Abstract
Purpose
In Prolactinomas, surgery or radiation are reserved for DA failure due to tumor resistance, intolerance to medication-induced side-effects, or patient preference. This systematic review and meta-analysis summarizes the currently available literature regarding the effectiveness of surgery to treat prolactinomas in patients who have failed DA therapy.
Method
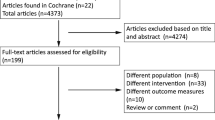
A literature search was conducted according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for studies that reported outcomes of medically resistant and intolerant prolactinoma treated surgically.
Results
10 articles (Total N = 816, Surgery N = 657) met the inclusion criteria. 38% of patients who underwent surgery following DA failure achieved remission without need for further treatment (p < 0.001, I2 = 67.09%) with a median follow-up of 49.2 +/− 40 months. 62% achieved remission with multimodal treatment (p < 0.001, I2 = 93.28%) with a median follow-up of 53 +/- 39.8 months. 16% of cases demonstrated recurrence after early remission (p = 0.02, I2 = 62.91%) with recurrence occurring on average at 27 +/- 9 months. Overall, 46% of patients required reinstitution of postoperative DA therapy at last follow up (p < 0.001, I2 = 82.57%). Subgroup analysis of macroprolactinoma and microprolactinoma has demonstrated that there is no statistical significance in achieving long-term remission with surgery stand-alone in macroprolactinoma group (p = 0.49) although 43% of patients were able to achieve remission with multimodal therapy at last follow-up in the same group (p < 0.001, I2 = 86.34%).
Conclusions
This systematic review and meta-analysis revealed 38% of operated patients achieved remission, while 62% achieved remission when additional modes of therapy were implemented. Therefore, although surgery has not been initial therapeutic choice for prolactinoma, it plays a significant role in medically failed prolactinoma care.






Similar content being viewed by others
Data availability
All available data and materials included in Text, figures, tables, supplementals and references.
Code availability
Not applicable.
References
Vroonen L, Daly AF, Beckers A (2019) Epidemiology and management challenges in prolactinomas. Neuroendocrinology 109(1):20–27. https://doi.org/10.1159/000497746
Ciccarelli A, Daly AF, Beckers A (2005) The epidemiology of prolactinomas. Pituitary 8(1):3–6. doi:https://doi.org/10.1007/s11102-005-5079-0
Melmed S, Casanueva FF, Hoffman AR et al (2011) Diagnosis and treatment of hyperprolactinemia: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96(2):273–288. https://doi.org/10.1210/jc.2010-1692
Ono M, Miki N, Kawamata T et al (2008) Prospective study of high-dose cabergoline treatment of prolactinomas in 150 patients. J Clin Endocrinol Metab 93(12):4721–4727. doi:https://doi.org/10.1210/jc.2007-2758
Webster J (1996) A comparative review of the tolerability profiles of dopamine agonists in the treatment of hyperprolactinaemia and inhibition of lactation. Drug Saf 14(4):228–238. https://doi.org/10.2165/00002018-199614040-00003
Colao A, Vitale G, Cappabianca P et al (2004) Outcome of cabergoline treatment in men with prolactinoma: effects of a 24-month treatment on prolactin levels, tumor mass, recovery of pituitary function, and semen analysis. J Clin Endocrinol Metab 89(4):1704–1711. https://academic.oup.com/jcem/article-abstract/89/4/1704/2844342
Webster J, Piscitelli G, Polll A et al. The efficacy and tolerability of long-term cabergoline therapy in hyperprolactinaemic disorders: an open, uncontrolled, multicentre study. Clin Endocrinol. 1993;39(3):323–329. https://onlinelibrary.wiley.com/doi/abs/https://doi.org/10.1111/j.1365-2265.1993.tb02372.x
Colao A, di Sarno A, Pivonello R, di Somma C, Lombardi G (2002) Dopamine receptor agonists for treating prolactinomas. Expert Opin Investig Drugs 11(6):787–800. doi:https://doi.org/10.1517/13543784.11.6.787
Serri O, Beauregard H, Lesage J et al (1990) Long term treatment with CV 205–502 in patients with prolactin-secreting pituitary macroadenomas. J Clin Endocrinol Metab 71(3):682–687. doi:https://doi.org/10.1210/jcem-71-3-682
Delgrange E, Crabbé J, Donckier J (1998) Late development of resistance to bromocriptine in a patient with macroprolactinoma. Horm Res 49(5):250–253. doi:https://doi.org/10.1159/000023180
Molitch ME (2003) Dopamine resistance of prolactinomas. Pituitary 6(1):19–27. doi:https://doi.org/10.1023/a:1026225625897
Molitch ME (2005) Pharmacologic resistance in prolactinoma patients. Pituitary 8(1):43–52. doi:https://doi.org/10.1007/s11102-005-5085-2
Souteiro P, Karavitaki N (2020) Dopamine agonist resistant prolactinomas: any alternative medical treatment? Pituitary 23(1):27–37. doi:https://doi.org/10.1007/s11102-019-00987-3
Maiter D (2019) Management of dopamine agonist-resistant prolactinoma. Neuroendocrinology 109(1):42–50. https://doi.org/10.1159/000495775
Gillam MP, Molitch ME, Lombardi G, Colao A (2006) Advances in the treatment of prolactinomas. Endocr Rev 27(5):485–534. doi:https://doi.org/10.1210/er.2005-9998
Bolko P, Jaskuła M, Waśko R, Wołuń M, Sowiński J (2003) The assessment of cabergoline efficacy and tolerability in patients with pituitary prolactinoma type. Pol Arch Med Wewn 109(5):489–495. https://www.ncbi.nlm.nih.gov/pubmed/14768178
Menucci M, Quiñones-Hinojosa A, Burger P, Salvatori R (2011) Effect of dopaminergic drug treatment on surgical findings in prolactinomas. Pituitary 14(1):68–74. doi:https://doi.org/10.1007/s11102-010-0261-4
Iglesias P, Díez JJ (2013) Macroprolactinoma: a diagnostic and therapeutic update. QJM 106(6):495–504. doi:https://doi.org/10.1093/qjmed/hcs240
Oh MC, Aghi MK (2011) Dopamine agonist-resistant prolactinomas. J Neurosurg 114(5):1369–1379. doi:https://doi.org/10.3171/2010.11.JNS101369
Casanueva FF, Molitch ME, Schlechte JA et al (2006) Guidelines of the pituitary society for the diagnosis and management of prolactinomas. Clin Endocrinol 65(2):265–273. https://doi.org/10.1111/j.1365-2265.2006.02562.x
Araujo-Castro M, López AA, Pardo JA, Kanaan LK, Palacios García N (2020) Phenotype and resistance patterns of 10 resistant prolactinomas. Endocrinol Diabetes Nutr 67(3):194–204. https://doi.org/10.1016/j.endinu.2019.04.007
Donegan D, Atkinson JLD, Jentoft M et al (2017) Surgical outcomes of prolactinomas in recent era: results of a heterogenous group. Endocr Pract 23(1):37–45. https://doi.org/10.4158/EP161446.OR
Kreutzer J, Buslei R, Wallaschofski H et al (2008) Operative treatment of prolactinomas: indications and results in a current consecutive series of 212 patients. Eur J Endocrinol 158(1):11–18. doi:https://doi.org/10.1530/EJE-07-0248
Smith TR, Hulou MM, Huang KT et al (2015) Current indications for the surgical treatment of prolactinomas. J Clin Neurosci 22(11):1785–1791. doi:https://doi.org/10.1016/j.jocn.2015.06.001
Primeau V, Raftopoulos C, Maiter D (2012) Outcomes of transsphenoidal surgery in prolactinomas: improvement of hormonal control in dopamine agonist-resistant patients. Eur J Endocrinol 166(5):779–786. doi:https://doi.org/10.1530/EJE-11-1000
Iuliano SL, Bi WL, Laws ER (2021) Changes in the options for management of prolactin secreting pituitary adenomas. J Neurol Surg B Skull BaseDoi. https://doi.org/10.1055/s-0040-1722665
Zamanipoor Najafabadi AH, Zandbergen IM, de Vries F et al (2020) Surgery as a viable alternative first-line treatment for prolactinoma patients. A systematic review and meta-analysis. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgz144
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. doi:https://doi.org/10.1016/j.ijsu.2010.02.007
Ottawa Hospital Research Institute. Accessed April 17 (2021) http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Atkins D, Best D, Briss PA et al (2004) Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490. doi:https://doi.org/10.1136/bmj.328.7454.1490
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. doi:https://doi.org/10.1136/bmj.327.7414.557
Akin S, Isikay I, Soylemezoglu F, Yucel T, Gurlek A, Berker M (2016) Reasons and results of endoscopic surgery for prolactinomas: 142 surgical cases. Acta Neurochir 158(5):933–942. doi:https://doi.org/10.1007/s00701-016-2762-z
Kars M, Pereira AM, Smit JW, Romijn JA (2009) Long-term outcome of patients with macroprolactinomas initially treated with dopamine agonists. Eur J Intern Med 20(4):387–393. doi:https://doi.org/10.1016/j.ejim.2008.11.012
Zhao Y, Jin D, Lian W et al (2019) Clinical characteristics and surgical outcome of prolactinoma in patients under 14 years old. Medicine 98(6):e14380. doi:https://doi.org/10.1097/MD.0000000000014380
Vale FL, Deukmedjian AR, Hann S, Shah V, Morrison AD (2013) Medically treated prolactin-secreting pituitary adenomas: when should we operate? Br J Neurosurg 27(1):56–62. doi:https://doi.org/10.3109/02688697.2012.714817
Vroonen L, Jaffrain-Rea M-L, Petrossians P et al (2012) Prolactinomas resistant to standard doses of cabergoline: a multicenter study of 92 patients. Eur J Endocrinol 167(5):651–662. doi:https://doi.org/10.1530/EJE-12-0236
Ioachimescu AG, Fleseriu M, Hoffman AR, Vaughan TB, Iii, Katznelson L (2019) Psychological effects of dopamine agonist treatment in patients with hyperprolactinemia and prolactin-secreting adenomas. Eur J Endocrinol 180(1):31–40. doi:https://doi.org/10.1530/EJE-18-0682
Bloomgarden E, Molitch ME (2014) Surgical treatment of prolactinomas: cons. Endocrine 47(3):730–733. https://doi.org/10.1007/s12020-014-0369-9
Mohan N, Chia YY, Goh GH, Ting E, Teo K, Yeo TT (2017) Cabergoline-induced fibrosis of prolactinomas: a neurosurgical perspective. BMJ Case RepDoi. https://doi.org/10.1136/bcr-2017-220971
Gen M, Uozumi T, Ohta M, Ito A, Kajiwara H, Mori S (1984) Necrotic changes in prolactinomas after long term administration of bromocriptine*. J Clin Endocrinol Metabol 59(3):463–470. https://doi.org/10.1210/jcem-59-3-463
Takahashi T, Kuwayama A, Katoh T, Kageyama N (1986) Histological changes and operative findings of pituitary adenomas after bromocriptine treatment. Nihon Naibunpi Gakkai Zasshi 62(12):1336–1351. doi:https://doi.org/10.1507/endocrine1927.62.12_1336
Zygourakis CC, Imber BS, Chen R et al (2017) Cost-effectiveness analysis of surgical versus medical treatment of prolactinomas. J Neurol Surg B Skull Base 78(2):125–131. https://doi.org/10.1055/s-0036-1592193
Funding
No funding sources to disclose.
Author information
Authors and Affiliations
Contributions
KJY—Conception and study design, data collection, data analysis, writing an original draft. DE, IB, JLDA, GC, MPC—Conception and study design, critically revising draft. JVG—Study supervision, conception and study design, critically revising draft, approving final version of draft.
Corresponding author
Ethics declarations
Conflict of interest
No conflict(s) of interest to disclose.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yagnik, K.J., Erickson, D., Bancos, I. et al. Surgical outcomes of medically failed prolactinomas: a systematic review and meta-analysis. Pituitary 24, 978–988 (2021). https://doi.org/10.1007/s11102-021-01188-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-021-01188-7