Abstract
Background
Dose modification of renally secreted drugs in patients with chronic kidney disease (CKD) has relied on serum creatinine concentration as a biomarker to estimate glomerular filtration (GFR) under the assumption that filtration and secretion decline in parallel. A discrepancy between actual renal clearance and predicted renal clearance based on GFR alone is observed in severe CKD patients with tenofovir, a compound secreted by renal OAT1/3. Uremic solutes that inhibit OAT1/3 may play a role in this divergence.
Methods
To examine the impact of transporter inhibition by uremic solutes on tenofovir renal clearance, we determined the inhibitory potential of uremic solutes hippuric acid, indoxyl sulfate, and p-cresol sulfate. The inhibition parameters (IC50) were incorporated into a previously validated mechanistic kidney model; simulated renal clearance and plasma PK profile were compared to data from clinical studies.
Results
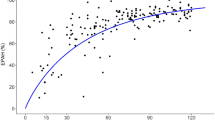
Without the incorporation of uremic solute inhibition, the PBPK model failed to capture the observed data with an absolute average fold error (AAFE) > 2. However, when the inhibition of renal uptake transporters and uptake transporters in the slow distribution tissues were included, the AAFE value was within the pre-defined twofold model acceptance criterion, demonstrating successful model extrapolation to CKD patients.
Conclusion
A PBPK model that incorporates inhibition by uremic solutes has potential to better predict renal clearance and systemic disposition of secreted drugs in patients with CKD. Ongoing research is warranted to determine if the model can be expanded to include other OAT1/3 substrate drugs and to evaluate how these findings can be translated to clinical guidance for drug selection and dose optimization in patients with CKD.




Similar content being viewed by others
Data Availability
The datasets and models generated during the current study have not been deposited into a publicly available database but are available from the corresponding author on reasonable request.
References
Cantu TG, Ellerbeck EF, Yun SW, Castine SD, Kornhauser DM. Drug prescribing for patients with changing renal function. Am J Hosp Pharm. 1992;49(12):2944–8.
Hu KT, Matayoshi A, Stevenson FT. Calculation of the estimated creatinine clearance in avoiding drug dosing errors in the older patient. Am J Med Sci. 2001;322(3):133–6.
Long CL, Raebel MA, Price DW, Magid DJ. Compliance with dosing guidelines in patients with chronic kidney disease. Ann Pharmacother. 2004;38(5):853–8. https://doi.org/10.1345/aph.1D399.
Papaioannou A, Clarke JA, Campbell G, Bedard M. Assessment of adherence to renal dosing guidelines in long-term care facilities. J Am Geriatr Soc. 2000;48(11):1470–3.
Pillans PI, Landsberg PG, Fleming AM, Fanning M, Sturtevant JM. Evaluation of dosage adjustment in patients with renal impairment. Intern Med J. 2003;33(1–2):10–3.
Sheen SS, Choi JE, Park RW, Kim EY, Lee YH, Kang UG. Overdose rate of drugs requiring renal dose adjustment: data analysis of 4 years prescriptions at a tertiary teaching hospital. J Gen Intern Med. 2008;23(4):423–8. https://doi.org/10.1007/s11606-007-0336-8.
Wong NA, Jones HW. An analysis of discharge drug prescribing amongst elderly patients with renal impairment. Postgrad Med J. 1998;74(873):420–2.
Yap C, Dunham D, Thompson J, Baker D. Medication dosing errors for patients with renal insufficiency in ambulatory care. Jt Comm J Qual Patient Saf. 2005;31(9):514–21.
Leendertse AJ, van Dijk EA, De Smet PA, Egberts TC, van den Bemt PM. Contribution of renal impairment to potentially preventable medication-related hospital admissions. Ann Pharmacother. 2012;46(5):625–33. https://doi.org/10.1345/aph.1Q633.
Bricker NS, Morrin PA, Kime Jr SW. The pathologic physiology of chronic Bright's disease. An exposition of the "intact nephron hypothesis". Am J Med. 1960;28:77-98. https://doi.org/10.1016/0002-9343(60)90225-4.
Petitpierre B, Perrin L, Rudhardt M, Herrera A, Fabre J. Behaviour of chlorpropamide in renal insufficiency and under the effect of associated drug therapy. Int J Clin Pharmacol Ther Toxicol. 1972;6(2):120–4.
Suchy-Dicey AM, Laha T, Hoofnagle A, Newitt R, Sirich TL, Meyer TW, et al. Tubular secretion in CKD. J Am Soc Nephrol. 2016;27(7):2148–55. https://doi.org/10.1681/ASN.2014121193.
Vallon V, Thomson SC. The tubular hypothesis of nephron filtration and diabetic kidney disease. Nat Rev Nephrol. 2020;16(6):317–36. https://doi.org/10.1038/s41581-020-0256-y.
Thomson SC, Blantz RC. Glomerulotubular balance, tubuloglomerular feedback, and salt homeostasis. J Am Soc Nephrol. 2008;19(12):2272–5. https://doi.org/10.1681/ASN.2007121326.
Kurokawa K. Tubuloglomerular feedback: its physiological and pathophysiological significance. Kidney Int Suppl. 1998;67:S71–4. https://doi.org/10.1046/j.1523-1755.1998.06714.x.
Kearney BP, Yale K, Shah J, Zhong L, Flaherty JF. Pharmacokinetics and dosing recommendations of tenofovir disoproxil fumarate in hepatic or renal impairment. Clin Pharmacokinet. 2006;45(11):1115–24. https://doi.org/10.2165/00003088-200645110-00005.
Chapron A, Shen DD, Kestenbaum BR, Robinson-Cohen C, Himmelfarb J, Yeung CK. Does Secretory Clearance Follow Glomerular Filtration Rate in Chronic Kidney Diseases? Reconsidering the Intact Nephron Hypothesis. Clin Transl Sci. 2017;10(5):395–403. https://doi.org/10.1111/cts.12481.
Kohler JJ, Hosseini SH, Green E, Abuin A, Ludaway T, Russ R, et al. Tenofovir renal proximal tubular toxicity is regulated by OAT1 and MRP4 transporters. Lab Invest. 2011;91(6):852–8. https://doi.org/10.1038/labinvest.2011.48.
Nagle MA, Truong DM, Dnyanmote AV, Ahn SY, Eraly SA, Wu W, et al. Analysis of three-dimensional systems for developing and mature kidneys clarifies the role of OAT1 and OAT3 in antiviral handling. J Biol Chem. 2011;286(1):243–51. https://doi.org/10.1074/jbc.M110.139949.
Hsueh CH, Yoshida K, Zhao P, Meyer TW, Zhang L, Huang SM, et al. Identification and Quantitative Assessment of Uremic Solutes as Inhibitors of Renal Organic Anion Transporters, OAT1 and OAT3. Mol Pharm. 2016;13(9):3130–40. https://doi.org/10.1021/acs.molpharmaceut.6b00332.
Duranton F, Cohen G, De Smet R, Rodriguez M, Jankowski J, Vanholder R, et al. Normal and pathologic concentrations of uremic toxins. J Am Soc Nephrol. 2012;23(7):1258–70. https://doi.org/10.1681/ASN.2011121175.
Mutsaers HA, van den Heuvel LP, Ringens LH, Dankers AC, Russel FG, Wetzels JF, et al. Uremic toxins inhibit transport by breast cancer resistance protein and multidrug resistance protein 4 at clinically relevant concentrations. PLoS One. 2011;6(4):e18438. https://doi.org/10.1371/journal.pone.0018438.
Huang W, Isoherranen N. Novel Mechanistic PBPK Model to Predict Renal Clearance in Varying Stages of CKD by Incorporating Tubular Adaptation and Dynamic Passive Reabsorption. CPT Pharmacometrics Syst Pharmacol. 2020;9(10):571–83. https://doi.org/10.1002/psp4.12553.
Imaoka T, Huang W, Shum S, Hailey DW, Chang SY, Chapron A, et al. Bridging the gap between in silico and in vivo by modeling opioid disposition in a kidney proximal tubule microphysiological system. Sci Rep. 2021;11(1):21356. https://doi.org/10.1038/s41598-021-00338-y.
Huang W, Isoherranen N. Development of a Dynamic Physiologically Based Mechanistic Kidney Model to Predict Renal Clearance. CPT Pharmacometrics Syst Pharmacol. 2018;7(9):593–602. https://doi.org/10.1002/psp4.12321.
Huang W, Czuba LC, Isoherranen N. Mechanistic PBPK Modeling of Urine pH Effect on Renal and Systemic Disposition of Methamphetamine and Amphetamine. J Pharmacol Exp Ther. 2020;373(3):488–501. https://doi.org/10.1124/jpet.120.264994.
Hsueh CH, Hsu V, Zhao P, Zhang L, Giacomini KM, Huang SM. PBPK Modeling of the Effect of Reduced Kidney Function on the Pharmacokinetics of Drugs Excreted Renally by Organic Anion Transporters. Clin Pharmacol Ther. 2018;103(3):485–92. https://doi.org/10.1002/cpt.750.
Ball K, Jamier T, Parmentier Y, Denizot C, Mallier A, Chenel M. Prediction of renal transporter-mediated drug-drug interactions for a drug which is an OAT substrate and inhibitor using PBPK modelling. Eur J Pharm Sci. 2017;106:122–32. https://doi.org/10.1016/j.ejps.2017.05.055.
Tan SPF, Scotcher D, Rostami-Hodjegan A, Galetin A. Effect of Chronic Kidney Disease on the Renal Secretion via Organic Anion Transporters 1/3: Implications for Physiologically-Based Pharmacokinetic Modeling and Dose Adjustment. Clin Pharmacol Ther. 2022;112(3):643–52. https://doi.org/10.1002/cpt.2642.
Duan H, Hu T, Foti RS, Pan Y, Swaan PW, Wang J. Potent and Selective Inhibition of Plasma Membrane Monoamine Transporter by HIV Protease Inhibitors. Drug Metab Dispos. 2015;43(11):1773–80. https://doi.org/10.1124/dmd.115.064824.
Yin J, Wagner DJ, Prasad B, Isoherranen N, Thummel KE, Wang J. Renal secretion of hydrochlorothiazide involves organic anion transporter 1/3, organic cation transporter 2, and multidrug and toxin extrusion protein 2-K. Am J Physiol Renal Physiol. 2019;317(4):F805–14. https://doi.org/10.1152/ajprenal.00141.2019.
Duan H, Wang J. Selective transport of monoamine neurotransmitters by human plasma membrane monoamine transporter and organic cation transporter 3. J Pharmacol Exp Ther. 2010;335(3):743–53. https://doi.org/10.1124/jpet.110.170142.
Uwai Y, Ida H, Tsuji Y, Katsura T, Inui K. Renal transport of adefovir, cidofovir, and tenofovir by SLC22A family members (hOAT1, hOAT3, and hOCT2). Pharm Res. 2007;24(4):811–5. https://doi.org/10.1007/s11095-006-9196-x.
Murphy RA, Valentovic MA. Factors Contributing to the Antiviral Effectiveness of Tenofovir. J Pharmacol Exp Ther. 2017;363(2):156–63. https://doi.org/10.1124/jpet.117.243139.
Brown RP, Delp MD, Lindstedt SL, Rhomberg LR, Beliles RP. Physiological parameter values for physiologically based pharmacokinetic models. Toxicol Ind Health. 1997;13(4):407–84. https://doi.org/10.1177/074823379701300401.
Di Mascio M, Srinivasula S, Bhattacharjee A, Cheng L, Martiniova L, Herscovitch P, et al. Antiretroviral tissue kinetics: in vivo imaging using positron emission tomography. Antimicrob Agents Chemother. 2009;53(10):4086–95. https://doi.org/10.1128/AAC.00419-09.
US prescribing information for VIREAD. 2012. https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/021356s042,022577s002lbl.pdf. Accessed May 2023.
Spinks CB, Zidan AS, Khan MA, Habib MJ, Faustino PJ. Pharmaceutical characterization of novel tenofovir liposomal formulations for enhanced oral drug delivery: in vitro pharmaceutics and Caco-2 permeability investigations. Clin Pharmacol. 2017;9:29–38. https://doi.org/10.2147/CPAA.S119875.
Lee WA, He GX, Eisenberg E, Cihlar T, Swaminathan S, Mulato A, et al. Selective intracellular activation of a novel prodrug of the human immunodeficiency virus reverse transcriptase inhibitor tenofovir leads to preferential distribution and accumulation in lymphatic tissue. Antimicrob Agents Chemother. 2005;49(5):1898–906. https://doi.org/10.1128/AAC.49.5.1898-1906.2005.
Liu SN, Desta Z, Gufford BT. Probenecid-Boosted Tenofovir: A Physiologically-Based Pharmacokinetic Model-Informed Strategy for On-Demand HIV Preexposure Prophylaxis. CPT Pharmacometrics Syst Pharmacol. 2020;9(1):40–7. https://doi.org/10.1002/psp4.12481.
Blank A, Eidam A, Haag M, Hohmann N, Burhenne J, Schwab M, et al. The NTCP-inhibitor Myrcludex B: Effects on Bile Acid Disposition and Tenofovir Pharmacokinetics. Clin Pharmacol Ther. 2018;103(2):341–8. https://doi.org/10.1002/cpt.744.
Deeks SG, Barditch-Crovo P, Lietman PS, Hwang F, Cundy KC, Rooney JF, et al. Safety, pharmacokinetics, and antiretroviral activity of intravenous 9-[2-(R)-(Phosphonomethoxy)propyl]adenine, a novel anti-human immunodeficiency virus (HIV) therapy, in HIV-infected adults. Antimicrob Agents Chemother. 1998;42(9):2380–4. https://doi.org/10.1128/AAC.42.9.2380.
Pradhan S, Duffull SB, Walker RJ, Wright DFB. The intact nephron hypothesis as a model for renal drug handling. Eur J Clin Pharmacol. 2019;75(2):147–56. https://doi.org/10.1007/s00228-018-2572-8.
Takita H, Scotcher D, Chinnadurai R, Kalra PA, Galetin A. Physiologically-Based Pharmacokinetic Modelling of Creatinine-Drug Interactions in the Chronic Kidney Disease Population. CPT Pharmacometrics Syst Pharmacol. 2020;9(12):695–706. https://doi.org/10.1002/psp4.12566.
Follman KE, Morris ME. Prediction of the Effects of Renal Impairment on Clearance for Organic Cation Drugs that Undergo Renal Secretion: A Simulation-Based Study. Drug Metab Dispos. 2018;46(5):758–69. https://doi.org/10.1124/dmd.117.079558.
Scotcher D, Jones CR, Galetin A, Rostami-Hodjegan A. Delineating the Role of Various Factors in Renal Disposition of Digoxin through Application of Physiologically Based Kidney Model to Renal Impairment Populations. J Pharmacol Exp Ther. 2017;360(3):484–95. https://doi.org/10.1124/jpet.116.237438.
Acknowledgements
CKY would like to gratefully acknowledge Dr. David E. Smith for his steady guidance, unwavering support, and good humor.
Funding
These studies were supported by funding from the National Institutes of Health National Institute of General Medical Sciences (NIGMS) R01GM121354, National Institute on Drug Abuse (NIDA) P01DA032507, and an unrestricted gift from the Northwest Kidney Centers to the Kidney Research Institute. A.C. and W.H. were recipients of the Warren G. Magnuson Scholarship at the University of Washington.
Author information
Authors and Affiliations
Contributions
SYC, AC, AL, JW, NI, DS, EK, JH, and CKY developed and designed the experiments, SYC, AC, and AL conducted the experiments and data analysis. WH and NI developed the PBPK model and performed simulations. All authors contributed to writing and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shih-Yu Chang and Weize Huang are co-first authors that contributed equally to the manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chang, SY., Huang, W., Chapron, A. et al. Incorporating Uremic Solute-mediated Inhibition of OAT1/3 Improves PBPK Prediction of Tenofovir Renal and Systemic Disposition in Patients with Severe Kidney Disease. Pharm Res 40, 2597–2606 (2023). https://doi.org/10.1007/s11095-023-03594-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-023-03594-x