Abstract
Purpose
To clarify the mechanism of renal impairment leading to different degrees of increased plasma exposure to dipeptidyl peptidase 4 inhibitor vildagliptin and its major metabolite, M20.7.
Methods
The 5/6 nephrectomized (5/6 Nx) rat model, to simulate chronic renal failure (CRF) patients, combined with kidney slices and transporter studies in vitro were used to assess this pharmacokinetic differences.
Results
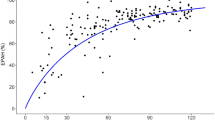
After intragastric administration to 5/6 Nx rats, vildagliptin showed increased plasma levels by 45.8%, and M20.7 by 7.51 times, which was similar to patients with severe renal impairment. The recovery rate of M20.7 in urine and feces increased by less than 20%, showing limited effect of renal impairment on vildagliptin metabolism. In vitro studies found M20.7 to be the substrate for organic anion transporter 3 (OAT3). However, the active uptake of M20.7 in renal slices showed no difference between the 5/6 Nx and normal rats. In OAT3 overexpressed cells, the protein-bound uremic toxins, 3-carboxy-4-methyl-5propyl-2-furanpropionate (CMPF), hippuric acid (HA) and indoxyl sulfate (IS), which accumulate in CRF patients, inhibited M20.7 uptake with IC50 values of 5.75, 29.0 and 69.5 μM respectively, far lower than plasma concentrations in CRF patients, and showed a mixed inhibition type.
Conclusions
The large increase in plasma exposure of M20.7 could be attributed to the accumulation of uremic toxins in CRF patients, which inhibited OAT3 activity and blocked renal excretion of M20.7, while vildagliptin, with high permeability, showed a slight increase in plasma exposure due to reduced glomerular filtration.












Similar content being viewed by others
References
Villhauer E. 1-[[(3-hydroxy-1-adamantyl) amino] acetyl]-2-cyano-(s)-pyrrolidine : a potent, selective, and orally bioavailable dipeptidyl peptidase iv inhibitor with antihyperglycemic properties. J Med Chem. 2003;46(13):2774–89.
Mentlein R. Dipeptidyl-peptidase iv (cd26)--role in the inactivation of regulatory peptides. Regul Pept. 1999;85(1):9–24. https://doi.org/10.1016/s0167-0115(99)00089-0.
Kreymann B, Williams G, Ghatei MA, Bloom SR. Glucagon-like peptide-1 7-36: a physiological incretin in man. Lancet. 1987;2(8571):1300–4. https://doi.org/10.1016/s0140-6736(87)91194-9.
He H, Tran P, Yin H, Smith H, Batard Y, Wang L, et al. Absorption, metabolism, and excretion of [14c]vildagliptin, a novel dipeptidyl peptidase 4 inhibitor, in humans. Drug Metab Dispos. 2009;37(3):536–44. https://doi.org/10.1124/dmd.108.023010.
Kong FD, Pang XY, Zhao JH, Deng P, Zheng MY, Zhong DF, et al. Hydrolytic metabolism of cyanopyrrolidine dpp-4 inhibitors mediated by dipeptidyl peptidases. Drug Metab Dispos. 2019;47(3):238–48. https://doi.org/10.1124/dmd.118.084640.
He Y. Clinical pharmacokinetics and pharmacodynamics of vildagliptin. Clin Pharmacokinet. 2012;51(3):147–62.
Scheen AJ. Pharmacokinetics of dipeptidylpeptidase-4 inhibitors. Diabetes Obes Metab. 2010;12(8):648–58. https://doi.org/10.1111/j.1463-1326.2010.01212.x.
Lukashevich V, Schweizer A, Shao Q, Groop PH, Kothny W. Safety and efficacy of vildagliptin versus placebo in patients with type 2 diabetes and moderate or severe renal impairment: a prospective 24-week randomized placebo-controlled trial. Diabetes Obes Metab. 2011;13(10):947–54. https://doi.org/10.1111/j.1463-1326.2011.01467.x.
Disease K. Improving global outcomes (kdigo) ckd work group. Kdigo 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Pol Arch Med Wewn. 2013;120(7–8):300–6.
Periclou A, Ventura D, Rao N, Abramowitz W. Pharmacokinetic study of memantine in healthy and renally impaired subjects. Clin Pharmacol Ther. 2006;79(1):134–43.
Asconapé JJ. Use of antiepileptic drugs in hepatic and renal disease. Handb Clin Neurol. 2014;119(119):417–32.
Zhong K, Li X, Xie C, Zhang Y, Zhong D, Chen X. Effects of renal impairment on the pharmacokinetics of morinidazole: uptake transporter-mediated renal clearance of the conjugated metabolites. Antimicrob Agents Chemother. 2014;58(7):4153–61. https://doi.org/10.1128/aac.02414-14.
Kong F, Pang X, Zhong K, Guo Z, Li X, Zhong D, et al. Increased plasma exposures of conjugated metabolites of morinidazole in renal failure patients: a critical role of uremic toxins. Drug Metab Dispos. 2017;45(6):593–603. https://doi.org/10.1124/dmd.116.074492.
Chu X, Bleasby K, Chan GH, et al. The complexities of interpreting reversible elevated serum creatinine levels in drug development: does a correlation with inhibition of renal transporters exist? Drug Metab Dispos. 2016;44(9):1498.
Vanholder R, De Smet R, Glorieux G, Argiles A, Baurmeister U, Brunet P, et al. Review on uremic toxins: classification, concentration, and interindividual variability. Kidney Int. 2003;63(5):1934–43. https://doi.org/10.1046/j.1523-1755.2003.00924.x.
Hsueh CH, Yoshida K, Zhao P, Meyer TW, Zhang L, Huang SM, et al. Identification and quantitative assessment of uremic solutes as inhibitors of renal organic anion transporters, oat1 and oat3. Mol Pharm. 2016;13(9):3130–40.
Kearney BP, Yale K, Shah J, Zhong L, Flaherty JF. Pharmacokinetics and dosing recommendations of tenofovir disoproxil fumarate in hepatic or renal impairment. Clin Pharmacokinet. 2006;45(11):1115–24.
Anderson S, Rennke HG, Brenner BM, Anderson S, Meyer TW, Rennke HG, et al. Control of glomerular hypertension limits glomerular injury in rats with reduced renal mass. J Clin Investig. 1985;76(2):612–9.
Kikuchi K, Itoh Y, Tateoka R, Ezawa A, Murakami K, Niwa T. Metabolomic analysis of uremic toxins by liquid chromatography/electrospray ionization-tandem mass spectrometry. J Chromatogr B Anal Technol Biomed Life Sci. 2010;878(20):1662–8.
Naud J, Michaud J, Beauchemin S, Hebert MJ, Roger M, Lefrancois S, et al. Effects of chronic renal failure on kidney drug transporters and cytochrome p450 in rats. Drug Metab Dispos. 2011;39(8):1363–9. https://doi.org/10.1124/dmd.111.039115.
Deguchi T, Nakamura M, Tsutsumi Y, Suenaga A, Otagiri M. Pharmacokinetics and tissue distribution of uraemic indoxyl sulphate in rats. Biopharm Drug Dispos. 2010;24(8):345–55.
Kaplan MM, Utiger RD. Iodothyronine metabolism in liver and kidney homogenates from hyperthyroid and hypothyroid rats. Endocrinology. 1978;103(1):156–61. https://doi.org/10.1210/endo-103-1-156.
Han YH, Busler D, Hong Y, Tian Y, Chen C, Rodrigues AD. Transporter studies with the 3-o-sulfate conjugate of 17alpha-ethinylestradiol: assessment of human kidney drug transporters. Drug Metab Dispos. 2010;38(7):1064–71. https://doi.org/10.1124/dmd.109.031526.
Obatomi DK, Brant S, Anthonypillai V, Early DA, Bach PH. Optimizing preincubation conditions for precision-cut rat kidney and liver tissue slices: effect of culture media and antioxidants. Toxicol in Vitro. 1998;12(6):725–37. https://doi.org/10.1016/S0887-2333(98)00055-1.
Keller F, Maiga M, Neumayer HH, Lode H, Distler A. Pharmacokinetic effects of altered plasma protein binding of drugs in renal disease. Eur J Drug Metab Pharmacokinet. 1984;9(3):275–82.
Reidenberg MM, Drayer DE. Alteration of drug-protein binding in renal disease. Clin Pharmacokinet. 1984;9(1 Supplement):18.
FDA. Guidance for industry pharmacokinetics in patients with impaired renal function – study design, data analysis, and impact on dosing, U.S. Department of health and human services food and drug administration center for drug evaluation and research (cder). 2020.
He YL, Kulmatycki K, Zhang YM, Zhou W, Reynolds C, Ligueros-Saylan M, et al. Pharmacokinetics of vildagliptin in patients with varying degrees of renal impairment. Int J Clin Pharmacol Ther. 2013;51(9):693–703. https://doi.org/10.5414/cp201885.
FDA. In vitro drug interaction studies —cytochrome p450 enzyme and transporter mediated drug interactions-guidance for industry. 2020.
Dixon M. The determination of enzyme inhibitor constants. Biochem J. 1953;55(1):170–1. https://doi.org/10.1042/bj0550170.
Cornish-Bowden A. A simple graphical method for determining the inhibition constants of mixed, uncompetitive and non-competitive inhibitors. Biochem J. 1974;137(1):143–4.
Ogilvie BW. Glucuronidation converts gemfibrozil to a potent, metabolism-dependent inhibitor of CYP2C8: implications for drug-drug interactions. Drug Metab Dispos. 2005;34(1):191–7.
Bailey MJ, Dickinson RG. Acyl glucuronide reactivity in perspective: biological consequences. Chem Biol Interact. 2003;145(2):117–37. https://doi.org/10.1016/s0009-2797(03)00020-6.
Acknowledgments
This study was supported by the National Natural Science Foundation of China (Grant 82073924). The authors thank Xiao-yan Pang for her assistance with the experiments.
Author information
Authors and Affiliations
Contributions
ZTG, FDK and XYC participated in research design; ZTG, FDK, NJX, ZDC and JFH performed experiments; ZTG and XYC wrote the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 355 kb)
Rights and permissions
About this article
Cite this article
Guo, Z., Kong, F., Xie, N. et al. Mechanistic Study on the Effect of Renal Impairment on the Pharmacokinetics of Vildagliptin and its Carboxylic Acid Metabolite. Pharm Res 39, 2147–2162 (2022). https://doi.org/10.1007/s11095-022-03324-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-022-03324-9