Abstract
Purpose
Individuals with moderate to severe traumatic brain injury (TBI) experience changes in their quality-of-life (QOL) post-injury. Given the vast literature that exists about QOL after TBI, a scoping review was performed to identify the different biopsychosocial factors that affect a person’s QOL after a moderate to severe TBI.
Methods
A scoping review was conducted using the following electronic databases: MEDLINE, CINAHL, Embase, and PsycINFO. Terms relating to TBI and QOL were used.
Results
There were 7576 articles obtained from the databases, resulting in 535 full-text articles. Ultimately, 52 articles were extracted, which consisted of biopsychosocial QOL factors after TBI. The biopsychosocial factors of QOL after TBI included 19 biological factors (i.e., sex, TBI severity, cognition), 16 psychological factors (i.e., depression, self-efficacy, coping styles), and 19 social factors (i.e., employment, social participation, social support). Factors such as fatigue, self-awareness, transition, and discharge from hospitals are known issues in TBI literature but were minimally reported in studies in this review, identifying them as potential gaps in research.
Conclusion
Identifying biopsychosocial factors relating to QOL after TBI can enable health services to develop targeted rehabilitation programs for individuals with TBI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Plain English summary
After traumatic brain injury, people can experience changes in quality-of-life. Quality-of-life may be defined as a person’s overall perception of their life, with regard to their health, expectations, and external influences. Although a lot of research has been conducted on this topic, a summary of this research is needed to provide information to clinicians, researchers, and individuals with brain injuries, to help improve quality-of-life after a traumatic brain injury. In this study, we conducted an extensive search of past literature and identified the different biological, psychological, and social factors of quality-of-life after a traumatic brain injury. The results describe the influence of factors, such as mental health and social support, on quality-of-life after traumatic brain injury. Findings can guide health services to tailor their rehabilitation treatments to help improve the lives of individuals with traumatic brain injury.
Background
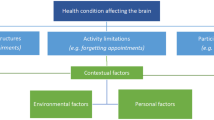
Traumatic brain injury (TBI) is sustained by approximately 69 million individuals each year worldwide [1]. Individuals with TBI can face long-term problems that impact their health, function, and daily life [2]. These may arise from the injury itself (i.e., mobility and cognitive issues), as well as from barriers in their surroundings (i.e., environmental and societal) [3, 4]. These problems can have a major impact on an individual’s quality-of-life (QOL) post-injury. QOL is an important outcome, with increasing interest in the investigation and implementation of strategies to improve QOL after TBI.
QOL is a broad construct with varying definitions. The World Health Organization describes QOL as having an individualized component, with subjective experiences shaping a person’s perception of life within their cultural context, and in relation to their personal goals, expectations, and interests [5]. Given this expansive definition, QOL can be described through the physical health, psychological, social relationships, and environmental domains, and are central in providing insight into an individual’s QOL [6]. These domains align with the biological, psychological, and social changes that are typically experienced by individuals with TBI. As QOL encompasses a broad range of aspects of human life, a more comprehensive measure known as the health-related QOL (HRQOL) was introduced. HRQOL is a multi-dimensional construct that measures how an individual perceives the effects of their injury on their physical, mental, and social function [7]. HRQOL is often used as an outcome measure for individuals with chronic illnesses to signify their QOL.
TBI can be defined as a chronic condition, as the problems that stem from a TBI can occur at any point post-injury [8]. There may be a low rate of full recovery after a moderate to severe TBI as the effects are often long lasting, making the navigation of life after TBI an ongoing process and impacting a person’s QOL [9]. As these changes post-TBI can affect a person in multiple ways, a biopsychosocial perspective can facilitate the understanding on how to improve QOL, which is a primary goal in TBI rehabilitation. Therefore, using a biopsychosocial framework enables the development and implementation of interventions needed to manage the challenges experienced after a TBI.
There have been a few reviews to date identifying factors exploring QOL and TBI [10]. One systematic review reported on the nature and predictors of QOL that affected children and adolescents with TBI [11]. Another review described the differences in QOL between individuals with and without a TBI, with studies reporting individuals with TBI having a lower QOL [12]. Finally, a systematic review identified 16 studies that assessed at least two of the four QOL domains (physical, social, environmental, cognitive) experienced post-injury [13]. However, despite the growing evidence of the numerous factors affecting QOL after a moderate to severe TBI, no recent reviews have been conducted.
Past reviews focus too broadly on QOL and have failed to explore in detail the biological, psychological, and social factors in the adult TBI population. As such, despite the growing number of research studies about these different factors in the TBI population, there have been no recent reviews conducted to provide a better understanding of the factors associated with QOL from a biopsychosocial perspective. Thus, the primary objective of this scoping review is to identify QOL factors and analyze potential knowledge gaps in QOL research in the moderate to severe adult TBI population with relation to biological, psychological, and social domains.
Methods
A scoping review was conducted, in accordance with the framework by Arksey and O’Malley [14] and Levac et al. [15]. Five stages were included in this scoping review: identifying the research question, identifying relevant studies, choosing studies, charting the data, and reporting the results [14]. This scoping review is reported using the PRISMA Extension for Scoping Reviews [16].
Search strategy
The articles were identified from the following databases: MEDLINE, CINAHL, Embase, and PsycINFO, with the search conducted on 24 April 2021. With the help of a subject-area expert librarian, the initial database search was developed using key search terms: ‘brain injuries,’ ‘quality of life,’ and ‘life quality.’ Boolean terms (‘AND,’ ‘OR,’ ‘NOT’) were used to combine terms, and asterisks were used to include variants in spelling.
Eligibility criteria
English peer-reviewed articles published since 1990 to the date of search were reviewed to limit the breadth of articles obtained and to analyze more recent QOL literature. Full-text articles were selected if they had: (1) presented data on half or more participants with a moderate to severe TBI who were 18 years or older, (2) identified biological, psychological, or social QOL factors, and (3) provided quantitative data on a validated global QOL measure. Adolescents or children with TBI were not included as there may be developmental causes affecting their QOL, which may not be present in the adult population. Furthermore, the exclusion criteria consisted of articles with no full-texts available (i.e., conference abstracts, poster, dissertations) or study designs such as case studies or qualitative methodologies. Articles with surgical (e.g., cranioplasty) or hormone-related interventions (e.g., pituitary dysfunction) were also excluded.
Data screening and extraction
The study selection and information extraction were performed using the software Covidence [17]. All authors were involved in each stage of the review process, with additional help of four research assistants. Authors RM, JG, JNG, and two research assistants independently performed the title and abstract screening, while authors RM, JNG, and JS independently conducted the full-text screening. Conflicts were resolved by JS. Data extraction was independently conducted by RM, JG, and two research assistants. In line with the aims of this scoping review, a critical appraisal was not conducted. Extracted data included the country of the study, authors, participant information, measures of QOL, factors associated with QOL, and other main findings (Tables 1, 2).
Results
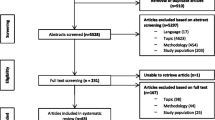
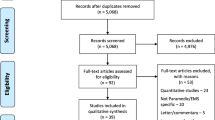
The initial database search identified 7576 articles as seen in Fig. 1 [18]. 535 articles were included in the full-text screening process, and a total of 52 articles were included in the review (Table 1). Most of the studies were from the United States of America (29%), Australia (13%), and Norway (12%). Of the included articles, 21 were cross-sectional, 20 used a prospective longitudinal design, six were case–control, four used retrospective longitudinal designs, and one followed a retrospective cross-sectional design (Table 1). The most common QOL measures were the Short Form-36 Health Survey (16 articles), Quality-of-Life After Brain Injury (6 articles), and Quality-of-Life Inventory (6 articles) (Table 1). Given the breadth of literature on QOL after TBI, our findings below are categorized based on biological, psychological, and social domains.
Biological factors
There were 28 studies that reported 19 biological QOL factors, such as sex, TBI severity, cognition, age, time since injury, mobility, functional independence, length of hospital stay, length of ICU treatment, pre-injury comorbidities, thoracic injury, trauma, epilepsy, fatigue, sleep disturbance, symptom severity, identifying emotions, global function, and duration of posttraumatic amnesia.
There were seven studies that reported on sex and QOL after TBI [19,20,21,22,23,24,25]. Most studies found that females reported lower HRQOL than males [19,20,21,22,23]. However, two studies reported contrasting findings, where being male was associated with lower QOL [24, 25]. One study identified that males had lower scores than females on all HRQOL domains, except for the domains of role-emotional and mental health [24], while another study reported that females had higher self-rated QOL [25].
A person’s age was another biological QOL factor after TBI, with differing results [23, 26,27,28,29,30,31,32]. Van Delft-Schreurs et al. [30] found that higher QOL in the environmental domain was associated with older age, while Tsaousides et al., [29] identified a positive correlation between the age at injury and QOL. In contrast, one study noted that older women reported worse QOL [23], and a separate study reported that participants aged 31 and above, had decreased scores in the role-physical domain of QOL [28]. However, the relationship of age and QOL varies across the lifespan and could explain the discrepant findings looking for linear correlations or associations.
The severity of a TBI was a common QOL factor, as illustrated by six studies [21, 28, 29, 32,33,34]. Mixed findings were described, with two studies associating higher severity of injury with better QOL [28, 34], while one study reported high severity of injury with low QOL [29]. A separate study identified that higher severity of TBI was associated with lower scores on the physical functioning domain, but higher scores on general health and role-physical domains [21]. Additionally, one study found TBI severity to be a predictor for mental HRQOL [32], while another study found a weak correlation between TBI severity and HRQOL [33].
There were six studies that described how cognition affected QOL [27, 35,36,37,38,39]. Except for one study, higher scores on neuropsychological tests were associated with higher QOL. Cognition was a direct predictor of QOL [27], and people with cognitive impairments, such as deficits in attention, memory, and executive functioning reported lower QOL scores [35,36,37, 39]. However, a case–control study reported that those with lower executive functioning had high scores in the social relationship QOL domain [38].
There were a few factors that were identified once or by only a small number of studies. The factors reported only once included sleep disturbance, pre-injury comorbidity, longer periods of posttraumatic amnesia, epilepsy, fatigue, mobility problems, symptom severity, lower global function, thoracic injuries, and longer length of ICU treatment [19, 22, 30, 36, 40,41,42,43]. These factors impacted QOL negatively, except for thoracic injuries, which were associated with better QOL in the environmental domain. Time since injury, functional independence, identifying emotions, and longer hospital stay were identified by a few studies. Time since injury was a predictor of QOL [32, 44], while two other studies reported that as time since injury increased, so did QOL [22, 24]. There were mixed findings for identifying emotions, with one study reporting poorer QOL for those who had difficulties [45], while another study noted lower QOL for those who had better facial affect recognition [46]. Functional independence was also identified as a factor, with three studies showing associations with physical HRQOL [28, 32, 39]. Finally, longer hospitalization reported decreased QOL and was a predictor for physical functioning [30, 32, 39].
Psychological factors
There were 31 studies that reported 16 psychological QOL factors, these included depression, anxiety, other psychiatric disorders, self-efficacy, coping styles, optimistic life orientation, positive affect, positive changes, positive views of self, self-awareness, posttraumatic stress, somatic impairments, motivation, health locus of control, suicide ideation, and self-appraisal.
Mental health disorders, such as depression, anxiety, and other psychiatric disorders, lowered QOL as identified by 18 studies. Depression was the most common mental health disorder, as depression was associated with lower QOL [27, 42, 44, 47, 48] with low scores in almost all the HRQOL subscales [19, 28, 36, 49, 50] and negative correlations with QOL [35, 51]. Additionally, a prospective longitudinal study found that individuals with no depression had higher QOL than those with late onset or chronic depression, and similar scores to those who had resolved depression [52]. Anxiety was assessed along with depression, and individuals with these disorders portrayed low QOL [33, 39, 42, 47]. Similar findings were noted for other psychiatric disorders, such as substance use, eating disorders, and personality changes [32, 47, 50, 53].
Coping styles and self-efficacy were psychological QOL factors identified in this review, which described how an individual with TBI approaches difficulties and attains goals. A case–control study reported that individuals with TBI used task-oriented coping styles less often than controls; however, individuals with this type of coping style reported higher QOL [54]. Three studies highlighted non-productive or avoidance strategies after TBI, with individuals portraying lower QOL [31, 55, 56] and one study portraying negative correlations with all domains of HRQOL [55]. Self-efficacy was reported to correlate positively with QOL by two studies [29, 41]. However, in one study, while general and employment-related self-efficacy were positively correlated with perceived QOL, there was a negative correlation with a global QOL measure [29].
Individuals who experienced optimistic life orientation, positive affect, changes, and views of self had higher QOL after TBI, while those with posttraumatic stress had lower QOL [28, 51, 54, 57,58,59,60]. Viewing life with optimism post-injury was positively correlated with all HRQOL domains [54]. Additionally, experiencing positive emotions, changes, and views of self in life post-injury also facilitated QOL [28, 51, 57, 58]. Participants with posttraumatic stress had lower QOL than individuals with no posttraumatic stress [59]. Furthermore, mental HRQOL was negatively associated with posttraumatic stress symptoms after TBI [60].
Other psychological factors that were identified in this review include self-awareness, somatic impairments, motivation, self-appraisal, and suicide ideation. With regard to self-awareness, as an individual’s awareness increased, QOL decreased [38, 48]. Somatic impairments, motivation, self-appraisal, and suicide ideation were identified once by the studies in this review. Somatic impairments and self-appraisal were predictors of QOL, while low motivation and thoughts about suicide portrayed low QOL [24, 27, 35, 61].
Social factors
There were 31 studies consisting of 19 social factors that affected QOL, these included employment, income, work discrepancy, productive activities, work adjustment, education, community integration, social participation, social support, marital status, friendships, living with others, intimate relationships, social isolation, discharge destination, transition success, pre-injury sick leave, relatives interpersonal functioning, and environmental setting.
Employment was the most common social factor, with 10 studies stating that individuals who were employed had higher QOL [19, 21, 22, 28,29,30, 34, 42, 53, 62]. Individuals with pre-injury employment had higher scores in all HRQOL domains [28], and it was also a predictor for higher HRQOL [22, 42, 53]. Income, work discrepancy, engagement in productive activities, work adjustment, and education were identified as other vocational-related social factors. Income correlated and was a predictor of high QOL after TBI [29, 34], while reduced work discrepancy (e.g., how work needs are met related to perceived importance of work) was associated with low QOL [34]. Productive activities, defined as work or study programs, were another predictor of QOL [24, 63], while work adjustment correlated with QOL [31]. Individuals with more education reported better QOL [21, 25, 28, 31, 37], with some studies noting an increase in specific QOL domains such as the physical functioning [21, 28] and environmental domain [37].
Community integration and social participation increased QOL. A retrospective longitudinal study identified that more community integration and fewer activity limitations, increased QOL [64], while a cross-sectional study found that those with community integration had higher HRQOL in almost all domains [28]. Additionally, community integration was stated as a predictor for QOL [20, 57]. Social participation had a positive impact on QOL [26, 65], with one study showing that participants who socially participated in more activities with others reported high QOL [26].
Individuals who had social support, friendships, and were married had higher QOL, hence, indicating the importance of having connections after TBI. There were 7 studies that portrayed individuals with high social support reported better QOL [25, 31, 41, 54, 57, 63, 66]. Two studies noted that satisfaction of social support correlated with higher QOL [31, 54], while another study identified positive appraisals in seeking support as a predictor of high QOL [63]. A larger number of friends were a predictor for QOL [67], while losing friendships reported a low QOL score [68]. Being married and living with other individuals was highlighted by three studies in increasing QOL [24, 25, 30]. Additionally, participants who reported a low QOL were more socially isolated and had fewer intimate relationships [68].
There were six additional social factors reported, such as discharge destination, transition success, pre-injury sick leave, relatives interpersonal functioning, and environmental setting. Home discharges compared to nursing home discharges was associated with greater QOL, and increased transition success from hospital to home was correlated with higher QOL [32, 39, 69]. A history of pre-injury sick leave predicted worse QOL, relatives interpersonal functioning was associated with mental and physical HRQOL, and rural settings were a predictor for high QOL [53, 63, 70].
Discussion
This scoping review identified 52 studies, which reported factors of QOL after sustaining a TBI. The following discussion considers these factors with regard to the biological, psychological, and social domains.
Biological factors
Many studies identified sex as a biological factor of QOL [19,20,21,22,23,24,25]. However, in these studies, the sex of the participant (e.g., male, female) was reported as ‘gender.’ As we now understand gender to be a sociocultural construct [71], for this review, we have used the term sex (biological) instead. Majority of the studies indicated that females reported lower QOL [19,20,21,22,23], while a few identified that being male was linked to low QOL [24, 25]. Females are reported to have shorter hospital stays and receive less intensive care and rehabilitation after their TBI [72]. As such, females may be at risk for poorer long-term outcomes, and hence, experience a negative impact on their QOL. Sex was also the only biological factor that affected the same QOL domain in multiple studies. In four studies, females reported low QOL on the mental health domains of their QOL outcome measures. Previous literature shows that women with TBI are likely to experience more depressive symptoms than men or those without the injury [73,74,75]. Gender roles can contribute to this, as gender or power imbalances may be amplified post-injury [76, 77]. For example, if a woman occupies the role of a caregiver in their household, they may be expected to retain these duties and receive minimum assistance from others. This disparity showcases the need for support and help for women to reformulate their roles and characteristics post-injury [78].
TBI severity was a biological factor that reported mixed findings in this review. For some studies in our review, higher TBI severity was associated with higher QOL [28, 34]. Literature has noted the paradox of high severity of injury associated with better QOL, indicating that reduced awareness of injury-related deficits may be a causal factor for higher QOL [79, 80]. This also aligns with another finding from this review, as two other studies associated high self-awareness with low QOL [38, 48]. Indeed, as an individual’s self-awareness improves, the realization of deficits and consequent changes in function are more apparent, thereby decreasing their perceived QOL. There was one study that reported increasing severity resulted in lower QOL, which could be indicative of the physical and cognitive problems from a TBI [29]. However, it must be noted that the studies reporting on injury severity and QOL have most likely excluded individuals who are not able to self-report. As QOL measures are self-reported, individuals who have severe injuries from their TBI may not have the capacity to complete a QOL measure and hence, may be excluded from the study sample.
Cognitive impairment, such as deficits in attention, memory, and executive functioning, were identified as a factor that lowered QOL [27, 35,36,37, 39]. This review highlights the extent in which cognitive impairments impede everyday functions as various QOL domains (e.g., environmental, psychosocial) were impacted. For example, Gorgoraptis et al. [36] reported that the physical functioning, social and emotional role functioning, and mental health domains were all affected. Additionally, poor cognition is often associated with comorbidities such as sleep disorders which also lower QOL [81, 82], as highlighted in this review [36]. As such, these findings add to the literature that state the importance of improving cognition in rehabilitation and the need for effective interventions [83,84,85].
Fatigue, among others, were identified only once by studies in this review, indicating a gap in the research on these biological factors. Fatigue is a complex symptom with debilitating effects that is often difficult to measure objectively. Approximately up to 80% of individuals after a TBI experience fatigue [86], and it is also common in various chronic populations such as multiple sclerosis and stroke [87, 88]. While research on fatigue in the TBI population has been conducted through reviews and intervention outcomes, there is still much to explore about post-TBI fatigue and QOL.
Psychological factors
The most common psychological factor identified was mental health disorders, with depression, anxiety, and other psychiatric disorders, with individuals reporting low QOL [19, 27, 28, 32, 33, 35, 36, 39, 42, 44, 47,48,49,50,51,52,53]. The risk of depression after a TBI is doubled compared to a non-TBI population [75]. The symptoms of depression after a TBI are pervasive, as in this review, most studies reported low scores in all QOL domains. This aligns with other findings in populations such as multiple sclerosis [89], cancer [90], and Parkinsons [91]. Depression is associated with poor health and social outcomes such as a decrease in social activity, occupational function, and relationship status [92, 93], and as such, these findings highlight the importance of long-term support systems and screenings that need to be available for individuals with TBI [94].
Studies in this review have identified that active or task-oriented coping strategies, such as cognitive behavior strategies, facilitates high QOL, when compared to maladaptive strategies (i.e., avoidance, trivialization) [31, 54,55,56]. Using coping styles that are characterized by actively working on problems have indicated positive associations with emotional adjustment and positive affect post-injury [95, 96]. Using problem-solving oriented coping styles were reported to correlate with the socially related domains in this review [54, 55]. This indicates that by developing strategies and actively working on ways to manage stressful situations, individuals may find it easier to resume their social interactions [97], and hence increase their QOL.
It was surprising that only two studies explored the effects of self-awareness on QOL [38, 48], given that up to 97% of individuals with moderate to severe TBI experience some degree of impaired self-awareness [98]. Furthermore, both studies reported varying results for different QOL domains, portraying the need for more research to enhance knowledge on the effects of self-awareness on QOL. Assessing self-awareness is an essential step in TBI rehabilitation, as those with impaired self-awareness can fail to recognize their lack of capabilities [99]. This can create challenges when trying to resume meaningful roles or participate in everyday activities, both factors which can affect QOL [25].
Social factors
The most common social factor identified in this review was employment, with individuals who were employed having higher QOL [19, 21, 22, 28,29,30, 34, 42, 53, 62]. Most studies reported high scores in the physical functioning QOL domain, indicating that physical performance is a necessary factor for vocational outcomes. Notably, while returning to work is an important goal in rehabilitation [100], a longitudinal study stated that only 44% of individuals with a moderate to severe TBI return to work after 3 years post-injury due to cognitive and physical difficulties [101]. This can have a negative impact on an individual’s QOL as being employed improves many psychosocial outcomes such as self-esteem and financial independence [102, 103]. Furthermore, higher income is associated with greater QOL, as reported by this review [29, 34]. Individuals can face more expenses post-injury, such as medical costs [104]. Direct medical costs for individuals with TBI are on average $4906 higher than the medical costs for individuals with non-head injuries [105]. Earning a higher income may help these individuals manage any financial challenges and reduce finance-related stressors.
This review identified social factors of community integration, participation, and support as prominent QOL contributors. After a TBI, a ‘gap’ may be identified in activities that are more physically and cognitively challenging (e.g., return to work, playing sports) [106]. Community integration and social participation are essential after a TBI, as it facilitates the participation in new and meaningful activities, building connections, and creating new life roles [107], all of which can help improve QOL. Social support can be important in facilitating participation and also increased QOL, as highlighted in this review [25, 31, 41, 54, 57, 63, 66]. Receiving support from brain injury communities, rehabilitation programs, family, and friends provides help to navigate the new and unexpected experiences that can arise post-injury [108]. However, findings from our present review and other literature, notes that these social supports often decrease overtime, emphasizing the need for long-term supports [31, 66, 109, 110].
Transition success and discharge destination were among two social factors that were reported only a few times [32, 39, 69]. The transition post-injury from hospital to home is complex as it involves the re-integration into pre-injury settings with the added challenges that stem from a TBI (e.g., cognition, greater dependence on others). There is a need for more research about the transition phase, as increased levels of depression and stress may be experienced as individuals start to adapt to life after injury [111]. While Wielenga-Bolten et al. reported that not being discharged to a nursing home was associated with total higher HRQOL [39], individuals with moderate to severe TBI may benefit from interdisciplinary in-patient rehabilitation instead [112]. Since substantial care may be needed after a moderate to severe TBI, discharge to home may mean reduced facilities for the individual post-injury or increased caregiver burden for family members [113]. More research on understanding the meaning and lived experiences of the transition phase and being discharged to non-home settings can help identify the barriers to QOL.
Limitations
This study had three main limitations. First, as the definition and scope of QOL are vast, there were a large volume of articles obtained in this review, and this may have impacted the rigor and specificity of our review. While we provided a broad account of the data and encompassed all literature relating to this broad construct of QOL, a detailed overview of the changes in different QOL domains have not been reported. Second, our search included only published literature, as gray literature was not explored. As such, relevant articles and theses may have been excluded and limited the depth of findings. Last, this review only included articles published in English and may have limited findings to English-speaking areas of the world. As factors relating to QOL may vary in non-English-speaking countries, excluding articles published in other languages may have limited the scope of the findings.
Conclusion
This scoping review, consisting of 52 articles, identified studies that looked at the biopsychosocial factors of QOL after a moderate to severe TBI. Future research can explore how these biopsychosocial factors can be modulated to inform targeted rehabilitation interventions to improve QOL and further understand the subjective experiences about potential biopsychosocial factors of QOL. The data from this review will inform best practices of care and the development of novel rehabilitative interventions to improve outcomes for people after TBI.
Data availability
Not applicable.
References
Dewan, M. C., Rattani, A., Gupta, S., Baticulon, R. E., Hung, Y. C., Punchak, M., Agrawal, A., Adeleye, A. O., Shrime, M. G., Rubiano, A. M., Rosenfeld, J. V., & Park, K.B. (2018). Estimating the global incidence of traumatic brain injury. Journal of Neurosurg, 130(4), 1080–1097.
Scholten, A. C., Haagsma, J. A., Andriessen, T. M. J. C., Vos, P. E., Steyerberg, E. W., van Beeck, E. F., & Polinder, S. (2015). Health-related quality of life after mild, moderate and severe traumatic brain injury: Patterns and predictors of suboptimal functioning during the first year after injury. Injury, 46(4), 616–624.
Beaulieu-Bonneau, S., Fortier-Brochu, E., Ivers, H., & Morin, C. M. (2017). Attention following traumatic brain injury: Neuropsychological and driving simulator data, and association with sleep, sleepiness, and fatigue. Neuropsychological Rehabilitation, 27(2), 216–238.
Wong, A. W. K., Ng, S., Dashner, J., Baum, M. C., Hammel, J., Magasi, S., Lai, J.-S., Carlozzi, N. E., Tulsky, D. S., Miskovic, A., Goldsmith, A., & Heinemann, A. W. (2017). Relationships between environmental factors and participation in adults with traumatic brain injury, stroke, and spinal cord injury: a cross-sectional multi-center study. Quality of life research, 26(10), 2633–2645.
Whoqol Group. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409.
Harper, A., Power, M., Orley, J., Herrman, H., Schofield, H., & Murphy, B. (1998). THE WHOQOL GROUP Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychological Medicine, 28(3), 551–558.
Polinder, S., Haagsma, J. A., van Klaveren, D., Steyerberg, E. W., & van Beeck, E. F. (2015). Health-related quality of life after TBI: A systematic review of study design, instruments, measurement properties, and outcome. Population Health Metrics, 13(1), 4.
Corrigan, J. D., & Hammond, F. M. (2013). Traumatic brain injury as a chronic health condition. Archives of Physical Medicine and Rehabilitation, 94, 1199–1201.
Ruet, A., Bayen, E., Jourdan, C., Ghout, I., Meaude, L., Lalanne, A., Pradat-Diehl, P., Nelson, G., Charanton, J., Aegerter, P., & Vallat-Azouvi, C. (2019). A detailed overview of long-term outcomes in severe traumatic brain injury eight years post-injury. Frontiers in Neurology, 10, 120.
Irtelli F, Durbano F. Quality of life and biopsychosocial paradigm: A narrative review of the concept and specific insights. In: Quality of Life - Biopsychosocial Perspectives. 2020.
di Battista, A., Soo, C., Catroppa, C., & Anderson, V. (2012). Quality of life in children and adolescents post-TBI: A systematic review and meta-analysis. Journal of Neurotrauma, 29(9), 1717–1727.
Dijkers, M. P. (2004). Quality of life after traumatic brain injury: A review of research approaches and findings. Archives of physical medicine and rehabilitation, 85(SUPPL. 2), S21-35.
Berger, E., Leven, F., Pirente, N., Bouillon, B., & Neugebauer, E. (1999). Quality of life after traumatic brain injury: A systematic review of the literature. Restorative Neurology and Neuroscience, 14(23), 93–102.
Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology: Theory and Practice, 8(1), 19–32.
Levac, D., Colquhoun, H., & O’Brien, K. K. (2010). Scoping studies: Advancing the methodology. Implementation Science, 5(1), 69.
Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169, 467–473.
Veritas Health Innovation. Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. 2020; Available at www.covidence.org. Melbourne Australia. 2018.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. The BMJ, 372, 71.
Andelic, N., Hammergren, N., Bautz-Holter, E., Sveen, U., Brunborg, C., & Røe, C. (2009). Functional outcome and health-related quality of life 10 years after moderate-to-severe traumatic brain injury. Acta Neurologica Scandinavica, 120(1), 16–23.
Andelic, N., Howe, E. I., Hellstrøm, T., Sanchez, M. F., Lu, J., Løvstad, M., & Røe, C. (2018). Disability and quality of life 20 years after traumatic brain injury. Brain Behavior, 8(7), e01018.
Andelic, N., Perrin, P. B., Forslund, M. V., Soberg, H. L., Sigurdardottir, S., Sveen, U., Jerstad, T., & Roe, C. (2015). Trajectories of physical health in the first 5 years after traumatic brain injury. Journal of Neurologgy, 262(3), 523–531.
Forslund, M. V., Perrin, P. B., Sigurdardottir, S., Howe, E. I., van Walsem, M. R., Arango-Lasprilla, J. C., Lu, J., Aza, A., Jerstad, T., Røe, C., & Andelic, N. (2021). Health-related quality of life trajectories across 10 years after moderate to severe traumatic brain injury in Norway. Journal of Clinical Medicine, 10(1), 1–14.
Rauen, K., Späni, C. B., Tartaglia, M. C., Ferretti, M. T., Reichelt, L., Probst, P., Schäpers, B., Müller, F., Jahn, K., & Plesnila, N. (2021). Quality of life after traumatic brain injury: A cross-sectional analysis uncovers age- and sex-related differences over the adult life span. Geroscience, 43(1), 263–278.
Jacobsson, L. J., Westerberg, M., & Lexell, J. (2010). Health-related quality-of-life and life satisfaction 615 years after traumatic brain injuries in northern Sweden. Brain Injury, 24(9), 1075–1086.
Steadman-Pare, D., Colantonio, A., Ratcliff, G., & Chase, S. (2001). Factors associated with perceived quality of life many years after traumatic brain injury. The Journal of Head Trauma Rehabilitation, 16(4), 330–342.
McLean, A. M., Jarus, T., Hubley, A. M., & Jongbloed, L. (2014). Associations between social participation and subjective quality of life for adults with moderate to severe traumatic brain injury. Disability and Rehabilitation, 36(17), 1409–1418.
Azouvi, P., Ghout, I., Bayen, E., Darnoux, E., Azerad, S., Ruet, A., Vallat-Azouvi, C., Pradat-Diehl, P., Aegerter, P., Charanton, J., & Jourdan, C. (2016). Disability and health-related quality-of-life 4 years after a severe traumatic brain injury: A structural equation modelling analysis. Brain Injury, 30(13–14), 1665–1671.
Forslund, M. V., Roe, C., Sigurdardottir, S., & Andelic, N. (2013). Predicting health-related quality of life 2 years after moderate-to-severe traumatic brain injury. Acta Neurologica Scandinavica, 128(4), 220–227.
Tsaousides, T., Warshowsky, A., Ashman, T. A., Cantor, J. B., Spielman, L., & Gordon, W. A. (2009). The relationship between employment-related self-efficacy and quality of life following traumatic brain injury. Rehabilitation Psychology, 54(3), 299–305.
Van Delft-Schreurs, C. C. H. M., Van Bergen, J. J. M., De Jongh, M. A. C., Van De Sande, P., Verhofstad, M. H. J., & De Vries, J. (2014). Quality of life in severely injured patients depends on psychosocial factors rather than on severity or type of injury. Injury, 45(1), 320–326.
Tomberg, T., Toomela, A., Ennok, M., & Tikk, A. (2007). Changes in coping strategies, social support, optimism and health-related quality of life following traumatic brain injury: A longitudinal study. Brain Injury, 21(5), 479–488.
Grauwmeijer, E., Heijenbrok-Kal, M. H., & Ribbers, G. M. (2014). Health-related quality of life 3 years after moderate to severe traumatic brain injury: A prospective cohort study. Archives of Physical Medicine and Rehabilitation, 95(7), 1268–1276.
Rauen, K., Reichelt, L., Probst, P., Schäpers, B., Müller, F., Jahn, K., & Plesnila, N. (2020). Quality of life up to 10 years after traumatic brain injury: A cross-sectional analysis. Health and Quality of Life Outcomes, 18(1), 166.
Tsaousides, T., Ashman, T., & Seter, C. (2008). The Psychological Effects of Employment After Traumatic Brain Injury: Objective and Subjective Indicators. Rehabilitation Psychology, 53(4), 456–463.
Esbjörnsson, E., Skoglund, T., & Sunnerhagen, K. S. (2013). Fatigue, psychosocial adaptation and Quality of Life ONE year after traumatic brain injury and suspected traumatic axonal injury; Evaluations of patients and relatives: A pilot study. Journal of Rehabilitation Medicine, 45(8), 771–777.
Gorgoraptis, N., Zaw-Linn, J., Feeney, C., Tenorio-Jimenez, C., Niemi, M., Malik, A., Ham, T., Goldstone, A. P., & Sharp, D. J. (2019). Cognitive impairment and health-related quality of life following traumatic brain injury. NeuroRehabilitation, 44(3), 321–331.
Reddy, R. P., Rajeswaran, J., Devi, B. I., & Kandavel, T. (2017). Cascade of traumatic brain injury: A correlational study of cognition, postconcussion symptoms, and quality of life. Indian Journal of Psychological Medicine, 39(1), 32–39.
Pettemeridou, E., Kennedy, M. R. T., & Constantinidou, F. (2020). Executive functions, self-awareness and quality of life in chronic moderate-to-severe TBI. NeuroRehabilitation, 46(1), 109–118.
Wielenga-Boiten, J. E., Heijenbrok-Kal, M. H., & Ribbers, G. M. (2015). The relationship of health locus of control and health-related quality of life in the chronic phase after traumatic brain injury. Journal of Head Trauma Rehabilitation, 30(6), 424–431.
Williams, G., & Willmott, C. (2012). Higher levels of mobility are associated with greater societal participation and better quality-of-life. Brain Injury, 26(9), 1065–1071.
Johnson, K., & Ditchman, N. (2020). Mediators of quality of life in brain injury. Brain Injury, 34(12), 1636–1645.
Soberg, H. L., Røe, C., Anke, A., Arango-Lasprilla, J. C., Skandsen, T., Sveen, U., Steinbüchel, N., Andelic, N. (2013). Health-related quality of life 12 months after severe traumatic brain injury: A prospective nationwide cohort study. Journal of Rehabilitation Medicine, 45(8), 785–791.
Cantor, J. B., Ashman, T., Gordon, W., Ginsberg, A., Engmann, C., Egan, M., Spielman, L., Dijkers, M., & Flanagan, S. (2008). Fatigue after traumatic brain injury and its impact on participation and quality of life. Journal of Head Trauma Rehabilitation, 23, 41–51.
Goverover, Y., Genova, H., Smith, A., Chiaravalloti, N., & Lengenfelder, J. (2017). Changes in activity participation following traumatic brain injury. Neuropsychological Rehabilitation, 27(4), 472–485.
Henry, J. D., Phillips, L. H., Crawford, J. R., Theodorou, G., & Summers, F. (2006). Cognitive and psychosocial correlates of alexithymia following traumatic brain injury. Neuropsychologia, 44(1), 62–72.
Genova, H. M., Genualdi, A., Goverover, Y., Chiaravalloti, N. D., Marino, C., & Lengenfelder, J. (2017). An investigation of the impact of facial affect recognition impairments in moderate to severe TBI on fatigue, depression, and quality of life. Social Neuroscience, 12(3), 303–307.
Gould, K. R., Ponsford, J. L., Johnston, L., & Schönberger, M. (2011). Predictive and associated factors of psychiatric disorders after traumatic brain injury: A prospective study. Journal of Neurotrauma, 28(7), 1155–1163.
Goverover, Y., & Chiaravalloti, N. (2014). The impact of self-awareness and depression on subjective reports of memory, quality-of-life and satisfaction with life following TBI. Brain Injury, 28(2), 174–180.
Grauwmeijer, E., Heijenbrok-Kal, M. H., Peppel, L. D., Hartjes, C. J., Haitsma, I. K., de Koning, I., & Ribbers GM. (2018). Cognition, health-related quality of life, and depression ten years after moderate to severe traumatic brain injury: A prospective cohort study. Journal of Neurotrauma, 35(13), 1543–1551.
Diaz, A. P., Schwarzbold, M. L., Thais, M. E., Hohl, A., Bertotti, M. M., Schmoeller, R., Nunes, J. C., Prediger, R., Linhares, M. N., Guarnieri, R., & Walz, R. (2012). Psychiatric disorders and health-related quality of life after severe traumatic brain injury: A prospective study. Journal of Neurotrauma, 29, 1029–1037.
Vickery, C. D., Gontkovsky, S. T., & Caroselli, J. S. (2005). Self-concept and quality of life following acquired brain injury: A pilot investigation. Brain Injury, 19(9), 657–665.
Hibbard, M. R., Ashman, T. A., Spielman, L. A., Chun, D., Charatz, H. J., & Melvin, S. (2004). Relationship between depression and psychosocial functioning after traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 85(SUPPL. 2), 43–53.
Ulfarsson, T., Lundgren-Nilsson, Å., Blomstrand, C., & Nilsson, M. (2014). A history of unemployment or sick leave influences long-term functioning and health-related quality-of-life after severe traumatic brain injury. Brain Injury, 28(3), 328–335.
Tomberg, T., Toomela, A., Pulver, A., & Tikk, A. (2005). Coping strategies, social support, life orientation and health-related quality of life following traumatic brain injury. Brain Injury, 19(14), 1181–1190.
Sasse, N., Gibbons, H., Wilson, L., Martinez, R., Sehmisch, S., Von Wild, K., Von Steinbüchel, N. (2014). Coping strategies in individuals after traumatic brain injury: Associations with health-related quality of life. Disability and Rehabilitation, 36(25), 2152–2160.
Gregório, G. W., Gould, K. R., Spitz, G., van Heugten, C. M., & Ponsford, J. L. (2014). Changes in self-reported pre-to postinjury coping styles in the first 3 years after traumatic brain injury and the effects on psychosocial and emotional functioning and quality of life. Journal of Head Trauma Rehabilitation, 29(3), E43–E53.
Kalpakjian, C. Z., Lam, C. S., Toussaint, L. L., & Merbitz, N. K. H. (2004). Describing quality of life and psychosocial outcomes after traumatic brain injury. American Journal of Physical Medicine and Rehabilitation, 83(4), 255–265.
Gould, K. R., & Ponsford, J. L. (2015). A longitudinal examination of positive changes in quality-of-life after traumatic brain injury. Brain Injury, 29(3), 283–290.
Alway, Y., McKay, A., Gould, K. R., Johnston, L., & Ponsford, J. (2016). Factors associated with posttraumatic stress disorder following moderate to severe traumatic brain injury: A prospective study. Depression and Anxiety, 33(1), 19–26.
Bosma, C. M., Mansoor, N., & Haller, C. S. (2018). Association of posttraumatic stress symptom severity with health-related quality of life and self-reported functioning across 12 months after severe traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 99(8), 1576–1583.
Tsaousides, T., Cantor, J. B., & Gordon, W. A. (2011). Suicidal ideation following traumatic brain injury: Prevalence rates and correlates in adults living in the community. Journal of Head Trauma Rehabilitation, 26(4), 265–275.
O’Neill, J., Hibbard, M. R., Brown, M., Jaffe, M., Sliwinski, M., Vandergoot, D., & Weiss, M. J. (1998). The effect of employment on quality of life and community integration after traumatic brain injury. Journal of Head Trauma Rehabilitation, 13(4), 68–79.
Farmer, J. E., Clark, M. J., & Sherman, A. K. (2003). Rural Versus Urban Social Support Seeking as a Moderating Variable in Traumatic Brain Injury Outcome. Journal of Head Trauma Rehabilitation, 18(2), 116–127.
Huebner, R. A., Johnson, K., Bennett, C. M., & Schneck, C. (2003). Community participation and quality of life outcomes after adult traumatic brain injury. The American Journal of Occupational Therapy, 57(2), 177–185.
Sashika, H., Takada, K., & Kikuchi, N. (2017). Rehabilitation needs and participation restriction in patients with cognitive disorder in the chronic phase of traumatic brain injury. Medicine, 96(4), e5968.
Takada, K., Sashika, H., Wakabayashi, H., & Hirayasu, Y. (2016). Social participation and quality-of-life of patients with traumatic brain injury living in the community: A mixed methods study. Brain Injury, 30(13–14), 1590–1598.
Douglas, J. (2020). Loss of friendship following traumatic brain injury: A model grounded in the experience of adults with severe injury. Neuropsychological Rehabilitation, 30(7), 1277–1302.
Koskinen, S. (1998). Quality of life 10 years after a very severe traumatic brain injury (TBI): the perspective of the injured and the closest relative. Brain Injury, 12(8), 631–648.
Nalder, E., Fleming, J., Foster, M., Cornwell, P., Shields, C., & Khan, A. (2012). Identifying factors associated with perceived success in the transition from hospital to home after brain injury. Journal of Head Trauma Rehabilitation, 27(2), 143–153.
Gaertner, L. H. C., Tsur, N., & Haller, C. S. (2020). Patients’ recovery after severe TBI is associated with their close relatives’ interpersonal functioning: A 12-months prospective cohort study. Brain Injury, 34(6), 764–772.
Lorber J. The Social Construction of Gender. In: Inequality in the 21st Century: A Reader. 2018.
Mikolić, A., van Klaveren, D., Groeniger, J. O., Wiegers, E. J., Lingsma, H. F., Zeldovich, M., von Steinbüchel, N., Maas, A. I., van Lennep, R. J. E., Polinder, S., CENTER-TBI Participants and Investigators. (2021). Differences between men and women in treatment and outcome after traumatic brain injury. Journal of Neurotrauma, 38(2), 235–251.
Chase, S., Ratcliff, G., Vernich, L., Al-Sukhni, E., Yasseen, B., & Colantonio, A. (2012). Preventive health practices and behavioral risk factors in women surviving traumatic brain injury. Health Care for Women International, 33(7), 631–645.
Lavoie, S., Sechrist, S., Quach, N., Ehsanian, R., Duong, T., Gotlib, I. H., & Isaac, L. (2017). Depression in men and women one year following traumatic brain injury (TBI): A TBI model systems study. Frontiers in Psychology, 8, 634.
Albrecht, J. S., Barbour, L., Abariga, S. A., Rao, V., & Perfetto, E. M. (2019). Risk of Depression after Traumatic Brain Injury in a Large National Sample. Journal of Neurotrauma, 36(2), 300–307.
Fabricius, A. M., D’Souza, A., Amodio, V., Colantonio, A., & Mollayeva, T. (2020). Women’s gendered experiences of traumatic brain injury. Qualitative Health Research, 30(7), 1033–1044.
Alston, M., Jones, J., & Curtin, M. (2012). Women and traumatic brain injury: “It’s not visible damage.” Australian Social Work, 65(1), 39–53.
Haag, H. L., Caringal, M., Sokoloff, S., Kontos, P., Yoshida, K., & Colantonio, A. (2016). Being a woman with acquired brain injury: Challenges and implications for practice. Archives of Physical Medicine and Rehabilitation, 97, S64–S70.
Siponkoski, S. T., Wilson, L., von Steinbüchel, N., Sarajuuri, J., & Koskinen, S. (2013). Quality of life after traumatic brain injury: finnish experience of the qolibri in residential rehabilitation. Journal of Rehabilitation Medicine, 45(8), 835–842.
Sasse, N., Gibbons, H., Wilson, L., Martinez-Olivera, R., Schmidt, H., Hasselhorn, M., von Wild, K., & von Steinbüchel, N. (2013). Self-awareness and health-related quality of life after traumatic brain injury. Journal of Head Trauma Rehabilitation, 28(6), 464–472.
Wilde, M. C., Castriotta, R. J., Lai, J. M., Atanasov, S., Masel, B. E., & Kuna, S. T. (2007). Cognitive impairment in patients with traumatic brain injury and obstructive sleep apnea. Archives of Physical Medicine and Rehabilitation, 88(10), 1284–1288.
Duclos, C., Beauregard, M. P., Bottari, C., Ouellet, M. C., & Gosselin, N. (2015). The impact of poor sleep on cognition and activities of daily living after traumatic brain injury: A review. Australian Occupational Therapy Journal, 62, 2.
De Luca, R., Calabrò, R. S., & Bramanti, P. (2018). Cognitive rehabilitation after severe acquired brain injury: current evidence and future directions. Neuropsychological Rehabilitation, 28, 579–898.
Barman, A., Chatterjee, A., & Bhide, R. (2016). Cognitive impairment and rehabilitation strategies after traumatic brain injury. Indian Journal of Psychological Medicine, 38, 172–181.
Skandsen, T., Finnanger, T. G., Andersson, S., Lydersen, S., Brunner, J. F., & Vik, A. (2010). Cognitive impairment 3 months after moderate and severe traumatic brain injury: A prospective follow-up study. Archives of Physical Medicine and Rehabilitation, 91(12), 1904–1913.
Mollayeva, T., Kendzerska, T., Mollayeva, S., Shapiro, C. M., Colantonio, A., & Cassidy, J. D. (2014). A systematic review of fatigue in patients with traumatic brain injury: The course, predictors and consequences. Neuroscience and Biobehavioral Reviews, 47, 684–716.
Capone, F., Collorone, S., Cortese, R., Di Lazzaro, V., & Moccia, M. (2020). Fatigue in multiple sclerosis: The role of thalamus. Multiple Sclerosis Journal, 26, 6–16.
Acciarresi, M., Bogousslavsky, J., & Paciaroni, M. (2014). Post-stroke fatigue: Epidemiology, clinical characteristics and treatment. European Neurology, 72, 255–261.
Fruewald, S., Loeffler-Stastka, H., Eher, R., Saletu, B., & Baumhacki, U. (2001). Depression and quality of life in multiple sclerosis. Acta Neurologica Scandinavica, 104(5), 257–261.
Purkayastha, D., Venkateswaran, C., Nayar, K., & Unnikrishnan, U. G. (2017). Prevalence of depression in breast cancer patients and its association with their quality of life: A cross-sectional observational study. Indian Journal of Palliative Care, 23(3), 268.
Su, W., Liu, H., Jiang, Y., Li, S., Jin, Y., Yan, C., & Chen, H. (2021). Correlation between depression and quality of life in patients with Parkinson’s disease. Clinical Neurology and Neurosurgery, 202, 106523.
Roy, D., Koliatsos, V., Vaishnavi, S., Han, D., & Rao, V. (2018). Risk factors for new-onset depression after first-time traumatic brain injury. Psychosomatics, 59(1), 47–57.
Whelan-Goodinson, R., Ponsford, J., & Schönberger, M. (2008). Association between psychiatric state and outcome following traumatic brain injury. Journal of Rehabilitation Medicine, 40(10), 850–587.
Stalder-Lüthy, F., Messerli-Bürgy, N., Hofer, H., Frischknecht, E., Znoj, H., & Barth, J. (2013). Effect of psychological interventions on depressive symptoms in long-term rehabilitation after an acquired brain injury: A systematic review and meta-analysis. Archives of Physical Medicine and Rehabilitation, 94, 1386–1397.
Anson, K., & Ponsford, J. (2006). Coping and emotional adjustment following traumatic brain injury. Journal of Head Trauma Rehabilitation, 21(3), 248–259.
Nalder, E., Hartman, L., Hunt, A., & King, G. (2019). Traumatic brain injury resiliency model: A conceptual model to guide rehabilitation research and practice. Disability and Rehabilitation, 41(22), 2708–2717.
Lundqvist, A., & Samuelsson, K. (2012). Return to work after acquired brain injury: A patient perspective. Brain Injury, 26(13–14), 1574–1585.
Sherer, M., Bergloff, P., Levin, E., High, W. M., Jr., Oden, K. E., & Nick, T. G. (1998). Impaired awareness and employment outcome after traumatic brain injury. Journal of Head Trauma Rehabilitation, 13(5), 52–61.
Toglia, J., & Kirk, U. (2000). Understanding awareness deficits following brain injury. NeuroRehabilitation, 15(1), 57–70.
Stergiou-Kita, M., Rappolt, S., & Dawson, D. (2012). Towards developing a guideline for vocational evaluation following traumatic brain injury: The qualitative synthesis of clients’ perspectives. Disability and Rehabilitation, 34(3), 179–188.
Ponsford, J. L., & Spitz, G. (2015). Stability of employment over the first 3 years following traumatic brain injury. The Journal of Head Trauma Rehabilitation, 30(3), E1-11.
Libeson, L., Ross, P., Downing, M., & Ponsford, J. (2022). Exploring employment following traumatic brain injury in persons who completed an insurer funded vocational rehabilitation program in Australia. Disability and Rehabilitation, 44(24), 7428–7438.
Matérne, M., Strandberg, T., & Lundqvist, L. O. (2018). Change in quality of life in relation to returning to work after acquired brain injury: a population-based register study. Brain Injury, 32(13–14), 1731–1739.
Fu, T. S., Jing, R., McFaull, S. R., & Cusimano, M. D. (2016). Health & economic burden of traumatic brain injury in the emergency department. Canadian Journal of Neurological Sciences, 43(2), 238–247.
Leibson, C. L., Brown, A. W., Hall Long, K., Ransom, J. E., Mandrekar, J., Osler, T. M., & Malec, J. F. (2012). Medical care costs associated with traumatic brain injury over the full spectrum of disease: A controlled population-based study. Journal of Neurotrauma, 29(11), 2038–2049.
Beadle, E. J., Ownsworth, T., Fleming, J., & Shum, D. H. K. (2020). The nature of occupational gaps and relationship with mood, psychosocial functioning and self-discrepancy after severe traumatic brain injury. Disability and Rehabilitation, 42(10), 1414–1422.
Douglas, J. M. (2013). Conceptualizing self and maintaining social connection following severe traumatic brain injury. Brain Injury, 27(1), 60–74.
Fadyl, J. K., Theadom, A., Channon, A., & McPherson, K. M. (2017). Recovery and adaptation after traumatic brain injury in New Zealand: Longitudinal qualitative findings over the first two years. Neuropsychological Rehabilitation, 29, 1095–1112.
Strandberg, T. (2009). Adults with acquired traumatic brain injury: Experiences of a changeover process and consequences in everyday life. Social Work in Health Care, 48(3), 276–297.
Stiekema, A. P. M., Winkens, I., Ponds, R., de Vugt, M. E., & van Heugten, C. M. (2020). Finding a new balance in life: A qualitative study on perceived long-term needs of people with acquired brain injury and partners. Brain Injury, 34(3), 421–429.
Turner, B., Fleming, J., Cornwell, P., Haines, T., & Ownsworth, T. (2009). Profiling early outcomes during the transition from hospital to home after brain injury. Brain Injury, 23(1), 51–60.
Rosenbaum, A. M., Gordon, W. A., Joannou, A., & Berman, B. A. (2018). Functional outcomes following post-acute rehabilitation for moderate-to-severe traumatic brain injury. Brain Injury, 32(7), 907–914.
Kreitzer, N., Bakas, T., Kurowski, B., Lindsell, C. J., Ferioli, S., Foreman, B., Ngwenya, L. B., Thomas, S., Keegan, S., & Adeoye, O. (2020). The Experience of Caregivers Following a Moderate to Severe Traumatic Brain Injury Requiring ICU Admission. Journal of Head Trauma Rehabilitation, 35(3), E299–E309.
Acknowledgements
The authors would like to thank research assistants Alyssa Turcott, Anika Cheng, Rebecca Tsow, and RJ Kang, and health-sciences reference librarian Charlotte Beck for their help in this study. The authors would also like to thank the Vancouver Foundation Participatory Action Research Grant for funding this study.
Funding
This study was funded by the Vancouver Foundation Participatory Action Research Grant.
Author information
Authors and Affiliations
Contributions
All authors have contributed to the study concept, design, and analysis of the data. RM, JG, JNG, and JS have screened the data, and RM and JG have extracted the data. RM is the major contributor in writing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Ethical approval
This is a scoping review. The Research Ethics Board of the University of British Columbia has confirmed that no ethical approval is required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mamman, R., Grewal, J., Garrone, J.N. et al. Biopsychosocial factors of quality of life in individuals with moderate to severe traumatic brain injury: a scoping review. Qual Life Res 33, 877–901 (2024). https://doi.org/10.1007/s11136-023-03511-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03511-0