Abstract
Migraine is a poorly understood neurological disorder and a leading cause of disability in young adults, particularly women. Migraines are characterized by recurring episodes of severe pulsating unilateral headache and usually visual symptoms. Currently there is some disagreement in the electrophysiological literature regarding the universality of all migraineurs exhibiting physiological visual impairments also during interictal periods (i.e., the symptom free period between migraines). Thus, this meta-analysis investigated the evidence for altered visual function as measured electrophysiologically via pattern-reversal visual evoked potential (VEP) amplitudes and habituation in adult migraineurs with or without visual aura and controls in the interictal period. Twenty-three studies were selected for random effects meta-analysis which demonstrated slightly diminished VEP amplitudes in the early fast conducting P100 component but not in N135, and substantially reduced habituation in the P100 and the N135 in migraineurs with and without visual aura symptoms compared to controls. No statistical differences were found between migraineurs with and without aura, possibly due to inadequate studies. Overall, insufficient published data and substantial heterogeneity between studies was observed for all latency components of pattern-reversal VEP, highlighting the need for further electrophysiological experimentation and more targeted temporal analysis of visual function, in episodic migraineurs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is an underdiagnosed and inadequately managed condition (Lipton et al., 2013) characterised by periodic severe recurring headaches and neurological symptoms that cause extended periods of disability (International Headache Society [IHS], 2018). Migraine is also the second most prevalent neurological condition across the adult lifespan, and the most prevalent neurological condition in young working age adults (Stewart et al., 2008), and the sixth leading cause of disability worldwide (Vos et al., 2017). A typical migraine involves pulsating headaches with moderate to severe unilateral pain, and is often accompanied by nausea, vomiting, or sensitivity to light (photophobia) and sound (phonophobia; Goadsby et al., 2017; IHS, 2018). The International Classification of Headache Disorders 3rd edition (ICHD-3) categorises migraine as two primary disorders: migraine without aura (MO) and migraine with aura (MA), where aura is defined as sensory symptoms that are predominantly visual, arising shortly before or during a headache (IHS, 2018). The MA subtype is primarily characterised by more extreme visual symptoms, often including perception of zigzag patterns or scintillating scotoma (holes in vision) that gradually spread across the visual field (IHS, 2018). Previous behavioural work has observed that both magnocellular and parvocellular visual pathways can be impacted in migraineurs with prior visual impairment during the interictal period (McKendrick & Badcock, 2003). Thus, the present study aimed to meta-analyse the current electrophysiological literature associated with visual function in migraineurs to determine whether visual function is only perturbed during migraine, or more permanently altered during the interictal period (i.e., between migraine events) in episodic migraineurs.
Visual symptoms are among the core diagnostic criteria of migraine (IHS, 2018), yet the role of interictal visual abnormalities in migraine pathophysiology remains unclear. Vision is the primary spatial and temporal information processing modality of the primate brain (Felleman & Van Essen, 1991; Livingstone & Hubel, 1987) driving attention, cognition, and goal-directed actions in humans (Corbetta & Shulman, 2002; Crewther et al., 2012; Laycock et al., 2007). Visual processing and eye movements also occupy large proportions of cortical (Felleman & Van Essen, 1991) and subcortical volume (Wurtz & Goldberg, 1971) and require the greatest proportion of the brain’s metabolic resources (Wong-Riley, 2010). Two interconnected theories that describe possible visual processing anomalies in migraineurs during the interictal period relate to visual system (i) excitability and (ii) habituation to repetitive stimulation (Magis et al., 2013), as briefly outlined in the following paragraphs.
Although heightened sensitivity to visual stimulation is predominantly experienced during a migraine episode, this has also been observed in some migraineurs during the interictal period (Peroutka, 2014; Shepherd, 2019), leading to the hypothesis that the visual system in migraineurs is abnormally sensitive or hyperexcitable to visual stimulation both during and outside of a migraine event (Aurora & Wilkinson, 2007). Vecchia and Pietrobon (2012) have further suggested that hyperexcitability and imbalances in visual cortex excitatory and inhibitory mechanisms contribute to susceptibility to cortical spreading depression (CSD) in MA. Brigo et al. (2013) meta-analysed transcranial magnetic stimulation (TMS) studies examining cortical arousal levels in interictal migraineurs and identified that primary visual cortex (V1) was hyperexcitable in MA but not MO, providing some support for the theory that vision is impacted in some migraineurs interictally. However, while meta-analyses are available summarising TMS in migraine populations, no current attempts have been made to systematically summarise other physiological studies relating to visual system function during the interictal period, such as visually evoked potentials (VEPs) recorded using electroencephalography (EEG). Indeed, the frequency of visual anomalies in migraine and their effects on baseline function and cortical excitability make this information extremely important to understanding migraine pathophysiology. Moreover, the high temporal and reasonable spatial resolution of the VEP technique allows objective quantification of the effects of cortical excitability in susceptibility to migraine (Magis et al., 2013).
To date there has been little consistency across studies analysing VEP component amplitudes and latencies in migraineurs during the interictal period, particularly for studies (Ambrosini et al., 2003). To address this inconsistency, Odom et al. (2016) initiated the use of clinical methodology of The International Society for Clinical Electrophysiology on Vision that states that between-participant variability in VEPs may be minimised by using black-and-white checkerboard pattern-reversal stimulus that reverses at a transient rate (approximately three or less reversals per second) whilst recording responses from an occipital electrode above V1. The majority of studies available using a checkerboard pattern-reversal VEP methodology in migraine populations have reported the P100 and N135 time point components (Coppola et al., 2019) based on the Baseler et al. (1994) and Klistorner et al. (1997) temporal analysis of the human multifocal flash VEP (mfVEP) that facilitates dissociation of separate magnocellular (P100-N115) and parvocellular (N100-P120-N160) contributions to V1. Thus, pattern-reversal VEP P100 may describe magnocellular contribution and N135 parvocellular, albeit less accurately than mfVEP.
Existing VEP studies of interictal migraineurs yield inconsistent results, with different authors identifying greater responses (hyperexcitability), diminished responses (hypo-excitability) and even normal responses when compared to non-migraineurs (Magis et al., 2016; Tolner et al., 2019). Furthermore, the role of methodological and confounding factors on electrophysiological response in migraineurs is poorly understood, such as time in the migraine cycle (Coppola & Schoenen, 2012; Schoenen, 2011; Stankewitz & May, 2009), preventative medications (Magis et al., 2013), participant age (Brown et al., 2019) and VEP stimulus size and optimal speed of stimulus reversal (Odom et al., 2016). Factors such as VEP stimuli and time of assessment with reference to the migraine cycle and time point during the interictal period varies significantly across previous studies (Ambrosini et al., 2003; Magis et al., 2007). A review by Magis et al. (2016) discussed findings across all visual electrophysiology methods in migraine post-2013, but only reported significant results and did not describe how studies were selected for review. Finally, a very recent review by de Tommaso (2019) summarised spectral analysis EEG and steady-state VEPs in migraine, but not transient VEPs as a means of understanding the impact of migraine on speed of visual processing. Thus, the literature remains highly controversial with conflicting evidence and inconsistent methodologies used to analyse VEPs in interictal migraineurs.
Electrophysiological function in migraineurs has also been associated with abnormal responses to prolonged stimulation and habituation mechanisms across visual, auditory, somatosensory, and nociceptive evoked potentials (Brighina et al., 2009; Magis et al., 2013). Habituation in VEP studies refers to a progressive decline in response amplitude across prolonged stimulation (Omland et al., 2011), and is often interpreted as the reduction in attention required to respond to a non-changing stimulus (McDiarmid et al., 2017). Abnormal habituation in migraine has also been linked to abnormal cortical excitability and vulnerability to sensory overload, possibly due to repeated exposure to pain/stress activation caused by migraine symptoms (Stankewitz & May, 2009). Repeated cortical inflammation and pain activation associated with frequent migraines may also alter the cortical resting state over time, causing abnormal electrophysiological responses in interictal migraineurs (Kowacs et al., 2015). If so, more frequent migraines and greater time between onset of recurring migraines could moderate VEP habituation, amplitudes, and latencies (Nguyen et al., 2012). However, habituation deficits in interictal periods are not consistently identified in migraineurs, possibly due to participant or methodological differences across studies (de Tommaso et al., 2014). Potentially the most important factor affecting VEP habituation patterns is the stage of the migraine cycle at which recordings are obtained (Coppola & Schoenen, 2012). As such, inconsistent findings across studies raises questions as to whether reduced habituation is a useful measure to understand the cortical and visual contributions to migraine aetiology, vulnerability, or treatments during the quiescent interictal period.
Thus, the present study aimed to examine visual processing in migraineurs during the interictal period by conducting a meta-analysis on case–control studies that have compared VEP responsivity and habituation in adult migraineurs and non-migraine controls. The foci of the meta-analysis were the traditional P100 and N135 timepoints measured using checkerboard pattern-reversal VEP stimuli, which are the most commonly available results. It was hypothesised that meta-analyses would demonstrate changes in early VEP amplitude and decreased habituation (i.e., smaller response decrement to prolonged stimulation) in individuals diagnosed with migraine compared to non-migraine controls. Our secondary aims were to examine differences between MA and MO subtypes and, where possible, explore potential confounds of VEPs in migraine including: Age, migraine frequency, years suffering migraines, and VEP stimulus check size and reversal rate.
Method
Search Strategy
This study was pre-registered with Open Science Framework on May 25th, 2020 (registration https://doi.org/10.17605/OSF.IO/VHWEP). Searches of MEDLINE, Embase, PubMed and Web of Science, PsycINFO and CINAHL databases were conducted for peer-reviewed studies written in the English language with no date restrictions published up to June 29th, 2021. Title and abstract search terms were: 1) "migraine" OR "migraine aura" OR "migraine headache" OR "headache disorder"; and 2) "VEP" OR "visual* evoked potential*" OR "VER" OR "visual* evoked response*" OR "functional vision"; and 3) "EEG" OR "electroencephalogra*", incorporating Medical Subject Headings (MeSH) where possible. Reference lists of extracted studies were also manually searched. Results were imported into Covidence Systematic Review Software ("Covidence"; Veritas Health Innovation, 2019).
Study Selection Criteria
Primary inclusion criteria were case–control studies with a between-groups design comprising adults (18–60 years of age) with migraine and non-migraine controls of similar age and gender distributions being compared in VEPs recorded with EEG. Studies primarily used the ICHD (IHS, 2018) to diagnose migraineurs with “migraine without aura” (MO) or “migraine with aura” (MA). Non-migraine headache disorders (e.g. tension-type headache) were excluded. Included studies required a healthy control group without migraine or headache history and screening participants for neurological disorders with abnormal electrophysiological responses (e.g. epilepsy) that could confound VEPs (Vialatte et al., 2010). Adult migraineurs aged 18–60 were selected to reduce age-related confounds on VEPs, as previous research suggests VEP amplitudes and latencies decrease across the lifespan (Brown et al., 2019). Age ranges were requested from authors if missing from articles. Studies were excluded if one standard deviation of the mean age lay outside 18–60. Included studies explicitly tested interictal migraineurs free from migraine symptoms for at least 48 h before and after testing. Studies where migraineurs used preventative medication during testing were excluded as this can impact VEPs (Coppola et al., 2009) (Fig. 1).
Methodological inclusion criteria were that VEPs were recorded using EEG according to international standards (Odom et al., 2016). The International Society for Clinical Electrophysiology on Vision states that VEPs require an active electrode on the occipital scalp (“Oz”) for recording the visual cortex in line with the 10–20 international system (Odom et al., 2016). Inclusion was limited to studies using checkerboard pattern-reversal VEP stimuli due to insufficient studies available using pattern onset/offset or flash stimulation or multifocal stimuli. Only transient VEPs were included within the scope of this meta-analysis. Steady-state VEPs and EEG spectral analysis were excluded but may answer future questions related to underlying brain activity in migraine (Vialatte et al., 2010). Thus, included studies assessed the main components of the transient pattern-reversal VEP waveform with amplitude, latency, and habituation (change in baseline wave amplitudes across testing) as outcome measures. Baseline data was obtained where studies recorded VEPs on multiple occasions and studies were excluded if baseline values were unobtainable. See Fig. 2 PRISMA flow chart for exclusion criteria and frequency.
Data Collection/Extraction
Data collection methodologies were based on and adhered to the Cochrane Handbook (2019) guidelines (Higgins et al., 2020). After TS, NR and VN independently screened abstracts, two independent reviewers (TS and VN) blindly extracted data from articles and resolved discrepancies with SC to create a single Microsoft Excel extraction spreadsheet for the variables summarised in Table 1. In line with Cochrane (Higgins et al., 2020), detailed scrutiny of confounds in screening phases led to a highly reliable data extraction consensus (Kappa = 0.80) (Table 2).
Where possible, data for MO and MA groups was extracted separately from each study. When migraine subsamples were not specified (i.e., not listed as samples of migraineurs with or without aura) or contained both MO and MA, data was extracted under a Migraine Grouped (MG) variable. Demographics were extracted for each sample to check eligibility and to ensure subsamples were comparable. Migraine characteristics and stimulus details were extracted as potential moderators. Outcome variables extracted were VEP amplitudes and habituation for the P100 and N135 components. As depicted in Fig. 1 below, P100 was defined as the positive peak occurring approximately 100 ms post-stimulus onset and N135 was defined as the second negative peak occurring between 120-150 ms post-onset (Odom et al., 2016).
Typical Transient Pattern-Reversal Visual Evoked Potential Waveform. Note. μV = microvolts, ms = milliseconds. Adapted from “ISCEV standard for clinical visual evoked potentials: (2016 update)” by Odom et al. (2016), Documenta Ophthalmologica, 133(1), p. 7 (https://doi.org/10.1007/s10633-016-9553-y)
Depending on data available, VEP amplitudes were extracted as either first block average or grand average across all blocks of testing. Habituation was reported in the following ways in the included studies: Percentage amplitude change between the first and last blocks of testing (8 studies), the regression slope of amplitude changes across all blocks of testing (3 studies) or both percentage and slope (6 studies). Where both percentage and slope were provided, percentage change was extracted rather than slope as percentage change was the most frequently reported index of habituation in included studies. Although percentage change and slope are not identical representations of habituation (McDiarmid et al., 2017), the relative magnitude of differences in habituation profiles between migraine and control groups within each study determined via either approach is readily comparable once study outcomes are considered as effect sizes. Hence, both indices were analysed together to assess physiological differences in VEP habituation between migraine and control groups. Authors were emailed requesting VEP data that were missing, unclear, or only displayed in graph form. Where such data could not be provided, Engauge Digitizer (version: 12.1; Mitchell et al., 2019) was used to digitally estimate means and standard deviations from graphs, given that digital extraction has been shown to be more reliable than manual estimation (Jelicic et al., 2016).
Risk of Bias
Risk of bias assessment was conducted in Covidence using the National Heart, Lung and Blood Institute (NHLBI) Quality Assessment of Case–Control Studies tool, which was developed for assessing specific risks of bias associated with drawing conclusions on clinical populations compared to non-clinical controls (National Heart, Lung, and Blood Institute [NHLBI], 2014). The complete risk assessment of the selected studies is provided in Supplementary Table 1.
Data Analysis
Data was analysed using JASP (version 0.13.1; JASP Team, 2020). Meta-analysis was used to assess differences in P100 and N135 amplitudes and habituation between groups. Four subgroups were compared: 1) All migraineurs (MG) versus healthy controls (HC); 2) Migraineurs without aura (MO) versus HC; 3) Migraineurs with aura (MA) versus HC; and 4) MO versus MA. Hedges’ g effect sizes were calculated for each two-group comparison within a study (Hedges, 1981). Where means and standard deviations were unavailable, other statistics (e.g., t statistic, confidence intervals) were converted to calculate effect sizes according to the Cochrane Handbook (Higgins et al., 2020). One study contributed two sets of effect sizes for different sized stimuli (Omland et al., 2013), as such the larger check size was included in P100 analysis that is thought to reflect preferential M-pathway responses (fast temporal low spatial frequency sensitivity) and the smaller in N135 that is more likely to be associated with preferential P-pathway processing (slower temporal high spatial frequency sensitivity) based on previous literature (Derrington & Lennie, 1984; Klistorner et al., 1997; Merigan, 1991; Nassi & Callaway, 2009).
A random effects meta-analysis was conducted using the restricted maximum likelihood method as a robust analysis to account for underlying differences between studies, minimise bias in the analysis, and control for heterogeneity (Kalaian & Raudenbush, 1996; Kontopantelis & Reeves, 2012; Langan et al., 2019). Meta-effects with 95% confidence intervals were calculated for each subgroup and visualised using forest plots. Heterogeneity between studies was assessed using I2 and was interpreted according to effect sizes and evidence for heterogeneity (Higgins et al., 2020). Where heterogeneity was significant (p < .05), meta-regression was conducted using migraine characteristics or stimulus details as moderator variables depending on available data. Significant meta-analyses were screened for publication bias using Rosenthal’s fail-safe N (Rosenberg, 2005; Rosenthal, 1979) and assessment of funnel plot asymmetry using rank correlation and Egger’s regression significance tests (p < .05). Funnel plots and asymmetry tests are provided for all analyses in Supplementary Figs. 6–13 and were only interpreted and reported in meta-analyses when ten or more studies existed (Sterne et al., 2011).
Results
Study Selection
Initial database searching identified 225 studies, of these 112 were retained for full-text screening, after which 88 were excluded from the analysis for the following reasons: 18 studies tested migraineurs within 48 h of a migraine or did not clearly report testing interictal migraineurs, 19 lacked sufficient sample information to assess eligibility (e.g. failure to disclose absence of epilepsy) or lacked usable VEP data (e.g., missing data or combining P100 and N135 data), 17 included participants aged outside 18–60, 15 performed EEG spectral analysis not applicable to the current study, 6 did not use transient pattern-reversal VEPs (e.g., steady-state or flash, 5 were duplicates, 3 lacked English translation, 3 lacked available full-text, 2 reported use of migraine preventatives during testing, and 1 lacked non-migraine controls. Eleven authors were emailed requesting additional data across 22 potentially eligible studies. Four authors provided data, one was unable to locate the data, two authors could not be contacted via email, and four did not respond. Risk assessment was performed on the 23 studies comprising the final sample of studies from which data was extracted for analysis. Figure 2 presents a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Moher et al., 2009) depicting the number of studies obtained from searches and screened for inclusion.
PRISMA Flow Diagram of Study Selection Process (Moher et al., 2009). Note. n = number of studies
Risk of Bias Assessment
Risk assessment was conducted on 23 studies using the NHLBI Quality Assessment of Case–Control Studies tool (NHLBI, 2014) and 15 studies were rated good quality with low risk of bias. Six studies were rated fair quality due to unclear interictal period description (Áfra et al., 1998), unclear or inconsistent method of migraine diagnosis (Ambrosini et al., 2016a, b), vague description of control group (Coppola et al., 2010b; Ince et al., 2017) or unclear exclusion of comorbid disorders (Ozkul & Bozlar, 2002). Two studies were rated poor quality due to incomplete description of the control group (Judit et al., 2000) and ambiguously described interictal period (Logi et al., 2001), but were not deemed to be outside the parameters of the inclusion criteria. Following risk assessment, 23 studies were included in the meta-analysis. See Supplementary Table 2 for detailed results of the risk of bias assessment.
Study Characteristics
Meta-analyses included 23 studies published between the years 1998 and 2018, providing 108 effect sizes across P100 and N135 amplitudes and habituation. Supplementary Table 3 lists the studies that contributed effect sizes for each meta-analysis. Of these studies, seven diagnosed migraineurs using the ICHD-1 (30.43%), nine used the ICHD-2 (39.13%), one used both ICHD-1 and ICHD-2 (4.35%), four used the ICHD-3 beta (17.39%) and two did not report a specific diagnostic tool (8.70%). No study contained chronic migraineurs. Thirteen studies exclusively recruited migraineurs from hospitals (56.52%) while the remaining studies used combinations of hospitals, universities, advertisements, or participant databases. Age and sex differences between samples were statistically controlled for in only one study, therefore neither could be used as moderators. Fifteen studies reported frequency of migraines per month (65.22%) and 15 reported years suffering migraines (65.22%) in migraine participants, thereby leaving insufficient studies to analyse these moderators. Eighteen studies tested migraineurs with an interictal interval of 72 h or greater before and after testing (78.26%), three used a 48 h interictal period (13.04%), and two were ambiguous (8.70%). Three studies included complete data for VEP latency (13.04%), providing inadequate statistical power for primary or exploratory meta-analysis.
Monocular stimulation was used in 22 studies (95.65%) and binocular stimulation in one study (4.35%). Only 12 monocular studies reported which eye was tested (52.17%), although none reported whether eyes stimulated was selected in relation to the brain hemisphere associated with migraine symptoms. Seventeen studies incorporated small stimuli with check sizes ranging 0.13–0.27’ (73.91%), four used large stimuli ranging 0.80–1.13’ (17.39%), one used both a small (0.13’) and a large (1.08’) stimuli (4.35%), and one did not report check size (4.35%). Seventeen studies used reversal rates of 3.1rps (73.91%), three used 3rps (13.04%) and three used 2rps (13.04%). Given the similarity of most temporal frequencies, reversal rates were not used as a moderator due to insufficient variability. Supplementary Table 4 provides the study characteristics extracted from articles and figures or supplied by authors. Supplementary Table 5 details the individual results from each study.
Meta-Analysis of Visual Evoked Potentials in Migraine
Meta-Analyses for VEP Amplitudes in Migraine
Random effects meta-analysis using the restricted maximum likelihood method of studies comparing all migraineurs (MG) to healthy controls (HC) in P100 and N135 VEP amplitudes showed no significant differences in P100 amplitude between MG and HC across 17 studies, g = -0.15, 95% C.I. [-0.30, 0.01], p = .06, I2 = 26.69%, p = .12. No significant differences were observed in N135 amplitude between MG and HC across six studies, g = -0.32, 95% C.I. [-0.83, 0.19], p = .22, I2 = 81.50%, p < .001. Although there was substantial variance between studies, there were too few studies reporting all potential moderators to perform moderator analysis. Figure 3 provides forest plots illustrating the results of differences between MG and HC in VEP amplitudes for both waveform components.
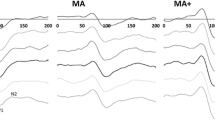
Subgroup analysis comparing VEP P100 and N135 amplitudes for diagnosis of migraine without aura (MO) versus HC, migraine with aura (MA) versus HC, and MO versus MA showed that the P100 amplitude was significantly reduced for MO, with a small effect size across 11 studies (g = -0.26, 95% C.I. [-0.50, -0.03], p = .03, I2 = 34.83%, p = .12), see Fig. 4, and MA (g = -0.30, 95% C.I. [-0.59, 0.00], p = .049, I2 = 26.25%, p = .24), see Fig. 5, when compared to HC. Amplitude of P100 was not found to differ between MO and MA across six studies, g = 0.22, 95% C.I. [-0.24, 0.67], p = .35, I2 = 62.86%, p = .02 (Supplementary Fig. 1a). This suggests diagnosis of MO or MA may not influence P100 amplitude during the interictal period, although more studies are required due to high heterogeneity.
No significant differences were seen for N135 amplitude between MO and HC across five studies, g = -0.29, 95% C.I. [-1.00, 0.42], p = .42, I2 = 84.86%, p < .001 (Supplementary Fig. 2), MA and HC across four studies, g = -0.50, 95% C.I. [-1.16, 0.16], p = .14, I2 = 73.60%, p < .01 (Supplementary Fig. 3), or MO and MA for N135 amplitude across four studies, g = 0.17, 95% C.I. [-0.17, 0.51], p = .34, I2 = 0.00%, p = .52 (Supplementary Fig. 1b).
Meta-Analyses for VEP Habituation in Migraine
Meta-analysis comparing differences between MG and HC in VEP P100 and N135 habituation showed significant differences in P100 habituation between MG and HC with a large effect size across 17 studies, g = 1.15, 95% C.I. [0.68, 1.62], p < .001, I2 = 93.61%, p < .001, see Fig. 6. The positive meta-effect indicates migraineurs may have reduced habituation of P100 amplitude compared to non-migraineurs.
Subgroup analysis comparing MO and HC in VEP habituation for P100 showed significant differences between MO and HC in P100 habituation with a large effect size across 12 studies, g = 1.30, 95% C.I. [0.63, 1.97], p < .001, I2 = 92.42%, p < .001, see Fig. 7. This suggests P100 habituation is largely reduced in migraineurs without aura compared to non-migraineurs, although high heterogeneity indicates moderating variables may impact this effect. Meta-regression showed check size significantly moderated the meta-effect calculation, p = .03, marginally reducing heterogeneity from I2 = 92.42% to I2 = 89.68%. This suggests variance in P100 habituation reported between studies is unlikely due to stimulus spatial frequency and may be due to other factors.
Significant differences in P100 habituation between MA and HC with a large effect size across eight studies are shown in Fig. 8, g = 0.88, 95% C.I. [0.52, 1.25], p < .001, I2 = 61.56%, p = .01. This suggests P100 habituation is also reduced in MA compared to controls, although high heterogeneity indicates moderating variables may impact this effect. Meta-regression showed check size significantly moderated the meta-effect calculation by reducing the influence of one outlier, p < .001, decreasing heterogeneity from I2 = 61.56% to I2 = 0.004%. Analysis of VEP habituation between migraineurs with and without aura showed no significant differences in P100 habituation between MO and MA across eight studies, g = 0.01, 95% C.I. [-0.22, 0.24], p = .92, I2 = 14.15%, p = .32 (Supplementary Fig. 4a). This suggests migraineurs with and without aura consistently show no differences in P100 habituation.
Significant differences were also found in N135 habituation between MG and HC across five studies are shown in Fig. 9, g = 1.09, 95% C.I. [0.13, 2.05], p = .03, I2 = 91.961%, p < .001. Although this suggests that migraineurs have largely reduced N135 habituation compared to non-migraineurs, this finding should be cautiously interpreted given the small number of studies analysed, wide confidence intervals and substantial heterogeneity.
Significant differences in N135 habituation were observed between MO and HC with a large effect size across four studies, g = 1.59, 95% C.I. [0.54, 2.64], p < .01, I2 = 86.71%, p < .001, see Fig. 10. Although this suggests N135 habituation appears largely reduced in migraineurs without aura compared to non-migraineurs, this finding should be cautiously interpreted given the small number of studies analysed, wide confidence intervals and substantial heterogeneity. There were no differences between MA and HC in N135 habituation across three studies, g = 1.02, 95% C.I. [-0.63, 2.67], p = .23, I2 = 92.87%, p < .001 (Supplementary Fig. 5), nor for N135 habituation between MO and MA across three studies, g = 0.29, 95% C.I. [-0.47, 1.05], p = .45, I2 = 68.42%, p = .04 (Supplementary Fig. 4b).
Summary of I2 patterns and Funnel Plot Findings
Meta-analyses using studies that measured VEP P100 amplitudes tended to show moderate heterogeneity. By comparison, similar analyses of N135 amplitude showed substantial heterogeneity. Analyses of VEP P100 and N135 habituation often showed substantial heterogeneity. Of the analyses with sufficient number of studies included, assessments of publication bias showed mixed results. Refer to Supplementary Figs. 6–13 for funnel plots and tests of asymmetry.
Discussion
This study aimed to meta-analyse case–control studies comparing visually evoked potentials (VEPs) between interictal migraineurs and non-migraine controls of similar age and gender. Initial searches yielded 225 articles, of which 23 met the inclusion criteria and risk of bias assessment. The most important findings from the meta-analyses on the included studies was that migraineurs with and without aura showed slightly reduced P100 amplitude compared to non-migraine controls, but did not differ in N135 amplitudes. Furthermore, migraineurs showed largely reduced P100 and N135 habituation compared to controls. Only migraineurs without aura showed statistically reduced N135 habituation compared to controls, possibly because there were greater sample numbers for migraineurs without aura than migraineurs with aura. However, this result is confounded by the small number of statistically heterogeneous studies analysed. Finally, differences in VEP amplitudes and habituation were not found when comparing migraine subgroups of migraine with aura (MA) to migraine without aura (MO). Latency of VEPs was not able to be meta-analysed due to only three studies supplying data on VEP latency in migraineurs and controls.
The primary hypothesis that migraineurs as a group would show altered VEP amplitudes during the interictal period compared to non-migraine controls was not supported by the 17 studies that met the criteria for a comparison of VEP amplitudes between all migraineurs and controls. However, in the 12 studies where sufficient subgroup data was present to allow meta-analysis, P100 amplitudes were reduced in the MA and MO subgroups when separately compared with controls. The second primary hypothesis was that migraineurs tested during the interictal period would show reduced VEP habituation to repeated stimulation compared to non-migraineurs, and this was partially supported with results demonstrating that all migraineurs (N = 17), including subgroups for MO (N = 12) and MA (N = 8), showed reduced P100 habituation compared to non-migraineurs. Although analysis of five studies found reduced N135 habituation in migraineurs compared to non-migraineurs, subgroup analysis found that only MO showed reduced N135 habituation compared to non-migraineurs in four studies.
The secondary aim of comparing visual function between migraine subgroups (MO compared with MA) demonstrated no differences in VEP amplitudes or habituation. Examination of the moderating effects of age, migraine frequency, years of migraine, and stimulus reversal rate or stimulus size on migraine VEPs was not possible due to insufficient number of studies providing data, lack of statistically matched samples, or insufficient variability between studies.
VEP Amplitudes During Interictal period of Migraine and Visual Processing
The present meta-analysis found reduced amplitude of visually evoked P100 waveform in the migraine MO and MA groups compared to non-migraineurs. It is important to note that (i) this finding does not appear to be robust against publication bias, with a small fail-safe N for both MO and MA groups suggesting that the significant findings could be negated by a few unpublished studies with non-significant results and (ii) a significant reduction in the P100 amplitude was not identified when comparing all migraineurs to controls (an analysis with larger sample size and greater statistical power). This may be due to studies that separately analysed migraineurs with and without aura providing more homogeneous groups, compared to studies using a single “migraine” sample containing mixed presentations of migraine, severity and time since disorder onset which possibly impacted the results. However, the subgroup analyses showed minimal heterogeneity, providing reasonable certainty that the findings were consistent across the literature.
These results suggest that migraineurs during the interictal period consistently experience a slight reduction in P100 amplitude, which is an early VEP component typically associated with the fast-conducting magnocellular pathway (M-pathway; Brown et al., 2018; Klistorner et al., 1997). This coincides with previous reviews suggesting that interictal migraineurs are impaired in the fast processing in visual tasks requiring perception of object motion and orientation by the M-pathway (O'Hare & Hibbard, 2016; Shepherd, 2019; Vallesi, 2020). However, analysis of temporal processing, in particular VEP latency, was not possible as only three of the 23 included studies provided complete latency data, requiring further research to definitively comment on the impact of migraine on M-pathway processing. Moreover, it is unclear whether reduced pattern-reversal VEPs are due to decreased excitatory mechanisms or increased inhibitory mechanisms (Cosentino et al., 2014), which remains an important gap in the literature (Vecchia & Pietrobon, 2012). The finding of reduced VEP amplitude in the present meta-analysis could be interpreted as decreased M-cell subcortical pathway recovery to repeated stimulation, contrasting the prominent theory that migraine, particularly with aura, is characterised by cortical hyperexcitability to sensory stimuli during the interictal period (Barbanti et al., 2020). Although we do not preclude the role of M-pathway driven activity in migraine, given the limitations described these results should be cautiously interpreted until more sensitive temporal analysis of migraine VEPs are researched in the future.
The term “cortical excitability” is often used to describe electrophysiological differences observed in interictal migraineurs when compared with non-migraineurs (Aurora & Wilkinson, 2007; Chen et al., 2012). However, it is difficult to interpret how decreased VEP amplitudes observed in the present meta-analysis relates to physiological changes in firing rate to repeated stimuli or to an underlying cortical excitability, in migraineurs. This is further complicated by differences in results across the different electrophysiology techniques used in migraine population studies. For instance, our meta-analysis may be compared to the findings of a previous meta-analysis by Brigo et al. (2013) examining the effects of direct transcranial magnetic stimulation (TMS) on the primary visual cortex (V1), which found that migraineurs with aura, but not migraineurs without aura, had heightened excitability (as measured by increased phosphenes) in V1 compared to non-migraineurs (Brigo et al., 2013). This may be explained by methodological differences between TMS and EEG, whereby TMS quantifies general cortical responsivity or arousal levels by directly stimulating V1 at variable stimulation levels (Magis et al., 2013), whereas VEPs recorded from occipital electrodes quantify the electrical responses to visual stimulation of the eye and processed between retina and V1 (Odom et al., 2016). Thus, hyperexcitability defined by using direct TMS may reflect a lower threshold for visual cortex activation in migraineurs (Stankewitz & May, 2009), rather than increased responsivity to visual stimulation. In addition to these differences in how visual system activity is measured by TMS and VEP methodologies, the meta-analysis on TMS studies found substantial heterogeneity and did not restrict inclusion to studies recruiting interictal migraineurs (Brigo et al., 2013). As the present VEP meta-analysis found minimal heterogeneity and only included studies that explicitly included interictal migraineurs, our finding of reduced VEP amplitudes may better reflect M pathway neuronal recovery to repeated stimulation during visual processing in interictal migraineurs than TMS. Nevertheless, methodological limitations of standard checkerboard pattern-reversal VEP technology limit further interpretation of the findings of this meta-analysis until multifocal VEPS can be recorded and temporal analysis of conduction latencies can be measured (Klistorner et al., 1997).
Migraineurs have often been reported to experience visual discomfort or have migraines triggered when viewing certain visual stimuli during the interictal period (Peroutka, 2014; Shepherd, 2019), such as high-contrast black-and-white striped (Harle et al., 2006) and checkerboard patterns (Sand & Vingen, 2000). Defocusing during stimulation may also reduce VEP amplitudes (Nguyen et al., 2016), particularly for P100 (Creel, 2019). Thus, reduced VEP amplitudes in migraine could be due to migraineurs defocusing from discomfort during pattern-reversal stimulation (Nguyen et al., 2012). Although it is recommended that at least two blocks of VEP recordings are averaged to establish a reliable VEP response (Odom et al., 2016), most included studies only reported amplitudes from the first block of VEP recordings to minimise the influence of response habituation over prolonged stimulation (Magis et al., 2007). This raises concerns regarding the precision of results of the studies analysed that showed reduced VEP amplitudes in migraineurs. Nevertheless, our meta-analytic finding of reduced VEP amplitudes is consistent with previous reports of atypical habituation patterns in migraineurs (Magis et al., 2013). Ambrosini et al. (2003) theorised that low visual responsivity, as indicated by reduced VEP amplitudes or slower latency and slower neuronal recovery to repetitive stimulation in the first block of testing, could prevent migraineurs from reaching the threshold required to trigger normal habituation and subsequently a VEP amplitude decrement. This could be a protective mechanism preventing migraineurs from excessive neuronal excitation in response to visual stimulation, allowing greater cortical activation before the maximum threshold is reached (Nguyen et al., 2012). Thus, the reduced VEP amplitudes in migraineurs identified in the present meta-analysis aligns with the second major finding that VEP habituation was reduced in interictal migraineurs across the literature.
VEP Habituation in Interictal Migraine – Impaired Filtering of Visual Information
The hypothesis that migraineurs possess atypical habituation patterns during the interictal period was supported by our results, that show reduced habituation of P100 amplitude over time compared to non-migraineurs. Analysis of all migraineurs versus controls showed a large effect and substantial heterogeneity, while MO and MA subgroups showed large effects with substantial heterogeneity. Subgroups with MA also showed minimal heterogeneity after meta-regression reduced the influence of one outlier. Together, results suggest that migraineurs during the interictal period may have a moderate to large impairment in neural habituation to repeated visual stimulation. Reduced P100 habituation and P100 amplitudes also support a hypothesis that impaired visual processing in the fast-conducting M-pathway is potentially associated with migraine during the interictal period.
Habituation is considered a basic biological mechanism associated with learning and memory, presumably as exposure and practice allows cortical neurons to direct metabolic resources towards novel stimuli by filtering out unimportant or familiar information (McDiarmid et al., 2017). Psychophysical migraine literature has suggested that migraineurs perform poorly in tasks related to object motion and orientation that require filtering of visual noise during the interictal period (Shepherd, 2019; Tibber et al., 2014), tasks that demand executive control of attention to visual stimuli (Han et al., 2019), and visuo-motor tasks such as the Trail Making Test (Vallesi, 2020). These findings in conjunction with reduced VEP habituation of P100 amplitude may point to anomalies in M-pathway driven visual attention and processing in migraine during the interictal period.
Atypical habituation has also been associated with disruptions in cortical mechanisms responsible for decreasing excitation or increasing inhibition in response to visual stimulation (Ramaswami, 2014). Similar to reduced P100 amplitudes, it remains unclear how cortical excitation and inhibition mechanisms each contribute to reduced pattern-reversal VEP habituation in migraineurs during the interictal period (Cosentino et al., 2014). Furthermore, de Tommaso et al. (2014) have suggested that reduced habituation in migraineurs could instead reflect potentiation or increase in visual responses over time. Since included studies used between-groups designs and few/none include measures of anxiety (Al-Ezzi et al., 2020) or visual discomfort, it is not possible to precisely differentiate lack of VEP habituation from potentiation when using results from the current meta-analysis.
In contrast to heightened cortical responsivity to visual stimulation, some authors argue that reduced habituation observed in migraine could result from increased stimulus-induced internal noise (i.e., nonspecific visual system activity; O'Hare & Hibbard, 2016). It is also possible that VEPs are impacted by chronic anxiety often associated with migraine (Al-Ezzi et al., 2020). This may explain why other sensory recordings, such as auditory, somatosensory, and nociceptive evoked potentials, have also shown atypical habituation in migraineurs (reviewed in Brighina et al., 2009; Magis et al., 2013). However, at this time atypical habituation of VEPs of the P100 is the only generalizable indicator of altered cortical processing associated with episodic migraines.
A recent review has noted that reduced cortical habituation occurs across many non-migraine disorders, including autism spectrum disorders, schizophrenia and Parkinson’s disease (McDiarmid et al., 2017) and fits with the hypothesis of Stankewitz and May (2009) who have argued that habituation deficits are a consequence of repeated exposure to pain activation and likely anxiety/stress caused by migraine symptoms, rather than a specific vulnerability factor underlying migraine pathophysiology. Consequently, atypical VEP habituation may worsen for migraineurs with more frequent migraines or more years suffering untreated migraines (Nguyen et al., 2012). However, as alluded to earlier, the present meta-analysis could not explore such modifiers due to insufficient data regarding participant’s migraine frequency or years experiencing migraines being included in study demographics. In addition to missing data, methodological confounds related to VEP habituation were another important shortcoming of the studies included.
Limitations of this Meta-Analysis & Future Research Directions
The generalisability of the results from this meta-analysis should be considered in the context of several methodological and data limitations. The meta-analysis suffered from limited data collected for small numbers of patients, heterogeneity of all comparisons, incomplete data on migraine severity, age at time of testing, age at disease onset, duration of disorder, visual discomfort and anxiety. Very few included studies reported the early N75 component, which is the earliest pattern-reversal VEP component depicting primarily M-pathway contribution to V1 (Klistorner et al., 1997). Furthermore, VEP stimulus check sizes varied across studies, further confounding the contribution of the M-pathway and P-pathway to P100 amplitudes and habituation. As such, it is not possible to precisely characterise reduced P100 amplitudes and habituation by M-pathway dysfunction in migraineurs during interictal periods. Rather than using alternating check sizes in pattern-reversal stimuli, future studies should incorporate a multifocal VEP stimulus and temporal analysis, which allows temporal dissociation of the M-pathway and P-pathway contributions to the cortical VEP (Klistorner et al., 1997). It is paramount that future studies assess both M and P pathway processing given the behavioural literature suggests both may be abnormal in some samples of migraineurs who also exhibit visual field deficits (McKendrick & Badcock, 2003). In addition, inadequate VEP latency data to date is another key limitation of this study and that of a previous review by Ambrosini et al. (2003) highlighting the need for further research and analysis. Thus, it remains unclear whether migraineurs possess normal visual attention and processing speed functions, or indeed experience predominantly M-pathway impairment that has been hypothesised from behavioural measures (Shepherd, 2019) or both M and P-pathway deficits.
The substantial heterogeneity between studies that have previously assessed VEP habituation in all migraineurs and subgroups with MO remains a limitation to understanding of attentional processing in migraineurs. Few studies reported controlling for potential modifiers of VEP habituation such as sensory adaptation/fatigue (McDiarmid et al., 2017; Rankin et al., 2009) or anxiety (Al-Ezzi et al., 2020). Furthermore, the studies included in the present meta-analyses used inconsistent measures of habituation, measured as either the percentage change in VEP amplitudes between the first and last blocks of testing or the linear regression slope of VEP amplitudes across all blocks. These indexes of habituation may produce distinct results even when used on the same datasets (Omland et al., 2011) and have led McDiarmid et al. (2017) to recommend authors include raw data alongside both VEP habituation indexes as this provides more comprehensive data for future meta-analyses. Nevertheless, the present meta-analysis has helped resolve previous controversies in the literature by highlighting that habituation of the P100 wave of pattern reversal VEPs is generally reduced in migraineurs during the interictal period.
Another limitation of this meta-analysis is that the contribution of migraine severity to VEP amplitudes and habituation for all included studies could not be tested. Aside from the aforementioned missing data for migraine frequency and years suffering migraines, conclusions can only be generalised to episodic migraine since no studies recruiting chronic migraineurs were included in this meta-analysis. Preliminary research has suggested that chronic migraineurs show similar VEPs to non-migraineurs when recorded using magnetoencephalography (Chen et al., 2011). A further EEG and VEP study (Viganò et al., 2018) that did not meet our age inclusion criteria has also found that electrophysiological responses were similar between chronic migraineurs during the interictal period and non-migraineurs. As such, further research is needed that measures VEPs in chronic migraineurs while excluding older adults due to age related declines in VEP latency (Brown et al., 2019).
Participant age was another limitation of the present meta-analysis. Aging is associated with both attenuation of VEPs (Brown et al., 2019) as well as changes in migraine symptoms (Antonaci et al., 2014; Wijeratne et al., 2019). For example, one large study of migraineurs aged 16 to 80 found symptoms such as photophobia were less frequent in older adults (Kelman, 2006), presumably due to age-related ocular degeneration impacting the quality of the visual signal (reviewed in Brown et al., 2019). Thus, it is highly likely that age is a confounder of the results of this meta-analysis.
Lastly, a potential problem in the included studies was the dearth of objective information relating to the stage in the interictal period and migraine cycle. Recent evidence demonstrates that the early stages of migraine before prodromal symptoms emerge can be identified by daily vision tests from home (McKendrick et al., 2018). This highlights the need for further objective research regarding visual function during the interictal period and the inclusion of such measures in migraine VEP research.
Conclusion & Future Directions
This meta-analysis has summarised the 23 studies that met the inclusion criteria regarding comparison of recording visually evoked potentials (VEPs) between migraineurs during the interictal period and non-migraine controls. The results indicate that migraineurs with and without aura, compared to non-migraineurs, showed slightly reduced P100 amplitudes and largely reduced P100 habituation to repeated stimulation during the interictal period. This suggests possible dysfunction in the fast-conducting magnocellular visual pathways that affect attention, motion detection and rates of visual processing in migraineurs during the interictal period. Although the generalisability of results is limited by missing data, participant confounds and inconsistent methodologies, these are unlikely to diminish the utility of abnormal VEPs as a physiological biomarker of relative cortical activation in migraineurs. Results from this meta-analysis highlight the likelihood of early magnocellular visual processing abnormalities in migraine, providing a platform for future experimental studies to advance migraine research by using temporal non-linear VEP analysis techniques specialised for separation of the magnocellular and parvocellular contributions to geniculostriate cortical visual processing.
References
*References marked with an asterisk were included in the meta-analysis
*Áfra, J., Cecchini, A. P., De Pasqua, V., Albert, A., & Schoenen, J. (1998). Visual evoked potentials during long periods of pattern-reversal stimulation in migraine. Brain, 121(2), 233–241. https://doi.org/10.1093/brain/121.2.233
*Áfra, J., Cecchini, A. P., Sándor, P. S., & Schoenen, J. (2000a). Comparison of visual and auditory evoked cortical potentials in migraine patients between attacks. Clinical Neurophysiology, 111(6), 1124–1129. https://doi.org/10.1016/s1388-2457(00)00271-6
*Áfra, J., Genicot, R., Ambrosini, A., Albert, A., & Schoenen, J. (2000b). Influence of colors on habituation of visual evoked potentials in patients with migraine with aura and in healthy volunteers. Headache, 40(1), 36–40. https://doi.org/10.1046/j.1526-4610.2000.00006.x
Al-Ezzi, A., Kamel, N., Faye, I., & Gunaseli, E. (2020). Review of EEG, ERP, and Brain Connectivity Estimators as Predictive Biomarkers of Social Anxiety Disorder. Frontiers in Psychology, 11, 730. https://doi.org/10.3389/fpsyg.2020.00730
*Ambrosini, A., Coppola, G., Iezzi, E., Pierelli, F., & Schoenen, J. (2016a). Reliability and repeatability of testing visual evoked potential habituation in migraine: A blinded case–control study. Cephalalgia, 37(5), 418–422. https://doi.org/10.1177/0333102416648656
Ambrosini, A., De Noordhout, A., Sándor, P. S., & Schoenen, J. (2003). Electrophysiological studies in migraine: A comprehensive review of their interest and limitations. Cephalalgia, 23(1), 13–31. https://doi.org/10.1046/j.1468-2982.2003.00571.x
*Ambrosini, A., Iezzi, E., Perrotta, A., Kisialiou, A., Nardella, A., Berardelli, A., Pierelli, F., & Schoenen, J. (2015). Correlation between habituation of visual-evoked potentials and magnetophosphene thresholds in migraine: A case-control study. Cephalalgia, 36(3), 258–264. https://doi.org/10.1177/0333102415590241
*Ambrosini, A., Kisialiou, A., Coppola, G., Finos, L., Magis, D., Pierelli, F., & Schoenen, J. (2016b). Visual and auditory cortical evoked potentials in interictal episodic migraine: An audit on 624 patients from three centres. Cephalalgia, 37(12), 1126–1134. https://doi.org/10.1177/0333102416665224
Antonaci, F., Voiticovschi-Iosob, C., Di Stefano, A. L., Galli, F., Ozge, A., & Balottin, U. (2014). The evolution of headache from childhood to adulthood: A review of the literature. Journal of Headache and Pain, 15(15), 1–11. https://doi.org/10.1186/1129-2377-15-15
Aurora, S. K., & Wilkinson, F. (2007). The brain is hyperexcitable in migraine. Cephalalgia, 27(12), 1442–1453. https://doi.org/10.1111/j.1468-2982.2007.01502.x
Barbanti, P., Brighina, F., Egeo, G., Di Stefano, V., Silvestro, M., & Russo, A. (2020). Migraine as a cortical brain disorder. Headache, 1–12. https://doi.org/10.1111/head.13935
Baseler, H. A., Sutter, E. E., Klein, S. A., & Carney, T. (1994). The topography of visual evoked response properties across the visual field. Electroencephalography and Clinical Neurophysiology, 90(1), 65–81. https://doi.org/10.1016/0013-4694(94)90114-7
*Bohotin, V., Fumal, A., Vandenheede, M., Gérard, P., Bohotin, C., Maertens de Noordhout, A., & Schoenen, J. (2002). Effects of repetitive transcranial magnetic stimulation on visual evoked potentials in migraine. Brain, 125(4), 912–922. https://doi.org/10.1093/brain/awf081
Brighina, F., Palermo, A., & Fierro, B. (2009). Cortical inhibition and habituation to evoked potentials: Relevance for pathophysiology of migraine. Journal of Headache and Pain, 10(2), 77–84. https://doi.org/10.1007/s10194-008-0095-x
Brigo, F., Storti, M., Tezzon, F., Manganotti, P., & Nardone, R. (2013). Primary visual cortex excitability in migraine: A systematic review with meta-analysis. Neurological Sciences, 34(6), 819–830. https://doi.org/10.1007/s10072-012-1274-8
Brown, A., Corner, M., Crewther, D., & Crewther, S. (2019). Age related decline in cortical multifocal flash VEP: Latency increases shown to be predominately magnocellular. Frontiers in Aging Neuroscience, 10(430), 1–10. https://doi.org/10.3389/fnagi.2018.00430
Brown, A., Corner, M., Crewther, D. P., & Crewther, S. G. (2018). Human flicker fusion correlates with physiological measures of magnocellular neural efficiency. Frontiers in Human Neuroscience, 12(176), 1–7. https://doi.org/10.3389/fnhum.2018.00176
Chen, W.-T., Wang, S.-J., Fuh, J.-L., Ko, Y.-C., Lee, Y.-C., Hämäläinen, M. S., & Lin, Y.-Y. (2012). Visual cortex excitability and plasticity associated with remission from chronic to episodic migraine. Cephalalgia, 32(7), 537–543. https://doi.org/10.1177/0333102412443337
Chen, W.-T., Wang, S.-J., Fuh, J.-L., Lin, C.-P., Ko, Y.-C., & Lin, Y.-Y. (2011). Persistent ictal-like visual cortical excitability in chronic migraine. Pain, 152(2), 254–258. https://doi.org/10.1016/j.pain.2010.08.047
*Coppola, G., Ambrosini, A., Clemente, L. D., Magis, D., Fumal, A., Gérard, P., Pierelli, F., & Schoenen, J. (2007). Interictal abnormalities of gamma band activity in visual evoked responses in migraine: An indication of thalamocortical dysrhythmia? Cephalalgia, 27(12), 1360–1367. https://doi.org/10.1111/j.1468-2982.2007.01466.x
*Coppola, G., Currà, A., Sava, S. L., Alibardi, A., Parisi, V., Pierelli, F., & Schoenen, J. (2010a). Changes in visual-evoked potential habituation induced by hyperventilation in migraine. Journal of Headache and Pain, 11(6), 497–503. https://doi.org/10.1007/s10194-010-0239-7
*Coppola, G., Currà, A., Serrao, M., Di Lorenzo, C., Gorini, M., Porretta, E., Alibardi, A., Parisi, V., & Pierelli, F. (2010b). Lack of cold pressor test-induced effect on visual-evoked potentials in migraine. Journal of Headache and Pain, 11(2), 115–121. https://doi.org/10.1007/s10194-009-0177-4
Coppola, G., Di Lorenzo, C., Parisi, V., Lisicki, M., Serrao, M., & Pierelli, F. (2019). Clinical neurophysiology of migraine with aura. Journal of Headache and Pain, 20(1), 42. https://doi.org/10.1186/s10194-019-0997-9
*Coppola, G., Parisi, V., Di Lorenzo, C., Serrao, M., Magis, D., Schoenen, J., & Pierelli, F. (2013). Lateral inhibition in visual cortex of migraine patients between attacks. Journal of Headache and Pain, 14(20), 1–12. https://doi.org/10.1186/1129-2377-14-20
Coppola, G., Pierelli, F., & Schoenen, J. (2009). Habituation and migraine. Neurobiology of Learning and Memory, 92(2), 249–259. https://doi.org/10.1016/j.nlm.2008.07.006
Coppola, G., & Schoenen, J. (2012). Cortical excitability in chronic migraine. Current Pain and Headache Reports, 16(1), 93–100. https://doi.org/10.1007/s11916-011-0231-1
Corbetta, M., & Shulman, G. L. (2002). Control of goal-directed and stimulus-driven attention in the brain. Nature Reviews: Neuroscience, 3(3), 215–229.
Cosentino, G., Fierro, B., & Brighina, F. (2014). From different neurophysiological methods to conflicting pathophysiological views in migraine: A critical review of literature. Clinical Neurophysiology, 125(9), 1721–1730. https://doi.org/10.1016/j.clinph.2014.05.005
Creel, D. J. (2019). Visually evoked potentials. In K. H. Levin & P. Chauvel (Eds.), Handbook of Clinical Neurology (3rd ed., Vol. 160, pp. 501–522). Elsevier. https://doi.org/10.1016/B978-0-444-64032-1.00034-5
Crewther, S. G., Goharpey, N., Bannister, L., & Lamp, G. (2012). Goal-driven attention and working memory. In L. Carey (Ed.), Stroke rehabilitation; Insights from neuroscience and imaging (pp. 191–2018). Oxford University Press.
de Tommaso, M. (2019). An update on EEG in migraine. Expert Review of Neurotherapeutics, 19(8), 729–737. https://doi.org/10.1080/14737175.2019.1586534
de Tommaso, M., Ambrosini, A., Brighina, F., Coppola, G., Perrotta, A., Pierelli, F., Sandrini, G., Valeriani, M., Marinazzo, D., Stramaglia, S., & Schoenen, J. (2014). Altered processing of sensory stimuli in patients with migraine. Nature Reviews: Neurology, 10, 144–155. https://doi.org/10.1038/nrneurol.2014.14
Derrington, A. M., & Lennie, P. (1984). Spatial and temporal contrast sensitivities of neurones in lateral geniculate nucleus of macaque. The Journal of Physiology, 357(1), 219–240. https://doi.org/10.1113/jphysiol.1984.sp015498
Felleman, D. J., & Van Essen, D. C. (1991). Distributed hierarchical processing in the primate cerebral cortex. Cerebral Cortex, 1(1), 1–47. https://doi.org/10.1093/cercor/1.1.1
*Fumal, A., Coppola, G., Bohotin, V., Gérardy, P. Y., Seidel, L., Donneau, A. F., Vandenheede, M., Maertens de Noordhout, A., & Schoenen, J. (2006). Induction of long-lasting changes of visual cortex excitability by five daily sessions of repetitive transcranial magnetic stimulation (rTMS) in healthy volunteers and migraine patients. Cephalalgia, 26(2), 143–149. https://doi.org/10.1111/j.1468-2982.2005.01013.x
Goadsby, P. J., Holland, P. R., Martins-Oliveira, M., Hoffmann, J., Schankin, C., & Akerman, S. (2017). Pathophysiology of migraine: A disorder of sensory processing. Physiological Reviews, 97(2), 553–622. https://doi.org/10.1152/physrev.00034.2015
Han, M., Hou, X., Xu, S., Hong, Y., Chen, J., Ma, Y., Nie, S., & Liu, X. (2019). Selective attention network impairment during the interictal period of migraine without aura. Journal of Clinical Neuroscience, 60, 73–78. https://doi.org/10.1016/j.jocn.2018.10.002
Harle, D. E., Shepherd, A. J., & Evans, B. J. W. (2006). Visual stimuli are common triggers of migraine and are associated with pattern glare. Headache, 46(9), 1431–1440. https://doi.org/10.1111/j.1526-4610.2006.00585.x
Hedges, L. V. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics, 6(2), 107–128. https://doi.org/10.2307/1164588
Higgins, J. P. T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M. J., & Welch, V. A. (2020). Cochrane handbook for systematic reviews of interventions version 6.1. Cochrane. https://www.training.cochrane.org/handbook
*Ince, F., Erdogan-Bakar, E., & Unal-Cevik, I. (2017). Preventive drugs restore visual evoked habituation and attention in migraineurs. Acta Neurologica Belgica, 117(2), 523–530. https://doi.org/10.1007/s13760-017-0749-z
International Headache Society [IHS]. (2018). The International Classification of Headache Disorders, 3rd edition. Cephalalgia, 38(1), 1–211. https://doi.org/10.1177/0333102417738202
JASP Team. (2020). JASP (Version 0.13.1)[Computer Software].
Jelicic, A. J., Vucic, K., Dosenovic, S., Sapunar, D., & Puljak, L. (2016). Extracting data from figures with software was faster, with higher interrater reliability than manual extraction. Journal of Clinical Epidemiology, 74, 119–123. https://doi.org/10.1016/j.jclinepi.2016.01.002
*Judit, Á., Sándor, P. S., & Schoenen, J. (2000). Habituation of visual and intensity dependence of auditory evoked cortical potentials tends to normalize just before and during the migraine attack. Cephalalgia, 20(8), 714–719. https://doi.org/10.1111/j.1468-2982.2000.00122.x
Kalaian, H., & Raudenbush, S. (1996). A multivariate mixed linear model for meta-analysis. Psychological Methods, 1(3), 227–235. https://doi.org/10.1037/1082-989X.1.3.227
Kelman, L. (2006). Migraine changes with age: Impact on migraine classification. Headache, 46(7), 1161–1171. https://doi.org/10.1111/j.1526-4610.2006.00444.x
Klistorner, A., Crewther, D. P., & Crewther, S. G. (1997). Separate magnocellular and parvocellular contributions from temporal analysis of the multifocal VEP. Vision Research, 37(15), 2161–2169. https://doi.org/10.1016/S0042-6989(97)00003-5
Kontopantelis, E., & Reeves, D. (2012). Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: A comparison between DerSimonian-Laird and restricted maximum likelihood. Statistical Methods in Medical Research, 21(6), 657–659. https://doi.org/10.1177/0962280211413451
Kowacs, P. A., Utiumi, M. A., & Piovesan, E. J. (2015). The visual system in migraine: From the bench side to the office. Headache, 55(S1), 84–98. https://doi.org/10.1111/head.12514
Langan, D., Higgins, J., Jackson, D., Bowden, J., Veroniki, A. A., Kontopantelis, E., Viechtbauer, W., & Simmonds, M. (2019). A comparison of heterogeneity variance estimators in simulated random-effects meta-analyses. Research Synthesis Methods, 10(1), 83–98. https://doi.org/10.1002/jrsm.1316
Laycock, R., Crewther, S. G., & Crewther, D. P. (2007). A role for the ‘magnocellular advantage’ in visual impairments in neurodevelopmental and psychiatric disorders. Neuroscience and Biobehavioral Reviews, 31(3), 363–376. https://doi.org/10.1016/j.neubiorev.2006.10.003
Lipton, R. B., Serrano, D., Holland, S., Fanning, K. M., Reed, M. L., & Buse, D. C. (2013). Barriers to the diagnosis and treatment of migraine: Effects of sex, income, and headache features. Headache, 53(1), 81–92. https://doi.org/10.1111/j.1526-4610.2012.02265.x
*Lisicki, M., D’Ostilio, K., Coppola, G., De Noordhout, A. M., Parisi, V., Schoenen, J., & Magis, D. (2018). Brain correlates of single trial visual evoked potentials in migraine: More than meets the eye. Frontiers in Neurology, 9(393), 1–10. https://doi.org/10.3389/fneur.2018.00393
*Lisicki, M., Ruiz-Romagnoli, E., D’Ostilio, K., Piedrabuena, R., Giobellina, R., Schoenen, J., & Magis, D. (2017). Familial history of migraine influences habituation of visual evoked potentials. Cephalalgia, 37(11), 1082–1087. https://doi.org/10.1177/0333102416673207
Livingstone, M. S., & Hubel, D. H. (1987). Psychophysical evidence for separate channels for the perception of form, color, movement, and depth. Journal of Neuroscience, 7(11), 3416. https://doi.org/10.1523/JNEUROSCI.07-11-03416.1987
*Logi, F., Bonfiglio, L., Orlandi, G., Bonanni, E., Iudice, A., & Sartucci, F. (2001). Asymmetric scalp distribution of pattern visual evoked potentials during interictal phases in migraine. Acta Neurologica Scandinavica, 104(5), 301–307. https://doi.org/10.1034/j.1600-0404.2001.00329.x
Magis, D., Ambrosini, A., Bendtsen, L., Ertas, M., Kaube, H., & Schoenen, J. (2007). Evaluation and proposal for optimalization of neurophysiological tests in migraine: Part 1—Electrophysiological tests. Cephalalgia, 27(12), 1323–1338. https://doi.org/10.1111/j.1468-2982.2007.01440.x
Magis, D., Lisicki, M., & Coppola, G. (2016). Highlights in migraine electrophysiology: Are controversies just reflecting disease heterogeneity? Current Opinion in Neurology, 29(3), 320–330. https://doi.org/10.1097/WCO.0000000000000335
Magis, D., Vigano, A., Sava, S., d’Elia, T. S., Schoenen, J., & Coppola, G. (2013). Pearls and pitfalls: Electrophysiology for primary headaches. Cephalalgia, 33(8), 526–539. https://doi.org/10.1177/0333102413477739
McDiarmid, T. A., Bernardos, A. C., & Rankin, C. H. (2017). Habituation is altered in neuropsychiatric disorders—A comprehensive review with recommendations for experimental design and analysis. Neuroscience and Biobehavioral Reviews, 80, 286–305. https://doi.org/10.1016/j.neubiorev.2017.05.028
McKendrick, A. M., & Badcock, D. R. (2003). Contrast-processing dysfunction in both Magnocellular and Parvocellular pathways in Migraineurs with or without Aura. Investigative Opthalmology & Visual Science, 44(1), 442. https://doi.org/10.1167/iovs.02-0630
McKendrick, A. M., Chan, Y. M., Vingrys, A. J., Turpin, A., & Badcock, D. R. (2018). Daily vision testing can expose the prodromal phase of migraine. Cephalalgia, 38(9), 1575–1584. https://doi.org/10.1177/0333102417741130
Merigan, W. H. (1991). P and M pathway specialisation in the macaque. In A. Valberg & B. B. Lee (Eds.), From pigments to perception (pp. 117–125). Springer. https://doi.org/10.1007/978-1-4615-3718-2_13
Mitchell, M., Muftakhidinov, B., & Wincheb, T. (2019). Engauge Digitizer Software. http://markummitchell.github.io/engauge-digitizer
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & The PRISMA Group. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. https://doi.org/10.1371/journal.pmed1000097
Nassi, J. J., & Callaway, E. M. (2009). Parallel processing strategies of the primate visual system. Nature Reviews Neuroscience, 10(5), 360–372. https://doi.org/10.1038/nrn2619
National Heart, Lung, and Blood Institute [NHLBI]. (2014). Quality assessment of case-control studies. National Institutes of Health. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
Nguyen, B. N., Lek, J. J., Vingrys, A. J., & McKendrick, A. M. (2016). Clinical impact of migraine for the management of glaucoma patients. Progress in Retinal and Eye Research, 51, 107–124. https://doi.org/10.1016/j.preteyeres.2015.07.006
*Nguyen, B. N., McKendrick, A. M., & Vingrys, A. J. (2012). Simultaneous retinal and cortical visually evoked electrophysiological responses in between migraine attacks. Cephalalgia, 32(12), 896–907. https://doi.org/10.1177/0333102412453953
*Nguyen, B. N., Vingrys, A. J., & McKendrick, A. M. (2014). The effect of duration post-migraine on visual electrophysiology and visual field performance in people with migraine. Cephalalgia, 34(1), 42–57. https://doi.org/10.1177/0333102413498939
O’Hare, L., & Hibbard, P. B. (2016). Visual processing in migraine. Cephalalgia, 36(11), 1057–1076. https://doi.org/10.1177/0333102415618952
Odom, J. V., Bach, M., Brigell, M., Holder, G. E., McCulloch, D. L., Mizota, A., & Tormene, A. P. (2016). ISCEV standard for clinical visual evoked potentials: (2016 update). Documenta Ophthalmologica, 133(1), 1–9. https://doi.org/10.1007/s10633-016-9553-y
Omland, P. M., Nilsen, K. B., & Sand, T. (2011). Habituation measured by pattern reversal visual evoked potentials depends more on check size than reversal rate. Clinical Neurophysiology, 122(9), 1846–1853. https://doi.org/10.1016/j.clinph.2011.02.025
*Omland, P. M., Nilsen, K. B., Uglem, M., Gravdahl, G., Linde, M., Hagen, K., & Sand, T. (2013). Visual evoked potentials in interictal migraine: No confirmation of abnormal Habituation. Headache, 53(7), 1071–1086. https://doi.org/10.1111/head.12006
*Omland, P. M., Uglem, M., Hagen, K., Linde, M., Tronvik, E., & Sand, T. (2016). Visual evoked potentials in migraine: Is the “neurophysiological hallmark” concept still valid? Clinical Neurophysiology, 127(1), 810–816. https://doi.org/10.1016/j.clinph.2014.12.035
*Ozkul, Y., & Bozlar, S. (2002). Effects of fluoxetine on habituation of pattern reversal visually evoked potentials in migraine prophylaxis. Headache: The Journal of Head and Face Pain, 42(7), 582–587. https://doi.org/10.1046/j.1526-4610.2002.02144.x
Peroutka, S. J. (2014). What turns on a migraine? A systematic review of migraine precipitating factors. Curr Pain and Headache Rep, 18(10), 454. https://doi.org/10.1007/s11916-014-0454-z
Ramaswami, M. (2014). Network plasticity in adaptive filtering and behavioral habituation. Neuron, 82(6), 1216–1229. https://doi.org/10.1016/j.neuron.2014.04.035
Rankin, C. H., Abrams, T., Barry, R. J., Bhatnagar, S., Clayton, D. F., Colombo, J., Coppola, G., Geyer, M. A., Glanzman, D. L., Marsland, S., McSweeney, F. K., Wilson, D. A., Wu, C.-F., & Thompson, R. F. (2009). Habituation revisited: An updated and revised description of the behavioral characteristics of habituation. Neurobiology of Learning and Memory, 92(2), 135–138. https://doi.org/10.1016/j.nlm.2008.09.012
*Rauschel, V., Ruscheweyh, R., Krafczyk, S., & Straube, A. (2015). Test-retest reliability of visual-evoked potential habituation. Cephalalgia, 36(9), 831–839. https://doi.org/10.1177/0333102415613613
Rosenberg, M. S. (2005). The file-drawer problem revisited: A general weighted method for calculating fail-safe numbers in meta-analysis. Evolution, 59(2), 464–468. https://doi.org/10.1111/j.0014-3820.2005.tb01004.x
Rosenthal, R. (1979). The file drawer problem and tolerance for null results. Psychological Bulletin, 86(3), 638–641. https://doi.org/10.1037/0033-2909.86.3.638
Sand, T., & Vingen, J. V. (2000). Visual, long-latency auditory and brainstem auditory evoked potentials in migraine: Relation to pattern size, stimulus intensity, sound and light discomfort thresholds and pre-attack state. Cephalalgia, 20(9), 804–820. https://doi.org/10.1046/j.1468-2982.2000.00098.x
Schoenen, J. (2011). Is chronic migraine a never-ending migraine attack? Pain, 152(2), 239–240. https://doi.org/10.1016/j.pain.2010.12.002
Shepherd, A. J. (2019). A review of motion and orientation processing in migraine. Vision (Basel), 3(2). https://doi.org/10.3390/vision3020012
Stankewitz, A., & May, A. (2009). The phenomenon of changes in cortical excitability in migraine is not migraine-specific – A unifying thesis. Pain, 145(1), 14–17. https://doi.org/10.1016/j.pain.2009.03.010
Sterne, J. A., Sutton, A. J., Ioannidis, J. P., Terrin, N., Jones, D. R., Lau, J., Carpenter, J., Rucker, G., Harbord, R. M., Schmid, C. H., Tetzlaff, J., Deeks, J. J., Peters, J., Macaskill, P., Schwarzer, G., Duval, S., Altman, D. G., Moher, D., & Higgins, J. P. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ, 343, d4002. https://doi.org/10.1136/bmj.d4002
Stewart, W. F., Wood, C., Reed, M. L., Roy, J., & Lipton, R. B. (2008). Cumulative lifetime migraine incidence in women and men. Cephalalgia, 28(11), 1170–1178. https://doi.org/10.1111/j.1468-2982.2008.01666.x
Tibber, M. S., Kelly, M. G., Jansari, A., Dakin, S. C., & Shepherd, A. J. (2014). An inability to exclude visual noise in migraine. Investigative Ophthalmology and Visual Science, 55(4), 2539–2546. https://doi.org/10.1167/iovs.14-13877
Tolner, E. A., Chen, S.-P., & Eikermann-Haerter, K. (2019). Current understanding of cortical structure and function in migraine. Cephalalgia, 39(13), 1683–1699. https://doi.org/10.1177/0333102419840643
Vallesi, A. (2020). On the utility of the trail making test in migraine with and without aura: A meta-analysis. The Journal of Headache and Pain, 21(1), 63. https://doi.org/10.1186/s10194-020-01137-y
Vecchia, D., & Pietrobon, D. (2012). Migraine: A disorder of brain excitatory–inhibitory balance? Trends in Neurosciences, 35(8), 507–520. https://doi.org/10.1016/j.tins.2012.04.007
Veritas Health Innovation. (2019). Covidence systematic review software, Melbourne, Australia. https://www.covidence.org
Vialatte, F.-B., Maurice, M., Dauwels, J., & Cichocki, A. (2010). Steady-state visually evoked potentials: Focus on essential paradigms and future perspectives. Progress in Neurobiology, 90(4), 418–438. https://doi.org/10.1016/j.pneurobio.2009.11.005
Viganò, A., Torrieri, M. C., Toscano, M., Puledda, F., Petolicchio, B., Sasso D’Elia, T., Verzina, A., Ruggiero, S., Altieri, M., Vicenzini, E., Schoenen, J., & Di Piero, V. (2018). Neurophysiological correlates of clinical improvement after greater occipital nerve (GON) block in chronic migraine: Relevance for chronic migraine pathophysiology. Journal of Headache and Pain, 19(1), 73. https://doi.org/10.1186/s10194-018-0901-z
Vos, T., & GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. (2017). Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. The Lancet, 390, 1211–1259. https://doi.org/10.1016/S0140-6736(17)32154-2
Wijeratne, T., Tang, H. M., Crewther, D., & Crewther, S. (2019). Prevalence of Migraine in the Elderly: A Narrated Review. Neuroepidemiology, 52(1–2), 104–110. https://doi.org/10.1159/000494758
Wong-Riley, M. T. T. (2010). Energy metabolism of the visual system. Eye and Brain, 2, 99–116. https://doi.org/10.2147/EB.S9078
Wurtz, R. H., & Goldberg, M. E. (1971). Superior colliculus cell responses related to eye movements in awake monkeys. Science, 171(3966), 82. https://doi.org/10.1126/science.171.3966.82
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
TS, SGC, MM and NR contributed to the review conception and design. Literature searching and screening were performed by TS, NR, and VN. Data analysis was conducted by TS, and results were interpreted and written by TS and MM. The first draft of the manuscript was written by TS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
The authors have no relevant financial or non-financial interests to disclose and no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sezai, T., Murphy, M.J., Riddell, N. et al. Visual Processing During the Interictal Period Between Migraines: A Meta-Analysis. Neuropsychol Rev 33, 765–782 (2023). https://doi.org/10.1007/s11065-022-09562-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-022-09562-3