Abstract
Purpose
To evaluate the outcome of the retrourethral transobturator sling (RTS) by functional magnetic resonance imaging (MRI) and to identify parameters associated with sling failure.
Methods
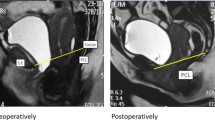
Of thirty recruited men with postprostatectomy stress urinary incontinence (SUI), 26 consecutively underwent functional MRI before sling procedure and 12 months thereafter in a prospective clinical cohort observational study. Periurethral/urethral fibrosis and sling visualization were evaluated on static sequences. The angle of the membranous urethra, position of the bladder neck and external urethral sphincter were assessed during Valsalva’s maneuver and voiding. Sling success was defined as no or one dry “security” pad.
Results
The success and failure rates were 58 % (15/26 patients) and 42 % (11/26 patients), respectively. The sling leads to reduction in the membranous urethra angle during Valsalva’s maneuver (39.55° vs. 36.82°, p = 0.025) and voiding (38.25° vs. 34.83°, p = 0.001) and elevation of the external urethral sphincter (2.9 vs. 4.8 mm, p = 0.017). Preoperative wider angle of the membranous urethra was significantly correlated with severe preoperative incontinence. Sling failure (p = 0.001) and severe preoperative incontinence (p = 0.001) were significantly related to only small changes of the membranous urethra angle. The interrater and intrarater reliability for membranous urethra angle was excellent (intraclass correlation coefficient ≥0.75).
Conclusions
The RTS leads to reduction in the membranous urethra angle. The extent of the changes in the membranous urethra angle is associated with RTS outcome. Functional MRI is a reliable noninvasive visualization tool of interactions between the sling and pelvic floor for further research on the complex nature of postprostatectomy SUI.

Similar content being viewed by others
References
Rehder P, Gozzi C (2007) Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol 52(3):860–866. doi:10.1016/j.eururo.2007.01.110
Zuckerman JM, Edwards B, Henderson K, Beydoun HA, McCammon KA (2014) Extended outcomes in the treatment of male stress urinary incontinence with a transobturator sling. Urology. doi:10.1016/j.urology.2013.10.065
Rehder P, Haab F, Cornu JN, Gozzi C, Bauer RM (2012) Treatment of postprostatectomy male urinary incontinence with the transobturator retroluminal repositioning sling suspension: 3-year follow-up. Eur Urol 62(1):140–145. doi:10.1016/j.eururo.2012.02.038
Rehder P, Webster G (2011) The AdVance® Male Sling: patient selection and workup. Eur Urol Suppl 10(4):390–394. doi:10.1016/j.eursup.2011.04.005
Cornu JN, Sebe P, Ciofu C, Peyrat L, Cussenot O, Haab F (2011) Mid-term evaluation of the transobturator male sling for post-prostatectomy incontinence: focus on prognostic factors. BJU Int 108(2):236–240. doi:10.1111/j.1464-410X.2010.09765.x
Soljanik I, Gozzi C, Becker AJ, Stief CG, Bauer RM (2012) Risk factors of treatment failure after retrourethral transobturator male sling. World J Urol 30(2):201–206. doi:10.1007/s00345-011-0671-6
Bauer RM, Gozzi C, Hubner W, Nitti VW, Novara G, Peterson A, Sandhu JS, Stief CG (2011) Contemporary management of postprostatectomy incontinence. Eur Urol 59(6):985–996. doi:10.1016/j.eururo.2011.03.020
Bauer RM, Gozzi C, Roosen A, Khoder W, Trottmann M, Waidelich R, Stief CG, Soljanik I (2013) Impact of the ‘repositioning test’ on postoperative outcome of retroluminar transobturator male sling implantation. Urol Int 90(3):334–338. doi:10.1159/000347123
Bauer RM, Mayer ME, Gratzke C, Soljanik I, Buchner A, Bastian PJ, Stief CG, Gozzi C (2009) Prospective evaluation of the functional sling suspension for male postprostatectomy stress urinary incontinence: results after 1 year. Eur Urol 56(6):928–933. doi:10.1016/j.eururo.2009.07.028
Bauer RM, Mayer ME, May F, Gratzke C, Buchner A, Soljanik I, Bastian PJ, Stief CG, Gozzi C (2010) Complications of the AdVance transobturator male sling in the treatment of male stress urinary incontinence. Urology 75(6):1494–1498. doi:10.1016/j.urology.2009.12.012
Paparel P, Akin O, Sandhu JS, Otero JR, Serio AM, Scardino PT, Hricak H, Guillonneau B (2009) Recovery of urinary continence after radical prostatectomy: association with urethral length and urethral fibrosis measured by preoperative and postoperative endorectal magnetic resonance imaging. Eur Urol 55(3):629–637. doi:10.1016/j.eururo.2008.08.057
Soljanik I, Bauer RM, Becker AJ, Stief CG, Gozzi C, Soljanik O, Kirchhoff SM (2013) Morphology and dynamics of the male pelvic floor before and after retrourethral transobturator sling placement: first insight using MRI. World J Urol 31(3):629–638. doi:10.1007/s00345-012-0884-3
Lienemann A, Sprenger D, Janssen U, Grosch E, Pellengahr C, Anthuber C (2004) Assessment of pelvic organ descent by use of functional cine-MRI: which reference line should be used? Neurourol Urodyn 23(1):33–37. doi:10.1002/nau.10170
Soljanik I, Bauer RM, Becker AJ, Stief CG, Gozzi C, Solyanik O, Brocker KA, Kirchhoff SM (2014) Is a wider angle of the membranous urethra associated with incontinence after radical prostatectomy? World J Urol. doi:10.1007/s00345-014-1241-5
Fleiss J (1981) Statistical methods for rates and proportions, 2nd edn. Wiley, New York
Warner JN, Grimsby GM, Tyson MD, Wolter CE (2012) Bladder capacity on preoperative urodynamics may impact outcomes on transobturator male slings. Neurourol Urodyn 31(7):1124–1127. doi:10.1002/nau.22233
Suskind AM, DeLancey JO, Hussain HK, Montgomery JS, Latini JM, Cameron AP (2014) Dynamic MRI evaluation of urethral hypermobility post-radical prostatectomy. Neurourol Urodyn 33(3):312–315. doi:10.1002/nau.22408
Pistolesi D, Zampa V, Gozzi C, Mariani C, Santarsieri M, Faggioni L, Bartolozzi C, Selli C (2014) Could the sling position influence the clinical outcome in male patients treated for urinary incontinence? A magnetic resonance imaging study with a 3 Tesla system. Urology 83(2):471–476. doi:10.1016/j.urology.2013.10.024
Conflict of interest
Ricarda M. Bauer and Christian Gozzi declare lectures, consultancy work and participation in clinical trials for AMS. All other authors declare that no funding or other agreement has limited their ability to fairly complete and publish this data, and they had full control of the primary data. There has been no extra-institutional funding for this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Soljanik, I., Solyanik, O., Stief, C.G. et al. The extent of changes in the membranous urethra angle is associated with the outcome of retrourethral transobturator sling procedure. Int Urol Nephrol 47, 249–255 (2015). https://doi.org/10.1007/s11255-014-0888-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-014-0888-6