol 10:1420. https://doi.org/10.3389/fimmu.2019.01420
Clavel T, Duck W, Charrier C, Wenning M, Elson C, Haller D (2010) Enterorhabdus caecimuris sp. nov., a member of the family Coriobacteriaceae isolated from a mouse model of spontaneous colitis, and emended description of the genus Enterorhabdus Clavel et al. 2009. Int. J. System. Evolut. Microbiol. 60:1527–1531. https://doi.org/10.1099/ijs.0.015016-0
Kandhare AD, Patil MVK, Bodhankar SL (2015) L-Arginine attenuates the ethylene glycol induced urolithiasis in ininephrectomized hypertensive rats: role of KIM-1, NGAL, and NOs. Ren Fail 37:709–721. https://doi.org/10.3109/0886022X.2015.1011967
Pragasam V, Kalaiselvi P, Sumitra K, Srinivasan S, Varalakshmi P (2005): Counteraction of oxalate induced nitrosative stress by supplementation of l-arginine, a potent antilithic agent. Clin. Chimica Acta 354:159–166. https://doi.org/10.1016/j.cccn.2004.11.029
Kizivat T, Smolić M, Marić I, Tolušić Levak M, Smolić R, Bilić Čurčić I et al (2017) Antioxidant pre-treatment reduces the toxic effects of oxalate on renal epithelial cells in a cell culture model of urolithiasis. Int J Environ Res Public Health 14:109. https://doi.org/10.3390/ijerph14010109
Kato J, Ruram AA, Singh SS, Devi SB, Devi TI, Singh WG (2007) Lipid peroxidation and antioxidant vitamins in urolithasis. Indian J Clin Biochem 22:128–130. https://doi.org/10.1007/BF02912895
Kancha RK, Anasuya A (1992) Contribution of vitamin A deficiency to calculogenic risk factors of urine: studies in children. Biochem Med Metab Biol 47:1–9. https://doi.org/10.1016/0885-4505(92)90002-g
Munday JS, McKinnon H, Aberdein D, Collett MG, Parton K, Thompson KG (2009) Cystitis, pyelonephritis, and urolithiasis in rats accidentally fed a diet deficient in vitamin A. J Am Assoc Lab Anim Sci 48:790–794 ((PMID: 19930829))
Gershoff SN, McGandy RB (1981) The effects of vitamin A-deficient diets containing lactose in producing bladder calculi and tumors in rats. Am J Clin Nutr 34:483–489. https://doi.org/10.1093/ajcn/34.4.483
Grases F, Garcia-Gonzalez R, Genestar C, Torres JJ, March JG (1998) Vitamin A and urolithiasis. Clin Chimica Acta 269:147–157. https://doi.org/10.1016/s0009-8981(97)00198-8
Pyo YH, Hwang JY, Seong KS (2018) Hypouricemic and antioxidant effects of soy vinegar extracts in hyperuricemic mice. J Med Food 21:1299–1305. https://doi.org/10.1089/jmf.2018.4181
Funding
This work was supported by the National Natural Science Foundation of China [81770703, 81970602], the Foundation of Science and Technology Department of Sichuan Province [2018SZ0118, 2019YFS0281], and the 1·3·5 Project for Disciplines of Excellence, West China Hospital, Sichuan University [ZYJC18015].
Author information
Authors and Affiliations
Contributions
Conceptualization: Yu Liu, Kunjie Wang; methodology: Yu Liu, Xi Jin, Yucheng Ma, Qun Sun; formal analysis and investigation: Yu Liu, Xi Jin, Yucheng Ma; writing—original draft: Yu Liu; writing—review and editing: Xi Jin, Qun Sun, Kunjie Wang; funding acquisition: Kunjie Wang, Hong Li; resources: Kunjie Wang, Hong Li; supervision: Kunjie Wang, Hong Li.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liu, Y., Jin, X., Ma, Y. et al. Vinegar reduced renal calcium oxalate stones by regulating acetate metabolism in gut microbiota and crystal adhesion in rats. Int Urol Nephrol 54, 2485–2495 (2022). https://doi.org/10.1007/s11255-022-03259-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-022-03259-5