Abstract
The COVID-19 pandemic presents several challenges to the organisation and workflow of pharmacovigilance centres as a result of the massive increase in reports, the need for quick detection, processing and reporting of safety issues and the management of these within the context of lack of complete information on the disease. Pharmacovigilance centres permanently monitor the safety profile of medicines, ensuring risk management to evaluate the benefit-risk relationship. However, traditional pharmacovigilance approaches of spontaneous reporting, are not suitable in the context of a pandemic; the scientific community and regulators need information on a near real-time point. The aim of this commentary is to suggest six interrelated multidimensional guiding axes for drug safety management by pharmacovigilance centres during the COVID-19 pandemic. This working plan can increase knowledge on COVID-19 and associated therapeutic approaches, support decisions by the regulatory authorities, oppose fake news and promote more efficient public health protection.
Similar content being viewed by others
Impacts on practice
-
Pharmacovigilance centres have to adapt their organisation and workflow to the needs of the COVID-19 pandemic.
-
Implementation of active pharmacovigilance approaches contributes to better coverage of pharmacoepidemiologic surveillance of COVID-19 drugs.
-
Effective communication strategies on drug safety promote greater awareness for the reporting of suspected adverse reactions related to COVID-19 vaccines and other drugs.
-
There is a need for pharmacovigilance centres to better link drug safety data with actual effectiveness in clinical practice.
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified in late December 2019 in Wuhan, China and is responsible for the COVID-19 disease. The COVID-19 pandemic is already one of the most disruptive events in modern history, affecting public health on a truly global scale. If the challenges arise in multiple research lines, those related to the prophylaxis and/or treatment of this disease are critical. Moreover, regardless of the therapeutic approaches that may be approved, active monitoring of drug safety needs to be prioritised [1].
Therapeutic approaches against SARS-CoV-2 and patient safety
Until now, several therapeutic approaches are under study in multiple countries to prevent and/or treat the infection by SARS-CoV-2 and the associated complications. The most used approach has been investigating drugs already marketed with approved indications for other diseases – "drug repurposing" [2], to bypass the limiting factor in the process of drug development: time. Particular attention has been given to drugs used in the field of antiviral therapies [3, 4], to reduce the replicating and infectious capacity of SARS-CoV-2 and to immunomodulatory therapies [5, 6], to limit the exacerbated inflammatory response of the immune system to SARS-CoV-2 infection. For now, only remdesivir and dexamethasone have been approved for the treatment of COVID-19 patients. Simultaneously, there has been an unprecedented effort to develop an effective vaccine to reduce the risk of infection and severe disease. Until the end of April 2021, four COVID-19 vaccines have been approved, which trigger the expression of the S protein of the SARS-CoV-2, thus prompting an immune response. Among the different possible approaches, the mRNA and viral vector vaccines have been extensively investigated in COVID-19.
Challenges for drug safety in the COVID-19 pandemic
Regardless of the therapeutic approach used to treat COVID-19 patients, one cannot afford to lose sight of the importance of patient safety. For that, the pharmacovigilance system, through its centres and experts, is of utmost relevance. Although the role of pharmacovigilance remains primarily focused on monitoring adverse drug reactions (ADRs), other medicine-related problems are also relevant, as (in)efficacy, so that the potential risk of a therapeutic approach should be weighted at the time of clinical decision.
Several studies have described some adverse drug events (i.e., without attributed direct causality) associated with the therapeutic approaches referred above [7, 8]. Despite this, very few studies were conducted in COVID-19 patients, which limits the generalization of results in this particular population. Also, in the last few months, large-scale vaccination programs have been implemented, raising the surveillance of vaccine safety and effectiveness to the highest priority. In Europe, the European Medicines Agency (EMA) and the European Centre for Disease Prevention and Control (ECDC) recently kicked off a new initiative aimed at strengthening post-marketing monitoring of the safety, effectiveness and impact of COVID-19 vaccines in the European Union and the European Economic Area [9]. The Center for Biologics Evaluation and Research at the Food and Drug Administration (FDA) also monitors the safety of authorised COVID-19 vaccines through both passive and active safety surveillance systems [10]. Of the therapeutic approaches approved for COVID-19, all except dexamethasone are under the scope of additional monitoring (Table 1), a concept introduced in the pharmacovigilance legislation in 2010 to identify medicines for which clinical evidence is less well established.
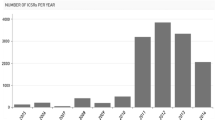
The COVID-19 pandemic presents some unusual challenges to the pharmacovigilance centres. For instance, it is quite complex to manage drug safety issues, even for drugs already in use, when we are faced with a new clinical indication for which there is very little information. In parallel, the pandemic nature of the disease demands for quick responses, which implies fast-tracking of detection, processing and reporting of safety issues to the EMA. This need for fast-tracking is a particular issue since pharmacovigilance centres are under-resourced for the massive increase in reports (particularly related to COVID-19 vaccines), leading to an overburden of pharmacovigilance professionals. Moreover, this overall situation associated with the COVID-19 pandemic has also seen a steep rise in misinformation and fake news. The rapid spread of misinformation about the safety of vaccines and other COVID-19 therapies has a serious impact on adherence to the population's therapeutic plans, compromising, for example, the achievement of group immunity. Through its methodological rigour, pharmacovigilance must know how to combat this parallel problem through the best scientific evidence available at any given moment.
These challenges pushed pharmacovigilance centres to adapt and reorganise in order to implement strategies to magnify the information available about the efficacy and ADRs of approaches used to prevent/treat COVID-19 and to come up with prompt answers to the needs of this public health issue. Also, the exponential increase in ADRs (as a result of the large-scale use of new drugs or drug repurposing strategies) supports the need for prioritising the activity of pharmacovigilance centres. In addition, it is essential to work on risk communication since the usefulness of all our pharmacovigilance efforts will manifest in our ability to communicate practical advice for the safe use of medicines. Overall, the information gathered from pharmacovigilance on COVID-19 will contribute to opposing fake news. Indeed, by using the most recent evidence available from studies from real-world data with methodological robustness and scrutinised by peer review, pharmacovigilance reports to provide relevant support for health authorities.
Guiding axes for drug safety management during the COVID-19 pandemic
In view of the earlier narrative, we propose six guiding axes to support the urgent response of pharmacovigilance centres (Fig. 1):
1. Active drug monitoring programs
The most common pharmacovigilance approaches are passive and largely spontaneous in nature. However, during situations requiring a fast-track of detection, processing and reporting of safety issues – like the COVID-19 pandemic, robust and responsive active drug monitoring pharmacovigilance programs are crucial to collect data on suspected drug incidents in near real-time. Active monitoring program approaches include collecting ADRs by direct contact with health professionals (e.g. scheduled visits and regular call meetings), adapting reporting systems to the needs of the institutions and respective units/services (e.g. simplified forms, adapted reporting flowchart and consensus meetings) [11] and engage social media as a potential promoter of patient reporting [12]. These active monitoring programs must transcend the different health services (e.g., pharmacies, nursing homes, family healthcare centres and, above all, hospitals) in order to increase the probability of detecting suspected drug incidents and accelerate the assessment of causality (or attribution of a degree of probability) of the events reported in COVID-19 patients. Also, the regional centres must be capable of comprehensive coverage of the region under their tutelage. For that, reinforcing human resources might be needed in order to overcome work overload and delayed response.
2. Intensive monitoring in special populations
Clinical trials prior to licensing collect and report information on ADRs but often include selected individuals. It is only after licencing that data will be gathered from more extensive and diverse populations. Certain vulnerable groups, e.g. those with increased age, high-risk comorbidities (renal and hepatic impaired, immunocompromised), pregnancy (including gestational age) or paediatrics, are usually not included in clinical trials. Also, high-risk patients are frequently on polypharmacy, which increases the risk for drug interactions. As so, the correlation of data from the pharmacotherapeutic profile of each patient can also contribute to understanding the relationship between the pre-infection pharmacotherapeutic profile and the course/prognostic of the disease and ADRs of therapeutic approaches. For this, the use of previously stored data in electronic clinical records (retrospective approach) must be crossed with clinical and ADRs data reported in real-time (real-time observational studies - prospective approach). However, during the COVID-19 pandemic, the rate of infection and associated complications requiring pharmacological treatment were markedly high in older people with multiple morbidities and polypharmacy. In situations such as the present COVID-19 pandemic, monitoring should be reinforced in special populations that are found to be more vulnerable either to the disease or the needed therapeutic approaches. This can be accomplished by following cohorts of patients at the regional levels or in collaborative models (at the national or international level) to monitor potential ADRs [13]. Prospective cohort observational studies can be a methodology to be adopted by pharmacovigilance centres. The goal is to follow over time a group of similar individuals (cohorts) who differ concerning certain factors under study to determine how these factors affect rates of a particular outcome. Intensifying monitoring in populations known to be at increased risk of infection by SARS-Cov-2 and/or associated complications due to the COVID-19 disease or treatment can help to assist the management of drug safety issues, by promptly supporting clinical decisions.
3. Electronic reporting
Electronic or paperless reporting tools are the most effective reporting method [14, 15], particularly in a highly dynamic public health context, like the COVID-19 pandemic, which required data to be gathered and reported quickly and efficiently. Multiple strategies can be adopted in this field, involving the information systems of the healthcare institutions. Examples of such electronic interventions include integrating electronic pharmacovigilance systems into hospital information systems -using Internet-based reporting systems -and using desktop applications to improve access to reporting tools. However, these systems also present barriers in their use, such as access to the Internet, problems related to the system's design and usability and challenges linked to the hybrid system of reporting [16]. Thus, institutions need a multidisciplinary approach to implement these interventions as quickly as the pandemic requires. Overall, electronic reporting is of valuable help to accelerate detection, processing and reporting of safety issues during the COVID-19 pandemic.
4. Integrative ADRs system
An integrative system for submitting ADRs related only to COVID-19 would foster knowledge on the topic. Each pharmacovigilance centre must effectively centralise all suspected ADRs and filter those coming from COVID-19 patients, bringing together the efforts of pharmacovigilance experts dedicated to COVID-19. Also, medical data from several sources, such as claims and clinical health records, has become common in providing rich insights on supporting ADRs investigation [15]. These systems must incorporate artificial intelligence tools to find and predict ADRs in large databases [17]. The use of the Bayesian network may be an option in countries with weak pharmacovigilance systems supporting imputation of causality [18].
5. Awareness campaigns
Major awareness campaigns on the importance of reporting all suspected ADRs should be launched [19]. These campaigns should bring together all community partners, namely health and social institutions, health professionals, pharmacovigilance delegates, patient organisations and local and national media, fostering a joint and targeted strategy under the best available evidence. These campaigns should mainly be aimed at patients vaccinated or diagnosed with COVID-19 and under treatment, with broad involvement of health professionals. An example of such is the campaigns directed to nurses to promote ADRs in vaccination centres set up on a large scale worldwide.
6. Effective communication
Some authors have been warning about the massive dissemination of information about the COVID-19 - an "infodemic" - that was mainly diffused through social media and sometimes included sensational and distorted information about different drugs [20]. Through the best evidence generated in the pharmacovigilance systems of each country, health authorities must be able to oppose, in an informed and transparent way, fake news. In this context, the permanent engagement of pharmacovigilance delegates from healthcare services is crucial for disseminating the pharmacovigilance system and for the active and close promotion of spontaneous report of adverse events. In addition, communication channels should be firmly established with other health professionals, patients, hospital managers and health, academic and scientific institutions.
In summary, spontaneous reporting remains the cornerstone of pharmacovigilance, but the effectiveness of active pharmacovigilance depends on the specific methods adopted and the work patterns put into place. However, spontaneous reporting is a slow approach that does not promptly answer the needs of situations like the present COVID-19 pandemic, in which the scientific community and regulators need information on a near real-time point. As so, we advocate a multidimensional strategy that, together with the traditional pharmacovigilance methods, can promote active pharmacovigilance [12] and accelerate the process while optimising resources. This multidimensional strategy embraces six interrelated guiding axes.
References
Sun J, Deng X, Chen X, Huang J, Huang S, Li Y, et al. Incidence of Adverse Drug Reactions in COVID-19 Patients in China: An Active Monitoring Study by Hospital Pharmacovigilance System. Clin Pharmacol Ther. 2020;108(4):791–7. https://doi.org/10.1002/cpt.1866.
Senanayake SL. Drug repurposing strategies for COVID-19. Future Drug Discov. 2020;2(2). doi: https://doi.org/10.4155/fdd-2020-0010.
Cao B, Wang Y, Wen D, Liu W, Wang J, Fan G, et al. A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N Engl J Med. 2020;382(19):1787–99. https://doi.org/10.1056/NEJMoa2001282.
Hung IF, Lung KC, Tso EY, Liu R, Chung TW, Chu MY, et al. Triple combination of interferon beta-1b, lopinavir-ritonavir and ribavirin in the treatment of patients admitted to hospital with COVID-19: an open-label, randomised, phase 2 trial. Lancet. 2020;395(10238):1695–704. https://doi.org/10.1016/s0140-6736(20)31042-4.
Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med. 2020;46(5):854–87. https://doi.org/10.1007/s00134-020-06022-5.
Low-Cost Dexamethasone Reduces Death By Up To One Third In Hospitalised Patients With Severe Respiratory Complications Of COVID-19 - RECOVERY Trial. https://www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19 (2020). Accessed February 20 2021.
Gatti M, Fusaroli M, Caraceni P, Poluzzi E, De Ponti F, Raschi E. Serious adverse events with tocilizumab: Pharmacovigilance as an aid to prioritize monitoring in COVID-19. Br J Clin Pharmacol. 2021;87(3):1533–40. https://doi.org/10.1111/bcp.14459.
Sato K, Mano T, Iwata A, Toda T. Neuropsychiatric adverse events of chloroquine: a real-world pharmacovigilance study using the FDA Adverse Event Reporting System (FAERS) database. Biosci Trends. 2020;14(2):139–43. https://doi.org/10.5582/bst.2020.03082.
Agency EM: EMA and ECDC join forces for enhanced post-marketing monitoring of COVID-19 vaccines in Europe. https://www.ema.europa.eu/en/news/ema-ecdc-join-forces-enhanced-post-marketing-monitoring-covid-19-vaccines-europe (2021). Accessed April 30 2021.
Food and Drug Administration US: COVID-19 Vaccine Safety Surveillance. https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/covid-19-vaccine-safety-surveillance (2021). Accessed April 30 2021.
Ferreira-da-Silva R, Ribeiro-Vaz I, Morato M, Silva AM, Junqueira PJ. The Role of Pharmacovigilance in the COVID-19 Pandemic. Acta Med Port. 2021;34(13):173–5. https://doi.org/10.20344/amp.15375.
Inácio P, Cavaco A, Airaksinen M. Current trends in pharmacovigilance: value and gaps of patient reporting. Int J Clin Pharm. 2018;40(4):754–7. https://doi.org/10.1007/s11096-018-0689-6.
(VAC4EU) VmCfE: Cohort Event Monitoring of safety of COVID-19 vaccines (EUPAS39798). http://www.encepp.eu/encepp/viewResource.htm?id=40288 (2021). Accessed May 24 2021.
Pontes H, Clément M, Rollason V. Safety signal detection: the relevance of literature review. Drug Saf. 2014;37(7):471–9. https://doi.org/10.1007/s40264-014-0180-9.
Meyboom RH, Egberts AC, Edwards IR, Hekster YA, de Koning FH, Gribnau FW. Principles of signal detection in pharmacovigilance. Drug Saf. 1997;16(6):355–65. https://doi.org/10.2165/00002018-199716060-00002.
Agoro OO, Kibira SW, Freeman JV, Fraser HSF. Barriers to the success of an electronic pharmacovigilance reporting system in Kenya: an evaluation three years post implementation. J Am Med Inform Assoc. 2017;25(6):627–34. https://doi.org/10.1093/jamia/ocx102.
Jensen PB, Jensen LJ, Brunak S. Mining electronic health records: towards better research applications and clinical care. Nat Rev Genet. 2012;13(6):395–405. https://doi.org/10.1038/nrg3208.
Rodrigues PP, Ferreira-Santos D, Silva A, Polonia J, Ribeiro-Vaz I. Causality assessment of adverse drug reaction reports using an expert-defined Bayesian network. Artif Intell Med. 2018;91:12–22. https://doi.org/10.1016/j.artmed.2018.07.005.
Chinchilla K, Matos C, Hall V, van Hunsel F. Patient Organizations’ Barriers in Pharmacovigilance and Strategies to Stimulate Their Participation. Drug Saf. 2021;44(2):181–91. https://doi.org/10.1007/s40264-020-00999-0.
Tuccori M, Convertino I, Ferraro S, Cappello E, Valdiserra G, Focosi D, et al. The Impact of the COVID-19 “Infodemic” on Drug-Utilization Behaviors: Implications for Pharmacovigilance. Drug Saf. 2020;43(8):699–709. https://doi.org/10.1007/s40264-020-00965-w.
Agency EM: List of medicines under additional monitoring. https://www.ema.europa.eu/en/documents/additional-monitoring/list-medicinal-products-under-additional-monitoring_en-0.pdf (2021). Accessed May 23 2021.
Funding
This commentary was supported by the PhD scholarship 2020.10231.BD (DOCTORATES 4 COVID-19), funded by Portuguese national funds and Community funds from the European Social Fund (ESF) through FCT – Fundação para a Ciência e a Tecnologia (Portugal).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferreira-da-Silva, R., Ribeiro-Vaz, I., Morato, M. et al. Guiding axes for drug safety management of pharmacovigilance centres during the COVID-19 era. Int J Clin Pharm 43, 1133–1138 (2021). https://doi.org/10.1007/s11096-021-01289-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-021-01289-0