Abstract
Delivery of neuropsychological interventions addressing the cognitive, psychological, and behavioural consequences of brain conditions is increasingly recognised as an important, if not essential, skill set for clinical neuropsychologists. It has the potential to add substantial value and impact to our role across clinical settings. However, there are numerous approaches to neuropsychological intervention, requiring different sets of skills, and with varying levels of supporting evidence across different diagnostic groups. This clinical guidance paper provides an overview of considerations and recommendations to help guide selection, delivery, and implementation of neuropsychological interventions for adults and older adults. We aimed to provide a useful source of information and guidance for clinicians, health service managers, policy-makers, educators, and researchers regarding the value and impact of such interventions. Considerations and recommendations were developed by an expert working group of neuropsychologists in Australia, based on relevant evidence and consensus opinion in consultation with members of a national clinical neuropsychology body. While the considerations and recommendations sit within the Australian context, many have international relevance. We include (i) principles important for neuropsychological intervention delivery (e.g. being based on biopsychosocial case formulation and person-centred goals); (ii) a description of clinical competencies important for effective intervention delivery; (iii) a summary of relevant evidence in three key cohorts: acquired brain injury, psychiatric disorders, and older adults, focusing on interventions with sound evidence for improving activity and participation outcomes; (iv) an overview of considerations for sustainable implementation of neuropsychological interventions as ‘core business’; and finally, (v) a call to action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Background
In Australia, and many other countries around the world, the role of the clinical neuropsychologist in diagnostic assessment has long been emphasised, recognising the specialised skills neuropsychologists bring to identifying the presence, extent, and impact of cognitive and psychosocial sequelae associated with brain conditions across the lifespan. However, given its fundamental origins in human psychology and behaviour, its biopsychosocial approach to understanding individuals with brain conditions, and its emphasis on evidence-based practice, clinical neuropsychology also provides an invaluable framework for developing, providing, and evaluating interventions that target cognitive, emotional, behavioural, and psychosocial difficulties to improve overall functioning. New technologies that assist with diagnosis of brain conditions have led to a changing role of clinical neuropsychologists, with an increasing focus on the delivery of effective interventions.
Despite a long history of research and practice in neuropsychological interventions (Brouwer, 2002; Ponsford et al., 1995; Zangwill, 1947) and a quickly growing evidence base (Wilson, 2017), this aspect of clinical neuropsychological practice remains under-recognised among medical specialists, allied health practitioners, health policy-makers, and the lay public in many Australian settings (exemplified by the Stroke Foundation’s, 2020 Rehabilitation Services audit: https://informme.org.au/stroke-data/Rehabilitation-audits). This limits our ability to optimally contribute to patient care and management. Many neuropsychologists in Australia lack confidence in delivering neuropsychological interventions, at least partly due to limited opportunities for supervised practice during postgraduate training (Wong et al., 2014). These factors have led to gaps in the understanding and delivery of neuropsychological interventions in Australian clinical settings, which limits access to evidence-based care for individuals with brain conditions (e.g. Andrew et al., 2014; Naismith et al., 2022). We hope that this clinical guidance paper will represent one step towards addressing this lack of access. In response to changes to the opportunities available for funding neuropsychological interventions in Australia (e.g. the National Disability Insurance Scheme) and in order to open up further funding avenues (e.g. Medicare), it is imperative that we have high quality evidence for these interventions, and that our training programs are equipping clinical neuropsychologists with the competencies necessary to deliver evidence-based interventions effectively.
Aims
This clinical guidance paper aims to provide an overview of key considerations in the effective delivery of neuropsychological interventions; clinical competencies important for intervention delivery; and clinical implementation of evidence-based interventions, alongside a summary of available evidence for their efficacy in the following populations:
-
Acquired brain injury/illness (including stroke, traumatic brain injury, and multiple sclerosis);
-
Psychiatric conditions (including early psychosis, schizophrenia, bipolar disorder, depression and eating disorders);
-
Older adults (ranging from healthy ageing through mild cognitive impairment to dementia).
We acknowledge that this is not an exhaustive list of the potential groups with which neuropsychological interventions can be conducted; however, both research and practice are the most prominent in these cohorts. The evidence-based practice principles outlined both generally and for these specific groups are likely to apply to interventions delivered with people with other primary diagnoses (e.g. adult ADHD), although clinicians are encouraged to explore the evidence base for these specific cohorts to determine which approaches or techniques may be most appropriate and effective. Pragmatically, and in recognition of the unique clinical, psychosocial, and environmental parameters of relevance to interventions in children and adolescents, only neuropsychological interventions conducted with adult and older adult populations will be included in this clinical guidance paper.
We do not aim to provide a systematic or meta-analytical review of the evidence, as in many cases, this has been done previously. Where available, we will draw on and cite such existing reviews (see ‘Resources’ section for a list of key systematic reviews). We have also not performed a systematic appraisal of the quality of evidence for each intervention type, as would be expected for formal clinical guidelines (which is one of the reasons we have termed this a ‘clinical guidance paper’). This is because there is a large number of cognitive, psychological and behavioural interventions reviewed for each cohort, and to provide a systematic appraisal of evidence quality would be a very substantial undertaking that was beyond the scope of this paper. Rather, we have provided a synthesis of existing findings, particularly regarding the nature of available evidence for interventions with meaningful impacts on everyday life, as well as guidance and recommendations for a ‘best practice’ approach to incorporating these interventions clinically.
In doing so, we also aim to:
-
(i)
Outline the role of clinical neuropsychologists in delivering neuropsychological interventions in Australia, while acknowledging interstate variability in training and roles within the public and private healthcare systems;
-
(ii)
Highlight issues to consider in the planning and implementation of neuropsychological interventions for various patient groups;
-
(iii)
Address key issues impacting the effectiveness of neuropsychological interventions, relating to the (a) client, (b) clinician, and (c) intervention technique;
-
(iv)
Recognise the role and value of neuropsychological interventions in collaboration with other allied health and medical disciplines (e.g. occupational therapy, speech pathology).
We anticipate this paper may provide a starting point for future development of formal clinical guidelines regarding the use of neuropsychological interventions. At a broader level, we hope this paper may also provide an impetus for further collaborative and multidisciplinary research into developing, evaluating, and implementing neuropsychological interventions in Australia and internationally.
Intended Audience
This clinical guidance paper is aimed primarily at clinical neuropsychologists with involvement, or intended involvement, in delivering neuropsychological interventions across a range of populations. It may also be useful for clinicians and researchers in other disciplines working within a multidisciplinary setting, where neuropsychological interventions may represent a component of a team-based therapeutic approach. In this case, the evidence and issues discussed herein may provide some context and parameters around the utility or expected outcomes from the neuropsychological intervention and how it may best be integrated alongside other medical or allied health interventions. Communication to our multidisciplinary colleagues about the potential benefits that neuropsychologists can offer was a critical need identified by Kubu et al. (2016); indeed, access to guidance papers detailing the value of neuropsychology was one of their specific recommendations.
We acknowledge that this paper has been written in the Australian context and that some issues (particularly relating to training, work roles, or funding) may differ in other countries. We have acknowledged these differences wherever relevant throughout the paper. We welcome commentary and perspectives from international colleagues about how the contents of this paper may apply in other countries.
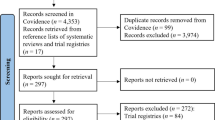
Development and Methodology
The concept for this paper was initially raised by Professor Sharon Naismith, following a symposium she led on this topic at the annual conference of the Australian Psychological Society’s College of Clinical Neuropsychologists (CCN), held in Melbourne, Victoria, September 2016.
The proposal was supported and a working party convened, comprising a network of clinical neuropsychologists actively working or researching the development, evaluation, or implementation of neuropsychological interventions. With support from Professor Naismith, A/Prof Dana Wong and Dr Loren Mowszowski were voluntarily appointed as co-chairs. Potential working party members were identified through professional networks and invited to participate on a voluntary basis. An effort was made to engage members throughout Australia, while limiting the number of members to a maximum of 15, to maintain project feasibility.
Once convened, the working party communicated via emails and teleconferences to develop a proposed outline regarding the aims of the paper, the populations to include, and key additional issues to include in the discussion (see the ‘Aims’ section, above). Subsections were allocated on a voluntary basis and according to areas of specialised skill or expertise.
The proposed paper outline was presented at an Open Forum event to delegates of the CCN’s annual conference in Perth, Western Australia (November 2017). Approximately 40 people attended the Open Forum, mostly neuropsychologists. During the forum, the working party requested feedback, comments, and suggestions from attendees regarding the proposed aims and outline of the clinical guidance paper. This feedback was documented, subsequently relayed to working party members not in attendance, and the aims and outline were amended accordingly. We note that few amendments were requested.
Thereafter, the working party proceeded to draft the paper according to their allocated subsections. All working party members reviewed each subsection and the entire paper to ensure consensus, consistency, and completeness. In April 2018, a paper draft was forwarded to the CCN Executive Committee, who provided feedback in September 2018. The working party subsequently amended the paper taking into consideration these comments and any updates in the field. Following this iterative process, a second draft was distributed to the CCN Executive Committee and overseeing expert Professor Sharon Naismith in 2020–2021. A presentation was also made to over 100 people outlining the contents of the paper as part of a CCN webinar (though non-CCN members also attended) in 2021, and attendees were invited to provide feedback, which was constructive and positive. Further revisions were made by the working party in 2021, with the revised version distributed to the CCN membership (966 members, including student members) for feedback towards the end of 2021. Respondents to this consultation supported the accuracy, clarity, and organisation of the contents, issues covered, evidence base, and usefulness of the paper. Feedback from respondents was considered when preparing the final version. Although CCN members were consulted, the expert working group are responsible for the contents of the paper.
Section 1: Characterising Neuropsychological Interventions
Defining Neuropsychological Interventions
There are multiple ways in which ‘neuropsychological interventions’ could be defined. For this clinical guidance paper, we define a neuropsychological intervention as an intervention that targets the cognitive, emotional, psychosocial, and/or behavioural consequences of conditions affecting the brain.
There are several points we wish to note about this definition. Firstly, we have chosen not to define ‘neuropsychological interventions’ according to the type or content of the intervention, as these are numerous. However, for the purpose of this paper, we will classify neuropsychological intervention types into the following main categories:
-
(i)
Psychoeducation (including feedback after neuropsychological assessment)
-
(ii)
Cognitive remediation/rehabilitation (encompassing restorative and compensatory approaches)
-
(iii)
Psychological therapies (e.g. cognitive behaviour therapy)
-
(iv)
Behaviour management (e.g. positive behaviour support plans)
-
(v)
Environmental modifications and supports
These categories are very similar to those used by Wong et al. (2014) in their survey about the experiences of Australian neuropsychology graduates in delivering neuropsychological interventions. However, we acknowledge there are many variations in the labelling of these intervention types. This is particularly true for cognitive remediation/rehabilitation, which can encompass cognitive training, stimulation, and management using compensatory strategies, among other things. Throughout this paper, where evidence is specific to a particular intervention type, descriptive details will be included for clarity. It is also worth noting that categorising interventions by type or technique may falsely imply that these intervention types are standalone or separate; however, many neuropsychological interventions incorporate content from several of these categories and may be delivered in conjunction with other interventions (e.g. speech pathology, occupational therapy, medical or lifestyle interventions).
We also acknowledge there are other types of interventions that may be used to improve cognition or brain function, including pharmacological interventions and brain stimulation approaches (e.g. transcranial magnetic stimulation). We consider these types of interventions to be outside the scope of this clinical guidance paper, given (i) these interventions are not usually delivered by or accessible to clinical neuropsychologists, and (ii) most of these interventions have little evidence supporting their impact beyond the impairment level — i.e. at the level of activity and/or participation (see the next point). If either the accessibility or evidence for these other types of interventions changes, they could be included in updates to this clinical guidance paper.
Throughout the paper, we will use the International Classification of Function (ICF; World Health Organization, 2013) as a framework within which neuropsychological interventions can be understood and evaluated. In describing disability, this model distinguishes between ‘body functions and structure’ (e.g. impairment on memory tests), ‘activity limitation’ (e.g. forgetting appointments), and ‘participation’ (e.g. not being able to work due to memory difficulties), as shown in Fig. 1. Outcome evaluation often targets the impairment level, by measuring the impact of the intervention on test performance. However, we contend that the outcomes of neuropsychological interventions should also be evaluated in broader terms, that is, regarding their impact at the levels of activity limitation and participation restrictions and overall quality of life. Fundamentally, the aim of neuropsychological interventions is to improve everyday functioning to make a meaningful difference to the life of the person with the brain condition. The level of the ICF model at which outcomes have been evaluated will therefore be noted throughout.
ICF model as applied to conditions affecting the brain, adapted from World Health Organization (2013)
Delivering Effective Neuropsychological Interventions: Key Principles
While the evidence base for neuropsychological interventions has developed largely separately in different clinical populations, there are several key principles or considerations for the effective delivery of interventions that apply broadly. In this section, we introduce these general principles, which relate to the (a) client, (b) clinician, and (c) intervention.
Client-Related Factors
Using a Biopsychosocial Case Formulation Framework
Neuropsychological interventions should be founded on a comprehensive biopsychosocial case formulation considering biological, psychological, and social factors (Wilson, 2002) as depicted in Fig. 2.
A comprehensive assessment of all these factors is therefore strongly recommended when planning a neuropsychological intervention, so the intervention can be tailored accordingly. For example, consider the following individuals, referred for intervention targeting their everyday memory difficulties:
-
John, a 39-year-old roof tiler, who had a severe traumatic brain injury (TBI) 6 months ago after falling from a ladder at work; has pre-existing sleep apnoea; lacks insight into his memory impairment; is apathetic with low levels of daily physical and mental activity; has low motivation to change; takes benzodiazepines more often than recommended; and whose wife works full-time while supporting their three young children and is very distressed;
-
Sarah, a 23-year-old medical student, recently diagnosed with multiple sclerosis; has everyday memory difficulties that appear to be closely related to her attentional abilities and fatigue; has a history of anxiety and perfectionism; is highly motivated to finish her medical degree; and lives at home with her parents who are of Indian background and are resistant to the idea of Sarah seeing a psychologist;
-
Brian, a 72-year-old farmer in a remote area, with possible early Alzheimer’s dementia; history of diabetes (with inconsistent medication adherence), cardiovascular disease, and depression; is the sole carer for his wife who has late-stage cancer; has been forgetting to feed the farm animals; is currently drinking at least four beers every night; distrusts doctors; has been told he should have a driving assessment and may lose his licence.
For each of these people, the content, timing, location, mode of delivery, sequence of intervention elements, and involvement of family in the memory intervention need tailoring according to their individual biopsychosocial formulation; as a one-size-fits-all approach is highly unlikely to be effective. For example, for John, behavioural and psychological interventions to address his apathy and motivational issues may need to be addressed prior to engaging him in memory rehabilitation strategies, while prioritising concurrent support for his wife (e.g. with a social worker). For Sarah, a focus on her study skills may enable engagement with a psychologist in the context of her family’s beliefs, and integrating fatigue and anxiety management strategies with memory interventions would be important. For Brian, establishing practical supports (e.g. through aged care services) to ensure the safety of his wife, farm animals, and other drivers would be of primary importance, along with memory and organisational strategies to ensure medication adherence.
Considering the Impact of Time Post-onset and Trajectory of Change
The nature of the neuropsychological intervention should also be tailored according to time since onset of the brain condition, and likely trajectory of the illness or injury. In the case of acquired brain injury (ABI), interventions in the first 6–12 months might focus on enhancing recovery and providing psychoeducation, with a later focus on managing and compensating for the residual effects of the ABI. In contrast, for mild cognitive impairment and dementia, in the early stages, interventions may focus on strategies used by the client themselves, whereas in later stages the interventions are likely to focus on family and environmental supports. For psychiatric disorders, interventions need to account for whether the mental illness is in an acute phase or remission and may also need to target issues such as risk of recurrence alongside improvement.
Clinician-Related Factors
Ensuring Clinicians Have the Appropriate Competencies
The clinician delivering the neuropsychological intervention should ensure they have the necessary competencies and resources to deliver the intervention effectively. This often involves additional training and/or supervised practice beyond that received in the context of university training programs. This topic is reviewed more comprehensively in ‘Section 2: Acquiring Competencies in Neuropsychological Interventions’.
Interdisciplinary Collaboration
Where possible, interdisciplinary approaches to management of individuals and families with brain conditions are recommended, throughout the continuum of care in hospital and community settings. This allows discipline-specific expertise to be integrated to work towards the client’s goals. Neuropsychological interventions are therefore often ideally delivered in an interdisciplinary or multidisciplinary context, together with other medical and allied health interventions and with the input of team members from other disciplines (Pagan et al., 2015) to determine priorities for targeted and timely intervention. For neuropsychologists working in private practice, there may be fewer opportunities to work within a multidisciplinary team. However, regular consultation and communication of treatment targets, plans, and progress to other health professionals involved in the person’s care (including the general practitioner or primary care physician) can be helpful in ensuring collaborative work towards common goals. Training that includes a multidisciplinary focus will provide team members with a necessary understanding of shared or complementary areas of practice in addition to more discipline-related expertise, assuring effective teamwork (Pagan et al., 2015).
Intervention-Related Factors
Intervention Targets Should Be Person-Centred and Goal-Directed
Neuropsychological interventions should adopt a collaborative goal-setting approach, where person-centred goal(s) are set and refined as a key part of the intervention and progress towards the goal(s) is actively monitored. Goals should be set by the client; however, clinicians often need to assist clients in ‘unpacking’ their goals to ensure that the goals are SMART (outlined in Fig. 3).
Inevitably, family members, caregivers, and other stakeholders (e.g. employers) may also wish to contribute to goal development. While it can be difficult to navigate these potentially differing perspectives, the clinician’s role is to prioritise person-centred care. This includes balancing the needs of the client and ensuring they have adequate opportunity and means to communicate their wishes and opinions, while respectfully and constructively considering input from relevant others (in accordance with the biopsychosocial framework, as above). It can be helpful to define the roles of the treatment team and explain the person-centred approach to all involved parties at the outset of the intervention.
Interventions Should Be Evidence-Based
Techniques and approaches with the strongest level of available evidence should be selected. Figure 4 shows the hierarchy of evidence that should be used to guide the choice of neuropsychological intervention.
In evaluating the evidence, clinicians should consider not just the strength and quality of the evidence for the overall efficacy of a particular intervention, but also:
-
Known predictors or moderators of intervention outcome, and how these apply to the client in question;
-
Whether or not the intervention outcome was clinically significant or meaningful, not just statistically significant; and
-
Whether the outcomes were measured at the levels of activity and participation as well as impairment, given the overall aim of optimising quality of life.
Tools such as NeuroBITE (https://neurorehab-evidence.com/web/cms/content/home) and CogTale (https://cogtale.org/) can be useful resources to help clinicians evaluate the available evidence for particular interventions. It is important that clinicians can justify their choice of neuropsychological intervention based on the available evidence, the patient’s goals and preferences, their biopsychosocial context, and the clinical setting. As stated by van Heugten (2017, p. 22), ‘planning treatment explicitly and evaluating the outcome should therefore be a self-evident process, either by monitoring the individual patient or applying the best available evidence in a careful and judicious manner’.
Optimising Frequency/Duration/Intensity
In planning the neuropsychological intervention, consideration should be given to the frequency and duration of intervention sessions, and the total duration of the intervention period. Decisions about these factors should be based on available evidence for the efficacy of the intervention techniques under consideration, as well as in relation to the client’s circumstances, client goals, and feasibility (e.g. availability of clinicians, funding, geographical location of client, resources required to implement the intervention).
Choosing the Appropriate Context/Location and Mode of Delivery
Neuropsychological interventions targeting a particular presenting problem (e.g. attentional difficulties, social anxiety) can be delivered in a range of contexts and modalities. These include home-based or centre-based locations, individual or group formats, computerised or clinician-facilitated programs, and telehealth or face-to-face delivery. Again, decisions about the context and mode of delivery of a neuropsychological intervention should be based on the available evidence for that intervention type, as well as the client’s circumstances, goals, and feasibility (e.g. availability of services, technological proficiency of client, geographical location of client).
Enhancing Generalisability and Maintenance
Key elements of the effectiveness of a neuropsychological intervention include its ability to generalise to daily life roles and activities that have not been directly targeted in the intervention; and for its effects to be sustained beyond the period of intervention. Ideally, neuropsychological interventions that have demonstrated evidence of both generalisability and maintenance should be selected, and in delivering the intervention, clinicians should also actively discuss with clients how best to apply or incorporate the intervention techniques into their daily lives, both during and beyond the intervention period. Clinicians and researchers should also include some evaluation of generalisability and maintenance as part of their outcome measurement.
Using Meaningful Outcome Measures
Both clinicians and researchers should select appropriate measures to evaluate the outcomes of neuropsychological interventions, which are meaningful and relevant to client goals, as well as reliable and valid. Even if the intervention targets an impairment (i.e. at the bodily functions and structures level of the WHO ICF framework), the outcomes of the intervention should also be measured at the levels of activity and participation. This means including measures that capture everyday activities and participation in life roles such as work and leisure. Measuring goal attainment, for example using Goal Attainment Scaling (GAS), is a clinically useful way to capture progress on personally meaningful outcomes. Using GAS in addition to validated questionnaires measuring relevant activity and participation outcomes can together capture the outomes that are most important to the person. Furthermore, measures of health-related quality of life and wellbeing (which are not incorporated particularly well within the ICF framework) are also important and capture unique and important outcomes that can influence policy-makers deciding where to allocate resources. For measuring health-related quality of life, clinicians and researchers should be clear in selecting and reporting the perspective(s) used – i.e. self or carer. These are complementary perspectives and provide valuable information when used concurrently (Bosboom et al., 2012; Burks et al., 2021). Efforts should also be made by researchers to use consistent outcome measures when evaluating neuropsychological interventions, particularly those that target the same presenting issue or clinical population. Lists of recommended outcome measures have been compiled for adult TBI (Honan et al., 2017), brain impairment generally (Tate, 2010), and in the older adult field (Simon et al., 2020).
Consideration of Costs and Benefits
Clinicians and researchers should also consider the cost-effectiveness of neuropsychological interventions. These interventions are generally delivered in resource-constrained settings, whether funded through the government (e.g. primary health networks), insurance agencies, or the client. Therefore, the best interventions are not always those that have the best efficacy, if the margin of improved efficacy is slim but the cost increase is large compared with the next most effective intervention. In other words, a good neuropsychological intervention should deliver ‘bang for your buck’. Appraisal of costs and benefits can be particularly challenging where there may be several ways to deliver an intervention (e.g. group vs individual; face-to-face vs. telehealth), or where decisions must be made to use resources to deliver fewer interventions to more clients or more interventions to fewer clients. Cost-effectiveness is re-visited in ‘Section 4: Implementation of Neuropsychological Interventions into Health Services’.
Section 2: Acquiring Competencies in Neuropsychological Interventions
Which Competencies Are Required for Effective Delivery of Neuropsychological Interventions and How Should Clinical Neuropsychologists Be Trained?
A key challenge for the clinical practice of evidence-based neuropsychological interventions is training clinicians to be competent to deliver them effectively. This is one of the primary barriers to more widespread clinical implementation of interventions, with many neuropsychologists not feeling confident or competent enough to incorporate neuropsychological interventions into their clinical roles, at least in Australia (Wong et al., 2014). In their review of the implementation of evidence-based psychological treatments, McHugh and Barlow (2010) argue that the greatest challenge to dissemination is training clinicians who can competently administer these therapies. As they highlight, successful training of clinicians in evidence-based psychological therapies requires a balance of both didactic training (i.e. knowledge transfer through written materials and workshops) and competence training (i.e. acquiring the skills needed for delivering the treatment effectively, usually through supervised practice). The importance of training competent clinicians was also highlighted by Powell et al. (2012), in their review of strategies for implementing clinical innovations in mental health.
There have been several attempts to develop lists of foundational knowledge- and skill-based competencies for neuropsychological interventions (Rey-Casserly et al., 2012; Smith & CNS, 2018), and very recently, training pathways and competencies for ‘neurorehabilitation psychology’ (Stucky et al., 2023). In one of the most recent and comprehensive of these efforts, a group of American organisations calling themselves the Clinical Neuropsychology Synarchy (Smith & CNS, 2018) outlined five knowledge-based and seven applied intervention competencies. These CNS intervention competencies were recently further expanded by the Australian Neuropsychology Alliance of Training and Practice Leaders (ANATPL; Wong et al., 2023a). They indicated that clinical neuropsychologists should have knowledge of:
-
Evidence-based intervention techniques and practices to address cognitive, emotional, and behavioural consequences of conditions affecting the brain, with consideration of both the quality of the evidence and whether there is evidence for meaningful impact on everyday activities, participation in life roles, and quality of life in the relevant clinical population.
-
Theoretical and procedural bases of intervention methods appropriate to address disorders of attention, processing speed, learning and memory, executive skills, problem solving, language, perceptual and visuospatial skills, social cognition, psychological/emotional adjustment, and behaviours of concern.
-
How complex neurobehavioural disorders (e.g. anosognosia, neuropsychiatric conditions) factors can affect the applicability of interventions.
-
Sociocultural considerations when planning and using interventions, referring on to other providers with specialised competence if appropriate, and/or seeking cultural consultation as required.
-
How to promote cognitive health with patients through activities such as physical exercise, cognitive stimulation, stress management, and healthy lifestyle (e.g. sleep, nutrition) practices.
-
Empirically supported interventions provided by other psychologists and other mental and behavioural health professionals.
In terms of applied competencies, they indicated that clinical neuropsychologists should be able to:
-
Identify targets of interventions and client goals and preferences.
-
Employ neuropsychological assessment and provision of feedback for therapeutic benefit.
-
Provide psychoeducation and information about neuropsychological disorders to aid the patient and family’s understanding of their presenting concerns and how to manage them.
-
Identify potential barriers to intervention and adapt interventions to minimise such barriers.
-
Develop a comprehensive biopsychosocial case formulation, including the cultural context, which usefully guides the intervention.
-
Develop and implement treatment plans for neuropsychological problems based on the case formulation and client goals.
-
Implement evidence-based cognitive interventions for neuropsychological disorders across the lifespan.
-
Deliver evidence-based psychological therapies (e.g. for depression, anxiety) appropriately adapted for people with neuropsychological impairment.
-
Provide behavioural interventions (e.g. positive behaviour support) for behaviours of concern in people with neuropsychological disorders.
-
Consider suitability and provide adequate training and support for use of technologies within neuropsychological interventions (e.g. assistive technologies, telehealth).
-
Independently evaluate the effectiveness of interventions employing appropriate outcome measures that are meaningful in everyday life, relevant to the patient’s goals, reliable and valid.
-
Demonstrate an awareness of ethical and legal ramifications of neuropsychological intervention strategies.
While these foundational competencies apply generally to neuropsychological interventions, they do not describe how these competencies should be measured or benchmarked for specific intervention types. Many neuropsychological interventions require a unique and specialised set of skills that require specific training. It is therefore crucial to identify (1) which key competencies are required for effective delivery of each intervention, and (2) which methods for training clinicians are effective in enabling them to acquire those competencies. However, at present there is a paucity of evidence available to answer these questions. While there is a growing body of research on competencies and training in psychological therapies such as cognitive behavioural therapy (CBT) and motivational interviewing (MI), this work cannot necessarily translate to psychological therapies that have been adapted for individuals with neuropsychological impairments, given the additional skills required for those adaptations to be successful. For example, Roth and Pilling (2007) published a useful framework describing the competencies required for effective CBT for depression and anxiety; however, it does not contain any competencies for adapting CBT techniques for people with impairments in domains of cognition that are important for deriving benefit from CBT, such as memory, cognitive flexibility, self-monitoring, and planning.
In terms of training, combined workshop training and ongoing supervision improved both community therapists’ skills and client outcomes in CBT for depression (Simons et al., 2010), and a similar combination of training methods resulted in the greatest gains in proficiency in clinicians learning MI (Miller et al., 2004). Again, however, treatment recipients in both studies did not have cognitive impairments associated with brain injury or illness. When modified for people with ABI, CBT, when delivered with booster sessions, has been found to be effective in reducing anxiety and depression symptoms over a six-month period (Ponsford et al., 2016). This manualised intervention has been published by ASSBI resources (Wong et al., 2019b). Recently, Wong et al. (2020) evaluated the impact of workshop training and three sessions of clinical supervision of delivery of this intervention on the competencies of a sample of primarily neuropsychologists. They found that a mix of didactic and competence training resulted in self-rated improvements in adapted CBT competencies, which were maintained over a 16-month period. This type of work has potential to reduce barriers to workplace practice of adapted CBT relating to clinician competence.
Further research has been conducted to identify competencies and training methods for other neuropsychological interventions, including development of a checklist of competencies required for group-based rehabilitation interventions (Wong et al., 2019a) and neuropsychological assessment feedback (Wong et al., 2023b). However, this body of research is at its early stages and much more work is needed to establish the evidence to guide the training of clinicians who are competent to deliver neuropsychological interventions. Nevertheless, the evidence so far consistently indicates that training in neuropsychological intervention skills should actively incorporate both didactic training (focused on knowledge acquisition) and competence training (focused on skill development); and that the competencies required sit at the crossroads of clinical neuropsychology and rehabilitation/intervention delivery (Stucky et al., 2023).
Current Training in Neuropsychological Interventions via Australian Clinical Neuropsychology Programs
At the time of writing and according to the Australian Psychology Accreditation Council (APAC) (www.psychologycouncil.org.au), training in clinical neuropsychology is offered by five accredited tertiary education providers across four states (New South Wales, Queensland, Victoria, and Western Australia). APAC provides accreditation standards for psychology programs (including Masters, PhD, Doctor of Psychology), which are approved by the Psychology Board of Australia (PsyBA), our national psychologist registration body. In the most recent iteration of the APAC guidelines (Australian Psychology Accreditation Council, 2019), which came into effect in January 2019, APAC is responsible for determining the accreditation of clinical neuropsychology training programs and have specified minimal content requirements for these programs. Intervention competencies for clinical neuropsychology programs (Section 4.1.3 of the APAC guidelines) comprise only:
-
Selection, tailoring, and implementation of psychological interventions appropriate for clients and their needs, including rehabilitation, behaviour management, monitoring, and remediation;
-
Consultation with and referral to other professionals regarding the neuropsychological implications of neurological and neuropsychiatric symptoms and disorders in a wider treatment context; and
-
Psychological interventions appropriate to the behavioural and cognitive dysfunctions associated with neuropathology.
Previously, clinical neuropsychology competencies and accreditation were determined and overseen by the Australian Psychological Society’s (APS) College Course Approval Guidelines for Postgraduate Specialist Courses drafted in late 2010 and published on the Psychology Board of Australia website in January 2011 (Australian Psychological Society, College of Clinical Neuropsychologists, 2011). These guidelines offer more detailed guidance regarding proficiency in neuropsychological interventions, specifying formal knowledge in theories of recovery (e.g. neural recovery and reorganisation; functional adaptation) as well as evidence-based models and techniques of neuropsychological intervention for neuropsychological disability. Section 4.2.d of the 2010 College Course Approval Guidelines includes::
-
Cognitive interventions for discrete cognitive impairments, such as visual neglect or memory disorder;
-
Cognitive behavioural approaches (e.g. anger management);
-
Psychotherapeutic approaches such as counselling;
-
A ‘lifespan perspective’ allowing for moderation of principles and techniques across stages of life;
-
Interdisciplinary teamwork and consultation; and
-
Evaluation of the implementation and outcomes of any intervention in order to determine its efficacy.
This is nevertheless a clearly shorter list than the more detailed competencies for neuropsychological interventions recommended by ANATPL (Wong et al., 2023a). These accreditation guidelines should therefore be considered a minimum baseline for intervention competencies for graduates. In addition, while the content and format of accredited clinical neuropsychology training programs must comply with accreditation guidelines, there is currently considerable variability between states and education providers in terms of their methods for supporting neuropsychological trainees in developing the practical skills to plan, deliver, and evaluate neuropsychological interventions in clinical and/or research practice. Thus, currently, a postgraduate qualification in clinical neuropsychology does not necessarily signify an equivalent level of competency in neuropsychological interventions across graduates. Clinicians must always be aware of their own boundaries in competent practice (as clearly stated in our standards of ethical professional conduct) and seek additional training and supervision in areas of practice in which they have not had the opportunity to acquire the relevant skills.
Key areas of variability in training programs between states include:
-
(i)
Proportion of course content devoted to intervention/rehabilitation, compared to diagnostic assessment and knowledge regarding various conditions affecting brain functioning;
-
(ii)
Coursework content and formal supervised practice or skill development in counselling and psychological therapies (e.g. cognitive behavioural therapy, acceptance and commitment therapy, motivational interviewing, mindfulness, relaxation techniques).
-
(iii)
Availability of clinical or research placements/internships where neuropsychological interventions are regularly implemented, in order to gain practical experience and develop skills in a supervised environment. Most placements tend to focus on developing and practising skills in diagnostic assessment, clinical formulation/interpretation, and communication of assessment outcomes, e.g. via reports and/or feedback.
-
(iv)
Incorporation of opportunities to conduct or co-facilitate interventions within university training clinics. Students report positive feedback on these experiences when they are offered, describing increased skills and confidence in delivering interventions and an increased interest in conducting interventions in future (Pike et al., 2020).
-
(v)
The inclusion of assessment tasks requiring students to demonstrate they can plan, implement, and evaluate neuropsychological interventions with real or simulated cases.
More consistent provision and evaluation of these training activities and models have the potential to enhance the breadth and depth of competencies in neuropsychological interventions among graduates of clinical neuropsychology training programs.
Ongoing training and upskilling beyond university training programs is necessary to ensure a skilled workforce, as reflected in the professional development requirements associated with psychology registration. Experienced clinicians may not have received comprehensive training or practice in delivering neuropsychological interventions and may have worked in settings where their role primarily involves assessment. Workshops, short courses, and clinical supervision may be beneficial for skill development and refinement in intervention skills and techniques throughout all career stages (Wong et al., 2021b, 2020).
While the structure of neuropsychology training differs around the world, these principles of ensuring neuropsychological intervention competencies, which have been clearly and comprehensively defined and are taught and assessed both during postgraduate training and beyond, apply internationally. Agreement on which competencies are essential for effective practice would facilitate international consistency in training and practice of neuropsychological interventions.
Section 3: Evidence Base and Clinical Utility of Neuropsychological Interventions in Adults and Older Adults
In this section, we summarise key evidence and considerations for neuropsychological interventions in three main cohorts: (i) acquired brain conditions including traumatic brain injury (TBI), stroke, and multiple sclerosis (MS); (ii) psychiatric disorders; and (iii) older adults including healthy older adults, mild cognitive impairment, and dementia. In the Appendices, we summarise the evidence based on existing systematic reviews and guidelines in separate tables (labelled with ‘a’ and ‘b’ throughout):
-
(a)
The interventions for each population for which there is sound evidence of impact at the level of activity/participation (for practical guidance on application of the WHO-ICF, see World Health Organization, 2013).
-
(b)
Interventions for which sound evidence of impact on activity/participation is still required (i.e. evidence is at the level of impairment only OR there is only limited evidence of impact on activity/participation).
The evidence presented in the tables in the Appendices represents meta-analytic-level evidence where available or otherwise the highest level of evidence possible. We note the evidence will continue to build and expand, and we encourage clinicians to use the framework presented in the tables (i.e. classifying according to whether evidence of impact is at the level of activity/participation) to guide their clinical decision-making into the future.
General Considerations
Across the three diagnostic cohorts, there is evidence that several types of neuropsychological interventions, particularly cognitive rehabilitation focused on personally meaningful goals and drawing on strategy-based training, can improve everyday function. There is limited support for functional or day-to-day benefits of computerised cognitive training as a standalone intervention when it is not combined with other (preferably personalised) support to apply strategies in everyday situations. Given that many computerised ‘brain training’ programs can require expensive subscriptions, clinicians should carefully seek high-level evidence of their efficacy and everyday impact before recommending them to clients. Brain training needs to be adaptive, intensive, and extensive for optimal restorative benefits. The SharpBrains checklist (Sharpbrains, n.d.) contains a good set of questions for consumers to ask themselves (or explore with their clinician) before embarking on a brain training program. Integrating health and lifestyle improvements (e.g. exercise, nutrition, and sleep) into neuropsychological interventions shows promise and clinical neuropsychologists are encouraged to incorporate evidence-based lifestyle recommendations in their feedback to clients. Group-based interventions also appear to have numerous benefits, including connection with others with similar lived experience. However, the ability to tailor interventions to individuals is a helpful advantage of those delivered one-on-one, and this is often necessary especially for people with complex needs.
There is some evidence that complex interventions that combine cognitive and psychological elements may be more effective in improving activity, participation and quality of life than treating impairments in isolation (Davies et al., 2023). The broader evidence for other combined or multicomponent interventions (e.g. combining behavioural with cognitive and/or psychological elements; combining restorative and compensatory cognitive training approaches; combining cognitive rehabilitation with physical or pharmacological interventions) is still developing and needs to be systematically evaluated across cohorts and intervention types. When considering whether to combine empirically supported intervention ‘modules’ into bespoke multicomponent interventions for individual clients, clinicians should consider not only the evidence for each component, but (i) also whether each component is justified by the case formulation, and (ii) the proposed underlying mechanism of action for each component, to ensure the combination of components has a solid rationale. The need for further research to help guide this kind of clinical decision-making is further detailed in the ‘Conclusions and Future Directions’ section.
Neuropsychological Assessment Feedback
Often overlooked as a form of neuropsychological intervention, neuropsychological assessment feedback to the patient and caregivers can be conceptualised as its own brief, therapeutic, psychoeducational, single-session intervention. We cover it briefly here as an intervention that applies equally to all three diagnostic cohorts. Models or frameworks for delivering feedback have been proposed, but not yet thoroughly evaluated (Gorske & Smith, 2009; Postal & Armstrong, 2013). Evidence supporting the benefits of neuropsychological feedback is currently based primarily on consumer satisfaction surveys (Gruters et al., 2021). In one of the most recent surveys, neuropsychological assessment feedback was found to be followed by improvements in the patients’ quality of life, knowledge about their condition, and ability to cope (Rosado et al., 2018). A prospective follow-up study (Lanca et al., 2020) subsequently replicated and extended these findings, adding reduced psychiatric and cognitive symptoms, and increased self-efficacy and confidence in achieving goals to the list of benefits following feedback.
These findings contrast with concerns that a proportion of patients in these survey studies reported negative outcome following feedback (Longley et al., 2022), and that providing diagnosis-focused feedback (e.g. confirming likely dementia) can be harmful to some patients if not delivered sensitively. Reassuringly, a recent RCT with cross-over, in MS, showed no adverse psychological effects one week after feedback, despite most patients receiving ‘bad news’, and significant improvements in mood, self-efficacy, and perceived everyday cognitive functioning 1 month later (Longley et al., 2022). The authors outlined a list of feedback components they thought might have been psychologically protective for those participants receiving the bad news. We are also aware of upcoming trials of neuropsychological assessment and feedback as an intervention in dementia/mild cognitive impairment (MCI) and stroke. Collecting evidence for the therapeutic impact of feedback, as well as the most effective model of delivery, is an urgent and important priority for our field. It is often the first part of the neuropsychological intervention process and can be critical for further engagement. With supporting evidence, it could arguably be a primary neuropsychological intervention that all clinical neuropsychologists should consider delivering as a matter of routine practice.
Common Neuropsychological Interventions
As many interventions have been trialled in all three of the populations discussed in this section, we have included a list of commonly used neuropsychological interventions that appear throughout the summaries and tables, briefly describing the nature and key features of each intervention. We note that this is not an exhaustive list of all existing neuropsychological interventions, and that the interventions listed here are not mutually exclusive. Where interventions have a high degree of overlap or have more than one label, we have indicated this in the table.
Adapted psychological therapies These aim to improve mental health and wellbeing in people with neuropsychological conditions and include adaptations to ensure therapy is suitable for people with cognitive impairment and/or neurological conditions | |
Acceptance and commitment therapy (ACT) — adapted for cognitive impairment | A psychological therapy that aims to change how an individual relates to distress and promotes engaging in behaviours consistent with the individual’s values. ACT components include the following: present moment awareness, acceptance, defusion, self-as-context, committed action, and values. Adaptations to ACT include reducing the more abstract components, and focusing on value-consistent behaviours |
Cognitive behaviour therapy (CBT) — adapted for brain injury (CBT-ABI) | A psychological therapy that aims to identify and change unhelpful patterns of thinking and behaviour that contribute to the presenting issues. CBT components include the following: cognitive restructuring, behavioural activation, relaxation techniques, structured problem solving, graded exposure, and relapse prevention. Adaptations include use of repetition, simplified explanations and handouts, scaffolded cognitive restructuring, and greater emphasis on behavioural components |
Compassion-focused therapy (CFT) — adapted for brain conditions | A psychological therapy promoting mental and emotional wellbeing by cultivating self-compassion. When applied to people with brain conditions, the focus of the self-compassion is on the impact of neuropsychological impairments |
Mindfulness-based cognitive therapy | Combines cognitive behavioural techniques and mindfulness strategies to regulate thoughts and emotions and reduce distress related to the brain condition |
Behavioural strategies These aim to support individuals and families with managing behaviours of concern related to their brain condition | |
Anger management training | The use of cognitive behavioural techniques targeted at anger management concerns |
Environmental modification | Aimed at reducing the impact of cognitive impairment or challenging behaviours by modifying the environment around a person to provide cognitive aids and/or remove potential triggers for challenging behaviour |
Positive behaviour support (PBS) | A client-centred holistic approach that teaches new skills to replace behaviours that are challenging and optimise quality of life. By identifying and changing the antecedents and consequences of behaviours of concern, a positive behaviour support plan is developed with a focus on developing new skills that enable the person to do things that are meaningful to them |
Social skills training | A form of behavioural therapy that covers a suite of interventions to improve social skills. Techniques include education and modelling appropriate behaviour, role play, corrective feedback, and positive reinforcement |
Cognitive strategies — compensatory These aim to minimise the impact of cognitive impairment on daily functioning through the use of aids or strategies to reduce cognitive load or perform affected tasks in a different way. Strategies include internal (mental) strategies, external aids (using tools in the environment), and systematic instructional approaches such as errorless learning. These are tailored to the cognitive strengths and weaknesses and personalised goals of the individual. Also can be termed ‘cognitive rehabilitation’ | |
Attention process training (APT) | A range of tasks designed to exercise specific types of attention (sustained, selective, alternating, divided), administered in a hierarchical fashion (i.e. become more demanding) |
Attention retraining | A range of exercises and compensatory strategies aimed at improving functional attentional abilities |
Chaining | Involves breaking a task or procedure down into discrete steps. Each step is trained using prompts (verbal, visual, modelling), with gradual fading of prompts as the client becomes independent. Each step can be used as a prompt for the next step, so that the behaviours are ‘chained’ together. Both forwards and backwards chaining can be used. Training of each step often draws on an ‘errorless learning’ approach (see below) |
Errorless learning | A method for systematically learning and remembering a novel task or skill. Tasks are broken down into small steps and the person receives immediate corrective feedback for each step to prevent them making a mistake (i.e. not trial and error learning). Helpful for those with intact procedural memory but impaired declarative memory |
Goal management training | Aims to improve a person’s ability to complete purposeful everyday activities, usually in the context of executive dysfunction. Teaches a sequence of steps to raise awareness of attentional lapses, identify any problems, develop alternative solutions, monitor implementation, and check for errors |
Group-based memory skills training | Group-based programs, usually of fixed length, that train use of internal and external memory strategies |
Gesture training | Developing non-verbal communication skills to enhance communication for people with speech difficulties |
Interpersonal process recall (IPR) | Aims to improve communication skills by using video playbacks of different social interactions between client and clinician. Clients are encouraged to provide self-feedback, in addition to the clinician’s feedback |
Mental imagery | An internal compensatory strategy aimed at improving spatial neglect by asking the person to imagine in detail moving their body on the neglected side or attending to visual information on the neglected side |
Metacognitive strategy training | Aims to improve performance of purposeful tasks through the use of various strategies to improve self-awareness, self-monitoring and self-correction of errors. Example strategies are self-talk, self-reflection and agendas to track progress |
Modified story memory technique (mSMT) | Aims to improve episodic memory through the use of context and imagery |
Music mnemonics | Aims to improve memory and recall by putting information to melodies |
Retrieval practice | Aims to improve learning and memory by deliberately recalling information and actively ‘bringing it to mind’ repeatedly, as opposed to passively re-reading or listening to the information |
Self-generation | Strategy to improve learning and memory in which people are given information with sections missing, and must generate answers themselves to fill the gaps (as opposed to being provided with all the information upfront) |
Spaced retrieval (SR) | Aims to improve recall of information by eliciting active recall of newly learned information over progressively longer intervals of time |
Strategy-based cognitive training (SCT) | Encourages the use of both internal techniques (e.g. visual imagery, categorisation, structured heuristics for problem-solving) and external techniques (e.g. calendars, environmental cues) to strengthen relevant cognitive functions and adapt to areas of weakness or decline by recruiting additional cognitive networks. SCT therefore involves active teaching, modelling and guidance in adaptive techniques by a facilitator. Many strategy-based approaches also incorporate psychoeducation regarding cognitive processes (e.g. encoding), which is often used to contextualise the strategies |
Time pressure management | Consists of a set of compensatory cognitive strategies, deployed using a systematic process, to allow for mental slowness during real-life tasks by either preventing or managing time pressure |
Video feedback | Direct corrective feedback may be used with people with impaired self-awareness. Approaches include involvement in contextualised occupationally-based activities, training to anticipate obstacles to optimise performance, verbal/audio-visual and experiential feedback, self-monitoring, and self-evaluation techniques |
Visual imagery | An internal compensatory strategy aimed at improving memory for specific information by visualising it in rich detail |
Visual scanning training | Encouraging people to actively pay attention (self-cue) to stimuli on a neglected side to improve visual scanning behaviour |
Cognitive strategies — restorative Aim to recover function in certain cognitive domains affected by brain injury by repetitive skill practice in the affected domain. Tasks are usually administered in a graded way, building on specific processes to become more complex | |
Cognitive remediation therapy (CRT) — includes computerised cognitive training (CCT) | Involves a broad range of learning-based interventions aimed at improving or restoring cognition broadly or in targeted domains. CRT typically involves repetitive drill-and-practice training exercises. CCT is the most common form of CRT, and involves specific computerised cognitive training programs aimed at improving particular aspects of cognition, commonly working memory. The software provides a structure in which to practice tasks, and is usually able to adapt task difficulty to suit ability. This can be paired with support from a clinician around strategies for improving task performance and how the training tasks and strategies are relevant and may be applied in daily life |
Dual task training | Aimed at improving impaired executive functioning by practicing performing two competing tasks at once. Tasks can be any combination of cognitive and/or motor in nature |
Eye patching | In the context of visual neglect, eye patching is used to encourage attention towards the neglected visual field by covering the intact visual field |
Gist reasoning | Gist reasoning is the ability to abstract and generalise meaning from complex information. Cognitive training based on this top-down reasoning approach (as opposed to ‘bottom-up’ rote learning) aims to improve long term learning and fact recall |
Mirror therapy | A body awareness intervention used in the rehabilitation of spatial neglect, focusing on proprioception and awareness of the body in space in relation to midline. A mirror is placed in the midsagittal plane to reflect the movements of one limb superimposed on the other limb |
Perceptual interventions (e.g. sensory stimulation) | Aims to recover perceptual deficits. For example, sensory stimulation aims to stimulate visual sensation, such as shape recognition tasks |
Strategic Memory Advanced Reasoning Training (SMART) | Aims to train functionally relevant complex reasoning abilities using a variety of control strategies (e.g. strategic attention learning to block out less relevant details) |
Other | |
Cognitive stimulation therapy | Promotes active cognitive stimulation and socialising, usually for people with mild to moderate dementia |
Feedback | The provision of neuropsychological assessment feedback after testing is completed, usually at an additional session with the patient and/or family members. Information covered usually includes the patient’s cognitive strengths and weaknesses, psychoeducation on the likely causes for their presenting concerns (including diagnostic/biopsychosocial formulation), and management recommendations |
Multimodal (or multicomponent) interventions | Interventions that draw on multiple components, often incorporating strategy-based CT, CCT, cognitive stimulation and psychoeducation; or combining cognitive, psychological and/or behavioural strategies. May also combine neuropsychological intervention with other forms of intervention, e.g. physical exercise, dietary supplementation, and medication |
Psychoeducation | Refers to active communication and exchange of information to improve understanding about psychological, cognitive and/or behavioural issues associated with a brain or mental health condition. Information about the nature and causes of symptoms and how to manage or treat them is typically included. Can be delivered in individual or group formats |
Social cognitive training | Includes a broad range of training exercises aimed at improving social cognition in everyday life. Social cognitive training typically involves engaging in therapist-facilitated exercises, and practice in applying the skills learnt to everyday social situations. These can include drill-and-practice exercises, strategy games, heuristic practice, mimicry, and role plays |
Virtual reality training (VR training) | The use of virtual reality technology to aid motor and cognitive rehabilitation, usually by simulating scenarios in which a person performs a daily task such as cooking in a kitchen or going to the supermarket |
The Evidence for Neuropsychological Interventions in Acquired Brain Injury and Illness
The following section summarises evidence for neuropsychological interventions in acquired brain injury and illness (ABI), with a particular focus on traumatic brain injury (TBI), stroke, and multiple sclerosis (MS). While the ABI umbrella includes a range of other diagnostic groups including brain tumour, hypoxic brain injury, encephalitis, and epilepsy, the available evidence on interventions with these groups is more limited. However, research in this field often includes mixed samples, and many of the same principles apply across the various ABI types.
In some reviews, MS is placed in a group with other progressive neurocognitive conditions, such as Parkinson’s disease, where the focus of interventions might be to preserve cognitive functioning or delay the functional impact of neurobiological changes (Sumowski, 2015). However, in the context of our focus on activity and participation outcomes in this clinical guidance paper, intervention research on MS fits more readily with other forms of ABI, for whom stage of life and personal goals tend to be similar (e.g. sustaining paid employment by learning to retain new work instructions, or contributing to parenting via improved concentration).
Much of the existing evidence on neuropsychological rehabilitation interventions has been collected with ABI cohorts, particularly TBI. There is a wide range of effective cognitive, psychological, and behavioural interventions in these groups, plus a large selection of emerging interventions. The literature points to the importance of person-centred, goal-directed, tailored interventions that are meaningfully embedded in the person’s life roles and valued activities.
Clinical neuropsychologists are central members of multidisciplinary teams that support clients in their rehabilitation post-TBI. However, the healthcare system supporting survivors of stroke has evolved differently, particularly given the lack of insurance systems funding rehabilitation prior to the onset of the NDIS. Australian audit data (Stroke Foundation, 2020) found that over 50% of stroke services reported no access to a neuropsychologist. This is despite the clinical guidelines for stroke management (Stroke Foundation, 2017) supporting the need for intervention across multiple cognitive, emotional, and behavioural domains. There is an urgent need for support for a greater neuropsychology workforce in stroke services, to optimise outcomes for survivors of stroke.
Likewise, the neuropsychology workforce supporting people living with MS is not centralised in specific MS services and instead tends to be mostly private practitioners. People with MS without sufficient personal funds cannot access these sorts of services. This is despite a number of recent, clinically-focused overviews of the state of the science in this area (Brochet, 2021; Chen et al., 2021; DeLuca et al., 2020) which have described the evidence supporting a wide range of neuropsychological interventions in MS. For instance, DeLuca and colleagues (2020) concluded that ‘… cognitive rehabilitation has shown consistent beneficial effects in patients with MS and currently represents the best approach for treating MS-related cognitive impairment’. Consequently, there is also a urgent need for support for greater access to neuropsychology workforce in MS services (Longley, 2022).
Key Considerations
-
The cognitive effects of TBI, stroke, and MS vary considerably from one individual to the next but may include impairments of attention and speed of information processing, memory, executive function, communication (including changes in social cognitive functions), and visuo-spatial function. Key principles that apply to addressing cognitive impairments in acquired conditions include the need to identify the individual’s pre-injury functioning and assessing the impact of problems in everyday contexts.
-
For conditions that fluctuate or deteriorate rather than recover or improve, such as MS, there are additional psychological challenges for both the person and their caregivers, such as learning to live with an unpredictable combination of symptoms over time and an uncertain future. Some may also have to find ways of coping with distressing transitions (e.g. moving from a relapsing-remitting phase of MS to a secondary progressive phase, or moving from being independently ambulant with a walking aid to needing to use a wheelchair to get around). It should be noted that psychological therapies for depression, anxiety, and adjustment in MS have not been reviewed in this clinical guidance paper, since neuropsychologists generally do not deliver these interventions in Australia. However, there is a moderate and accumulating evidence base supporting therapies such as cognitive behaviour therapy in people with MS to treat depression (Khan & Amatya, 2017), stress and distress (Taylor et al., 2020), and fatigue (Harrison et al., 2021).
-
Many TBI survivors are young and still in the process of establishing independence from parental support, studying or learning a vocation, and establishing important personal and social relationships. The inability to attain these important life goals can have devastating effects on their self-esteem and emotional state. Therefore, proactively addressing the cognitive, behavioural, social, and psychological barriers to attaining these goals is imperative. Their needs will change across the lifespan, so a long-term perspective is important.
-
Due to the older demographic of many stroke survivors, it is important to advocate for access to rehabilitation to address goals such as independent living, work, caring, and leisure-related life roles. Compared to people who sustain an ABI in early adulthood, many older stroke survivors have established work and life skills and other resources that can be drawn upon to support their engagement in interventions. However, survivors are at an increased risk of developing dementia, particularly vascular dementia, Alzheimer’s disease (AD), or mixed vascular/AD (Savva & Stephan, 2010). Thus, ongoing monitoring of cognitive functioning is recommended to ensure the most appropriate neuropsychological interventions are provided over time.
-
Multiple systematic reviews have highlighted a lack of high-quality studies investigating the efficacy of psychological therapies such as CBT in ABI (TBI/stroke) populations, which constrains the ability to provide firm recommendations (Fann et al., 2009; Gertler et al., 2015; Guillamondegui et al., 2011). Evidence for psychological therapies should be considered preliminary and clinicians are encouraged to monitor treatment progress to establish its efficacy in individuals (Gertler et al., 2015). In the absence of evidence for ABI specifically, psychological intervention is recommended if efficacy is demonstrated in the general population. However, psychological therapies such as CBT require modification for clients with ABI due to their cognitive impairments (Gallagher et al., 2019; Wong et al., 2019b).
-
There is limited research evidence regarding the efficacy of antecedent or traditional consequence-based behaviour modification approaches to addressing behaviours of concern following ABI (including TBI, stroke, and MS). There is growing clinician support for contextualised approaches that modify the antecedents to behaviour problems based on consideration of precipitating factors that maintain negative behaviour, relating to the person, their injury-related cognitive impairments, and the environment, as well as factors that facilitate positive behaviour. Such approaches aim to assist individuals to self-manage behaviour, promote positive lifestyle changes, and increase community functioning and positive family environments. Personally meaningful activities and identified valued outcomes provide a basis for re-engagement with post-acute life (Ylvisaker et al., 2003). Positive, well-rehearsed routines are encouraged, to promote structure in and engagement with daily living. Feedback and consequences must be context sensitive and meaningful, and behavioural supports positive and proactive (Ylvisaker et al., 2007). Importantly, existing family members, friends, and carers are included in the adoption and integration of management techniques, and feedback is provided in the individual’s own environment, to encourage community-based and integrated supports (Ylvisaker et al., 2007). The integration of goal setting and community and clinical supports is important to achieving gains. An RCT of positive behaviour support (PBS) has shown that this approach can be effective in reducing challenging behaviours, with gains maintained over at least eight months post-intervention, in increasing the self-efficacy of close others in managing these behaviours (Ponsford et al., 2022), as well as attaining meaningful individual goals (Gould et al., 2021). A clinic has now been established and training resources for clinicians are under development using a co-design approach (Gould et al., 2019).
-
For individuals with severe cognitive and behavioural difficulties following ABI, family members are an integral part of the support team. Recent evidence adopting a family-directed intervention approach shows promise in supporting the capability of family members to provide behaviour support (Fisher et al., 2021). The abovementioned recent RCT showed that a positive behaviour support intervention that actively involved close others including family (PBS-PLUS) resulted in a significant increase in their self-efficacy in managing challenging behaviours (Ponsford et al., 2022). However, much more research is needed.
-
ABI is more common in indigenous Australians than in non-indigenous Australians; however, there is limited research evaluating culturally appropriate rehabilitation, and the research is particularly sparse when it comes to neuropsychological interventions (Lakhani et al., 2017). This is an urgent area for future research.
-
The tables in this section have been separated into two Appendices, such that TBI, stroke, and other non-degenerative ABIs are included in Appendix 1 (Tables 1 and 2), and MS is included in Appendix 2 (Tables 3 and 4). This is because the MS literature is different in nature and scope, partly because MS is most commonly progressive, and much of the neuropsychological intervention research in MS has focused on specific techniques rather than the complex holistic interventions prominent in the TBI/stroke literature.
The evidence for the interventions presented in these tables is large and rapidly expanding. A number of systematic reviews and meta-analyses of RCTs or quasi-RCTs provide low-moderate evidence mostly at the impairment level (e.g. as measured by objective cognitive performance), but there is also growing evidence for positive activity, participation, and quality of life outcomes. There are numerous individual studies showing some benefits on these broader outcomes, but these findings may not yet have been replicated, so they have not been listed as providing sufficient evidence at the level of participation to warrant inclusion in Tables 1 and 2 (the literature on CBT for ABI is an example of this).
See Appendix 1 for a summary of the evidence in TBI, stroke and non-degenerative ABI (Tables 1 and 2). See Appendix 2 for a summary of the evidence in MS (Tables 3 and 4).
The Evidence for Neuropsychological Interventions in Psychiatric Disorders
Neuropsychological interventions are critical for addressing functional recovery in adult psychiatric disorders, as neuropsychological (including social cognitive) impairments are common and often marked in psychiatric disorders (Abramovitch et al., 2021; McIntyre et al., 2019; Mesholam-Gately et al., 2009; Miskowiak et al., 2018; Semkovska et al., 2019). Such impairments are often evident early in the course of illness, even prior to the onset of full-threshold disorder, and are therefore considered to be core features of severe mental illnesses such as schizophrenia (Keefe & Fenton, 2007). Cognitive impairments tend to be persistent, including during periods of remission of other symptoms, and are more strongly associated with poorer daily living, social, and vocational functioning than mental health symptoms (Cowman et al., 2021; Fett et al., 2011; Lee et al., 2018). Accordingly, addressing cognitive impairment, is explicitly recommended in the Australian clinical practice guidelines for schizophrenia, other psychotic, and mood disorders (Galletly et al., 2016; Malhi et al., 2021). As neuropsychological interventions occur in the context of other mental health treatments, their prioritisation depends on the broader goals and preferences of the individual. Another consideration is the extent to which neuropsychological deficits prevent individuals from fully participating in and engaging with such mental health treatments. At a minimum, the neuropsychologist can provide psychoeducation to the client and their treating team regarding the role that cognitive impairment plays in hindering recovery goals and provide suggestions as to how this could be addressed in line with the individual’s priorities and incorporated with other treatments. Neuropsychologists take into account developmental, biological, psychological, environmental, social, behavioural, and treatment-related factors (both current and premorbid/developmental) when understanding neuropsychological profiles and prioritising areas for intervention, including, but not limited to, neurologically based disturbances, neurocognitive and social cognitive impairments, and social and daily living impairments. Cognitive strengths that are identified can be harnessed for promoting functional recovery and may help to address the commonly experienced motivational issues (Allott et al., 2020). In this cohort, consideration of the potential adverse effects of medication on cognitive function is also important (Albert et al., 2019), and may be dose dependent (Kasper & Resinger, 2003; Takeuchi, 2015).
Key Considerations
-
The strongest evidence base for neuropsychological interventions is in schizophrenia and other psychotic disorders across the various clinical stages of illness (i.e. first episode through to non-remitting and chronic illness). These interventions are mostly grouped into computerised cognitive training (CCT) (Kambeitz-Ilankovic et al., 2019), cognitive remediation therapy (CRT) (Vita et al., 2021), or social cognition training (Nijman et al., 2020), but compensatory approaches are also well studied in psychotic disorders (Allott et al., 2020). There is emerging evidence for neuropsychological interventions in mood disorders (depression, bipolar disorder) (Bowie et al., 2013; Motter et al., 2016; Woolf et al., 2021) and eating disorders (particularly anorexia nervosa) (Tchanturia et al., 2014), given the growing recognition of cognitive impairments that impact on functional recovery in these conditions.
-
Neuropsychological interventions within psychiatric populations typically target cognitive deficits and processes, with the goal of improving daily and community functioning. Interventions are commonly delivered in groups but may also be provided individually. Most neuropsychological interventions involve psychoeducation about cognition and/or social cognition and its relationship to the psychiatric condition as well as with daily functioning. Some neuropsychological rehabilitation programs are provided adjunctively with other psychosocial treatment programs (e.g. CBT or supported employment). Some studies have explored family/caregiver involvement to assist with implementation/adherence to the intervention outside of the immediate therapy environment (e.g. Kidd et al., 2018; Kumar et al., 2019), and this seems to be an area worthy of further research. Lifestyle interventions, including physical exercise and nutrition, are gaining traction in randomised controlled trials in psychiatric conditions, with growing evidence of benefits to cognitive function, particularly as adjunctive interventions (Firth et al., 2017).
-
One issue that has impeded progress is that neuropsychological interventions have tended to be trialled in people with heterogeneous cognitive abilities and functioning in a ‘one-size-fits-all’ approach. There is growing recognition for the need to personalise neuropsychological interventions, with a large body of research examining predictors of treatment response, aiming to stratify or select participants based on particular characteristics (such as a particular degree of cognitive impairment and level of motivation). Recent reviews, however, have not been able to identify reliable predictors (i.e. demographic, biological, cognitive and functional, psychological, and illness-related characteristics) of response to cognitive remediation therapy in schizophrenia (Reser et al., 2019; Seccomandi et al., 2019), so the field still has some way to go to improve appropriate stratification of clients into cognitive rehabilitation trials.
-
Nevertheless, recent efforts aim to identify the core components of effective cognitive remediation therapy within specific diagnostic groups to better guide future research and clinical practice that is personalised, effective, and meaningful to clients. Bowie et al. (2020) recently proposed four core components of cognitive remediation in psychosis as part of an expert working group which were found in a meta-analysis to positively moderate outcomes (Vita et al., 2021). These core components include the following: (1) involvement of trained cognitive remediation therapists, (2) multiple repetitions of cognitive exercises, (3) opportunities for participants to identify, use and monitor cognitive strategies, and (4) procedures to support transfer of trained skills to real-world functioning. This conceptualisation emphasises the importance of formulating cognitive problems and their relationship with functioning, capitalising on intrinsic motivation in the learning process, and modifying task difficulty to optimise success and collaborative, realistic goal setting and tracking (Bowie et al., 2020). Similar therapeutic considerations have been recently suggested for major depression (Douglas et al., 2020).
-
For mood disorders, expert consensus statements focusing on cognition trial methodology have been proposed to guide the field in developing a strong evidence base for personalised neuropsychological interventions (Douglas et al., 2020; Miskowiak et al., 2017). Some of the key recommendations include the following: (1) ensuring adequate pre-screening to ascertain clients have cognitive impairment before enrolment; (2) enrolling clients when their mood is stable and relatively euthymic; (3) consideration of the effects of prescribed medication on the ability to benefit from the intervention and possibly optimise dosage (e.g. minimise use of benzodiazepines); (4) ensure outcome measures include co-primary or secondary measures of functioning (i.e. activity/participation), in addition to cognition; and (5) ensure participants receive an adequate dose (i.e. 10–20 weeks) of cognitive remediation therapy to maximise the intervention effects.
-
While some cognitive remediation programs have been translated into languages other than English (e.g. Spanish, Arabic), we are not aware of published work that has directly addressed cultural sensitivity and/or adaptation in psychiatry (e.g. for Aboriginal and Torres Strait Islander peoples, or other culturally diverse groups), which is unfortunate and an area ripe for research and implementation.
See Appendix 3 for a summary of the evidence in psychiatric disorders (Table 5).
The Evidence for Neuropsychological Interventions with Older Adults
There is an unfortunate tendency in the general community and among many health professionals, to underestimate or dismiss the utility of rehabilitation-focused interventions for cognitive decline in older adults. This is often due to misunderstandings including (a) that the underlying cause of all cognitive decline in older people is dementia, and (b) that therapeutic approaches in dementia are either unavailable, ineffective, or unrealistic given its progressive course (see discussion by Cations et al., 2018). However, clinical practice guidelines and current World Health Organisation recommendations for dementia care emphasise cognitive interventions among those rehabilitation approaches with the strongest evidence base (see Jeon et al., 2022; World Health Organisation, 2023), as there is sound evidence that neuropsychological interventions, particularly when individualised and goal-oriented, can improve everyday function in people with dementia. These interventions can maximise independence, delay the need for residential care, and result in important benefits for mood, quality of life, and meaningful participation in life roles such as grandparenting and community involvement.
Moreover, in those with MCI and even in older adults without objective cognitive impairment, there is sufficient evidence to support a recommendation from the World Health Organization (WHO) for the use of cognitive training to reduce the risk of cognitive decline and/or dementia (World Health Organization, 2019). In fact, these older adults with a higher risk of developing dementia are considered to represent an ideal population for early and selective prevention using cognitive interventions (Gates et al., 2014; Mowszowski et al., 2010; Pike & Kinsella, 2019), due to greater residual or compensatory cognitive resources, as well as greater insight. There is insufficient data to determine whether cognitive interventions have the capacity to prevent conversion to dementia (Butler et al., 2018), which at least partly relates to the methodological difficulties and expense in following participants for sufficiently long periods to gain these data (Huckans et al., 2013). Evidence in these groups indicates small improvements in cognition as well as some aspects of daily functioning following neuropsychological interventions. Given the small effects, tailoring an intervention to focus on individual goals is highly recommended. However, this does not mean that interventions should only be provided in a one-on-one format, as group interventions have several benefits, including peer support, opportunity for normalisation of experiences, and modelling.
A burgeoning area of clinical and research interest is the use of neuropsychological interventions for older adults without objective cognitive impairment, but who are concerned about a subjective decline in their cognition. There is mounting evidence that older adults with subjective cognitive decline have an increased risk for developing dementia and MCI (Mitchell et al., 2014; Pike et al., 2022). Furthermore, given that approximately 40% of dementia cases worldwide are attributable to potentially modifiable risk factors (Livingston et al., 2020), prevention of cognitive decline has become a particularly hot topic in recent years (Butler et al., 2018; Zokaei et al., 2017).
Indeed, a recent systematic overview of systematic reviews by Gavelin and colleagues (Gavelin et al., 2020) affirms the efficacy of cognition-oriented treatments across the continuum of cognitive presentations ageing. This rigorous review process synthesised quantitative findings for interventions spanning cognitive stimulation, training, and rehabilitation approaches across 46 previous systematic reviews and reported effect sizes of 0.3 to 0.4 for cognitive outcomes across healthy older adults, mild cognitive impairment, and dementia. While the systematic overview found that non-cognitive outcomes are unfortunately sparsely reported and recommended further research to more consistently evaluate clinical value across the field, we note that individual systematic reviews (e.g. Chandler et al., 2016) have reported effects on non-cognitive outcomes of clear clinical relevance (e.g. activities of daily living, mood, self-efficacy) and this is summarised in Appendices 4, 5, and 6.
It is also worth highlighting that among the dementia literature, few research studies have been conducted in non-AD or in young onset dementia (YOD). Considering that people with YOD are usually physically strong and healthy, often working at the time of diagnosis, may be supporting dependent children and/or ageing parents, and have significant financial obligations and commitments, the impact and burden of YOD can be great and often requires different types of support and services (Aplaon et al., 2017; Loi et al, 2023). There is some evidence that cognitive interventions improve functional outcomes and affective symptoms (Aplaon et al., 2017), but in general, the literature on YOD has limited methodological rigour (e.g. small sample sizes, few randomised controlled trials) (e.g. Fox et al., 2020) and thus is not included in our Appendices.
There is also evidence that health and lifestyle changes can positively impact cognition, with particularly strong evidence for the benefit of physical activity. Promising research is underway using technology to support memory in dementia, and we wait with anticipation for results of ongoing trials.
Key Considerations
-
From a biopsychosocial perspective, significant issues frequently arise in this phase of life and may contribute to, or exacerbate, cognitive and/or day-to-day functioning. These include retirement, bereavement, adjustment and role change, mental health (e.g. depression, anxiety, loneliness), general health (e.g. chronic pain, diabetes), polypharmacy, sensory status (i.e. hearing, vision), and environmental context (e.g. independent living, residential care, or assisted living). It is critical to consider the impact of these concurrent factors on intervention planning and outcomes, as well as considering whether other, multidisciplinary approaches may assist in addressing these factors
-
Psychological interventions play a key role in managing many of the highlighted factors, with important flow-on effects for cognition. Despite this, there is limited research on the cognitive effects of these interventions in older people, and psychological interventions are often delivered separately to neuropsychological interventions in this cohort. We propose that a more integrated approach to these intervention types may be optimal and may provide synergistic benefits and look forward to further research in this area (see the ‘Conclusions and Future Directions’ section).
-
Family or other informal caregivers can play an integral role and should be involved and supported in the intervention process (Clare, 2017), but this must be balanced with upholding a person-centred approach. For example, avoiding (inadvertent or intentional) caregiver direction of intervention goals or selective adherence to intervention techniques. This balance can be facilitated by framing the caregiver as a ‘care partner’ in delivering the intervention and providing structured support and education regarding their role throughout (see, for example, the I-HARP trial; Jeon et al., 2019). Furthermore, caregivers of people with dementia often experience their own significant psychological, social, and financial impact. Here, neuropsychological interventions can address caregiver wellbeing including symptoms of depression and anxiety, as well as their ability to provide care, by providing psychoeducation to enhance understanding of changed cognition/behaviour and training in problem-solving, coping strategies, and behavioural management approaches (Bayly et al., 2021; Gilhooly et al., 2016).
-
Older Aboriginal and Torres Strait Islander peoples have a higher prevalence of dementia, which has been linked with a variety of biomedical and sociocultural factors (e.g. male sex, childhood adversity and trauma, unskilled work, current smoking, head injury, and other chronic conditions) (see Li et al., 2014; Radford et al., 2015). Despite this, no research on neuropsychological interventions in this group has been published, and this is an important gap. Future research is critically needed and must incorporate collaborative work with Aboriginal and Torres Strait Islanders, such as a ‘collaborative yarning group’ (e.g. Lavrencic et al., 2021) study to help ensure feasible and culturally safe interventions.
-
Many older people experience subtle cognitive changes as part of the normal ageing process. Some, however, experience more significant cognitive impairment relating to a variety of aetiological factors. Where neurodegenerative disease is a primary cause, cognitive impairments may be progressive, change in nature over time, and involve reduced awareness or insight. This does not mean that effective and meaningful therapeutic intervention is not warranted or cannot be achieved; rather, it again highlights the need for a considered and tailored approach to designing and implementing interventions for specific subgroups and individuals. Thus, we will consider separately (a) neurodegenerative diseases, with a focus on AD (as this is where most of the literature lies), (b) mild cognitive impairment (MCI), and (c) healthy ageing, including subjective cognitive decline.
-
While most research in neurodegenerative disease is focused on AD, benefits of neuropsychological interventions in other less common types of dementia are emerging. Overall, an individualised approach is recommended to account for distinct symptom profiles (e.g. environmental, behavioural, and physical strategies for people with behavioural variant frontotemporal dementia and communication strategies for people with language variant frontotemporal dementia; see key resources for FTD at http://ecdc.org.au/ftd-toolkit.htm), and emotion recognition training in people with Huntington’s disease (see Kempnich et al., 2017).
-
Notably, people with MCI may experience only subtle or minimal functional change due to cognition, while healthy older adults have no objective cognitive impairment or functional change due to cognitive impairment. As such, most studies in these subgroups focus solely or heavily on objective improvement in cognition (i.e. level of impairment) as a critical outcome, rather than measures reflecting activity or participation. In keeping with the overall approach of this clinical guidance paper, we have separately summarised the relevant literature with respect to effects at the levels of participation and activity (Tables 6 and 8) and impairment (Tables 7 and 9) for dementia and for MCI (Appendices 4 and 5, respectively). For healthy older adults, it should be noted that improvement in cognition, even in persons without cognitive impairment, is an important outcome that should not be dismissed (Table 10).
See Appendix 4 for a summary of the evidence in dementia (Tables 6 and 7).
See Appendix 5 for a summary of the evidence in MCI (Tables 8 and 9).
See Appendix 6 for a summary of the evidence in healthy older adults (Table 10).
Section 4: Implementation of Neuropsychological Interventions into Health Services
The translation of research evidence on neuropsychological interventions (as reviewed in ‘Section 3: Evidence Base and Clinical Utility of Neuropsychological Interventions in Adults and Older Adults’) into widespread clinical practice is crucial to ensure improved outcomes can be achieved for individuals with brain conditions as part of their usual health care. The gulf between evidence and practice continues to be wide in many areas of health care (Bayley et al., 2012; Rogers, 2003), and it is incumbent upon clinicians, researchers, and health service managers to identify and apply methods for closing this gap to ensure consumers benefit from investment in research (Davis et al., 2003; Graham et al., 2006; Greenhalgh et al., 2004). This is a significant challenge for this field, given the traditional focus of the neuropsychologist’s role on assessment and diagnosis in Australia, which means that health services often do not have staffing and resources dedicated for clinical neuropsychologists to deliver interventions. For example, a recent national survey of memory clinics by the Australian Dementia Network (Naismith et al., 2022) indicated the limited provision of neuropsychological interventions even within these dedicated settings. Of the 55 memory clinics identified, only 20% provided memory strategy training; just two clinics (i.e. 3.6%) provided telehealth memory rehabilitation, and one (i.e. 1.8%) provided computerised cognitive training. Only 14.5% provided more than one session of a neuropsychological intervention, and even these were often limited to just two sessions. Group-based programs focused on cognition and wellbeing were provided by 12.7%. This is despite 74.4% of memory clinic respondents identifying neuropsychological intervention as a key ingredient of adequate post-diagnostic care.
Despite this appetite for additional intervention services, any staffing increases in resource-constrained health services require strong advocacy and evidence that the additional service provision will address a significant unmet need and potentially reduce future downstream costs. Collaboration with health economists can be extremely useful in providing an analysis of the cost-effectiveness of a new intervention, which is often crucial evidence for inclusion in a business case. Additionally, the involvement of and advocacy from consumers, particularly in highlighting the need for and benefit of the intervention, is important to health service managers whose job is to meet the needs of their consumers.
In the current climate of increasing pressure on healthcare resources, a key challenge is to demonstrate to funding agencies, healthcare services, and clients that neuropsychological interventions are not only effective, but also represent value for money (Prigatano & Morrone-Strupinsky, 2010; Stolwyk et al., 2021; Worthington et al., 2017). Health economic analyses include cost–benefit analysis (measuring the outcomes of an intervention in monetary terms such as productivity), cost-effectiveness analysis (measuring outcomes in terms of natural or health units such as days off work or health appointments), and cost-utility analysis (measuring outcomes in terms of quality-adjusted life years). Worthington et al. (2017) and Stolwyk et al. (2021) are helpful sources of further information about these concepts. These analyses can be used to demonstrate both the costs and benefits of various interventions which can inform clinical practice, service implementation, and the business case for rehabilitation programs or interventions. For example, van Heugten and colleagues (2011) reported cost savings from a societal perspective associated with participation in a community reintegration program following acquired brain injury. Using these data, the authors could argue that the cost of the program would be recouped after 8 years and therefore health insurance companies ought to reimburse these costs in view of the potential for long term savings with individuals having an average of 35 years to live before being eligible for pension support. In another example, Radford and colleagues (2013) demonstrated that individuals with traumatic brain injury were more likely to return to work following a vocational rehabilitation group, at a marginally increased cost compared to usual care. However, once the societal costs (e.g. loss of wages, expenses, employer costs) were considered, the vocational intervention was more cost-effective with it costing £12,418.20 (more than AUD 22,000) less to return a person to work with the intervention than usual care. These studies illustrate how clinical neuropsychologists and research teams can collaborate with health economists to justify the implementation of neuropsychological interventions within clinical rehabilitation practice.
Several theoretical frameworks are available to guide clinical translation and implementation efforts, including the Knowledge to Action Framework (Graham et al., 2006), the Consolidated Framework for Implementation Research (Damschroder et al., 2009), and the RE-AIM Framework (Glasgow et al., 1999). Common features of these frameworks include (i) identifying barriers and enablers, (ii) selecting intervention components and adapting them for the local context, and (iii) systematically monitoring the outcomes of implementation. Based on a review of strategies for implementing health innovations (Powell et al., 2012) and evidence from specific evaluations of neuropsychological intervention implementations (Kinsella et al., 2020; Wong et al., 2021b), the following key strategies for clinical implementation initiatives are recommended in Box 1.
Box 1 Key strategies for clinical implementation of neuropsychological interventions
Plan and build engagement (Allow plenty of time for this) | Discuss the goals of the organisation in implementing the new service — build ‘buy-in’ Develop the relationships necessary for successful implementation Engage service users/consumers as essential stakeholders Help stakeholders gather data Identify the organisation service delivery team and available staffing resources, and initiate leadership Restructure existing professional roles if necessary Identify a Change Champion in the organisation for leadership in delivery of the intervention |
Educate stakeholders | Inform all relevant stakeholders about the innovation |
Tailor the intervention to the setting | Determine the core components in the intervention that cannot be altered, and communicate these clearly to clinicians Be prepared to be flexible in responding to feedback from clinicians Adapt and adjust the non-core elements of the intervention |
Establish a training approach that maintains intervention fidelity | Fit the training model to the capabilities and resources of the service Decide on strategies to maintain fidelity of the intervention (e.g. provide a detailed manual; provide opportunities for new clinicians to observe the intervention live or via video; provide supervision during initial stages of the roll-out) — this should encompass both adherence (to the intervention content) and competence (in its delivery) |
Secure finance | Seek relevant funds/grants to finance the implementation Leverage existing funds to incentivise the use of clinical innovations and provide resources for training and ongoing support |
Evaluate the implementation to ensure quality management | Agree on measurable intervention goals, and the available resources for evaluation Identify/develop outcome measures that are sustainable and appropriate to the organisation Evaluate outcomes for clients, clinicians, and the organisation Pilot, trial, and regularly review |
Examine sustainability | Use the results of the outcome evaluation to identify costs and benefits Develop a plan for sustainability, including managing attrition of trained clinicians Encourage promotion of the innovation through hospital networks, foundations, events and media Proactively disseminate knowledge about the program to policy-makers to seek new funding arrangements |
These strategies were effectively utilised in several recent Australian examples in which new neuropsychological interventions were introduced into public health services. In the MemoRI project (Wong et al., 2021b), a memory skills group program was implemented at two health services in which clinical neuropsychologists were trained and supervised in group facilitation. Subsequently, in collaboration with health economists, the cost-effectiveness of the new pathway of care was evaluated along with participant outcomes. The memory group was found to be clinically effective and more cost effective than standard care, and consumers and referrers provided strong feedback in support of the program. This information was used to support a business case for staffing increases/restructure at the two health services. That project was then replicated at several other health services in Victoria. In a separate initiative, Stolwyk and colleagues (in preparation) demonstrated the successful development and implementation of a pilot teleneuropsychology stroke rehabilitation (TNSR) service, delivered to a rural stroke rehabilitation unit from a metropolitan hub. Implementation of TNSR resulted in improved clinician competence and service quality in the provision of assessment and treatment for mood and cognitive dysfunction, with positive experience of the service reported from both patients and clinicians. Economic simulations demonstrated TNSR could be delivered more cost-effectively compared to an equivalent in-person service. This evidence was incorporated into a business case which supported ongoing funding for the service in addition to planned scale-up to multiple rural hospital sites.
Similar work is currently underway at St Vincent’s Hospital in Sydney and demonstrates the lengthy and complex process that often contributes to the evidence-to-practice lag. Commencing in 2017, an evidence-based cognitive training and psychoeducation program (see Diamond et al., 2015) was implemented within this metropolitan public health service for older outpatients with late-life depression. An initial pilot feasibility study was undertaken to iteratively adapt the intervention to suit the priorities and needs of patients and staff within the setting, including staff training and acquiring resources for the intervention. Having shown that the pilot implementation was feasible, well-tolerated, and highly acceptable to both patients and staff (referrers from within the service, clinicians trained to facilitate the intervention, administrative staff) (Woolf et al., under review), in accordance with implementation science methodology, a full-scale feasibility randomised controlled trial is now underway to produce additional feasibility outcomes and data regarding efficacy and health/cost analyses, with preliminary data indicating considerable cost savings for the 10-week neuropsychological intervention (estimated at AUD 600 per patient) compared to traditional CBT programs (costed at AUD 2000 per patient) for this cohort (Woolf et al., under review). Thus, even where clinical benefit, acceptability and potential economic savings are immediately apparent, the process of implementation requires extensive and often resource-intensive commitment to demonstrating sustainable embedment within the service.
In a different kind of implementation initiative, Kinsella and colleagues (2020) worked with a consumer-advocate organisation (Dementia Australia) to support their staff to deliver a memory group intervention to their client group. In that instance, neuropsychologists provided specialist leadership, training, and consultation to support the implementation. This allowed much wider access to the neuropsychological intervention than would have been possible if neuropsychologists were directly funded to conduct the intervention. This example highlights the general issue of limited availability of specialist neuropsychology services, which in Australia tend to be concentrated within metropolitan areas, thus critically reducing the ‘reach’ (see Peters et al., 2013a, b) of both diagnostic and intervention services especially for geographically, socially, or financially isolated individuals. While the COVID-19 pandemic and associated public health restrictions have undoubtedly broadened the use of telehealth for remote delivery of clinical services and this is likely to be helpful for expanding access, not all neuropsychological interventions are amenable to remote or digital delivery.
These examples demonstrate that it is possible to enhance clinical implementation of evidence-based neuropsychological interventions into health services if clinicians, researchers, health service managers, and consumers work together towards the common goal of improving access to these interventions. It is important to recognise, however, that few clinical neuropsychologists have training or experience in service implementation. To achieve progress in this field, neuropsychologists are likely to require training, mentoring, and collaboration with experts in service implementation, project management, and change management. This is greatly enhanced when formal organisations provide a cohesive and structured pathway for collaboration. For example, in the older adult cohort, the federally-funded Australian Dementia Network’s core ‘Memory Clinic Initiative’ has a key goal to enhance and harmonise post-diagnostic support for older people with cognitive impairment in memory clinic settings across Australia, with a dedicated sub-group currently working to provide targeted professional development and training, peer support, and representation of patient and health professional (including neuropsychologists’) needs at the policy level. For more information on access to resources and opportunities to become involved, see: https://www.australiandementianetwork.org.au/.
In addition to several common implementation framework examples referenced above and key strategies provided in Box 1, additional guides covering key principles and practical examples are also provided in the ‘Resources’ section.
Conclusions and Future Directions
Figure 5 summarises the key considerations and recommendations put forward in this clinical guidance paper.
As a profession, we now need to progress in several important future directions.
Building a Clinically Meaningful Evidence Base
There have been major and exciting developments in our understanding and application of neuropsychological interventions. However, there also remain key gaps in our knowledge and skill base, and there are several clear directions that would take us forward.
Firstly, more level 1 evidence is needed for many neuropsychological interventions. In particular, consistent inclusion of measures of activity and participation outcomes is crucial. The continued reliance on measures of objective cognitive impairment as primary outcomes has hampered ongoing development in the field and limited the impact of research on the everyday lives of people affected by brain conditions. The development of core outcome sets to allow better comparison of the everyday impact of various interventions would help progress towards this aim, such as those developed for TBI (Honan et al., 2017). Additionally, the development of rigorous trial designs that better reflect clinical practice (e.g. allocating participants to groups based on their biopsychosocial formulation and goals and randomising within those groups, rather than randomly allocating participants to treatments for which they are not suited) in combination with high-quality single case experimental designs will be important as we move towards an era of ‘precision rehabilitation’. Greater collaboration across the world will undoubtedly be necessary to achieve this, given the challenges with recruiting large samples for clinical trials with cohorts with neuropsychological conditions. Ultimately, a greater focus on designing research that is both methodologically sound and clinically relevant will facilitate smoother and more rapid translation to clinical practice.
Furthermore, evaluation of holistic interventions that combine cognitive, psychological, and behavioural elements (again, aligning more closely with clinical practice) is urgently needed. Related to this, the move towards evaluation of transdiagnostic, process-based psychological interventions would also help take the field beyond ‘siloed’ diagnosis-specific clinical trials. Integrated, multidisciplinary, transdiagnostic interventions enable a greater focus on clients’ goals, values, and preferences and provide opportunities for collaborative care and management of difficulties from multiple perspectives; however, rigorous research of such multifaceted interventions is often seen as costly (time, resources, training, collaboration) and may be vulnerable to criticism around an inability to define the ‘active ingredient’. Nonetheless, the benefits of such integrated care programs are currently being explored in both the ABI and dementia space. In ABI, holistic interventions that combine cognitive, emotional, and behavioural components are increasingly being evaluated, with promising results (e.g. Sathananthan et al., 2021). In dementia, a variety of neuropsychological interventions are being incorporated to add value to broader programs of person-centred, goal-oriented care, often sitting alongside complementary and well-established approaches including reablement, function-focused (a.k.a. restorative) care, and occupational therapist-led interventions (see Jeon et al., 2022). An example within the Australian context is the Interdisciplinary Home-based Reablement Program (I-HARP) currently under evaluation across five hospital and community-based sites within NSW (Jeon et al., 2019). This program uniquely recognises the key contribution of evidence-based neuropsychological techniques such as errorless learning and compensatory strategy training towards functional outcomes, within and alongside the more traditional home-based occupational therapy and nursing services which have previously been emphasised in other multidisciplinary programs, e.g. COPE (Clemson et al., 2018).
Finally, there is an unacceptable dearth of evidence for, and access to, culturally safe neuropsychological interventions for people from culturally and linguistically diverse backgrounds. This is particularly the case for indigenous Australians. Clinicians and researchers must act to address this gap as a matter of urgent priority.
Embracing Telehealth and Other Technologies
In our current COVID-affected world and beyond, the use of telehealth and other technologies such as smartphones, virtual reality, and wearable devices for intervention delivery has become more important than ever. Therefore, another priority for future research and practice is to grow the evidence base and clinical translation of technology-enabled neuropsychological interventions. Neuropsychological interventions that have been trialled successfully so far using telehealth delivery (that is clinician-facilitated, rather than fully online or self-guided) include cognitive (usually memory) rehabilitation following stroke (Lawson et al., 2020), TBI (Bergquist et al., 2009; Bourgeois et al., 2007), and mild cognitive impairment and dementia (Cotelli et al., 2019); psychological therapies for depression, psychological distress, posttraumatic symptoms, sleep quality, and fatigue in TBI cohorts (Ownsworth et al., 2018); psychosocial interventions for depression post-stroke (Laver et al., 2020); interventions for challenging behaviours following TBI (McDonald et al., 2019); improving emotional wellbeing and cognitive function in brain tumour survivors (Ozier et al., 2019); support for caregivers of individuals with TBI (Powell et al., 2016) and dementia (Williams et al., 2018); and group treatment for emotional regulation post-TBI (Tsaousides et al., 2014). We are aware of numerous trials currently underway to expand this evidence base. Given these interventions often require the development of new clinical competencies, training clinicians in telehealth delivery will be essential for widespread access. Detailed teleneuropsychology guidelines are now available to guide telehealth delivery of neuropsychological interventions (Stolwyk et al., 2022).
Weaving Interventions into Our Core Skill Base and Professional Identity
This clinical guidance paper arose from a need to clearly characterise a practical, evidence-based approach to the delivery of adult and older adult neuropsychological interventions in Australia, on the background of a professional history steeped in the tradition of assessment. To effectively transform our professional identity and clinical impact such that interventions are seen by both ourselves and others as central to our profession, it will be crucial to ensure that comprehensive, effective, skill-based training that incorporates opportunities for observational and experiential learning is widely available — and not only to students and registrars, but also to the senior clinicians who may not have received adequate (or any) training previously. We encourage all clinical neuropsychologists to consider engaging in opportunities to continually expand and/or update their skills in intervention delivery, which has the potential to improve their practice and outcomes across all types of clinical settings. Currently, there are limited such opportunities available (Wong et al., 2021a), and so, creating more is also a pressing need.
Call to Action
We urge clinicians, researchers, and educators reading this clinical guidance paper to ask themselves what they can do in response to the issues and recommendations raised, to help move the field forward so that neuropsychological interventions can be considered ‘core business’ for clinical neuropsychologists.
We would encourage you to consider the following actions:
-
1.
Understand and apply the key principles of neuropsychological intervention delivery to maximise your effectiveness.
-
2.
Familiarise yourself with the evidence — and collect your own (on an individual client level and/or group level if possible).
-
3.
Fill competency gaps with professional development including workshops, short courses, and supervision — and by implementing new skills in clinical practice.
-
4.
Generate neuropsychological assessment recommendations that include feasible, evidence-based interventions and ensure these are implemented wherever possible.
-
5.
Advocate up the line:
-
(a)
For resources and funding to support staff who can deliver interventions in your work setting — talk to managers, submit business cases, and ask people with lived experience to let health services know that they want to access neuropsychological intervention services and how they feel this would add value to the overall service they receive.
-
(b)
By reporting the outcomes and ‘telling the story’ of your interventions to team members, referrers, managers, and policy-makers.
-
(c)
By encouraging students to incorporate intervention delivery into their clinical practicum activities.
-
(a)
Resources
Existing Cochrane Reviews and Other High-Quality Meta-analyses on Neuropsychological Interventions
-
Allida, S., Cox, K. L., Hsieh, C. F., Lang, H., House, A., & Hackett, M. L. (2020). Pharmacological, psychological, and non-invasive brain stimulation interventions for treating depression after stroke. Cochrane Database of Systematic Reviews, 1(1), CD003437. https://doi.org/10.1002/14651858.CD003437.pub4
-
Allott, K., van-der-EL, K., Bryce, S., Parrish, E. M., McGurk, S. R., Hetrick, S., . . . Velligan, D. (2020). Compensatory interventions for cognitive impairments in psychosis: A systematic review and meta-analysis. Schizophrenia Bulletin, 46, 869-883. https://doi.org/10.1093/schbul/sbz134
-
Amatya, B., Khan, F., & Galea, M. (2019). Rehabilitation for people with multiple sclerosis: An overview of Cochrane reviews. Cochrane Database of Systematic Reviews 1(1), CD012732. https://doi.org/10.1002/14651858.CD012732.pub2
-
Bahar-Fuchs, A., Martyr, A., Goh, A.M., Sabates, J. & Clare, L. (2019). Cognitive training for people with mild to moderate dementia. Cochrane Database of Systematic Reviews, (3):CD013069. https://doi.org/10.1002/14651858.CD013069.pub2
-
Baker C., Worrall L, Rose M, Hudson K, Ryan B, O’Byrne L. A systematic review of rehabilitation interventions to prevent and treat depression in post-stroke aphasia. Disability and Rehabilitation. 2018;40(16):1870-1892.
-
Beedham W, Belli A, Ingaralingam S, Haque S, Upthegrove R. The management of depression following traumatic brain injury: A systematic review with meta-analysis. Brain injury. 2020;34(10):1287-1304.
-
Chandler, M.J., Parks, A.C., Marsiske, M., Rotblatt, L.J., & Smith, G.E. (2016). Everyday impact of cognitive interventions in mild cognitive impairment: A systematic review and meta-analysis. Neuropsychology Review, 26(3), 225–251. https://doi.org/10.1007/s11065-016-9330-4
-
Chun H-YY, Newman R, Whiteley WN, Dennis M, Mead GE, Carson AJ. A systematic review of anxiety interventions in stroke and acquired brain injury: Efficacy and trial design. Journal of Psychosomatic Research. 2018;104:65-75.
-
das Nair, R., Cogger, H., Worthington, E., & Lincoln, N. B. (2016). Cognitive rehabilitation for memory deficits after stroke. Cochrane Database of Systematic Reviews, (9).
-
Ford ME, Groet E, Daams JG, Geurtsen GJ, Van Bennekom CAM, Van Someren EJW. Non-pharmacological treatment for insomnia following acquired brain injury: A systematic review. Sleep Medicine Reviews. 2020;50:101255.
-
Gavelin, H.M., Lampit, A., Hallock, H., Sabatés, J. & Bahar-Fuchs, A. (2020). Cognition-oriented treatments for older adults: A systematic overview of systematic reviews. Neuropsychology Review, 30(2), 167–193. https://doi.org/10.1007/s11065-020-09434-8
-
Gertler, P., Tate, R. L., & Cameron, I. D. (2015). Non-pharmacological interventions for depression in adults and children with traumatic brain injury. Cochrane Database Syst Rev(12), Cd009871. https://doi.org/10.1002/14651858.CD009871.pub2
-
Goverover, Y., Chiaravalloti, N. D., O’Brien, A., & DeLuca, J. (2018). Evidenced based cognitive rehabilitation for persons with multiple sclerosis: An updated review of the literature from 2007-2016. Archives of physical medicine and rehabilitation, 99, 390-407.
-
Gromisch, E. S., Fiszdon, J. M., & Kurtz, M. M. (2018). The effects of cognitive-focused interventions on cognition and psychological well-being in persons with multiple sclerosis: A meta-analysis. Neuropsychological rehabilitation, 1-20.
-
Hill, N.T., Mowszowski, L., Naismith, S.L., Chadwick, V.L., Valenzuela, M., & Lampit, A. (2017). Computerized cognitive training in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. The American Journal of Psychiatry, 174(4), 329–340.
-
Kambeitz-Ilankovic, L., Betz, L. T., Dominke, C., Haas, S. S., Subramaniam, K., Fisher, M., . . . Kambeitz, J. (2019). Multi-outcome meta-analysis (MOMA) of cognitive remediation in schizophrenia: Revisiting the relevance of human coaching and elucidating interplay between multiple outcomes. Neuroscience And Biobehavioral Reviews, 107, 828-845. https://doi.org/10.1016/j.neubiorev.2019.09.031
-
Khan, F., & Amatya, B. (2017). Rehabilitation in multiple sclerosis: A systematic review of systematic reviews. Archives of physical medicine and rehabilitation, 98(2), 353-367.
-
Klein, O. A., Drummond, A., Mhizha-Murira, J. R., Mansford, L., & dasNair, R. (2019). Effectiveness of cognitive rehabilitation for people with multiple sclerosis: A meta-synthesis of patient perspectives. Neuropsychological rehabilitation, 29(4), 491-512.
-
Lampit, A., Heine, J., Finke, C., Barnett, M. H., Valenzuela, M., Wolf, A., . . . Hill, N. T. M. (2019). Computerized cognitive training in multiple sclerosis: A systematic review and meta-analysis. Neurorehabilitation and neural repair, 33(9), 695-706. https://doi.org/10.1177/1545968319860490
-
Loetscher, T., Potter, K. J., Wong, D., & das Nair, R. (2019). Cognitive rehabilitation for attention deficits following stroke. Cochrane Database of Systematic Reviews, Issue 11. Art. No.: CD002842. https://doi.org/10.1002/14651858.CD002842.pub3
-
Liu, K. P., Hanly, J., Fahey, P., Fong, S. S., & Bye, R. (2019). A systematic review and meta-analysis of rehabilitative interventions for unilateral spatial neglect and hemianopia poststroke from 2006 through 2016. Archives of physical medicine and rehabilitation, 100(5), 956-979.
-
Merriman, N. A., Sexton, E., McCabe, G., Walsh, M. E., Rohde, D., Gorman, A., ... & Hickey, A. (2019). Addressing cognitive impairment following stroke: Systematic review and meta-analysis of non-randomised controlled studies of psychological interventions. BMJ open, 9(2), e024429.
-
Mewborn, C.M., Lindbergh, C.A., Stephen Miller, L. (2017). Cognitive interventions for cognitively healthy, mildly impaired, and mixed samples of older adults: A systematic review and meta-analysis of randomized-controlled trials. Neuropsychology Review, 27(4), 403-439. https://doi.org/10.1007/s11065-017-9350-8
-
Mowszowski, L., Lampit, A., Walton, C.C. & Naismith, S.L. (2016). Strategy-based cognitive training for improving executive functions in older adults: A systematic review. Neuropsychology Review, 26 (3), 252-270.
-
Nijman, S. A., Veling, W., van der Stouwe, E. C. D., & Pijnenborg, G. H. M. (2020). Social cognition training for people with a psychotic disorder: A network meta-analysis. Schizophrenia Bulletin, 46(5), 1086-1103. https://doi.org/10.1093/schbul/sbaa023
-
O’Donoghue, M., Leahy, S., Boland, P., Galvin, R., McManus, J., & Hayes, S. (2022). Rehabilitation of cognitive deficits poststroke: Systematic review and meta-analysis of randomized controlled trials. Stroke, 53(5), 1700-1710. https://doi.org/10.1161/STROKEAHA.121.034218
-
Peppel LD, Ribbers GM, Heijenbrok-Kal MH. (2020). Pharmacological and non-pharmacological interventions for depression after moderate-to-severe traumatic brain injury: A systematic review and meta-analysis. Journal of Neurotrauma, 37(14):1587-1596.
-
Rogers, J. M., Foord, R., Stolwyk, R. J., Wong, D., & Wilson, P. H. (2018). General and domain-specific effectiveness of cognitive remediation after stroke: Systematic literature review and meta-analysis. Neuropsychology Review, 28(3), 285-309.
-
Shah, T.M., Weinborn, M., Verdile, G., Sohrabi, H.R. & Martins, R.N. (2017). Enhancing cognitive functioning in healthly older adults: A systematic review of the clinical significance of commercially available computerized cognitive training in preventing cognitive decline. Neuropsychology Review, 27(1), 62-80. https://doi.org/10.1007/s11065-016-9338-9
-
Sherman, D.S., Mauser, J., Nuno, M., & Sherzai, D. (2017). The efficacy of cognitive intervention in mild cognitive impairment (MCI): A meta-analysis of outcomes on neuropsychological measures. Neuropsychology Review, 27(4), 440–484. https://doi.org/10.1007/s11065-017-9363-3
-
Sigmundsdottir, L., Longley, W. A., & Tate, R. L. (2016). Computerised cognitive training in acquired brain injury: A systematic review of outcomes using the International Classification of Functioning (ICF). Neuropsychological rehabilitation, 26(5-6), 673-741.
-
Su Y, Yuki M & Otsuki M. Non-pharmacological interventions for post-stroke fatigue: Systematic review and network meta-analysis. Journal of Clinical Medicine. 2020;9(3).
-
Sullivan KA, Kaye S-A, Blaine H, et al. Psychological approaches for the management of persistent postconcussion symptoms after mild traumatic brain injury: A systematic review. Disability and Rehabilitation. 2020;42(16):2243-2251.
-
Taylor, L.A., Mhizha-Murira, J.R., Smith, L., Potter, K-J., Wong, D., Evangelou, N., Lincoln, N.B., & das Nair, R. (2021). Memory rehabilitation for people with multiple sclerosis. Cochrane Database of Systematic Reviews, Issue 10, Art. No.: CD008754. https://doi.org/10.1002/14651858.CD008754.pub4
-
ten Brinke, L.F., Davis, J.C., Barha, C.K., & Liu-Ambrose, T. (2017). Effects of computerized cognitive training on neuroimaging outcomes in older adults: A systematic review. BMC Geriatrics, 17(1), 139. https://doi.org/10.1186/s12877-017-0529-x
-
Vita, A., Barlati, S., Ceraso, A., Nibbio, G., Ariu, C., Deste, G., & Wykes, T. (2021). Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. https://doi.org/10.1001/jamapsychiatry.2021.0620
Suggested Further Reading
-
Clare, L. (2008). Neuropsychological rehabilitation and people with dementia. Psychology Press. ISBN13: 9781841696768
-
Lincoln, N.B., Kneebone, I.I., Macniven, J.A., & Morris, R.C. (2011). Psychological management of stroke. Wiley-Blackwell. ISBN13: 9780470684269
-
Low, L., & Laver, K. (2021). Dementia rehabilitation: Evidence-based interventions and clinical recommendations. Australia: Academic Press.
-
Peters, D. H., Adam, T., Alonge, O., Agyepong, I. A., & Tran, N. (2013a). Implementation research: What it is and how to do it. British Medical Journal, 347, f6753. https://doi.org/10.1136/bmj.f6753
-
Peters, D.H., Tran, N.T. & Adam, T. (2013b). Implementation research in health: A practical guide. Alliance for Health Policy and Systems Research, World Health Organization. ISBN: 9789241506212
-
Ponsford, J., Sloan, S., & Snow, P. (2013). Traumatic brain injury: Rehabilitation for everyday adaptive living (2nd Ed.). Psychology Press. ISBN13: 9781848720275
-
Sohlberg, M.M. & Turkstra, L.S. (2011). Optimizing cognitive rehabilitation: Effective instructional methods. Guilford Publications. ISBN: 9781609182007
-
Wilson, B.A., Gracey, F., Evans, J.J., & Bateman, A. (2009). Neuropsychological rehabilitation: Theory, models, therapy and outcome. Cambridge University Press. ISBN: 9780521841498
-
Wilson, B., Winegardner, J., Van Heugten, C.M., & Ownsworth, T. (Eds). (2017). Neuropsychological rehabilitation: The international handbook. Routledge. ISBN: 9781138643093
Resources for Clinicians
Websites
-
CogTALE: https://cogtale.org
-
NeuroBITE: https://neurorehab-evidence.com/web/cms/content/home
-
ASSBI Resources: https://assbi.com.au/OnlineStore
-
Australian Dementia Network: https://www.australiandementianetwork.org.au/clinician/resources/
-
SharpBrains Brain Training Evaluation Checklist: https://sharpbrains.com/resources/10-question-evaluation-checklist
Communities of Practice
-
BRAINSPaN: https://assbi.com.au/BrainSPan (Australia, NZ, Asia–Pacific).
-
International Neuropsychological Society – Neuropsychological Intervention Special Interest Group (INS NI-SIG) (Worldwide).
-
Neuropsychologists in Rehabilitation Consultation Group (Victoria, Australia).
-
Victorian Neuropsychologists in the Community (VicNIC).
-
Neuropsychological Rehabilitation Interest Group (Western Australia).
-
Special Interest Group for Neuropsychological Intervention (NSW, Australia).
Short Courses
Availability of Data and Materials
No data was generated or analysed for this paper.
References
Aboulafia-Brakha, T., Buschbeck, C., Rochat, L., & Annoni, J. (2013). Feasibility and initial efficacy of a cognitive-behavioural group programme for managing anger and aggressiveness after traumatic brain injury. Neuropsychological Rehabilitation, 23(2), 216–233. https://doi.org/10.1080/09602011.2012.747443
Abramovitch, A., Short, T., & Schweiger, A. (2021). The C factor: Cognitive dysfunction as a transdiagnostic dimension in psychopathology. Clinical Psychology Review, 86, 102007. https://doi.org/10.1016/j.cpr.2021.102007
Ahrens, J., Shao, R., Blackport, D., Macaluso, S., Viana, R., Teasell, R., & Mehta, S. (2022). Cognitive-behavioral therapy for managing depressive and anxiety symptoms after stroke: A systematic review and meta-analysis. Topics in Stroke Rehabilitation, 1–16. https://doi.org/10.1080/10749357.2022.2049505
Alashram, A. R., Annino, G., & Padua, E. (2022). Rehabilitation interventions for cognitive deficits in stroke survivors: A systematic review of randomized controlled trials. Applied Neuropsychology: Adult, 1–27. https://doi.org/10.1080/23279095.2022.2130319
Alashram, A. R., Annino, G., Padua, E., Romagnoli, C., & Mercuri, N. B. (2019). Cognitive rehabilitation post traumatic brain injury: A systematic review for emerging use of virtual reality technology. Journal of Clinical Neuroscience, 66, 209–219. https://doi.org/10.1016/j.jocn.2019.04.026
Albert, N., Randers, L., Allott, K., Jensen, H. D., Melau, M., Hjorthøj, C., & Nordentoft, M. (2019). Cognitive functioning following discontinuation of antipsychotic medication. A naturalistic sub-group analysis from the OPUS II trial. Psychological Medicine, 49(7), 1138–1147. https://doi.org/10.1017/s0033291718001836
Ali, A., Morfin, J., Mills, J., Pasipanodya, E. C., Maas, Y. J., Huang, E., & Zedlitz, A. (2022). Fatigue after traumatic brain injury: A systematic review. Journal of Head Trauma Rehabilitation, 37(4), E249–E257. https://doi.org/10.1097/HTR.0000000000000710
Allott, K., Steele, P., Boyer, F., de Winter, A., Bryce, S., Alvarez-Jimenez, M., & Phillips, L. (2020). Cognitive strengths-based assessment and intervention in first-episode psychosis: A complementary approach to addressing functional recovery? Clinical Psychology Review, 79, 101871. https://doi.org/10.1016/j.cpr.2020.101871
Allott, K., van-der-EL, K., Bryce, S., Parrish, E. M., McGurk, S. R., Hetrick, S., Bowie, C. R., Kidd, S., Hamilton, M., Killackey, E., & Velligan, D. (2020). Compensatory interventions for cognitive impairments in psychosis: A systematic review and meta-analysis. Schizophrenia Bulletin. https://doi.org/10.1093/schbul/sbz134
Amieva, H., Robert, P. H., Grandoulier, A. S., Meillon, C., De Rotrou, J., Andrieu, S., & Dartigues, J. F. (2016). Group and individual cognitive therapies in Alzheimer’s disease: The ETNA3 randomized trial. International Psychogeriatrics, 28(5), 707–717. https://doi.org/10.1017/s1041610215001830
Anderson, N. (2019). State of the science on mild cognitive impairment (MCI). CNS Spectrums, 24(1), 78–87. https://doi.org/10.1017/S1092852918001347
Andrew, N. E., Kilkenny, M., Naylor, R., Purvis, T., Lalor, E., Moloczij, N., & Cadilhac, D. A. (2014). Understanding long-term unmet needs in Australian survivors of stroke. International Journal of Stroke, 9(Suppl A100), 106–112. https://doi.org/10.1111/ijs.12325
Aplaon, M., Belchior, P., Gelinas, I., Bier, N., & Aboujaoude, A. (2017). Interventions for individuals with young-onset dementia. A review of the literature. Journal of Aging Research and Lifestyle, 6, 28–31. https://doi.org/10.14283/jarcp.2016.123
Ashworth, F., Clarke, A., Jones, L., Jennings, C., & Longworth, C. (2015). An exploration of compassion focused therapy following acquired brain injury. Psychology and Psychotherapy, 88(2), 143–162. https://doi.org/10.1111/papt.12037
Australian Psychology Accreditation Council. (2019). Accreditation Standards for Psychology Programs (Version 1.2). https://apac.au/wp-content/uploads/2021/09/APAC-Accreditation-Standards_v1.2_rebranded.pdf
Australian Psychological Society, College of Clinical Neuropsychologists. (2011). College course approval guidelines for postgraduate specialist courses. https://www.psychologyboard.gov.au/search.aspx?profile=psychology&query=&collection=ahpra-websites-web&f.Content+type%7Ccontent=college+course+approaval+guidelines&f.website%7Cboard=ahpra
Baetge, S. J., Filser, M., Renner, A., Raithel, L. M., Lau, S., Pöttgen, J., & Penner, I. K. (2023). Supporting brain health in multiple sclerosis: Exploring the potential of neuroeducation combined with practical mindfulness exercises in the management of neuropsychological symptoms. Journal of Neurology, 1–14. https://doi.org/10.1007/s00415-023-11616-2
Bahar‐Fuchs, A., Martyr, A., Goh, A. M. Y., Sabates, J., & Clare, L. (2019). Cognitive training for people with mild to moderate dementia. Cochrane Database of Systematic Reviews (3). https://doi.org/10.1002/14651858.CD013069.pub2
Basso, M. R., Lowery, N., Ghormley, C., Combs, D., & Johnson, J. (2006). Self-generated learning in people with multiple sclerosis. Journal of the International Neuropsychological Society, 12(5), 640–648.
Bayley, M. T., Hurdowar, A., Richards, C. L., Korner-Bitensky, N., Wood-Dauphinee, S., Eng, J. J., & Graham, I. D. (2012). Barriers to implementation of stroke rehabilitation evidence: Findings from a multi-site pilot project. Disability and Rehabilitation, 34(19), 1633–1638. https://doi.org/10.3109/09638288.2012.656790
Bayly, M., Morgan, D. E., V., Kotsteniuk, J., Froehlich Chow, A., Peacock, S., & O'Connell, M. E. (2021). Does early-stage intervention improve caregiver well-being or their ability to provide care to persons with mild dementia or mild cognitive impairment? A systematic review and meta-analysis. Psychology and Aging, epub ahead of print. https://doi.org/10.1037/pag0000642
Beedham, W., Belli, A., Ingaralingam, S., Haque, S., & Upthegrove, R. (2020). The management of depression following traumatic brain injury: A systematic review with meta-analysis. Brain Injury, 34(10), 1287–1304. https://doi.org/10.1080/02699052.2020.1797169
Belleville, S., & Bherer, L. (2012). Biomarkers of cognitive training effects in aging. Current Translational Geriatrics and Experimental Gerontology Reports, 1(2), 104–110. https://doi.org/10.1007/s13670-012-0014-5
Bergquist, T., Gehl, C., Mandrekar, J., Lepore, S., Hanna, S., Osten, A., & Beaulieu, W. (2009). The effect of internet-based cognitive rehabilitation in persons with memory impairments after severe traumatic brain injury. Brain Injury, 23(10), 790–799. https://doi.org/10.1080/02699050903196688
Bhome, R., Berry, A. J., Huntley, J. D., & Howard, R. J. (2018). Interventions for subjective cognitive decline: Systematic review and meta-analysis. British Medical Journal Open, 8(7), e021610. https://doi.org/10.1136/bmjopen-2018-021610
Blatchford, L., & Cook, J. (2020). Patient perspectives about mild cognitive impairment: A systematic review. Clinical Gerontologist, 1–13. https://doi.org/10.1080/07317115.2020.1805536
Bosboom, P. R., Alfonso, H., Eaton, J., & Almeida, O. P. (2012). Quality of life in Alzheimer’s disease: Different factors associated with complementary ratings by patients and family carers. International Psychogeriatrics, 24(5), 708–721. https://doi.org/10.1017/s1041610211002493
Bourgeois, M. S., Lenius, K., Turkstra, L., & Camp, C. (2007). The effects of cognitive teletherapy on reported everyday memory behaviours of persons with chronic traumatic brain injury. Brain Injury, 21(12), 1245–1257. https://doi.org/10.1080/02699050701727452
Bowen, A., Hazelton, C., Pollock, A., & Lincoln, N. B. (2013). Cognitive rehabilitation for spatial neglect following stroke. Cochrane Database of Systematic Reviews (7), Cd003586. https://doi.org/10.1002/14651858.CD003586.pub3
Bowie, C. R., Bell, M. D., Fiszdon, J. M., Johannesen, J. K., Lindenmayer, J. P., McGurk, S. R., & Wykes, T. (2020). Cognitive remediation for schizophrenia: An expert working group white paper on core techniques. Schizophrenia Research, 215, 49–53. https://doi.org/10.1016/j.schres.2019.10.047
Bowie, C. R., Gupta, M., & Holshausen, K. (2013). Cognitive remediation therapy for mood disorders: Rationale, early evidence, and future directions. Canadian Journal of Psychiatry, 58(6), 319–325. https://doi.org/10.1177/070674371305800603
Brochet, B. (2021). Cognitive rehabilitation in multiple sclerosis in the period from 2013 and 2021: A narrative review. Brain Sciences, 12(1). https://doi.org/10.3390/brainsci12010055
Brodaty, H., & Arasaratnam, C. (2012). Meta-analysis of nonpharmacological interventions for neuropsychiatric symptoms of dementia. American Journal of Psychiatry, 169(9), 946–953. https://doi.org/10.1176/appi.ajp.2012.11101529
Brouwer, W., Van Zomneren, E., Berg, I., Bouma, A., & De Haan, E. (Eds.). (2002). Cognitive rehabilitation - A neuropsychological approach. Boom.
Bryce, S. D., Lee, S. J., Ponsford, J. L., & Rossell, S. L. (2016). Desire for greater clarity when defining ‘cognitive remediation’ in reviews of treatment efficacy for schizophrenia. Australian and New Zealand Journal of Psychiatry, 50(5), 497. https://doi.org/10.1177/0004867415617838
Burks, H. B., des Bordes, J. K. A., Chadha, R., Holmes, H. M., & Rianon, N. J. (2021). Quality of life assessment in older adults with dementia: A systematic review. Dementia and Geriatric Cognitive Disorders, 50(2), 103–110. https://doi.org/10.1159/000515317
Butler, M., McCreedy, E., Nelson, V. A., Desai, P., Ratner, E., Fink, H. A., & Kane, R. L. (2018). Does cognitive training prevent cognitive decline?: A systematic review. Annals of Internal Medicine, 168(1), 63–68. https://doi.org/10.7326/m17-1531
Camp, C. J. (2001). From efficacy to effectiveness to diffusion: Making the transitions in dementia intervention research. Neuropsychological Rehabilitation, 11(3–4), 495–517. https://doi.org/10.1080/09602010042000079
Carrier, S. L., Ponsford, J., Phyland, R. K., Hicks, A. J., & McKay, A. (2022). Effectiveness of non-pharmacological interventions for agitation during post-traumatic amnesia following traumatic brain injury: A systematic review. Neuropsychology Review. https://doi.org/10.1007/s11065-022-09544-5
Cations, M., Laver, K. E., Crotty, M., & Cameron, I. D. (2018). Rehabilitation in dementia care. Age and Ageing, 47(2), 171–174. https://doi.org/10.1093/ageing/afx173
Chandler, M., Parks, A., Marsiske, M., Rotblatt, L., & Smith, G. (2016). Everyday impact of cognitive interventions in mild cognitive impairment: A systematic review and meta-analysis. Neuropsychology Review, 26(3), 225–251. https://doi.org/10.1007/s11065-016-9330-4
Chen, C. L., Lin, M. Y., Huda, M. H., & Tsai, P. S. (2020). Effects of cognitive behavioral therapy for adults with post-concussion syndrome: A systematic review and meta-analysis of randomized controlled trials. Journal of Psychosomatic Research, 136, 110190. https://doi.org/10.1016/j.jpsychores.2020.110190
Chen, M. H., Chiaravalloti, N. D., & DeLuca, J. (2021). Neurological update: Cognitive rehabilitation in multiple sclerosis. Journal of Neurology, 268(12), 4908–4914. https://doi.org/10.1007/s00415-021-10618-2
Chiaravalloti, N. D., DeLuca, J., Moore, N. B., & Ricker, J. H. (2005). Treating learning impairments improves memory performance in multiple sclerosis: A randomized clinical trial. Multiple Sclerosis Journal, 11(1), 58–68.
Chiaravalloti, N. D., Moore, N. B., Nikelshpur, O. M., & DeLuca, J. (2013). An RCT to treat learning impairment in multiple sclerosis: The MEMREHAB trial. Neurology, 81(24), 2066–2072.
Chun, H. Y., Ford, A., Kutlubaev, M. A., Almeida, O. P., & Mead, G. E. (2022). Depression, anxiety, and suicide after stroke: A narrative review of the best available evidence. Stroke, 53(4), 1402–1410. https://doi.org/10.1161/STROKEAHA.121.035499
Clare, L. (2017). Rehabilitation for people living with dementia: A practical framework of positive support. PLOS Medicine, 14(3), e1002245. https://doi.org/10.1371/journal.pmed.1002245
Clare, L., Kudlicka, A., Oyebode, J. R., Jones, R. W., Bayer, A., Leroi, I., & Woods, B. (2019a). Goal-oriented cognitive rehabilitation for early-stage Alzheimer’s and related dementias: The GREAT RCT. Health Technology Assessment, 23(10), 1–242. https://doi.org/10.3310/hta23100
Clare, L., Kudlicka, A., Oyebode, J. R., Jones, R. W., Bayer, A., Leroi, I., & Woods, B. (2019b). Individual goal-oriented cognitive rehabilitation to improve everyday functioning for people with early-stage dementia: A multicentre randomised controlled trial (the GREAT trial). International Journal of Geriatric Psychiatry, 34(5), 709–721. https://doi.org/10.1002/gps.5076
Clare, L., Linden, D. E., Woods, R. T., Whitaker, R., Evans, S. J., Parkinson, C. H., & Rugg, M. D. (2010). Goal-oriented cognitive rehabilitation for people with early-stage Alzheimer disease: A single-blind randomized controlled trial of clinical efficacy. The American Journal of Geriatric Psychiatry, 18(10), 928–939. https://doi.org/10.1097/JGP.0b013e3181d5792a
Clare, L., Wilson, B. A., Carter, G., Roth, I., & Hodges, J. R. (2002). Relearning face-name associations in early Alzheimer’s disease. Neuropsychology, 16(4), 538–547. https://doi.org/10.1037/0894-4105.16.4.538
Clemson, L., Laver, K., Jeon, Y. H., Comans, T. A., Scanlan, J., Rahja, M., & Gitlin, L. N. (2018). Implementation of an evidence-based intervention to improve the wellbeing of people with dementia and their carers: Study protocol for ‘Care of People with dementia in their Environments (COPE)’ in the Australian context. BMC Geriatrics, 18(1), 108. https://doi.org/10.1186/s12877-018-0790-7
Cotelli, M., Manenti, R., Brambilla, M., Gobbi, E., Ferrari, C., Binetti, G., & Cappa, S. F. (2019). Cognitive telerehabilitation in mild cognitive impairment, Alzheimer’s disease and frontotemporal dementia: A systematic review. Journal of Telemedicine and Telecare, 25(2), 67–79. https://doi.org/10.1177/1357633X17740390
Couillet, J., Soury, S., Lebornec, G., Asloun, S., Joseph, P. A., Mazaux, J. M., & Azouvi, P. (2010). Rehabilitation of divided attention after severe traumatic brain injury: A randomised trial. Neuropsychological Rehabilitation, 20(3), 321–339. https://doi.org/10.1080/09602010903467746
Cowman, M., Holleran, L., Lonergan, E., O’Connor, K., Birchwood, M., & Donohoe, G. (2021). Cognitive predictors of social and occupational functioning in early psychosis: A systematic review and meta-analysis of cross-sectional and longitudinal data. Schizophrenia Bulletin. https://doi.org/10.1093/schbul/sbab033
Creighton, A. S., van der Ploeg, E. S., & O’Connor, D. W. (2013). A literature review of spaced-retrieval interventions: A direct memory intervention for people with dementia. International Psychogeriatrics, 25(11), 1743–1763. https://doi.org/10.1017/s1041610213001233
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implementation Science, 4, 50. https://doi.org/10.1186/1748-5908-4-50
Danner, U. N., Dingemans, A. E., & Steinglass, J. (2015). Cognitive remediation therapy for eating disorders. Current Opinion in Psychiatry, 28(6), 468–472. https://doi.org/10.1097/yco.0000000000000192
Dardiotis, E., Nousia, A., Siokas, V., Tsouris, Z., Andravizou, A., Mentis, A. A., & Nasios, G. (2018). Efficacy of computer-based cognitive training in neuropsychological performance of patients with multiple sclerosis: A systematic review and meta-analysis. Multiple Sclerosis and Related Disorders, 20, 58–66. https://doi.org/10.1016/j.msard.2017.12.017
das Nair, R., Cogger, H., Worthington, E., & Lincoln, N. B. (2016a). Cognitive rehabilitation for memory deficits after stroke. Cochrane Database of Systematic Reviews, 9, Cd002293. https://doi.org/10.1002/14651858.CD002293.pub3
das Nair, R., Martin, K. J., & Lincoln, N. B. (2016b). Memory rehabilitation for people with multiple sclerosis. Cochrane Database of Systematic Reviews, 3, Cd008754. https://doi.org/10.1002/14651858.CD008754.pub3
Davies, A., Rogers, J., Baker, K., Li, L., Llerena, J., das Nair, R., & Wong, D. (2023). Combined cognitive and psychological interventions improve meaningful outcomes after acquired brain injury: A systematic review and meta-analysis. Neuropsychology Review. https://doi.org/10.1007/s11065-023-09625-z
Davis, D., Evans, M., Jadad, A., Perrier, L., Rath, D., Ryan, D., & Zwarenstein, M. (2003). The case for knowledge translation: Shortening the journey from evidence to effect. British Medical Journal, 327(7405), 33–35. https://doi.org/10.1136/bmj.327.7405.33
de Vugt, M. E., & Verhey, F. R. (2013). The impact of early dementia diagnosis and intervention on informal caregivers. Progress in Neurobiology, 110, 54–62. https://doi.org/10.1016/j.pneurobio.2013.04.005
DeLuca, J., Chiaravalloti, N. D., & Sandroff, B. M. (2020). Treatment and management of cognitive dysfunction in patients with multiple sclerosis. Nature Reviews Neurology, 16(6), 319–332. https://doi.org/10.1038/s41582-020-0355-1
Diamond, K., Mowszowski, L., Cockayne, N., Norrie, L., Paradise, M., Hermens, D. F., & Naismith, S. L. (2015). Randomized controlled trial of a healthy brain ageing cognitive training program: Effects on memory, mood, and sleep. Journal of Alzheimer’s Disease, 44(4), 1181–1191. https://doi.org/10.3233/jad-142061
Douglas, K. M., Milanovic, M., Porter, R. J., & Bowie, C. R. (2020). Clinical and methodological considerations for psychological treatment of cognitive impairment in major depressive disorder. Bjpsych Open, 6(4), e67. https://doi.org/10.1192/bjo.2020.53
Dubois, B., Padovani, A., Scheltens, P., Rossi, A., & Dell’Agnello, G. (2016). Timely diagnosis for Alzheimer’s disease: A literature review on benefits and challenges. Journal of Alzheimer’s Disease, 49(3), 617–631. https://doi.org/10.3233/jad-150692
Durfee, A. Z., & Hillis, A. E. (2023). Unilateral spatial neglect recovery poststroke. Stroke, 54(1), 10–19. https://doi.org/10.1161/STROKEAHA.122.041710
Ernst, A., Blanc, F., De Seze, J., & Manning, L. (2015). Using mental visual imagery to improve autobiographical memory and episodic future thinking in relapsing-remitting multiple sclerosis patients: A randomised-controlled trial study. Restorative Neurology and Neuroscience, 33(5), 621–638.
Ernst, A., Botzung, A., Gounot, D., Sellal, F., Blanc, F., De Seze, J., & Manning, L. (2012). Induced brain plasticity after a facilitation programme for autobiographical memory in multiple sclerosis: A preliminary study. Multiple Sclerosis International, 2012.
Eslinger, P. J., & Damasio, A. R. (1986). Preserved motor learning in Alzheimer’s disease: Implications for anatomy and behavior. Journal of Neuroscience, 6(10), 3006–3009.
Evans, J. J., Greenfield, E., Wilson, B. A., & Bateman, A. (2009). Walking and talking therapy: Improving cognitive-motor dual-tasking in neurological illness. Journal of the International Neuropsychological Society, 15(1), 112–120. https://doi.org/10.1017/S1355617708090152
Fann, J. R., Hart, T., & Schomer, K. G. (2009). Treatment for depression after traumatic brain injury: A systematic review. Journal of Neurotrauma, 26(12), 2383–2402. https://doi.org/10.1089/neu.2009.1091
Fasotti, L., Kovacs, F., Eling, P. A. T. M., & Brouwer, W. H. (2000). Time pressure management as a compensatory strategy training after closed head injury. Neuropsychological Rehabilitation, 10(1), 47–65. https://doi.org/10.1080/096020100389291
Fett, A. K., Viechtbauer, W., Dominguez, M. D., Penn, D. L., van Os, J., & Krabbendam, L. (2011). The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: A meta-analysis. Neuroscience and Biobehavioral Reviews, 35(3), 573–588. https://doi.org/10.1016/j.neubiorev.2010.07.001
Firth, J., Stubbs, B., Rosenbaum, S., Vancampfort, D., Malchow, B., Schuch, F., & Yung, A. R. (2017). Aerobic exercise improves cognitive functioning in people with schizophrenia: A systematic review and meta-analysis. Schizophrenia Bulletin, 43(3), 546–556. https://doi.org/10.1093/schbul/sbw115
Fisher, A., Bellon, M., Lawn, S., & Lennon, S. (2021). Family perspectives on the acceptability and usefulness of the FAB Positive Behaviour Support program: A pilot study. Brain Injury, 35(5), 609–619. https://doi.org/10.1080/02699052.2021.1894479
Fleming, J., Shum, D., Strong, J., & Lightbody, S. (2005). Prospective memory rehabilitation for adults with traumatic brain injury: A compensatory training programme. Brain Injury, 19(1), 1–10. https://doi.org/10.1080/02699050410001720059
Fleming, R., & Purandare, N. (2010). Long-term care for people with dementia: Environmental design guidelines. International Psychogeriatrics, 22(7), 1084–1096. https://doi.org/10.1017/s1041610210000438
Fleming, R., & Sum, S. (2014). Empirical studies on the effectiveness of assistive technology in the care of people with dementia: A systematic review. Journal of Assistive Technologies, 8. https://doi.org/10.1108/JAT-09-2012-0021
Fox, S., Cahill, S., McGown, R., & Kilty, C. (2020). Young onset dementia: A review of diagnostic and post-diagnostic processes and pathways. National Dementia Office: Tullamore, Ireland. http://hdl.handle.net/10147/628311
Gallagher, M., McLeod, H. J., & McMillan, T. M. (2019). A systematic review of recommended modifications of CBT for people with cognitive impairments following brain injury. Neuropsychological Rehabilitation, 29(1), 1–21. https://doi.org/10.1080/09602011.2016.1258367
Galletly, C., Castle, D., Dark, F., Humberstone, V., Jablensky, A., Killackey, E., & Tran, N. (2016). Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for the management of schizophrenia and related disorders. Australian and New Zealand Journal of Psychiatry, 50(5), 410–472. https://doi.org/10.1177/0004867416641195
Gardner, B., Lally, P., & Wardle, J. (2012). Making health habitual: The psychology of ‘habit-formation’ and general practice. British Journal of General Practice, 62(605), 664–666. https://doi.org/10.3399/bjgp12X659466
Gates, N., Valenzuela, M., Sachdev, P. S., & Singh, M. A. (2014). Psychological well-being in individuals with mild cognitive impairment. Clinical Interventions in Aging, 9, 779–792. https://doi.org/10.2147/cia.S58866
Gates, N. J., & Sachdev, P. (2014). Is cognitive training an effective treatment for preclinical and early Alzheimer’s disease? Journal of Alzheimer’s Disease, 42(Suppl 4), S551-559. https://doi.org/10.3233/jad-141302
Gates, N. J., Vernooij, R. W., Di Nisio, M., Karim, S., March, E., Martínez, G., & Rutjes, A. W. (2019). Computerised cognitive training for preventing dementia in people with mild cognitive impairment. Cochrane Database of Systematic Reviews, 3(3), CD012279. https://doi.org/10.1002/14651858.CD012279.pub2
Gavelin, H. M., Lampit, A., Hallock, H., Sabatés, J., & Bahar-Fuchs, A. (2020). Cognition-oriented treatments for older adults: A systematic overview of systematic reviews. Neuropsychology Review, 30(2), 167–193. https://doi.org/10.1007/s11065-020-09434-8
Germain, S., Wojtasik, V., Lekeu, F., Quittre, A., Olivier, C., Godichard, V., & Salmon, E. (2019). Efficacy of cognitive rehabilitation in Alzheimer disease: A 1-year follow-up study. Journal of Geriatric Psychiatry and Neurology, 32(1), 16–23. https://doi.org/10.1177/0891988718813724
Gertler, P., Tate, R. L., & Cameron, I. D. (2015). Non-pharmacological interventions for depression in adults and children with traumatic brain injury. Cochrane Database of Systematic Reviews, (12), Cd009871. https://doi.org/10.1002/14651858.CD009871.pub2
Giebel, C., & Challis, D. (2015). Translating cognitive and everyday activity deficits into cognitive interventions in mild dementia and mild cognitive impairment. International Journal of Geriatric Psychiatry, 30(1), 21–31. https://doi.org/10.1002/gps.4170
Gilhooly, K. J., Gilhooly, M. L. M., Sullivan, M. P., McIntyre, A., Wilson, L., Harding, E., & Crutch, S. (2016). A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatrics, 16(1), 106. https://doi.org/10.1186/s12877-016-0280-8
Gillespie, D. C., Bowen, A., Chung, C. S., Cockburn, J., Knapp, P., & Pollock, A. (2015). Rehabilitation for post-stroke cognitive impairment: An overview of recommendations arising from systematic reviews of current evidence. Clinical Rehabilitation, 29(2), 120–128. https://doi.org/10.1177/0269215514538982
Glasgow, R. E., Vogt, T. M., & Boles, S. M. (1999). Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health, 89(9), 1322–1327. https://doi.org/10.2105/ajph.89.9.1322
Glenthøj, L. B., Hjorthøj, C., Kristensen, T. D., Davidson, C. A., & Nordentoft, M. (2017). The effect of cognitive remediation in individuals at ultra-high risk for psychosis: A systematic review. Npj Schizophrenia, 3(1), 20. https://doi.org/10.1038/s41537-017-0021-9
Goldenberg, G., & Hagmann, S. (1998). Therapy of activities of daily living in patients with apraxia. Neuropsychological Rehabilitation, 8(2), 123–141. https://doi.org/10.1080/713755559
Gorske, T. T., & Smith, S. R. (2009). Collaborative therapeutic neuropsychological assessment. Springer Science + Business Media. https://doi.org/10.1007/978-0-387-75426-0
Gould, K. R., Feeney, T. J., Hicks, A. J., & Ponsford, J. L. (2021). Individualized goal attainment scaling during a trial of positive behaviour support in adults with acquired brain injury. Neuropsychol Rehabilitation, 1–19. https://doi.org/10.1080/09602011.2021.1947325
Gould, K. R., Ponsford, J. L., Hicks, A. J., Hopwood, M., Renison, B., & Feeney, T. J. (2019). Positive behaviour support for challenging behaviour after acquired brain injury: An introduction to PBS + PLUS and three case studies. Neuropsychological Rehabilitation, 1–35. https://doi.org/10.1080/09602011.2019.1656647
Goverover, Y., Chiaravalloti, N., & DeLuca, J. (2008). Self-generation to improve learning and memory of functional activities in persons with multiple sclerosis: Meal preparation and managing finances. Archives of Physical Medicine and Rehabilitation, 89(8), 1514–1521.
Goverover, Y., Chiaravalloti, N., Genova, H., & DeLuca, J. (2018a). A randomized controlled trial to treat impaired learning and memory in multiple sclerosis: The self-GEN trial. Multiple Sclerosis Journal, 24(8), 1096–1104.
Goverover, Y., Chiaravalloti, N. D., O’Brien, A., & DeLuca, J. (2018b). Evidenced based cognitive rehabilitation for persons with multiple sclerosis: An updated review of the literature from 2007–2016. Archives of Physical Medicine and Rehabilitation, 99, 390–407.
Graham, I. D., Logan, J., Harrison, M. B., Straus, S. E., Tetroe, J., Caswell, W., & Robinson, N. (2006). Lost in knowledge translation: Time for a map? The Journal of Continuing Education in the Health Professions, 26(1), 13–24. https://doi.org/10.1002/chp.47
Greenhalgh, T., Robert, G., Macfarlane, F., Bate, P., & Kyriakidou, O. (2004). Diffusion of innovations in service organizations: Systematic review and recommendations. Milbank Quarterly, 82(4), 581–629. https://doi.org/10.1111/j.0887-378X.2004.00325.x
Grill, J. D., Apostolova, L. G., Bullain, S., Burns, J. M., Cox, C. G., Dick, M., & Karlawish, J. (2017). Communicating mild cognitive impairment diagnoses with and without amyloid imaging. Alzheimer’s Research & Therapy, 9(1), 35. https://doi.org/10.1186/s13195-017-0261-y
Gromisch, E. S., Fiszdon, J. M., & Kurtz, M. M. (2018). The effects of cognitive-focused interventions on cognition and psychological well-being in persons with multiple sclerosis: A meta-analysis. Neuropsychological Rehabilitation, 1–20.
Gruters, A. A., Ramakers, I. H., Verhey, F. R., Kessels, R. P., & de Vugt, M. E. (2021). A scoping review of communicating neuropsychological test results to patients and family members. Neuropsychology Review. https://doi.org/10.1007/s11065-021-09507-2
Grynszpan, O., Perbal, S., Pelissolo, A., Fossati, P., Jouvent, R., Dubal, S., & Perez-Diaz, F. (2011). Efficacy and specificity of computer-assisted cognitive remediation in schizophrenia: A meta-analytical study. Psychological Medicine, 41(1), 163–173. https://doi.org/10.1017/s0033291710000607
Guillamondegui, O. D., Montgomery, S. A., Phibbs, F. T., McPheeters, M. L., Alexander, P. T., Jerome, R. N., McKoy, J. N., Seroogy, J. J., Eicken, J. J., Krishnaswami, S., Salomon, R. M., & Hartmann, K. E. (2011). Traumatic brain injury and depression. Agency for Healthcare Research and Quality (US).
Hamalainen, P., & Rosti-Otajarvi, E. (2014). Is neuropsychological rehabilitation effective in multiple sclerosis? Neurodegenerative Disease Management, 4(2), 147–154. https://doi.org/10.2217/nmt.14.8
Hampstead, B. M., Gillis, M. M., & Stringer, A. Y. (2014). Cognitive rehabilitation of memory for mild cognitive impairment: A methodological review and model for future research. Journal of the International Neuropsychological Society, 20(2), 135–151. https://doi.org/10.1017/s1355617713001306
Hampstead, B. M., Stringer, A. Y., Iordan, A. D., Ploutz-Snyder, R., & Sathian, K. (2022). Toward rational use of cognitive training in those with mild cognitive impairment. Alzheimer’s & Dementia: THe Journal of the Alzheimer’s Association. https://doi.org/10.1002/alz.12718
Harrison, A. M., Safari, R., Mercer, T., Picariello, F., van der Linden, M. L., White, C., & Norton, S. (2021). Which exercise and behavioural interventions show most promise for treating fatigue in multiple sclerosis? A network meta-analysis. Multiple Sclerosis Journalt Scler, 27(11), 1657–1678. https://doi.org/10.1177/1352458521996002
Harrison, S. L., Dyer, S. M., Laver, K. E., Milte, R. K., Fleming, R., & Crotty, M. (2022). Physical environmental designs in residential care to improve quality of life of older people. Cochrane Database of Systematic Reviews, 3(3), CD012892. https://doi.org/10.1002/14651858.CD012892.pub2
Hart, T., Brockway, J. A., Maiuro, R. D., Vaccaro, M., Fann, J. R., Mellick, D., & Temkin, N. (2017). Anger self-management training for chronic moderate to severe traumatic brain injury: Results of a randomized controlled trial. The Journal of Head Trauma Rehabilitation, 32(5), 319–331. https://doi.org/10.1097/HTR.0000000000000316
Hill, N. T., Mowszowski, L., Naismith, S. L., Chadwick, V. L., Valenzuela, M., & Lampit, A. (2017). Computerized cognitive training in older adults with mild cognitive impairment or dementia: A systematic review and meta-analysis. American Journal of Psychiatry, 174(4), 329–340. https://doi.org/10.1176/appi.ajp.2016.16030360
Honan, C. A., McDonald, S., Tate, R., Ownsworth, T., Togher, L., Fleming, J., & Ponsford, J. (2017). Outcome instruments in moderate-to-severe adult traumatic brain injury: Recommendations for use in psychosocial research. Neuropsychol Rehabilitation, 1–21. https://doi.org/10.1080/09602011.2017.1339616
Huckans, M., Hutson, L., Twamley, E., Jak, A., Kaye, J., & Storzbach, D. (2013). Efficacy of cognitive rehabilitation therapies for mild cognitive impairment (MCI) in older adults: Working toward a theoretical model and evidence-based interventions. Neuropsychology Review, 23(1), 63–80. https://doi.org/10.1007/s11065-013-9230-9
Hudes, R., Baptist-Mohseni, N., Dimech, C., Rich, J. B., Troyer, A. K., & Vandermorris, S. (2022). Evaluating the effectiveness of compensatory memory interventions in adults with acquired brain injury: A systematic review and meta-analysis of memory and everyday outcomes. Neuropsychology, 36(4), 243–265. https://doi.org/10.1037/neu0000799
Hudes, R., Rich, J. B., Troyer, A. K., Yusupov, I., & Vandermorris, S. (2019). The impact of memory-strategy training interventions on participant-reported outcomes in healthy older adults: A systematic review and meta-analysis. Psychology and Aging, 34(4), 587–597. https://doi.org/10.1037/pag0000340
Impellizzeri, F., Leonardi, S., Latella, D., Maggio, M. G., Foti Cuzzola, M., Russo, M., & Calabrò, R. S. (2020). An integrative cognitive rehabilitation using neurologic music therapy in multiple sclerosis: A pilot study. Medicine (baltimore), 99(4), e18866. https://doi.org/10.1097/MD.0000000000018866
Iruthayarajah, J., Alibrahim, F., Mehta, S., Janzen, S., McIntyre, A., & Teasell, R. (2018). Cognitive behavioural therapy for aggression among individuals with moderate to severe acquired brain injury: A systematic review and meta-analysis. Brain Injury, 32(12), 1443–1449. https://doi.org/10.1080/02699052.2018.1496481
Jacoby, M., Averbuch, S., Sacher, Y., Katz, N., Weiss, P. L., & Kizony, R. (2013). Effectiveness of executive functions training within a virtual supermarket for adults with traumatic brain injury: A pilot study. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 21(2), 182–190. https://doi.org/10.1109/TNSRE.2012.2235184
Jeffay, E., Ponsford, J., Harnett, A., Janzen, S., Patsakos, E., Douglas, J., & Green, R. (2023). INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part III: Executive functions. The Journal of Head Trauma Rehabilitation, 38(1), 52–64. https://doi.org/10.1097/HTR.0000000000000834
Jeon, Y. H., Krein, L., O’Connor, C., Mowszowski, L., Duffy, S., Seeher, K., & Rauch, A. (2022). A systematic review of quality dementia clinical guidelines for the development of WHO’s package of interventions for rehabilitation. The Gerontologist. (Epub ahead of print, 31/08/2022). https://doi.org/10.1093/geront/gnac105
Jeon, Y. H., Simpson, J. M., Low, L.-F., Woods, R., Norman, R., Mowszowski, L., & Szanton, S. (2019). A pragmatic randomised controlled trial (RCT) and realist evaluation of the interdisciplinary home-bAsed Reablement program (I-HARP) for improving functional independence of community dwelling older people with dementia: An effectiveness-implementation hybrid design. BMC Geriatrics, 19(1), 199. https://doi.org/10.1186/s12877-019-1216-x
Kalb, R., Beier, M., Benedict, R. H., Charvet, L., Costello, K., Feinstein, A., & Harris, C. (2018). Recommendations for cognitive screening and management in multiple sclerosis care. Multiple Sclerosis Journal, 1352458518803785.
Kambeitz-Ilankovic, L., Betz, L. T., Dominke, C., Haas, S. S., Subramaniam, K., Fisher, M., & Kambeitz, J. (2019). Multi-outcome meta-analysis (MOMA) of cognitive remediation in schizophrenia: Revisiting the relevance of human coaching and elucidating interplay between multiple outcomes. Neuroscience and Biobehavioral Reviews, 107, 828–845. https://doi.org/10.1016/j.neubiorev.2019.09.031
Kangas, M., McDonald, S., Williams, J. R., & Smee, R. I. (2015). Acceptance and commitment therapy program for distressed adults with a primary brain tumor: A case series study. Supportive Care in Cancer, 23(10), 2855–2859. https://doi.org/10.1007/s00520-015-2804-8
Kasper, S., & Resinger, E. (2003). Cognitive effects and antipsychotic treatment. Psychoneuroendocrinology, 28, 27–38. https://doi.org/10.1016/S0306-4530(02)00115-4
Keefe, R. S., & Fenton, W. S. (2007). How should DSM-V criteria for schizophrenia include cognitive impairment? Schizophrenia Bulletin, 33(4), 912–920. https://doi.org/10.1093/schbul/sbm046
Kempnich, C. L., Wong, D., Georgiou-Karistianis, N., & Stout, J. C. (2017). Feasibility and efficacy of brief computerized training to improve emotion recognition in premanifest and early-symptomatic Huntington’s disease. Journal of the International Neuropsychological Society, 23(4), 314–321. https://doi.org/10.1017/S1355617717000145
Khan, F., & Amatya, B. (2017). Rehabilitation in multiple sclerosis: A systematic review of systematic reviews. Archives of Physical Medicine and Rehabilitation, 98(2), 353–367. https://doi.org/10.1016/j.apmr.2016.04.016
Kidd, S. A., Kerman, N., Ernest, D., Maples, N., Arthur, C., de Souza, S., & Velligan, D. (2018). A pilot study of a family cognitive adaptation training guide for individuals with schizophrenia. Psychiatric Rehabilitation Journal, 41(2), 109–117. https://doi.org/10.1037/prj0000204
Kim, S. (2015). Cognitive rehabilitation for elderly people with early-stage Alzheimer’s disease. Journal of Physical Therapy Science, 27(2), 543–546. https://doi.org/10.1589/jpts.27.543
King, A. C., & Dwan, C. (2017). Electronic memory aids for people with dementia experiencing prospective memory loss: A review of empirical studies. Dementia, 18(6), 1994–2007. https://doi.org/10.1177/1471301217735180
Kinsella, G. J., Ames, D., Storey, E., Ong, B., Pike, K. E., Saling, M. M., & Rand, E. (2016). Strategies for improving memory: A randomized trial of memory groups for older people, including those with mild cognitive impairment. Journal of Alzheimer’s Disease, 49, 31–43. https://doi.org/10.3233/JAD-150378
Kinsella, G. J., Mullaly, E., Rand, E., Pike, K. E., Reilly, A., & Cavuoto, M. G. (2020). Bridging the gap between clinical trials and community care: Translating a memory group for older people with mild cognitive impairment into a community-based organisation. Australasian Journal on Ageing, 39(2), e168–e177. https://doi.org/10.1111/ajag.12724
Kinsella, G. J., Ong, O., Storey, E., Wallace, J., & Hester, R. L. (2007). Elaborated spaced-retrieval & prospective memory in mild Alzheimer’s disease. Neuropsychological Rehabilitation, 17, 688–706. https://doi.org/10.1080/09602010600892824
Kubu, C. S., Ready, R. E., Festa, J. R., Roper, B. L., & Pliskin, N. H. (2016). The times they are a changin’: Neuropsychology and integrated care teams. The Clinical Neuropsychologist, 30(1), 51–65. https://doi.org/10.1080/13854046.2015.1134670
Kudlicka, A., Martyr, A., Bahar-Fuchs, A., Sabates, J., Woods, B., & Clare, L. (2023). Cognitive rehabilitation for people with mild to moderate dementia. Cochrane Database of Systematic Reviews, 2023(6), CD013388. https://doi.org/10.1002/14651858.CD013388.pub2
Kumar, D., Ashwini, K., Hegde, S., Prasanna, L., Joseph, B., Bose, A., & Gangadhar, B. N. (2019). Caregiver assisted home-based cognitive remediation for individuals diagnosed with schizophrenia: A pilot study. Asian Journal of Psychiatry, 42, 87–93. https://doi.org/10.1016/j.ajp.2019.03.010
Kurtz, M. M., Gagen, E., Rocha, N. B., Machado, S., & Penn, D. L. (2016). Comprehensive treatments for social cognitive deficits in schizophrenia: A critical review and effect-size analysis of controlled studies. Clinical Psychology Review, 43, 80–89. https://doi.org/10.1016/j.cpr.2015.09.003
Kurtz, M. M., & Richardson, C. L. (2012). Social cognitive training for schizophrenia: A meta-analytic investigation of controlled research. Schizophrenia Bulletin, 38(5), 1092–1104. https://doi.org/10.1093/schbul/sbr036
Kurz, A., Pohl, C., Ramsenthaler, M., & Sorg, C. (2009). Cognitive rehabilitation in patients with mild cognitive impairment. International Journal of Geriatric Psychiatry, 24(2), 163–168. https://doi.org/10.1002/gps.2086
Lakhani, A., Townsend, C., & Bishara, J. (2017). Traumatic brain injury amongst indigenous people: A systematic review. Brain Injury, 31(13–14), 1718–1730. https://doi.org/10.1080/02699052.2017.1374468
Lampit, A., Hallock, H., & Valenzuela, M. (2014). Computerized cognitive training in cognitively healthy older adults: A systematic review and meta-analysis of effect modifiers. PLoS Medicine, 11(11), e1001756. https://doi.org/10.1371/journal.pmed.1001756
Lampit, A., Heine, J., Finke, C., Barnett, M. H., Valenzuela, M., Wolf, A., & Hill, N. T. M. (2019). Computerized cognitive training in multiple sclerosis: A systematic review and meta-analysis. Neurorehabilitation and Neural Repair, 33(9), 695–706. https://doi.org/10.1177/1545968319860490
Lanca, M., Giuliano, A. J., Sarapas, C., Potter, A. I., Kim, M. S., West, A. L., & Chow, C. M. (2020). Clinical outcomes and satisfaction following neuropsychological assessment for adults: A community hospital prospective quasi-experimental study. Archives of Clinical Neuropsychology, 35(8), 1303–1311. https://doi.org/10.1093/arclin/acz059
Laver, K. E., Adey-Wakeling, Z., Crotty, M., Lannin, N. A., George, S., & Sherrington, C. (2020). Telerehabilitation services for stroke. Cochrane Database of Systematic Reviews, 1, CD010255. https://doi.org/10.1002/14651858.CD010255.pub3
Lavrencic, L. M., Donovan, T., Moffatt, L., Keiller, T., Allan, W., Delbaere, K., & Radford, K. (2021). Ngarraanga Giinganay (‘thinking peacefully’): Co-design and pilot study of a culturally-grounded mindfulness-based stress reduction program with older First Nations Australians. Evaluation and Program Planning, 87, 101929. https://doi.org/10.1016/j.evalprogplan.2021.101929
Lawson, D. W., Stolwyk, R. J., Ponsford, J. L., McKenzie, D. P., Downing, M. G., & Wong, D. (2020). Telehealth delivery of memory rehabilitation following stroke. Journal of the International Neuropsychological Society, 26(1), 58–71. https://doi.org/10.1017/S1355617719000651
Lee, R. S. C., Hermens, D. F., Naismith, S. L., Kaur, M., Guastella, A. J., Glozier, N., & Hickie, I. B. (2018). Clinical, neurocognitive and demographic factors associated with functional impairment in the Australian Brain and Mind Youth Cohort Study (2008–2016). British Medical Journal Open, 8(12), 022659. https://doi.org/10.1136/bmjopen-2018-022659
Li, H., Li, J., Li, N., Li, B., Wang, P., & Zhou, T. (2011). Cognitive intervention for persons with mild cognitive impairment: A meta-analysis. Ageing Research Reviews, 10(2), 285–296. https://doi.org/10.1016/j.arr.2010.11.003
Li, S. Q., Guthridge, S., Eswara Aratchige, P., Lowe, M. P., Wang, Z., Zhao, Y.-B., & Krause, V. L. (2014). Dementia prevalence and incidence among the Indigenous and non Indigenous populations of the Northern Territory. Medical Journal of Australia, 200.
Lincoln, N. B., Kneebone, I. I., Macniven, J. A. B., & Morris, R. C. (2012). Psychological management of stroke. John Wiley & Sons.
Lindsten-McQueen, K., Weiner, N. W., Wang, H. Y., Josman, N., & Connor, L. T. (2014). Systematic review of apraxia treatments to improve occupational performance outcomes. OTJR (Thorofare N J), 34(4), 183–192. https://doi.org/10.3928/15394492-20141006-02
Lindvall Dahlgren, C., & Ro, O. (2014). A systematic review of cognitive remediation therapy for anorexia nervosa - Development, current state and implications for future research and clinical practice. Journal of Eating Disorders, 2(1), 26. https://doi.org/10.1186/s40337-014-0026-y
Little, A., Byrne, C., & Coetzer, R. (2021). The effectiveness of cognitive behaviour therapy for reducing anxiety symptoms following traumatic brain injury: A meta-analysis and systematic review. NeuroRehabilitation, 48(1), 67–82. https://doi.org/10.3233/NRE-201544
Livingston, G., Huntley, J., Sommerlad, A., Ames, D., Ballard, C., Banerjee, S., & Mukadam, N. (2020). Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. The Lancet, 396(10248), 413–446. https://doi.org/10.1016/S0140-6736(20)30367-6
Loetscher, T., Potter, K. J., Wong, D., & das Nair, R. (2019). Cognitive rehabilitation for attention deficits following stroke. Cochrane Database of Systematic Reviews, 2019(11). https://doi.org/10.1002/14651858.CD002842.pub3
Loi, S. M., Cations, M., & Velakoulis, D. (2023). Young-onset dementia diagnosis, management and care: A narrative review. Medical Journal of Australia, 218(4), 182–189. https://doi.org/10.5694/mja2.51849
Londos, E., Boschian, K., Lindén, A., Persson, C., Minthon, L., & Lexell, J. (2008). Effects of a goal-oriented rehabilitation program in mild cognitive impairment: A pilot study. American Journal of Alzheimer’s Disease and Other Dementias, 23(2), 177–183. https://doi.org/10.1177/1533317507312622
Longley, W. A. (2022). Cognitive rehabilitation in multiple sclerosis. Australian Journal of General Practitioners, 51(4), 233–237.
Longley, W. A., Tate, R. L., & Brown, R. F. (2022). The psychological benefits of neuropsychological assessment feedback as a psycho-educational therapeutic intervention: A randomized-controlled trial with cross-over in multiple sclerosis. Neuropsychological Rehabilitation, 1–30. https://doi.org/10.1080/09602011.2022.2047734
Malhi, G. S., Bell, E., Bassett, D., Boyce, P., Bryant, R., Hazell, P., & Murray, G. (2021). The 2020 Royal Australian and New Zealand College of Psychiatrists clinical practice guidelines for mood disorders. Australian and New Zealand Journal of Psychiatry, 55(1), 7–117. https://doi.org/10.1177/0004867420979353
Man, D. W., Poon, W. S., & Lam, C. (2013). The effectiveness of artificial intelligent 3-D virtual reality vocational problem-solving training in enhancing employment opportunities for people with traumatic brain injury. Brain Injury, 27(9), 1016–1025. https://doi.org/10.3109/02699052.2013.794969
Matthews, M. L., Wells, Y., Pike, K. E., & Kinsella, G. J. (2020). Long-term effects of a memory group intervention reported by older adults. Neuropsychological Rehabilitation, 30(6), 1044–1058. https://doi.org/10.1080/09602011.2018.1544570
McDonald, S., Trimmer, E., Newby, J., Grant, S., Gertler, P., & Simpson, G. K. (2019). Providing on-line support to families of people with brain injury and challenging behaviour: A feasibility study. Neuropsychological Rehabilitation, 1–22. https://doi.org/10.1080/09602011.2019.1696846
McGurk, S. R., Twamley, E. W., Sitzer, D. I., McHugo, G. J., & Mueser, K. T. (2007). A meta-analysis of cognitive remediation in schizophrenia. American Journal of Psychiatry, 164(12), 1791–1802. https://doi.org/10.1176/appi.ajp.2007.07060906
McHugh, R. K., & Barlow, D. H. (2010). The dissemination and implementation of evidence-based psychological treatments. A review of current efforts. American Psychologist, 65(2), 73–84. https://doi.org/10.1037/a0018121
McIntyre, R. S., Anderson, N., Baune, B. T., Brietzke, E., Burdick, K., Fossati, P., & Stahl, S. M. (2019). Expert consensus on screening and assessment of cognition in psychiatry. CNS Spectrums, 24(1), 154–162. https://doi.org/10.1017/s1092852918001189
Medd, J., & Tate, R. L. (2000). Evaluation of an anger management therapy programme following acquired brain injury: A preliminary study. Neuropsychological Rehabilitation, 10(2), 185–201. https://doi.org/10.1080/096020100389246
Mesholam-Gately, R., Giuliano, A. J., Faraone, S. V., Goff, K. P., & Seidman, L. J. (2009). Neurocognition in first-episode schizophrenia: A meta-analytic review. Neuropsychology, 23(3), 315–336. https://doi.org/10.1037/a0014708
Mewborn, C. M., Lindbergh, C. A., & Stephen Miller, L. (2017). Cognitive interventions for cognitively healthy, mildly impaired, and mixed samples of older adults: A systematic review and meta-analysis of randomized-controlled trials. Neuropsychology Review, 27(4), 403–439. https://doi.org/10.1007/s11065-017-9350-8
Miller, L. A., & Radford, K. (2014). Testing the effectiveness of group-based memory rehabilitation in chronic stroke patients. Neuropsychological Rehabilitation, 24(5), 721–737. https://doi.org/10.1080/09602011.2014.894479
Miller, W. R., Yahne, C. E., Moyers, T. B., Martinez, J., & Pirritano, M. (2004). A randomized trial of methods to help clinicians learn motivational interviewing. Journal of Consulting and Clinical Psychology, 72(6), 1050–1062. https://doi.org/10.1037/0022-006X.72.6.1050
Miotto, E. C., Batista, A., Simon, S. S., & Hampstead, B. M. (2018). Neurophysiologic and cognitive changes arising from cognitive training interventions in persons with mild cognitive impairment: A systematic review. Neural Plasticity, 7301530.
Miskowiak, K. W., Burdick, K. E., Martinez-Aran, A., Bonnin, C. M., Bowie, C. R., Carvalho, A. F., & Vieta, E. (2017). Methodological recommendations for cognition trials in bipolar disorder by the International Society for Bipolar Disorders Targeting Cognition Task Force. Bipolar Disorders, 19(8), 614–626. https://doi.org/10.1111/bdi.12534
Miskowiak, K. W., Burdick, K. E., Martinez-Aran, A., Bonnin, C. M., Bowie, C. R., Carvalho, A. F., & Vieta, E. (2018). Assessing and addressing cognitive impairment in bipolar disorder: The International Society for Bipolar Disorders Targeting Cognition Task Force recommendations for clinicians. Bipolar Disorders, 20(3), 184–194. https://doi.org/10.1111/bdi.12595
Mitchell, A. J., Beaumont, H., Ferguson, D., Yadegarfar, M., & Stubbs, B. (2014). Risk of dementia and mild cognitive impairment in older people with subjective memory complaints: Meta-analysis. Acta Psychiatrica Scandinavica, 130(6), 439–451. https://doi.org/10.1111/acps.12336
Moniz Cook, E. D., Swift, K., James, I., Malouf, R., De Vugt, M., & Verhey, F. (2012). Functional analysis-based interventions for challenging behaviour in dementia. Cochrane Database of Systematic Reviews, (2), Cd006929. https://doi.org/10.1002/14651858.CD006929.pub2
Motter, J. N., Pimontel, M. A., Rindskopf, D., Devanand, D. P., Doraiswamy, P. M., & Sneed, J. R. (2016). Computerized cognitive training and functional recovery in major depressive disorder: A meta-analysis. Journal of Affective Disorders, 189, 184–191. https://doi.org/10.1016/j.jad.2015.09.022
Mowszowski, L., Batchelor, J., & Naismith, S. L. (2010). Early intervention for cognitive decline: Can cognitive training be used as a selective prevention technique? International Psychogeriatrics, 22(4), 537–548. https://doi.org/10.1017/s1041610209991748
Mowszowski, L., Lampit, A., Walton, C. C., & Naismith, S. L. (2016). Strategy-based cognitive training for improving executive functions in older adults: A systematic review. Neuropsychology Review, 26(3), 252–270. https://doi.org/10.1007/s11065-016-9329-x
Moyle, W., Jones, C. J., Murfield, J. E., Thalib, L., Beattie, E. R. A., Shum, D. K. H., & Draper, B. M. (2017). Use of a robotic seal as a therapeutic tool to improve dementia symptoms: A cluster-randomized controlled trial. Journal of the American Medical Directors Association, 18(9), 766–773. https://doi.org/10.1016/j.jamda.2017.03.018
Naismith, S. L., Michaelian, J. C., Low, L. F., Arsenova, V., Mehrani, I., Fyfe, K., & Sachdev, P. S. (2022). Characterising Australian memory clinics: Current practice and service needs informing national service guidelines. BMC Geriatrics, 22(1), 578. https://doi.org/10.1186/s12877-022-03253-7
Nauta, I. M., Bertens, D., Fasotti, L., Fieldhouse, J., Uitdehaag, B. M. J., Kessels, R. P. C., & de Jong, B. A. (2023). Cognitive rehabilitation and mindfulness reduce cognitive complaints in multiple sclerosis (REMIND-MS): A randomized controlled trial. Multiple Sclerosis and Related Disorders, 71, 104529. https://doi.org/10.1016/j.msard.2023.104529
Nguyen, L., Murphy, K., & Andrews, G. (2019a). Immediate and long-term efficacy of executive functions cognitive training in older adults: A systematic review and meta-analysis. Psychological Bulletin, 145(7), 698–733. https://doi.org/10.1037/bul0000196
Nguyen, S., McKay, A., Wong, D., Rajaratnam, S. M., Spitz, G., Williams, G., & Ponsford, J. L. (2017). Cognitive behavior therapy to treat sleep disturbance and fatigue after traumatic brain injury: A pilot randomized controlled trial. Archives of Physical Medicine and Rehabilitation, 98(8), 1508-1517.e1502. https://doi.org/10.1016/j.apmr.2017.02.031
Nguyen, S., Wong, D., McKay, A., Rajaratnam, S. M. W., Spitz, G., Williams, G., & Ponsford, J. L. (2019b). Cognitive behavioural therapy for post-stroke fatigue and sleep disturbance: A pilot randomised controlled trial with blind assessment. Neuropsychological Rehabilitation, 29(5), 723–738. https://doi.org/10.1080/09602011.2017.1326945
Nijman, S. A., Veling, W., van der Stouwe, E. C. D., & Pijnenborg, G. H. M. (2020). Social cognition training for people with a psychotic disorder: A network meta-analysis. Schizophrenia Bulletin, 46(5), 1086–1103. https://doi.org/10.1093/schbul/sbaa023
Njomboro, P. (2017). Social cognition deficits: Current position and future directions for neuropsychological interventions in cerebrovascular disease. Behavioural Neurology, 2017, 2627487. https://doi.org/10.1155/2017/2627487
Norton, S., Matthews, F. E., Barnes, D. E., Yaffe, K., & Brayne, C. (2014). Potential for primary prevention of Alzheimer’s disease: An analysis of population-based data. Lancet Neurology, 13(8), 788–794. https://doi.org/10.1016/s1474-4422(14)70136-x
O’Donoghue, M., Leahy, S., Boland, P., Galvin, R., McManus, J., & Hayes, S. (2022). Rehabilitation of cognitive deficits poststroke: Systematic review and meta-analysis of randomized controlled trials. Stroke, 53(5), 1700–1710. https://doi.org/10.1161/STROKEAHA.121.034218
O’Neil-Pirozzi, T. M., Strangman, G. E., Goldstein, R., Katz, D. I., Savage, C. R., Kelkar, K., & Glenn, M. B. (2010). A controlled treatment study of internal memory strategies (I-MEMS) following traumatic brain injury. The Journal of Head Trauma Rehabilitation, 25(1), 43–51. https://doi.org/10.1097/HTR.0b013e3181bf24b1
Ownsworth, T., Arnautovska, U., Beadle, E., Shum, D. H. K., & Moyle, W. (2018). Efficacy of telerehabilitation for adults with traumatic brain injury: A systematic review. The Journal of Head Trauma Rehabilitation, 33(4), E33–E46. https://doi.org/10.1097/HTR.0000000000000350
Ozier, D., Mariani, M., & Collins, M. (2019). Feasibility study of an intervention to improve emotional well-being and cognitive functioning in brain tumour survivors. Psycho-Oncology, 28(11), 2244–2246. https://doi.org/10.1002/pon.5217
Pagan, E., Ownsworth, T., McDonald, S., Fleming, J., Honan, C., & Togher, L. (2015). A survey of multidisciplinary clinicians working in rehabilitation for people with traumatic brain injury. Brain Impairment, 16(3), 173–195. https://doi.org/10.1017/BrImp.2015.34
Peppel, L. D., Ribbers, G. M., & Heijenbrok-Kal, M. H. (2020). Pharmacological and non-pharmacological interventions for depression after moderate-to-severe traumatic brain injury: A systematic review and meta-analysis. Journal of Neurotrauma, 37(14), 1587–1596. https://doi.org/10.1089/neu.2019.6735
Peters, D. H., Adam, T., Alonge, O., Agyepong, I. A., & Tran, N. (2013a). Implementation research: What it is and how to do it. British Medical Journal, 347, f6753. https://doi.org/10.1136/bmj.f6753
Peters, D. H., Tran, N. T., & Adam, T. (2013b). Implementation research in health: A practical guide. Alliance for Health Policy and Systems Research, World Health Organization. ISBN: 9789241506212.
Pike, K., & Kinsella, G. (2019). Alzheimer’s disease: Prodromal stages and dementia. In Degenerative disorders of the brain (pp. 32–65). Routledge.
Pike, K., Castellani, M., Morris, E., & Kinsella, G. (2020). Increasing skills of trainee psychologists for interventions with older clients. International Neuropsychological Society Conference, Denver, USA.
Pike, K. E., Cavuoto, M. G., Li, L., Wright, B. J., & Kinsella, G. J. (2022). Subjective cognitive decline: Level of risk for future dementia and mild cognitive impairment, a meta-analysis of longitudinal studies. Neuropsychology Review, 32(4), 703–735. https://doi.org/10.1007/s11065-021-09522-3
Pinner, G., & Bouman, W. P. (2003). Attitudes of patients with mild dementia and their carers towards disclosure of the diagnosis. International Psychogeriatrics, 15(3), 279–288. https://doi.org/10.1017/s1041610203009530
Ponsford, J., Lee, N. K., Wong, D., McKay, A., Haines, K., Alway, Y., & O’Donnell, M. L. (2016). Efficacy of motivational interviewing and cognitive behavioral therapy for anxiety and depression symptoms following traumatic brain injury. Psychological Medicine, 46(5), 1079–1090. https://doi.org/10.1017/S0033291715002640
Ponsford, J., Sloan, S., & Snow, P. (1995). Traumatic brain injury: Rehabilitation for everyday adaptive living. Lawrence Erlbaum Associates.
Ponsford, J., Trevena-Peters, J., Janzen, S., Harnett, A., Marshall, S., Patsakos, E., ... & INCOG Expert Panel. (2023a). INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part I: Posttraumatic amnesia. The Journal of Head Trauma Rehabilitation, 38(1), 24–37. https://doi.org/10.1097/HTR.0000000000000840
Ponsford, J., Velikonja, D., Janzen, S., Harnett, A., McIntyre, A., Wiseman-Hakes, C., & Bayley, M. T. (2023b). INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part II: Attention and information processing speed. The Journal of Head Trauma Rehabilitation, 38(1), 38–51. https://doi.org/10.1097/HTR.0000000000000839
Ponsford, J. L., Hicks, A. J., Gould, K. R., Downing, M. G., Hopwood, M., & Feeney, T. J. (2022). Positive behaviour support for adults with acquired brain injury and challenging behaviour: A randomised controlled trial. Annals of Physical and Rehabilitation Medicine, 65(2), 101604. https://doi.org/10.1016/j.rehab.2021.101604
Pöttgen, J., Friede, T., Lau, S., Gold, S. M., Letsch, C., Bender, G., & Penner, I. K. (2022). Managing neuropsychological impairment in multiple sclerosis - Controlled study on a standardized metacognitive intervention (MaTiMS). Multiple Sclerosis and Related Disorders, 59, 103687. https://doi.org/10.1016/j.msard.2022.103687
Pöttgen, J., Lau, S., Penner, I., Heesen, C., & Moritz, S. (2015). Managing neuropsychological impairment in multiple sclerosis: Pilot study on a standardized metacognitive intervention. International of Journal of MS Care, 17(3), 130–137. https://doi.org/10.7224/1537-2073.2014-015
Postal, K., & Armstrong, K. (2013). Feedback that sticks: The art of effectively communicating neuropsychological assessment results. Oxford University Press.
Poulin, V., Korner-Bitensky, N., Dawson, D. R., & Bherer, L. (2012). Efficacy of executive function interventions after stroke: A systematic review. Topics in Stroke Rehabilitation, 19(2), 158–171. https://doi.org/10.1310/tsr1902-158
Powell, B. J., McMillen, J. C., Proctor, E. K., Carpenter, C. R., Griffey, R. T., Bunger, A. C., & York, J. L. (2012). A compilation of strategies for implementing clinical innovations in health and mental health. Medical Care Research & Review, 69(2), 123–157. https://doi.org/10.1177/1077558711430690
Powell, J. M., Fraser, R., Brockway, J. A., Temkin, N., & Bell, K. R. (2016). A telehealth approach to caregiver self-management following traumatic brain injury: A randomized controlled trial. Journal of Head Trauma Rehabilitation, 31(3), 180–190. https://doi.org/10.1097/HTR.0000000000000167
Prigatano, G. P., & Morrone-Strupinsky, J. (2010). Advancing the profession of clinical neuropsychology with appropriate outcome studies and demonstrated clinical skills. The Clinical Neuropsychologist, 24(3), 468–480. https://doi.org/10.1080/13854040802585048
Radford, K., Mack, H. A., Draper, B., Chalkley, S., Daylight, G., Cumming, R., & Broe, G. A. (2015). Prevalence of dementia in urban and regional Aboriginal Australians. Alzheimers & Dementia, 11(3), 271–279. https://doi.org/10.1016/j.jalz.2014.03.007
Radford, K., Phillips, J., Drummond, A., Sach, T., Walker, M., Tyerman, A., & Jones, T. (2013). Return to work after traumatic brain injury: Cohort comparison and economic evaluation. Brain Injury, 27(5), 507–520. https://doi.org/10.3109/02699052.2013.766929
Radford, K., Say, M., Thayer, Z., & Miller, L. A. (2010). Making the most of your memory: An everyday memory skills program. ASSBI Resources.
Reijnders, J., van Heugten, C., & van Boxtel, M. (2013). Cognitive interventions in healthy older adults and people with mild cognitive impairment: A systematic review. Ageing Research Reviews, 12(1), 263–275. https://doi.org/10.1016/j.arr.2012.07.003
Reser, M. P., Slikboer, R., & Rossell, S. L. (2019). A systematic review of factors that influence the efficacy of cognitive remediation therapy in schizophrenia. Australian and New Zealand Journal of Psychiatry, 53(7), 624–641. https://doi.org/10.1177/0004867419853348
Rey-Casserly, C., Roper, B. L., & Bauer, R. M. (2012). Application of a competency model to clinical neuropsychology. Professional Psychology: Research and Practice, 43(5), 422–431. https://doi.org/10.1037/a0028721
Rogers, E. M. (2003). Diffusion of innovations (5th ed.). Free Press.
Rosado, D. L., Buehler, S., Botbol-Berman, E., Feigon, M., Leon, A., Luu, H., & Pliskin, N. H. (2018). Neuropsychological feedback services improve quality of life and social adjustment. The Clinical Neuropsychologist, 32(3), 422–435. https://doi.org/10.1080/13854046.2017.1400105
Rosti-Otajarvi, E. M., & Hamalainen, P. I. (2014). Neuropsychological rehabilitation for multiple sclerosis. Cochrane Database of Systematic Reviews, 2, Cd009131. https://doi.org/10.1002/14651858.CD009131.pub3
Roth, A. D., & Pilling, S. (2007). The competences required to deliver effective cognitive and behavioural therapy for people with depression and with anxiety disorders.
Sabe, L., Jason, L., Juejati, M., Leiguarda, R., & Starkstein, S. E. (1995). Dissociation between declarative and procedural learning in dementia and depression. Journal of Clinical & Experimental Neuropsychology: Official Journal of the International Neuropsychological Society, 17(6), 841–848. https://doi.org/10.1080/01688639508402433
Sander, A. M., Clark, A. N., Arciniegas, D. B., Tran, K., Leon-Novelo, L., Ngan, E., & Walser, R. (2020). A randomized controlled trial of acceptance and commitment therapy for psychological distress among persons with traumatic brain injury. Neuropsychological Rehabilitation, 1–25. https://doi.org/10.1080/09602011.2020.1762670
Salzman, T., Sarquis-Adamson, Y., Son, S., Montero-Odasso, M., & Fraser, S. (2022). Associations of multidomain interventions with improvements in cognition in mild cognitive impairment: A systematic review and meta-analysis. JAMA Network Open, 5, e226744. https://doi.org/10.1001/jamanetworkopen.2022.6744
Sanz Simon, S., Yokomizo, J. E., & Bottino, C. M. (2012). Cognitive intervention in amnestic mild cognitive impairment: A systematic review. Neuroscience & Biobehavioral Reviews, 36(4), 1163–1178. https://doi.org/10.1016/j.neubiorev.2012.01.007
Sathananthan, N., Dimech-Betancourt, B., Morris, E., Vicendese, D., Knox, L., Gillanders, D., & Wong, D. (2021). A single-case experimental evaluation of a new group-based intervention to enhance adjustment to life with acquired brain injury: VaLiANT (valued living after neurological trauma). Neuropsychological Rehabilitation, 1–33. https://doi.org/10.1080/09602011.2021.1971094
Savva, G. M., & Stephan, B. C. (2010). Epidemiological studies of the effect of stroke on incident dementia: A systematic review. Stroke, 41(1), e41-46. https://doi.org/10.1161/strokeaha.109.559880
Schefft, B. K., Dulay, M. F., & Fargo, J. D. (2008). The use of a self-generation memory encoding strategy to improve verbal memory and learning in patients with traumatic brain injury. Applied Neuropsychology, 15(1), 61–68. https://doi.org/10.1080/09084280801917806
Seccomandi, B., Tsapekos, D., Newbery, K., Wykes, T., & Cella, M. (2019). A systematic review of moderators of cognitive remediation response for people with schizophrenia. Schizophrenia Research: Cognition. https://doi.org/10.1016/j.scog.2019.100160
Semkovska, M., Quinlivan, L., O’Grady, T., Johnson, R., Collins, A., O’Connor, J., & Gload, T. (2019). Cognitive function following a major depressive episode: A systematic review and meta-analysis. Lancet Psychiatry, 6(10), 851–861. https://doi.org/10.1016/S2215-0366(19)30291-3
Shao, Y. K., Mang, J., Li, P. L., Wang, J., Deng, T., & Xu, Z. X. (2015). Computer-based cognitive programs for improvement of memory, processing speed and executive function during age-related cognitive decline: A meta-analysis. PLoS ONE, 10(6), e0130831. https://doi.org/10.1371/journal.pone.0130831
Sharpbrains. (n.d.). Brain Training Evaluation Checklist. Sharpbrains. Retrieved August 29, 2020, from https://sharpbrains.com/resources/10-question-evaluation-checklist/
Sherman, D. S., Mauser, J., Nuno, M., & Sherzai, D. (2017). The efficacy of cognitive intervention in mild cognitive impairment (MCI): A meta-analysis of outcomes on neuropsychological measures. Neuropsychology Review, 27(4), 440–484. https://doi.org/10.1007/s11065-017-9363-3
Shum, D., Fleming, J., Gill, H., Gullo, M. J., & Strong, J. (2011). A randomized controlled trial of prospective memory rehabilitation in adults with traumatic brain injury. Journal of Rehabilitation Medicine, 43(3), 216–223. https://doi.org/10.2340/16501977-0647
Sigmundsdottir, L., Longley, W. A., & Tate, R. L. (2016). Computerised cognitive training in acquired brain injury: A systematic review of outcomes using the International Classification of Functioning (ICF). Neuropsychological Rehabilitation, 26(5–6), 673–741. https://doi.org/10.1080/09602011.2016.1140657
Silva, A. R., Pinho, M. S., Macedo, L., & Moulin, C. J. A. (2017). The cognitive effects of wearable cameras in mild Alzheimer disease - An experimental study. Current Alzheimer Research, 14(12), 1270–1282. https://doi.org/10.2174/1567205014666170531083015
Simon, S. S., Castellani, M., Belleville, S., Dwolatzky, T., Hampstead, B. M., & Bahar-Fuchs, A. (2020). The design, evaluation, and reporting on non-pharmacological, cognition-oriented treatments for older adults: Results of a survey of experts. Alzheimer’s & Dementia: Translational Research & Clinical Interventions, 6(1), e12024. https://doi.org/10.1002/trc2.12024
Simons, A. D., Padesky, C. A., Montemarano, J., Lewis, C. C., Murakami, J., Lamb, K., & Beck, A. T. (2010). Training and dissemination of cognitive behavior therapy for depression in adults: A preliminary examination of therapist competence and client outcomes. Journal of Consulting & Clinical Psychology, 78(5), 751–756. https://doi.org/10.1037/a0020569
Smith, G., & CNS. (2018). Education and training in clinical neuropsychology: Recent developments and documents from the clinical neuropsychology synarchy. Archives of Clinical Neuropsychology, 34(3), 418–431. https://doi.org/10.1093/arclin/acy075
Stolwyk, R. J., Gooden, J. R., Kim, J., & Cadilhac, D. A. (2021). What is known about the cost-effectiveness of neuropsychological interventions for individuals with acquired brain injury? A Scoping Review. Neuropsychol Rehabil, 31(2), 316–344. https://doi.org/10.1080/09602011.2019.1692672
Stolwyk, R., Kelso, W., Hodge, A., Mullaly, E., Philpott, A., & Wong, D. (2022). Guidelines for the use of telehealth for clinical neuropsychological services: A practical guide to providing neuropsychological assessment and intervention via telehealth. Available upon request.
Stroke Foundation. (2017). Clinical guidelines for stroke management. https://informme.org.au/guidelines/clinical-guidelines-for-stroke-management
Stroke Foundation. (2020). National Stroke Audit – Rehabilitation services report 2020. https://informme.org.au/stroke-data/rehabilitation-audits
Stucky, K. J., Baker, L., Rush, B., Waldron-Perrine, B., Dean, P. M., & Barisa, M. (2023). Training in neurorehabilitation psychology: Defining competencies, requisite skill sets, and a proposed developmental pathway. Archives of Physical Medicine and Rehabilitation. https://doi.org/10.1016/j.apmr.2023.08.016
Sumowski, J. F. (2015). Cognitive reserve as a useful concept for early intervention research in multiple sclerosis. Frontiers in Neurology, 6, 176. https://doi.org/10.3389/fneur.2015.00176
Sumowski, J. F., Chiaravalloti, N., & DeLuca, J. (2010). Retrieval practice improves memory in multiple sclerosis: Clinical application of the testing effect. Neuropsychology, 24(2), 267.
Suo, C., & Valenzuela, M. J. (2012). Neuroimaging outcomes of brain training trials. Prof. Peter Bright (Ed.) Neuroimaging-Cognitive and Clinical Neuroscience, 417–430.
Takeuchi, H. (2015). Optimal antipsychotic dose and dosing interval in the treatment of schizophrenia. Seishin Shinkeigaku Zasshi, 117(7), 562–567. Japanese. PMID: 26552322.
Tappen, R. M., & Hain, D. (2014). The effect of in-home cognitive training on functional performance of individuals with mild cognitive impairment and early-stage Alzheimer’s disease. Research in Gerontological Nursing, 7(1), 14–24. https://doi.org/10.3928/19404921-20131009-01
Tate, R. L. (2010). A compendium of tests, scales and questionnaires: The practitioner’s guide to measuring outcomes after acquired brain impairment. Hove, UK: Psychology Press.
Taylor, L. A., Mhizha-Murira, J. R., Smith, L., Potter, K. J., Wong, D., Evangelou, N., & das Nair, R. (2021). Memory rehabilitation for people with multiple sclerosis. Cochrane Database of Systematic Reviews, 10, CD008754. https://doi.org/10.1002/14651858.CD008754.pub4
Taylor, P., Dorstyn, D. S., & Prior, E. (2020). Stress management interventions for multiple sclerosis: A meta-analysis of randomized controlled trials. Journal of Health Psychology, 25(2), 266–279. https://doi.org/10.1177/1359105319860185
Tchanturia, K., Lounes, N., & Holttum, S. (2014). Cognitive remediation in anorexia nervosa and related conditions: A systematic review. European Eating Disorders Review, 22(6), 454–462. https://doi.org/10.1002/erv.2326
ten Brinke, L. F., Davis, J. C., Barha, C. K., & Liu-Ambrose, T. (2017). Effects of computerized cognitive training on neuroimaging outcomes in older adults: A systematic review. BMC Geriatrics, 17(1), 139. https://doi.org/10.1186/s12877-017-0529-x
Tetlow, A. M., & Edwards, J. D. (2017). Systematic literature review and meta-analysis of commercially available computerized cognitive training among older adults. Journal of Cognitive Enhancement, 1(4), 559–575. https://doi.org/10.1007/s41465-017-0051-2
Thaut, M. H., Peterson, D. A., McIntosh, G. C., & Hoemberg, V. (2014). Music mnemonics aid verbal memory and induce learning–related brain plasticity in multiple sclerosis. Frontiers in Human Neuroscience, 8, 395.
Tible, O. P., Riese, F., Savaskan, E., & von Gunten, A. (2017). Best practice in the management of behavioural and psychological symptoms of dementia. Therapeutic Advances in Neurological Disorders, 10(8), 297–309. https://doi.org/10.1177/1756285617712979
Tsaousides, T., D’Antonio, E., Varbanova, V., & Spielman, L. (2014). Delivering group treatment via videoconference to individuals with traumatic brain injury: A feasibility study. Neuropsychological Rehabilitation, 24(5), 784–803. https://doi.org/10.1080/09602011.2014.907186
Turunen, M., Hokkanen, L., Bäckman, L., Stigsdotter-Neely, A., Hänninen, T., Paajanen, T., & Ngandu, T. (2019). Computer-based cognitive training for older adults: Determinants of adherence. PLoS ONE, 14(7), e0219541. https://doi.org/10.1371/journal.pone.0219541
Twamley, E. W., Vella, L., Burton, C. Z., Heaton, R. K., & Jeste, D. V. (2012). Compensatory cognitive training for psychosis: Effects in a randomized controlled trial. Journal of Clinical Psychiatry, 73(9), 1212–1219. https://doi.org/10.4088/JCP.12m07686
Valenzuela, M., & Sachdev, P. (2009). Can cognitive exercise prevent the onset of dementia? Systematic review of randomized clinical trials with longitudinal follow-up. The American Journal of Geriatric Psychiatry, 17(3), 179–187. https://doi.org/10.1097/JGP.0b013e3181953b57
Vallat-Azouvi, C., Azouvi, P., Le-Bornec, G., & Brunet-Gouet, E. (2019). Treatment of social cognition impairments in patients with traumatic brain injury: A critical review. Brain Injury, 33(1), 87–93. https://doi.org/10.1080/02699052.2018.1531309
Van der Roest, H. G., Wenborn, J., Pastink, C., Dröes, R.-M., & Orrell, M. (2017). Assistive technology for memory support in dementia. The Cochrane Database of Systematic Reviews, 6(6), CD009627–CD009627. https://doi.org/10.1002/14651858.CD009627.pub2
van Heugten, C. M. (2017). Evidence-based treatment. In Neuropsychological rehabillitation: The international handbook (pp. 17–24). Routledge.
van Heugten, C. M., Geurtsen, G. J., Derksen, R. E., Martina, J. D., Geurts, A. C., & Evers, S. M. (2011). Intervention and societal costs of residential community reintegration for patients with acquired brain injury: A cost-analysis of the Brain Integration Programme. Journal of Rehabilitation Medicine, 43(7), 647–652.
Vas, A. K., Chapman, S. B., Cook, L. G., Elliott, A. C., & Keebler, M. (2011). Higher-order reasoning training years after traumatic brain injury in adults. The Journal of Head Trauma Rehabilitation, 26(3), 224–239. https://doi.org/10.1097/HTR.0b013e318218dd3d
Velikonja, D., Ponsford, J., Janzen, S., Harnett, A., Patsakos, E., Kennedy, M., & Bayley, M. T. (2023). INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, part V: Memory. The Journal of Head Trauma Rehabilitation, 38(1), 83–102. https://doi.org/10.1097/HTR.0000000000000837
Velligan, D. I., Bow-Thomas, C. C., Huntzinger, C., Ritch, J., Ledbetter, N., Prihoda, T. J., & Miller, A. L. (2000). Randomized controlled trial of the use of compensatory strategies to enhance adaptive functioning in outpatients with schizophrenia. American Journal of Psychiatry, 157(8), 1317–1323. https://doi.org/10.1176/appi.ajp.157.8.1317
Verberne, D. P. J., Spauwen, P. J. J., & van Heugten, C. M. (2019). Psychological interventions for treating neuropsychiatric consequences of acquired brain injury: A systematic review. Neuropsychological Rehabilitation, 29(10), 1509–1542. https://doi.org/10.1080/09602011.2018.1433049
Vita, A., Barlati, S., Ceraso, A., Nibbio, G., Ariu, C., Deste, G., & Wykes, T. (2021). Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. https://doi.org/10.1001/jamapsychiatry.2021.0620
Wang, S. B., Wang, Y. Y., Zhang, Q. E., Wu, S. L., Ng, C. H., Ungvari, G. S., & Xiang, Y. T. (2018). Cognitive behavioral therapy for post-stroke depression: A meta-analysis. Journal of Affective Disorders, 235, 589–596. https://doi.org/10.1016/j.jad.2018.04.011
West, R. L., Bagwell, D. K., & Dark-Freudeman, A. (2008). Self-efficacy and memory aging: The impact of a memory intervention based on self-efficacy. Neuropsychology, Development, and Cognition. Section b, Aging, Neuropsychology and Cognition, 15(3), 302–329. https://doi.org/10.1080/13825580701440510
Whiting, D., Deane, F., McLeod, H., Ciarrochi, J., & Simpson, G. (2019). Can acceptance and commitment therapy facilitate psychological adjustment after a severe traumatic brain injury? A pilot randomized controlled trial. Neuropsychological Rehabilitation. https://doi.org/10.1080/09602011.2019.1583582
Williams, K., Blyler, D., Vidoni, E. D., Shaw, C., Wurth, J., Seabold, D., & Van Sciver, A. (2018). A randomized trial using telehealth technology to link caregivers with dementia care experts for in-home caregiving support: FamTechCare protocol. Research in Nursing & Health, 41(3), 219–227. https://doi.org/10.1002/nur.21869
Wilson, B. A. (2002). Towards a comprehensive model of cognitive rehabilitation. Neuropsychological Rehabilitation, 12(2), 97–110.
Wilson, B. A. (2017). The development of neuropsychological rehabilitation: An historical examination of theoretical and practical issues. In Neuropsychological rehabilitation: The international handbook (pp. 6–16). London: Routledge/Taylor & Francis Group. https://doi.org/10.4324/9781315629537
Withiel, T. D., Wong, D., Ponsford, J. L., Cadilhac, D. A., New, P., Mihaljcic, T., & Stolwyk, R. J. (2019). Comparing memory group training and computerized cognitive training for improving memory function following stroke: A phase II randomized controlled trial. Journal of Rehabilitation Medicine, 51, 343–351. https://doi.org/10.2340/16501977-2540
Wong, D., Baker, K., & Morris, E. M. J. (2021a). Psychology graduate outcomes: Evaluating the quality and impact of clinical psychology and clinical neuropsychology training in Australia. Australian Psychologist, 56(3), 204–216. https://doi.org/10.1080/00050067.2021.1890982
Wong, D., Grace, N., Baker, K., & McMahon, G. (2019a). Measuring clinical competencies in facilitating group-based rehabilitation interventions: Development of a new competency checklist. Clinical Rehabilitation, 33(6), 1079–1087. https://doi.org/10.1177/0269215519831048
Wong, D., Hsieh, M.-Y., McKay, A., Haines, K., O’Donnell, M., & Ponsford, J. (2019b). Cognitive behaviour therapy for anxiety and depression – adapted for brain injury (CBT-ABI): A treatment manual. ASSBI Resources.
Wong, D., Kempnich, C., Bradshaw, J., Grayson, S., Lillywhite, L., O’Shea, M., Kim, J., Stolwyk, R., & Cadilhac, D. A. (2021b). Real world implementation of a group-based memory rehabilitation program into stroke services: A knowledge translation evaluation. Topics in Stroke Rehabilitation, 28(6), 410–421. https://doi.org/10.1080/10749357.2020.1838084
Wong, D., McKay, A., & Stolwyk, R. (2014). Delivery of psychological interventions by clinical neuropsychologists: Current practice in Australia and implications for training. Australian Psychologist, 49(4), 209–222.
Wong, D., McKay, A., Kazantzis, N., & Ponsford, J. (2020). Clinical translation of cognitive behavioural therapy for anxiety and depression - adapted for brain injury (CBT-ABI): How do we train competent clinicians? International Journal of Cognitive Therapy. https://doi.org/10.1007/s41811-020-00079-2
Wong, D., Pestell, C., Oxenham, V., Stolwyk, R., Anderson, J., on behalf of the Australian Neuropsychology Alliance of Training and Practice Leaders (ANATPL). (2023a). Competencies unique to clinical neuropsychology: A consensus statement of educators, practitioners, and professional leaders in Australia. The Clinical Neuropsychologist. https://doi.org/10.1080/13854046.2023.2200035
Wong, D., Pinto, R., Price, S., Watson, L., & McKay, A. (2023b). What does competently delivered neuropsychological assessment feedback look like? Development and validation of a competency evaluation tool. The Clinical Neuropsychologist. https://doi.org/10.1080/13854046.2023.2200205
Woods, B., Rai, H. K., Elliott, E., Aguirre, E., Orrell, M., & Spector, A. (2023). Cognitive stimulation to improve cognitive functioning in people with dementia. Cochrane Database of Systematic Reviews, 2023(Issue 1), CD005562. https://doi.org/10.1002/14651858.CD005562.pub3
Woolf, C., Kaplan, L., Norrie, L. M., Burke, D., Cunich, M., Mowszowski, L. & Naismith, S. L. (under review). A feasibility, randomised controlled trial of Club Connect: a group-based healthy brain ageing cognitive training program for older adults with major depression within an Older People’s Mental Health Service [Manuscript submitted for publication]. Healthy Brain Ageing Program, Brain and Mind Centre, The University of Sydney.
Woolf, C., Lampit, A., Shahnawaz, Z., Sabates, J., Norrie, L. M., Burke, D., & Mowszowski, L. (2021). A systematic review and meta-analysis of cognitive training in adults with major depressive disorder. Neuropsychology Review. https://doi.org/10.1007/s11065-021-09487-3
World Health Organization. (2013). How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health (ICF). Exposure draft for comment. Geneva: World Health Organization.
World Health Organization. (2019). Risk reduction of cognitive decline and dementia: WHO guidelines. World Health Organization.
World Health Organisation. (2023). Package of interventions for rehabilitation. Module 3. Neurological conditions. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO.
Worthington, A. D., da Silva Ramos, S., & Oddy, M. (2017). The cost-effectiveness of neuropsychological rehabilitation. In B. A. Wilson, J. Winegardner, C. van Heugten, & T. Ownsworth (Eds.), Neuropsychological rehabilitation: The international handbook (1st ed., pp. 469–479). Routledge.
Wykes, T., Huddy, V., Cellard, C., McGurk, S. R., & Czobor, P. (2011). A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. American Journal of Psychiatry, 168(5), 472–485. https://doi.org/10.1176/appi.ajp.2010.10060855
Yip, B. C., & Man, D. W. (2009). Virtual reality (VR)-based community living skills training for people with acquired brain injury: A pilot study. Brain Injury, 23(13–14), 1017–1026. https://doi.org/10.3109/02699050903379412
Ylvisaker, M., Jacobs, H. E., & Feeney, T. (2003). Positive supports for people who experience behavioral and cognitive disability after brain injury: A review. The Journal of Head Trauma Rehabilitation, 18(1), 7–32. https://doi.org/10.1097/00001199-200301000-00005
Ylvisaker, M., Turkstra, L., Coehlo, C., Yorkston, K., Kennedy, M., Sohlberg, M. M., & Avery, J. (2007). Behavioural interventions for children and adults with behaviour disorders after TBI: A systematic review of the evidence. Brain Injury, 21(8), 769–805. https://doi.org/10.1080/02699050701482470
Ymer, L., McKay, A., Wong, D., Frencham, K., Grima, N., Tran, J., & Ponsford, J. (2021). Cognitive behavioural therapy versus health education for sleep disturbance and fatigue after acquired brain injury: A pilot randomised trial. Annals of Physical and Rehabilitation Medicine, 64(5), 101560. https://doi.org/10.1016/j.rehab.2021.101560
Yu, C., Sommerlad, A., Sakure, L., & Livingston, G. (2022). Socially assistive robots for people with dementia: Systematic review and meta-analysis of feasibility, acceptability and the effect on cognition, neuropsychiatric symptoms and quality of life. Ageing Research Reviews, 78, 101633. https://doi.org/10.1016/j.arr.2022.101633
Zamiri, M., Sarraipa, J., Luis-Ferreira, F., Manus, G. M., O'Brien, P., Camarinha-Matos, L. M., & Jardim-Goncalves, R. (2021). Review of technology-supported multimodal solutions for people with dementia. Sensors (Basel), 21(14). https://doi.org/10.3390/s21144806
Zangwill, O. L. (1947). Psychological aspects of rehabilitation in cases of brain injury. The British Journal of Psychology. General Section, 37(2), 60–69.
Zedlitz, A. M. E. E., Rietveld, T. C. M., Geurts, A. C., & Fasotti, L. (2012). Cognitive and graded activity training can alleviate persistent fatigue after stroke. Stroke, 43(4), 1046–1051. https://doi.org/10.1161/STROKEAHA.111.632117
Zhang, H., Huntley, J., Bhome, R., Holmes, B., Cahill, J., Gould, R. L., & Howard, R. (2019). Effect of computerised cognitive training on cognitive outcomes in mild cognitive impairment: A systematic review and meta-analysis. British Medical Journal Open, 9(8), e027062. https://doi.org/10.1136/bmjopen-2018-027062
Zokaei, N., MacKellar, C., Čepukaitytė, G., Patai, E. Z., & Nobre, A. C. (2017). Cognitive training in the elderly: Bottlenecks and new avenues. Journal of Cognitive Neuroscience, 29(9), 1473–1482. https://doi.org/10.1162/jocn_a_01080
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Partial financial support was received from a La Trobe University Social Research Assistance grant to Dana Wong and Kerryn Pike.
Author information
Authors and Affiliations
Contributions
All authors contributed to the paper’s conception and design and performed relevant literature searches. All authors contributed to various sections in the first draft of the manuscript and revisions to these. Dana Wong and Loren Mowszowski were responsible for integrating the sections and finalising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
As no data was collected directly for this paper, no ethical approval was required.
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1. Tables 1 and 2 (summary of evidence in TBI, stroke, and non-degenerative ABI)
Appendix 2. Tables 3 and 4 (summary of evidence in MS)
Appendix 3. Table 5 (summary of evidence in psychiatric disorders)
Appendix 4. Tables 6 and 7 (summary of evidence in dementia)
Appendix 5. Tables 8 and 9 (summary of evidence in MCI)
Appendix 6. Table 10 (summary of evidence in healthy older adults)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wong, D., Pike, K., Stolwyk, R. et al. Delivery of Neuropsychological Interventions for Adult and Older Adult Clinical Populations: An Australian Expert Working Group Clinical Guidance Paper. Neuropsychol Rev (2023). https://doi.org/10.1007/s11065-023-09624-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11065-023-09624-0