Abstract
Both substance-related as well as non-substance-related addictions may include recurrent engagement in risky actions despite adverse outcomes. We here apply a unified approach and review task-based neuroimaging studies on substance-related (SRAs) and non-substance related addictions (NSRAs) to examine commonalities and differences in neural correlates of risk-taking in these two addiction types. To this end, we conducted a systematic review adhering to the PRISMA guidelines. Two databases were searched with predefined search terms to identify neuroimaging studies on risk-taking tasks in individuals with addiction disorders. In total, 19 studies on SRAs (comprising a total of 648 individuals with SRAs) and 10 studies on NSRAs (comprising a total of 187 individuals with NSRAs) were included. Risk-related brain activation in SRAs and NSRAs was summarized individually and subsequently compared to each other. Results suggest convergent altered risk-related neural processes, including hyperactivity in the OFC and the striatum. As characteristic for both addiction types, these brain regions may represent an underlying mechanism of suboptimal decision-making. In contrast, decreased DLPFC activity may be specific to SRAs and decreased IFG activity could only be identified for NSRAs. The precuneus and posterior cingulate show elevated activity in SRAs, while findings regarding these areas were mixed in NSRAs. Additional scarce evidence suggests decreased ventral ACC activity and increased dorsal ACC activity in both addiction types. Associations between identified activation patterns with drug use severity underpin the clinical relevance of these findings. However, this exploratory evidence should be interpreted with caution and should be regarded as preliminary. Future research is needed to evaluate the findings gathered by this review.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Addictive disorders are among the most common psychopathologies with lifetime prevalence rates ranging from around 1.2% for gambling disorder (American Psychiatric Association, 2013) to 9.9% for drug use disorder (Grant et al., 2016) and 21.9% for alcohol use disorder (Grant et al., 2015). Negative sequelae include considerable economic burden on society (Collins et al., 2000) and a reduced quality of life with elevated levels of mental and physical health problems in affected individuals (Bizzarri et al., 2005; Black et al., 2013). Addictive disorders encompass a broad spectrum of maladaptive behaviors, including substance-related addictions (SRAs) such as drug dependence and non-substance-related addictions (NSRAs) such as pathological gambling. A growing body of research shows that SRAs and NSRAs present similarities in behavioral as well as in biological alterations. Both, SRAs and NSRAs manifest similar core symptoms, such as withdrawal, tolerance, craving, and impaired behavioral control (Olsen, 2011; Potenza, 2008). Moreover, both addiction types are characterized by an inability to resist impulses towards rewarding stimuli despite potential adverse consequences (Potenza, 2006; West, 2001). The question as to why someone would repeatedly decide to engage in risky actions with possible adverse outcomes and despite significant negative consequences is puzzling. Greater insight into neural mechanisms of altered risk-taking behavior could contribute to a better understanding of maladaptive choice in addictive disorders.
Broadly, risk-taking is the tendency to choose an action with the potential for a relatively large, either beneficial or adverse outcome over an alternative that results in a comparably small, beneficial outcome. Thus, the individual has to evaluate the rewarding and punishing consequences of each option and their likelihood of occurring (Mellers et al., 1997; Paulus et al., 2003). Research on risk-taking has a long tradition and emerged predominantly from two fields. In economics, risk seeking is commonly defined as the preference for choosing an action with a higher, as opposed to lower, outcome variance holding the expected value constant (Hertwig et al., 2019; Schonberg et al., 2011). The outcome of such choices is probabilistic. In addition, the probability distributions of each possible outcome may be either known (decisions under risk) or unknown (decisions under uncertainty; Knight, 1921). Decisions which entail unknown probability distributions may best represent the psychological conception of risk, namely, behaviors with an uncertain potential for harmful outcomes for oneself or others (e.g., reckless driving, engaging in unprotected sex, free-climbing). Thus, in psychology, risky behavior is more broadly conceptualized as the tendency to engage in behaviors with potential detrimental consequences, but also with potential personal benefits, in situations which do not contain complete information about potential costs and benefits. This behavior is often seen in individuals with certain psychiatric disorders (e.g., Borderline Personality Disorder, Bipolar Disorder, Attention-Deficit/Hyperactivity Disorder). Addictive behaviors are also characterized by this kind of naturalistic risk-taking behavior from a psychological perspective: affected individuals show addictive behaviors despite potentially harmful, unknown consequences.
As a consequence of these different conceptualizations of risk-taking, different measurement traditions and paradigms have emerged and are used in neuroscientific studies investigating neural correlates of risk-taking and associated constructs. Insights gained through these studies point to several brain regions and networks involved. Early meta-analytic results identified several brain regions to be involved in the complex evaluation of decision alternatives (Krain et al., 2006; Mohr et al., 2010), including the dorsolateral prefrontal cortex (DLPFC), the ventromedial prefrontal cortex (vmPFC), the orbitofrontal cortex (OFC), the posterior parietal cortex (PPC), the anterior cingulate cortex (ACC), as well as the insula. Specifically, the vmPFC, the ventral striatum, and (in some cases) the posterior cingulate cortex are thought to form the core of the brain’s valuation system and to track the value of choice options across a variety of different contexts (Bartra et al., 2013; Lopez-Guzman et al., 2019). Activity in these brain areas can be observed both during decision-making and during outcome delivery (Bartra et al., 2013). In addition, activity in vmPFC and OFC is also associated with more emotional aspects of decision-making, such as affective attribution of choice (Ernst & Paulus, 2005), and it has also been shown to be involved in several other functions related to decision-making such as flexible representation of stimulus-outcome associations or inhibitory control (Murray & Rudebeck, 2018; Stalnaker et al., 2015). A more recent hypothesis proposes a unifying theory of OFC function which may integrate the above mentioned tasks, suggesting that the OFC may provide abstraction of currently available information/ higher-order representations that enable inference of unobservable information (Murray & Rudebeck, 2018; Stalnaker et al., 2015; Wilson et al., 2014; Yu et al., 2020). That is, it may represent the state of the world, all information that is relevant to the current decision. Thus, the OFC may provide a cognitive map of task/state space, a neural representation of stimuli, actions and other sensory features that occur in associations with outcomes.
The anterior insula and the (dorsal/caudal) striatum seem to be more related to emotional arousal or salience during risk-taking (Bartra et al., 2013). In addition, anterior insula activity codes individual risk perception (Christopoulos et al., 2009; Fukunaga et al., 2018; Paulus et al., 2003; Preuschoff et al., 2006). Another brain region that is commonly mentioned in the context of risk-taking is the DLPFC. It has been argued that during decision-making, it represents both cognitive and value-based information such as integrating rule-outcome associations and that it is especially activated during complex choices (Dixon & Christoff, 2014). The influence of the DLPFC on risk-taking may be of particular relevance for addictions due to its role in self-control.
Activity in many of these regions has been shown to differ in addiction. Moreover, research has already demonstrated that affective mechanisms such as reward processing and cognitive control (e.g., the inhibition of impulses) are altered in both SRAs and NSRAs. Specifically, altered (anticipatory) signaling in the amygdala and striatum seems to underlie aberrant reward processing in addictive disorders (in NSRAs as well as SRAs; Balodis & Potenza, 2015; García-García et al., 2014; Luijten et al., 2017). During inhibitory control tasks, individuals with addictive disorders show reduced activity in the ACC as well as prefrontal regions, including the DLPFC (Luijten et al., 2014). Since reward-processing as well as inhibitory control constitute essential and integral aspects of decision-making, it is likely that decision-making processes are also altered among individuals with addictive disorders (Balodis & Potenza, 2015; Hommer et al., 2011; Lawrence et al., 2009; Leyton & Vezina, 2013; Potenza et al., 2013).
A meta-analytic review from 2013 identified alterations in the ACC, OFC, DLPFC, striatum, insula, and the somatosensory cortex during risk-related decisions in individuals with SRAs (Gowin et al., 2013). Moreover, a sub-analysis of a recent meta-analysis on functional brain networks of different kinds of decision-making identified the thalamus, the caudate, and the cingulate to show reduced brain activity in SRAs (Poudel et al., 2020). It should be noted, however, that this meta-analysis included many studies employing paradigms which we do not consider in our review, such as the stop-signal task, which is an index for motor response inhibition rather than for decision making under risk or uncertainty. Moreover, the current literature is lacking an overview on risk-taking in individuals with NSRAs and comparisons between different addiction types.
The core of this comparative review is, therefore, to explore differences and similarities in neural correlates of risk-related decisions between SRAs and NSRAs. In NSRAs, phenotypic features and neural alterations are – in contrast to SRAs – not confounded by pharmacological effects of drugs, which cause additional neural changes (Goldstein & Volkow, 2011). Specifically, the objectives of this review are (1) to summarize neural correlates of risk-related decision-making in SRAs and NSRAs separately, and (2) to provide a preliminary investigation of commonalities and differences in neural correlates of risk-taking decision-making in individuals with SRAs and in individuals with NSRAs.
Method
This review was not pre-registered and was conducted adhering to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Mohr et al., 2010). A systematic literature search of the scientific databases PubMed and Web of Science, including all available empirical studies until January 2022, was conducted to find articles on functional neuroimaging studies investigating risky and uncertain decision-making in addictive disorders. Studies fulfilling inclusion criteria were identified by one author searching the databases after applying search terms, filters and exclusion criteria (see Table 1). In addition, reference lists of identified records were used to identify additional studies. Duplicates were removed, and titles and abstracts of remaining records were screened. In the present review, we consider studies investigating decision-making where outcome probabilities are tied to different choice options (i.e., are not random) and are either known (i.e., decisions under risk) or unknown (i.e., decisions under uncertainty) to participants. Finally, decisions should have rewarding or punishing consequences. We focused on statistical contrasts between risky decisions versus safe decisions or control conditions of the decision phase (in case where studies differentiated between different task phases). We included studies with a primary focus on whole-brain analyses (ROI analysis may be conducted in addition). Please refer to Table 1 for all inclusion criteria. For the ease of reading, we refer to both decision-making under risk and decision-making under uncertainty as risk-related decisions or risk-taking.
Results
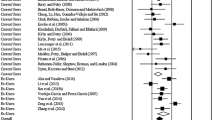
A total of 847 studies were screened. After exclusion, 109 studies were assessed for eligibility. Finally, 29 studies examining neural correlates of risk-taking in addictive disorders were included and reviewed. Results of the study selection process are presented in Fig. 1. Included studies employed a variety of prominent risk-taking paradigms and five self-developed tasks (see Table S1 of the supplementary online material for an overview and description of the different tasks). In all paradigms, positive trial outcomes were associated with monetary wins or virtual points. Negative trial outcomes were associated with either a deduction of money/points or had no consequences. The risk contrasts of the decision phase (focus of the current review) of the imaging analyses aggregated over positive and negative trial outcomes of the subsequent outcome phase.
Results of the present review are presented in two main sections. The first section presents findings on SRAs, and the second section presents findings on NSRAs which are compared to those of SRAs. In order to provide context, for each main section, we report findings on neural alterations in these groups stratified by studies reporting behavioral differences and studies which could not find any behavioral differences regarding risk-taking in comparison with controls. Each subsection is concluded by a brief summary of findings. Figure 2 compares findings on SRAs with those on NSRAs.
Altered risk-related brain activation patterns in individuals with a substance related addictions and b non-substance related addictions. Arrows indicate relative increase (↑) or decrease (↓) in brain activation compared to controls. c shows brain regions where substance related addictions and non-substance related addictions differ. Regions in brackets indicate mixed or limited evidence (< 3 studies reporting consistent alterations in this brain area)
Substance-related Addictions
Our review identified 19 eligible functional imaging studies which investigate risk-related decisions in SRAs compared to controls. A total of 648 individuals participated across all SRA studies. The number of included SRA individuals per study ranged from 11 to 75. Among the included studies, four studies were identified which did not include a healthy control group, but assessed the (longitudinal) relationship between clinical characteristics (e.g., symptom severity) and altered neural correlates during risk-taking (Blair et al., 2018; Forster et al., 2016, 2017; Gowin et al., 2014a). Approximately half (k = 7) of the reviewed studies examined risk-taking in individuals with stimulant addiction (k = 2 in cocaine addiction, k = 3 in methamphetamine addiction, and k = 2 in stimulant addiction, not further specified). Of the remaining studies, k = 3 studies investigated cannabis addiction, k = 2 studies investigated alcohol addiction and k = 5 studies did not report the exact addiction type or included mixed samples. Table 2 provides an overview of the study and sample characteristics of reviewed studies. Ten of the 19 studies reported increased risk-taking in individuals with SRAs, whereas nine of the 19 studies did not find any behavioral differences between individuals with SRAs and controls.
DLPFC and Extending Regions
Across different tasks and decision-making domains, activation within prefrontal areas, particularly within the right DLPFC (middle frontal gyrus) was decreased in individuals with SRAs (k = 6; Bolla et al., 2003; Bolla et al., 2005; Burnette et al., 2020; Ersche et al., 2005; Gilman et al., 2015; Kohno et al., 2014). Other prefrontal areas which were reported to show decreased risk-related brain activity in individuals with SRAs included the superior and medial frontal gyri (Bolla et al., 2003; Burnette et al., 2020; Gilman et al., 2015). Among the six studies reporting decreased risk-related DLPFC activity, only one study found increased behavioral risk-taking in the SRA group; the remaining studies did not find any behavioral differences between SRAs and HCs. One study reported increased middle frontal (DLPFC), and medial/superior frontal activity in individuals with SRAs (Yamamoto et al., 2014). Finally, a longitudinal study on SRA investigated substance use outcomes for a duration of three months and reported a positive correlation between substance use and activation in the supplementary motor area on the BART task (Forster et al., 2017).
ACC
Three studies reported a trend toward riskier behavior in individuals with SRAs on an uncertainty task (specifically, an increased frequency of risky decisions after losses) and also identified increased risk-related dorsal ACC activity (k = 3; Gowin et al., 2017, 2014b; Yamamoto et al., 2014). Interestingly, the studies conducted by Gowin et al. revealed that their control participants showed greater dorsal ACC activity during safe relative to risky choices whereas their SRAs groups either showed enhanced activity when they chose risky options or showed no differential activity for risky compared to safe choices. In addition, increased risk-related dorsal ACC activity seems to be related to greater symptom severity (Gowin et al., 2017). This finding is supported by a longitudinal study which tracked substance use in an SRA sample throughout a 3-month period. Improved substance use outcomes were related to a decreased risk-related response in the dorsal ACC (extending to the vmPFC; as well as in the putamen) at follow-up relative to a baseline assessment (Forster et al., 2016). Conversely, duration of use was negatively correlated with dorsal ACC activity (Vaidya et al., 2012).
Conversely, the ventral ACC showed decreased risk-related activity in the context of similar (Ersche et al., 2005) as well as increased behavioral risk-taking (Fishbein et al., 2005) in SRAs compared to HCs (k = 2). Both studies used the Cambridge Risk Task which measures decision-making under risk.
Insula/IFG
In total, k = 2 studies reported decreased risk-related brain activity in the anterior insula under uncertainty. Specifically, relapsed as opposed to abstinent individuals with SRAs showed blunted risk-related activity in the anterior insula (Gowin et al., 2014a). Furthermore, Fukunaga et al. (2013) identified regions which showed a difference in brain activation associated with risky relative to safe decisions. They further investigated regions showing such a difference and found that individuals with SRAs showed lower differential activity in the anterior insula that corresponded to greater risk-taking behavior.
Conversely, risk-related activity in the insula/mid insula was found to be increased in SRAs under uncertainty (k = 2; Gowin et al., 2014b; Yamamoto et al., 2014). Increased activity in the mid insula correlated with the frequency of risky choices after losses as well as with a longer substance use history (Gowin et al., 2014b).
OFC/vmPFC
Regions around the OFC/vmPFC were reported to exhibit increased risk-related activity in SRAs (k = 6; Bolla et al., 2003; Ersche et al., 2005; Tanabe et al., 2007; Vaidya et al., 2012; Yamamoto et al., 2014, 2017). Moreover, a positive relationship between risk-related OFC activity and duration of substance use (Vaidya et al., 2012) as well as symptom severity was reported (Fishbein et al., 2005). Of those, one study employed a decision-making under risk task, whereas the remaining studies employed the IGT (decision-making under uncertainty). Only one of the five studies that reported increased OFC activity also identified increased behavioral risk-taking in SRAs (during the IGT). A further study which found elevated levels of behavioral risk-taking (also employing the IGT), revealed decreased risk-related OFC activity in individuals with SRAs (Bolla et al., 2005).
Striatum
The ventral striatum as well as the putamen showed increased risk-related activity in SRAs in two studies where behavioral performance did not differ between SRAs and HCs under uncertainty (Bolla et al., 2003; Kohno et al., 2014). In addition, Yamamoto et al. (2014) found increased risk-related activity in the dorsal and ventral striatum, extending to the thalamus and the pallidum, paralleled by increased risk-taking in SRAs on the IGT. Thus, in total, k = 3 studies reported increased striatal activity in SRAs. Conversely, one study found decreased ventral striatal activity (caudate) in a sample of individuals with SRAs who exhibited increased risk-taking behavior after experiencing losses under uncertainty (k = 1; Gowin et al., 2017). The putamen seems to respond particularly in the context of rewards as shown by Gilman et al. (2015). These authors investigated the effect of accumulated rewards on risk-related brain activation. Specifically, they found that individuals with SRAs exhibit heightened activation in the putamen (in addition to the posterior cingulate, the precuneus, and the thalamus) that correlated with the total accumulated reward during decisions under uncertainty (Gilman et al., 2015). Correspondingly, a longitudinal study on individuals with SRAs reported decreased putamen (as well as decreased dorsal ACC) activity at follow-up relative to a baseline assessment to correlate with less substance use during the study interval (Forster et al., 2016).
Parietal Lobe
In total, k = 3 studies revealed increased risk-related activity of the postcentral gyrus/posterior parietal lobe under uncertainty (Bolla et al., 2003, 2005; Yamamoto et al., 2014). Two of those, also reported increased behavioral risk-taking in the SRA group, while the other study found no elevated risk-taking. In addition, Yamamoto et al. (2014) reported increased superior parietal activity, while Bolla et al. (2003) found decreased activity in the superior parietal lobe in their SRA group. The precuneus, a neighboring region of the superior parietal lobe also seems to be involved in risk processing. One study reported increased risk-related precuneus activity in SRAs compared to controls (Yamamoto et al., 2014). In addition, Blair et al. (2018) conducted a longitudinal study on stimulant users and investigated whether risk-related brain activity differentiated occasional stimulant users who became problem stimulant users from those who desisted from stimulant use. Those who became problem users showed greater precuneus and (posterior cingulate) activity during risk-related decisions as opposed to those participants who desisted from use. Similarly, Gilman et al. (2015) reported increased activation in the precuneus (in addition to the posterior cingulate, the thalamus, and the putamen) that correlated with total accumulated reward during risk-taking under uncertainty (Gilman et al., 2015).
Temporal Lobe
Three (decision-making under uncertainty) studies that included a HC group reported risk-related alterations in the temporal lobe in SRAs. All used the IGT task. Alterations included decreased activity in the middle temporal gyrus (Bolla et al., 2003), and decreased (Vaidya et al., 2012) as well as increased activity in the superior temporal gyrus (Yamamoto et al., 2014). A longitudinal study on a SRA-only group reported increased risk-related activity in the middle temporal as well as inferior temporal gyrus on the IGT to be associated with an increase in substance use after 6 months (Cousijn et al., 2013). Similarly, another longitudinal study on individuals with SRAs found a longitudinal decrease in substance use over a 3-month period to correlate with less activity in the middle temporal gyrus (Forster et al., 2016). Both longitudinal studies used decision-making under uncertainty tasks.
Additional Areas
One study reported increased risk-related activity in the cuneus (Yamamoto et al., 2014) and k = 4 studies identified altered activity in the cerebellum on the IGT. Of those, three studies reported increased cerebellar activity (Bolla et al., 2005; Vaidya et al., 2012; Yamamoto et al., 2014) and one reported decreased cerebellar activity (Bolla et al., 2003).
Summary
Among studies which investigated risk-related decision-making in SRAs, convergent attenuated brain activity was reported for prefrontal areas, especially the right DLPFC. This finding seems to be independent of risk-taking behavior, as it was reported by studies which observed behavioral differences in risk-related decision-making and studies which did not observe such differences. Results further point to a hyperactivation of the OFC/vmPFC and associations between OFC hyperactivity and symptom severity across several studies. Moreover, some evidence suggests risk-related alterations in additional brain areas, including the posterior cingulate cortex, the precuneus and the postcentral gyrus which show increased activity across studies, and also show associations to reward. While results point to decreased risk-related activity in the anterior insula, risk-related activity may be increased in the mid insula. Results regarding the (dorsal) striatum and the dorsal ACC point to elevated risk-related brain activity. Increased dorsal ACC activity was mostly reported by studies which could also show trends towards increased behavioral risk-taking or could show associations to clinical symptoms. In contrast, activity in the ventral ACC may be decreased in SRAs. Findings on the temporal lobe are mixed but point to a positive relationship between activity in the middle temporal lobe and a longitudinal increase in substance use.
Non-substance Related Addictions
In total, 10 studies investigated neural correlates of risk-related decisions in individuals with NSRAs, with k = 6 studies on individuals with Internet Gaming Disorder (IGD) and k = 4 studies on Pathological Gambling. Of those, seven studies did find elevated levels of behavioral risk-taking in individuals with NSRAs, whereas three studies could not find any behavioral differences regarding risk-taking behavior in NSRAs relative to controls. A total of 187 individuals participated across all NSRA studies. The number of included NSRA individuals per study ranged from 8 to 41. Table 2 provides an overview of study and sample characteristics of reviewed studies. No symptom-severity-relationships were reported by any of these studies.
DLPFC and Extending Regions
Decreased risk-related brain activity in the DLPFC could only be identified by one study (Liu et al., 2017). In this study, participants chose between a safe and a risky option (decision-making under risk task), either in a gain domain, where they should win as much money as possible or in a loss domain, where they should avoid losing money. Parametric analyses revealed decreased activation in the DLPFC (and the inferior parietal lobe/precuneus) in individuals with Internet Gaming Disorder compared to controls – only for the loss domain. No group differences were found for the gain domain. It should be noted that all other studies reviewed here employed tasks, where participants played for potential gains. In addition, decreased frontal activity was reported for the medial frontal gyrus (k = 1; Wang et al., 2017) as well as the precentral gyrus (k = 2; Lin et al., 2015; Wang et al., 2017). These studies revealed increased risk-taking behavior in individuals with NSRAs on probability discounting tasks (decision-making under risk).
The superior frontal gyrus was reported to show increased risk-related activity in k = 2 decision-making under uncertainty studies. Increased risk-taking in NSRAs was reported only by one of these studies (Power et al., 2012) but not by the other (Miedl et al., 2014).
ACC
Decreased brain activation under risk was reported for the ventral ACC which was accompanied by increased behavioral risk-taking in individuals with NSRAs (k = 1; Dong & Potenza, 2016).
In contrast, increased brain activation was identified for the dorsal ACC during a decision-making under risk task (k = 1; Seok et al., 2015). This study also revealed increased risk-taking behavior.
Insula/IFG
A total of k = 5 studies identified decreased risk-related activity in the left IFG/ventrolateral prefrontal cortex in NSRAs (Dong & Potenza, 2016; Lin et al., 2015; Liu et al., 2017; Seok et al., 2015; Wang et al., 2017). All, but one study used decision-making under risk tasks and revealed increased behavioral risk-taking in individuals with NSRAs. The study which could not reveal increased risk-taking employed the Cups Task (decision making under risk) and – as mentioned before – reported effects for conditions focusing on loss avoidance (Liu et al., 2017). In contrast, in a decision-making under uncertainty setting which did not reveal any behavioral differences between individuals with NSRAs and HCs, right IFG activity seems to be increased (k = 1; Miedl et al., 2010).
OFC/vmPFC
In total, k = 3 studies (k = 2 decision-making under uncertainty and k = 1 decision-making under risk) revealed increased OFC/vmPFC activity in individuals with NSRAs. Of those, two studies investigated decision-making under uncertainty (Miedl et al., 2014; Power et al., 2012) and one study investigated decision-making under risk (Liu et al., 2017).
Striatum
Increased striatal activity in individuals with NSRAs was reported by k = 4 studies. All of them also reported increased risk-taking in NSRAs. The dorsal striatum (putamen and well as caudate nucleus) showed increased activity in k = 3 studies (under risk as well as uncertainty; Brevers et al., 2015; Power et al., 2012; Seok et al., 2015). Moreover, the adjacent nucleus accumbens (ventral striatum) showed increased activity under risky decision-making (k = 1; Wang et al., 2021).
Parietal Lobe
The inferior parietal lobe/the precuneus showed reduced activity in k = 2 studies (Dong & Potenza, 2016; Liu et al., 2017). Specifically, Liu et al. (2017) could not identify any behavioral alterations during a decision-making under risk task in their NRA group. Moreover, as mentioned above, they could not find any group differences when their participants played for potential gains – only when they played to avoid losses. Dong and Potenza (2016) reported less activation in the inferior partial lobe (and the posterior cingulate cortex) along with increased risk-taking behavior in individuals with NSRAs during a decision-making under uncertainty task. In contrast, one study identified increased precuneus activity and increased risk-taking behavior under risky decision-making (Wang et al., 2021).
Temporal Lobe
Findings on the temporal lobe are mixed. In total, k = 3 studies reported altered risk-related temporal activity. Specifically, Dong and Potenza (2016) reported decreased superior temporal and middle temporal activity (accompanied by increased behavioral risk-taking). In contrast, Miedl et al. (2010) reported increased superior temporal activity and Wang et al. (2021) reported increased middle temporal activity.
Additional Areas
In addition, k = 2 studies identified increased risk-related activity in the thalamus during decision-making under uncertainty (Miedl et al., 2010, 2014). Power et al. (2012) employed the IGT (decision-making under uncertainty) and reported increased activity in the amygdala and in the brainstem which was accompanied by increased risk-taking. Finally, several studies (k = 3) reported decreased activity in occipital brain regions for decisions under risk (k = 2; Dong & Potenza, 2016; Liu et al., 2017) and under uncertainty (k = 1; Power et al., 2012). In contrast, one study found increased activity in the middle occipital gyrus under risk (Wang et al., 2021).
Summary
Taken together, studies on risk-related decision-making in individuals with NSRAs reported widespread activation differences compared to controls. Concordant alterations point to hypoactivity in the inferior frontal cortex and hyperactivity in the OFC/vmPFC in both those studies reporting increased behavioral risk-taking in NSRAs and those studies which did not report such behavioral differences. In contrast, (dorsal) striatal hyperactivity was only reported by studies that also found increased behavioral risk-taking. Additional preliminary evidence points to hyperactivity of the thalamus, the dorsal ACC and hypoactivity of the ventral ACC. Findings regarding further brain areas are rather mixed.
Compared to studies on SRAs, this review identified both overlapping and specific brain activation patterns for NSRAs. These preliminary findings suggest concordant alterations in SRAs and NSRAs in the OFC/vmPFC and the striatum. These regions show increased activity in both addiction types during risk-related decisions. Across studies, increased activity could be identified in both SRAs and NSRAs, irrespective of behavioral task performance. Increased dorsal ACC activity was also reported for both addiction types, but only in studies which also revealed relationships to behavioral risk-taking. In contrast, studies that identified neural alterations in the ventral ACC revealed decreased activity in both addiction groups. Interestingly, the postcentral gyrus, posterior cingulate and precuneus activity seem to be increased in SRAs. In contrast, activity in these regions seem to be decreased in NSRAs. We could also identify differing risk-related patterns of brain activity for the two addiction types. A finding specific to SRA studies is decreased right DLPFC activity, whereas left IFG activity was mostly reported by NSRA studies. To clarify if frontal areas that altered in NSRAs are distinct from the DLPFC, we extracted reported brain coordinates and overlaid them with a DLPFC mask (see supporting information Fig. S1). This underlined that reduced DLPFC activity may only occur in individuals with SRAs.
Discussion
We here examined neural correlates of risk-related decision making in individuals with SRAs and individuals with NSRAs. Furthermore, we aimed to provide preliminary comparative results of these two groups to identify overlapping as well as differing alterations in neural correlates of risk-related decision-making. This approach is in line with the Research Domain Criteria principle of studying mental disorders beyond their diagnostic boundaries (Cuthbert & Insel, 2013).
Although currently available studies on risk-related decision-making, especially in the domain of NSRAs, are sparse, we did find interesting similarities and differences between the two addiction types that may be further validated by future studies. One difference relates to alterations in posterior cingulate and precuneus activation. These areas may be affected by both SRAs and NSRAs. However, while activity in these regions seems to be increased in SRAs, the activity appears to be decreased in NSRAs. Activity in these regions in response to risky situations has also been observed in normative samples (Paulus et al., 2003; Roy et al., 2011) and it has been suggested that these regions may be involved in tracking risky subjective value and may provide a willingness to accept uncertain outcomes for a chance to receive greater rewards (Coutlee et al., 2016). Interestingly, decreased precuneus/inferior parietal lobe activation in NSRAs was reported, amongst others, for situations where participants played to avoid losses. This experimental situation differs from all other studies reviewed here, which all employed tasks where participants play for potential gains. Future studies may ascertain whether individuals with SRAs also show increased precuneus/inferior parietal lobe activation under loss avoidance situations. The precuneus and the posterior cingulate cortex are part of the default mode network, which is active during self-referential processes, such as self-awareness and self-reflection (Andrews-Hanna, 2012). A review on the involvement of different brain networks in different addiction cycles concluded that default mode network activity was decreased during decision-making tasks in individuals with SRAs (Zilverstand et al., 2018). This stands in contrast to results of our review suggesting increased default mode network activity. It should be noted that the review by Zilverstand et al. (2018) included studies which focus on outcome-processing (i.e., loss evaluation), whereas our review focuses on the actual decision stage. Together with our findings on NSRAs, it may be speculated that default mode network activity may be increased during risk-related decisions and decreased under loss evaluation conditions in addiction. However, this speculation needs to be further investigated.
Another area of divergence relates to the inferior frontal gyrus (IFG). Compared to HCs, neural activity during risk-taking in this brain region is reduced in individuals with NSRAs. Our systematic review could not find any evidence for altered patterns of IFG activity in SRAs. However, we did find reduced activity in the anterior insula, a region adjacent to the IFG, in SRAs. The anterior insula is often coactivated with the IFG and reviewed studies may have detected and reported peak activation only for one of the regions. Activity in the IFG/anterior insula is modulated by individual risk processing and more specifically by risk/harm avoidance (Christopoulos et al., 2009; Fukunaga et al., 2018; Paulus et al., 2003; Preuschoff et al., 2006). Interestingly, studies that reported diminished IFG activity in NSRAs all used decision-making under risk tasks and reported increased risk-taking behavior. The majority of studies on SRAs employed decision-making under uncertainty tasks and, mostly, could not reveal altered risk-taking behavior. One of the reviewed studies that reported diminished activity in the anterior insula, extending to the IFG also found increased risk-taking behavior in their SRA group. In fact, they reported a link between risk behavior and anterior insula activity where task performance of the SRA group reflects lower risk-aversion signals in the anterior insula/IFG (Fukunaga et al., 2013). The extent to which diminished IFG activity in NSRAs may relate to task properties, risk perception, or another factor specific to individuals with NSRAs remains to be further investigated.
The dorsal ACC is closely connected to the anterior insula/IFG and is also implicated in a wealth of functions during decision-making, such as signaling error and reward (Alexander & Brown, 2019), as well as the value of behavioral change and individuals risk tendencies (Fukunaga et al., 2018; Kolling et al., 2012, 2016). For both addiction types, findings regarding the dorsal ACC point to increased activity, which was always accompanied by increased behavioral risk-taking. As suggested elsewhere, for SRAs the dorsal ACC may fail to integrate outcomes into an online prediction of what will happen for each choice, which leads to repeatedly choosing disadvantageous options (Gowin et al., 2017). Additionally, increased dorsal ACC activity may be related to symptom severity in SRAs.
Another difference in findings regards the DLPFC. Hypoactivation of the right DLPFC was characteristic of SRAs during risk-related decisions across a variety of different tasks. DLPFC hypoactivation in SRAs has been identified before in previous reviews (Gowin et al., 2013) and it has been suggested that structural and functional alterations in the DLPFC may originate from severe drug use (Bolla et al., 2005). This is supported by structural imaging studies reporting reduced prefrontal grey matter density in several SRAs, including alcohol, cocaine, methamphetamine, and heroin addiction (Goldstein & Volkow, 2011). The right DLPFC plays a rather specific role in risk-related decision-making and is involved in valuing and integrating choice options before making a decision (Ernst & Paulus, 2005; Mohr et al., 2010). Moreover, it has been argued that DLPFC activity during value-based processes cannot be attributed entirely to a strict “cognitive” role. In fact, it may represent value information in relation to cognitive information (e.g., task-rules) providing a top-down control on core value regions (Dixon & Christoff, 2014). Interestingly, areas belonging to the brain’s valuation system such as the vmPFC, the striatum as well as the posterior cingulate show increased brain activation in studies reporting decreased DLPFC activity (c.f. Table 2), supporting the notion of a potential top-down influence of the DLPFC on the value system. However, this is an associative observation and may be tested by connectivity analyses. Attenuated risk-related activity in the DLPFC may thus lead to a devaluation of disadvantageous stimuli during decision-making in SRAs and to a reduced top-down influence on core value regions. We could only identify sparse evidence for reduced risk related (right) DLPFC activity in NSRAs. Due to paucity of data, firm conclusions, however, cannot be drawn about functional DLFPC reactivity in response to risk-related decision-making in NSRAs. Further research is needed in order to clarify whether individuals with NSRAs are able to recruit the DLPFC during risk-related decision making or not.
As mentioned above, results of the current review point to increased striatal as well as OFC activity under risky situations in SRAs but also in NSRAs. Areas adjacent to the striatum such as the thalamus and the globus pallidus also seem to show increased risk-related activity as reported by some studies. These findings represent a similarity across addiction types and suggest that alterations in these brain areas may be implicated in the psychopathology of addictive disorders. The striatum and the vmPFC have been ascribed to the brain’s core value system. In the neuroscientific literature, it is well established that they represent reward and preference and automatically track subjective value across different contexts (Bartra et al., 2013; Clithero & Rangel, 2014; Levy & Glimcher, 2012; Schmidt et al., 2017). In addition to its role in tracking subjective value during value-based decisions, the striatum (especially the dorsal striatum) has been associated with action-contingent learning in addiction and has been implicated in the transition from recreational to chronic use (Everitt & Robbins, 2013). Moreover, frontostriatal loops that initially involve the ventral striatum may progressively transition to recruit more dorsal parts of the striatum in SRAs and other impulse control disorders (Brewer & Potenza, 2008).
Increased OFC/vmPFC as well as striatal activation in addictive disorders are in line with the general notion of an increased reward sensitivity (Balodis & Potenza, 2015; García-García et al., 2014; Luijten et al., 2017) and an overvaluation of rewarding stimuli in addiction (Schultz, 2011). Recently, the OFC has been conceptualized as providing a cognitive map of task/state space that enables inference of relationships that are not directly observed (Murray & Rudebeck, 2018; Stalnaker et al., 2015; Wilson et al., 2014; Yu et al., 2020). Such a neural representation of stimuli, actions, value, and other sensory features could explain OFC’s role in decision-making as a comparison of different values at each task state which may be over-valuated in addiction. Rewarding stimuli may include disorder-specific stimuli as well as secondary rewards (e.g., money). Importantly, this seems to be true for the anticipation of rewards, or in the case of risk-taking, the decision phase as identified by this review. In contrast, studies focusing on reward delivery suggest that individuals with SRAs exhibit a neural overvaluation of drug-related rewards and an undervaluation of nondrug rewards in response to reward reception (Gradin et al., 2014); albeit studies on neural responses to secondary rewards are somewhat inconclusive (Balodis & Potenza, 2015).
A further similarity corresponds to findings regarding the ventral ACC, although studies reporting risk-related alterations in this area are scare. Specifically, activity in the ventral ACC seems to be attenuated in both addiction types, but especially in SRAs. The ventral ACC is involved in hedonic evaluation during decision-making (Bush et al., 2000; Park et al., 2011; Phan et al., 2002; Vogt et al., 2005). Animal studies on the ventral ACC show that it is implicated in maintaining heightened arousal in reward contexts (Rudebeck et al., 2014). Reduced processing of risky stimuli in SRAs and NSRAs may represent apathetic behavior seen in individuals with addictions. A study not included in this review also reported attenuated ventral ACC activity on occasional stimulant users (Reske et al., 2015). Ventral ACC activity may be, therefore, already altered in individuals not showing the full-blown symptomatology of addiction. This speculation needs to be further investigated in longitudinal or family studies.
Additional risk-related alterations in activity were reported by several studies and included temporal and occipital regions as well as the cerebellum. Data on these regions is, however, scarce and mixed regarding the direction of alterations. Therefore, no concluding evidence can be obtained.
Limitations, Implications and Future Directions
At this juncture, open questions remain and more research is needed in order to validate the preliminary findings gathered in this review. Interpretation of the results from this review are limited by several factors. The most important factors to note are (1) variability in methods (utilized tasks and neuroimaging approaches) and (2) heterogeneity in included disorders. Specifically, we compared different kind of tasks in different populations. While most SRA studies employed standard decision-making under uncertainty tasks (e.g., Balloon Analogue Risk Task, Iowa Gambling Task, Risky Gains Task; c.f. Table 2), the majority of NSRA studies used self-developed tasks and probability discounting tasks. Therefore, it is possible that the lack of evidence for altered DLPFC activity in NSRAs (and for altered IFG activity in SRAs) is related to differences in tasks used. Future studies may compare individuals with SRAs to those with NSRAs in one study in order to examine potential differences and similarities more directly. In particular, studies may use standardized tasks or a task battery and use these tasks in both addiction types, ideally in one study. Moreover, due to the sparsity of studies, we included both fMRI and PET studies. Although both methods measure cerebral blood flow, there are differences between the two methods. Most important to note is that fMRI usually has a higher resolution compared to PET imaging.
The second factor adding complexity to this review is the heterogeneity of included disorders. Specifically, we reviewed different SRA types, with different substances underlying the addiction, and with different substances expressing distinct psychopharmacological profiles. It is likely that these different SRAs may also have different neural profiles (depending on pharmacological properties of the specific substance), which we could not identify in this review.
Moreover, most reviewed studies were cross-sectional in nature. More longitudinal studies are needed in order to investigate whether alterations in risky decision-making processes are a cause or a consequence of addictive disorders. In addition, within-subject designs may also reveal predictors for relapse or recovery as shown by the study conducted by Blair et al. (2018).
It should also be noted that our conclusions are based on a small number of studies. We identify a lack of studies specifically with regard to investigating neural correlates of NSRAs. Therefore, meta-analytic techniques in order to quantitatively support our conclusions could not be applied. Future single studies as well as study syntheses may focus on brain networks related to risk-related decision-making in addiction. For example, several single fMRI studies as well as reviews on brain structure point to an aberrant frontostriatal network in SRAs (Hampton et al., 2019; Jentsch & Taylor, 1999; Suckling & Nestor, 2017). It may be of interest to investigate different networks under risky situations.
Future studies may also investigate potential differences between decisions under risk and decisions under uncertainty in these populations. In the current review, we could not identify alterations specific to either risk-taking type, which may be owed to the sparsity of studies (c.f. Table 2). Further task properties may also influence risk-related brain activation. For example, the presence of potential losses may yield different brain activation patterns compared to situations where negative trial outcomes have no consequences at all or only lead to smaller positive gains compared to positive trial outcomes. In healthy individuals, the possibility of facing losses indeed modulates brain activity (Mohr et al., 2010). It is beyond the scope of this review to investigate such potential task effects which are worth investigating in addiction in the future. An overview on identified limitations and suggestions for future directions may be found in Table 3.
Conclusions
This systematic review highlights similarities and differences in neural correlates of risk-related decision-making between different addiction types (SRAs and NSRAs). Here, we gather exploratory evidence of altered risk-related processes, including hyperactivity in the OFC and the striatum in both addiction types. As characteristic for both addiction types, these brain regions may represent an underlying mechanism of suboptimal decision-making. In contrast, decreased DLPFC activity may be specific to SRAs and decreased IFG activity could only be identified for NSRAs. While findings regarding the precuneus and posterior cingulate point to elevated risk-related activity in SRAs, findings regarding these regions are mixed but rather point to attenuated activation patterns in NSRAs. Additional scarce evidence suggests decreased ventral ACC activity and increased dorsal ACC activity in both addiction types. However, these preliminary findings should be interpreted with caution due to a lack of studies is this field. Future research is needed to evaluate the findings gathered by this review.
Availability of Data and Material
All of the reviewed studies are publicly available.
Code Availability
Not applicable.
References
Alexander, W. H., & Brown, J. W. (2019). The role of the anterior cingulate cortex in prediction error and signaling surprise. Topics in Cognitive Science, 11(1), 119–135. https://doi.org/10.1111/TOPS.12307
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
Andrews-Hanna, J. R. (2012). The brain’s default network and its adaptive role in internal mentation. The Neuroscientist, 18(3), 251–270. https://doi.org/10.1177/1073858411403316
Balodis, I. M., & Potenza, M. N. (2015). Anticipatory reward processing in addicted populations: a focus on the monetary incentive delay task. Biological Psychiatry, 77(5), 434–444. https://doi.org/10.1016/j.biopsych.2014.08.020
Bartra, O., McGuire, J. T., & Kable, J. W. (2013). The valuation system: A coordinate-based meta-analysis of BOLD fMRI experiments examining neural correlates of subjective value. NeuroImage, 76, 412–427. https://doi.org/10.1016/j.neuroimage.2013.02.063
Bizzarri, J., Rucci, P., Vallotta, A., Girelli, M., Scandolari, A., Zerbetto, E., Sbrana, A., Iagher, C., & Dellantonio, E. (2005). Dual diagnosis and quality of life in patients in treatment for opioid dependence. Substance Use & Misuse, 40(12), 1765–1776. https://doi.org/10.1080/10826080500260800
Black, D. W., Shaw, M., McCormick, B., & Allen, J. (2013). Pathological gambling: Relationship to obesity, self-reported chronic medical conditions, poor lifestyle choices, and impaired quality of life. Comprehensive Psychiatry, 54(2), 97–104. https://doi.org/10.1016/j.comppsych.2012.07.001
Blair, M. A., Stewart, J. L., May, A. C., Reske, M., Tapert, S. F., & Paulus, M. P. (2018). Blunted frontostriatal blood oxygen level-dependent signals predict stimulant and marijuana use. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 3(11), 947–958. https://doi.org/10.1016/j.bpsc.2018.03.005
Bolla, K. I., Eldreth, D. A., London, E. D., Kiehl, K. A., Mouratidis, M., Contoreggi, C., Matochik, J. A., Kurian, V., Cadet, J. L., Kimes, A. S., Funderburk, F. R., & Ernst, M. (2003). Orbitofrontal cortex dysfunction in abstinent cocaine abusers performing a decision-making task. NeuroImage, 19(3), 1085–1094. https://doi.org/10.1016/S1053-8119(03)00113-7
Bolla, K. I., Eldreth, D. A., Matochik, J. A., & Cadet, J. L. (2005). Neural substrates of faulty decision-making in abstinent marijuana users. NeuroImage, 26(2), 480–492. https://doi.org/10.1016/j.neuroimage.2005.02.012
Brevers, D., Bechara, A., Hermoye, L., Divano, L., Kornreich, C., Verbanck, P., & Noel, X. (2015). Comfort for uncertainty in pathological gamblers: A fMRI study. Behavioural Brain Research, 278, 262–270. https://doi.org/10.1016/j.bbr.2014.09.026
Brewer, J. A., & Potenza, M. N. (2008). The neurobiology and genetics of impulse control disorders: Relationships to drug addictions. Biochemical Pharmacology, 75(1), 63–75. https://doi.org/10.1016/j.bcp.2007.06.043
Burnette, E. M., Grodin, E. N., Ghahremani, D. G., Galván, A., Kohno, M., Ray, L. A., & London, E. D. (2020). Diminished cortical response to risk and loss during risky decision making in alcohol use disorder. Drug and Alcohol Dependence. https://doi.org/10.1016/j.drugalcdep.2020.108391
Bush, G., Luu, P., & Posner, M. I. (2000). Cognitive and emotional influences in anterior cingulate cortex. Trends in Cognitive Sciences, 4(6), 215–222. https://doi.org/10.1016/S1364-6613(00)01483-2
Christopoulos, G. I., Tobler, P. N., Bossaerts, P., Dolan, R. J., & Schultz, W. (2009). Neural correlates of value, risk, and risk aversion contributing to decision making under risk. Journal of Neuroscience, 29(40), 12574–12583. https://doi.org/10.1523/JNEUROSCI.2614-09.2009
Clithero, J. A., & Rangel, A. (2014). Informatic parcellation of the network involved in the computation of subjective value. Social Cognitive and Affective Neuroscience, 9(9), 1289–1302. https://doi.org/10.1093/scan/nst106
Collins, D., Lapsley, H., Lecavalier, J., & Single, E. (2000). Introduction: Improving economic data to inform decisions in drug control. Bulletin On Narcotics, 52, 1–20. https://www.unodc.org/unodc/en/data-and-analysis/bulletin/bulletin_2000-01-01_1_page003.html
Cousijn, J., Wiers, R. W., Ridderinkhof, K. R., van den Brink, W., Veltman, D. J., Porrino, L. J., & Goudriaan, A. E. (2013). Individual differences in decision making and reward processing predict changes in cannabis use: A prospective functional magnetic resonance imaging study. Addiction Biology, 18(6), 1013–1023. https://doi.org/10.1111/j.1369-1600.2012.00498.x
Coutlee, C. G., Kiyonaga, A., Korb, F. M., Huettel, S. A., & Egner, T. (2016). Reduced risk-taking following disruption of the intraparietal sulcus. Frontiers in Neuroscience, 10(DEC), 588. https://doi.org/10.3389/fnins.2016.00588
Cuthbert, B. N., & Insel, T. R. (2013). Toward the future of psychiatric diagnosis: The seven pillars of RDoC. BMC Medicine, 11(1), 126. https://doi.org/10.1186/1741-7015-11-126
Dixon, M. L., & Christoff, K. (2014). The lateral prefrontal cortex and complex value-based learning and decision making. Neuroscience & Biobehavioral Reviews, 45, 9–18. https://doi.org/10.1016/j.neubiorev.2014.04.011
Dong, G., & Potenza, M. N. (2016). Risk-taking and risky decision-making in Internet gaming disorder: Implications regarding online gaming in the setting of negative consequences. Journal of Psychiatric Research, 73(November 2015), 1–8. https://doi.org/10.1016/j.jpsychires.2015.11.011
Ernst, M., & Paulus, M. P. (2005). Neurobiology of decision making: A selective review from a neurocognitive and clinical perspective. Biological Psychiatry, 58(8), 597–604. https://doi.org/10.1016/j.biopsych.2005.06.004
Ersche, K. D., Fletcher, P. C., Lewis, S. J. G., Clark, L., Stocks-Gee, G., London, M., Deakin, J. B., Robbins, T. W., & Sahakian, B. J. (2005). Abnormal frontal activations related to decision-making in current and former amphetamine and opiate dependent individuals. Psychopharmacology (berl), 180(4), 612–623. https://doi.org/10.1007/s00213-005-2205-7
Everitt, B. J., & Robbins, T. W. (2013). From the ventral to the dorsal striatum: Devolving views of their roles in drug addiction. Neuroscience & Biobehavioral Reviews, 37(9), 1946–1954. https://doi.org/10.1016/j.neubiorev.2013.02.010
Fishbein, D. H., Eldreth, D. L., Hyde, C., Matochik, J. A., London, E. D., Contoreggi, C., Kurian, V., Kimes, A. S., Breeden, A., & Grant, S. (2005). Risky decision making and the anterior cingulate cortex in abstinent drug abusers and nonusers. Cognitive Brain Research, 23(1), 119–136. https://doi.org/10.1016/j.cogbrainres.2004.12.010
Forster, S. E., Finn, P. R., & Brown, J. W. (2016). A preliminary study of longitudinal neuroadaptation associated with recovery from addiction. Drug and Alcohol Dependence, 168, 52–60. https://doi.org/10.1016/j.drugalcdep.2016.08.626
Forster, S. E., Finn, P. R., & Brown, J. W. (2017). Neural responses to negative outcomes predict success in community-based substance use treatment. Addiction, 112(5), 884–896. https://doi.org/10.1111/add.13734
Fukunaga, R., Bogg, T., Finn, P. R., & Brown, J. W. (2013). Decisions during negatively-framed messages yield smaller risk-aversion-related brain activation in substance-dependent individuals. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors, 27(4), 1141–1152. https://doi.org/10.1037/a0030633
Fukunaga, R., Purcell, J. R., & Brown, J. W. (2018). Discriminating formal representations of risk in anterior cingulate cortex and inferior frontal gyrus. Frontiers in Neuroscience, 12, 553. https://doi.org/10.3389/fnins.2018.00553
García-García, I., Horstmann, A., Jurado, M. A., Garolera, M., Chaudhry, S. J., Margulies, D. S., Villringer, A., & Neumann, J. (2014). Reward processing in obesity, substance addiction and non-substance addiction. Obesity Reviews, 15(11), 853–869. https://doi.org/10.1111/obr.12221
Gilman, J. M., Smith, A. R., Bjork, J. M., Ramchandani, V. A., Momenan, R., & Hommer, D. W. (2015). Cumulative gains enhance striatal response to reward opportunities in alcohol-dependent patients. Addiction Biology, 20(3), 580–593. https://doi.org/10.1111/adb.12147
Goldstein, R. Z., & Volkow, N. D. (2011). Dysfunction of the prefrontal cortex in addiction: Neuroimaging findings and clinical implications. Nature Reviews Neuroscience, 12(11), 652–669. https://doi.org/10.1038/nrn3119
Gowin, J. L., Harlé, K. M., Stewart, J. L., Wittmann, M., Tapert, S. F., & Paulus, M. P. (2014a). Attenuated insular processing during risk predicts relapse in early abstinent methamphetamine-dependent individuals. Neuropsychopharmacology, 39(6), 1379–1387. https://doi.org/10.1038/npp.2013.333
Gowin, J. L., Mackey, S., & Paulus, M. P. (2013). Altered risk-related processing in substance users: Imbalance of pain and gain. Drug and Alcohol Dependence, 132(1–2), 13–21. https://doi.org/10.1016/j.drugalcdep.2013.03.019
Gowin, J. L., May, A. C., Wittmann, M., Tapert, S. F., & Paulus, M. P. (2017). Doubling down: Increased risk-taking behavior following a loss by individuals with cocaine use disorder is associated with striatal and anterior cingulate dysfunction. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 2(1), 94–103. https://doi.org/10.1016/j.bpsc.2016.02.002
Gowin, J. L., Stewart, J. L., May, A. C., Ball, T. M., Wittmann, M., Tapert, S. F., & Paulus, M. P. (2014b). Altered cingulate and insular cortex activation during risk-taking in methamphetamine dependence: Losses lose impact. Addiction, 109(2), 237–247. https://doi.org/10.1111/add.12354
Gradin, V. B., Baldacchino, A., Balfour, D., Matthews, K., & Steele, J. D. (2014). Abnormal brain activity during a reward and loss task in opiate-dependent patients receiving methadone maintenance Therapy. Neuropsychopharmacology, 39(4), 885–894. https://doi.org/10.1038/npp.2013.289
Grant, B. F., Goldstein, R. B., Saha, T. D., Patricia Chou, S., Jung, J., Zhang, H., Pickering, R. P., June Ruan, W., Smith, S. M., Huang, B., & Hasin, D. S. (2015). Epidemiology of DSM-5 alcohol use disorder results from the national epidemiologic survey on alcohol and related conditions III. JAMA Psychiatry, 72(8), 757–766. https://doi.org/10.1001/jamapsychiatry.2015.0584
Grant, B. F., Saha, T. D., June Ruan, W., Goldstein, R. B., Patricia Chou, S., Jung, J., Zhang, H., Smith, S. M., Pickering, R. P., Huang, B., & Hasin, D. S. (2016). Epidemiology of DSM-5 drug use disorder results from the national epidemiologic survey on alcohol and related conditions-III. JAMA Psychiatry, 73(1), 39–47. https://doi.org/10.1001/jamapsychiatry.2015.2132
Hampton, W. H., Hanik, I. M., & Olson, I. R. (2019). Substance abuse and white matter: Findings, limitations, and future of diffusion tensor imaging research. In Drug and Alcohol Dependence (Vol. 197, pp. 288–298). Elsevier Ireland Ltd. https://doi.org/10.1016/j.drugalcdep.2019.02.005
Hertwig, R., Wulff, D. U., & Mata, R. (2019). Three gaps and what they may mean for risk preference. Philosophical Transactions of the Royal Society b: Biological Sciences, 374(1766), 20180140. https://doi.org/10.1098/rstb.2018.0140
Hommer, D. W., Bjork, J. M., & Gilman, J. M. (2011). Imaging brain response to reward in addictive disorders. Annals of the New York Academy of Sciences, 1216(1), 50–61. https://doi.org/10.1111/j.1749-6632.2010.05898.x
Jentsch, J. D., & Taylor, J. R. (1999). Impulsivity resulting from frontostriatal dysfunction in drug abuse: Implications for the control of behavior by reward-related stimuli. In Psychopharmacology (Vol. 146, Issue 4, pp. 373–390). Springer. https://doi.org/10.1007/PL00005483
Knight, F. H. (1921). Risk, Uncertainty and Profit. Houghton Mifflin. https://books.google.de/books?id=Im2dnQAACAAJ&pg=PR5&hl=de&source=gbs_selected_pages&cad=2#v=onepage&q&f=false
Kohno, M., Morales, A. M., Ghahremani, D. G., Hellemann, G., & London, E. D. (2014). Risky decision making, prefrontal cortex, and mesocorticolimbic functional connectivity in methamphetamine dependence. JAMA Psychiatry, 71(7), 812–820. https://doi.org/10.1001/jamapsychiatry.2014.399
Kolling, N., Behrens, T. E. J., Mars, R. B., & Rushworth, M. F. S. (2012). Neural mechanisms of foraging. Science, 336(6077), 95–98. https://doi.org/10.1126/science.1216930
Kolling, N., Wittmann, M. K., Behrens, T. E. J., Boorman, E. D., Mars, R. B., & Rushworth, M. F. S. (2016). Value, search, persistence and model updating in anterior cingulate cortex. Nature Neuroscience, 19(10), 1280–1285. https://doi.org/10.1038/nn.4382
Krain, A. L., Wilson, A. M., Arbuckle, R., Castellanos, F. X., & Milham, M. P. (2006). Distinct neural mechanisms of risk and ambiguity: A meta-analysis of decision-making. NeuroImage, 32(1), 477–484. https://doi.org/10.1016/j.neuroimage.2006.02.047
Lawrence, A. J., Luty, J., Bogdan, N. A., Sahakian, B. J., & Clark, L. (2009). Problem gamblers share deficits in impulsive decision-making with alcohol-dependent individuals. Addiction, 104(6), 1006–1015. https://doi.org/10.1111/j.1360-0443.2009.02533.x
Levy, D. J., & Glimcher, P. W. (2012). The root of all value: A neural common currency for choice. Current Opinion in Neurobiology, 22(6), 1027–1038. https://doi.org/10.1016/j.conb.2012.06.001
Leyton, M., & Vezina, P. (2013). Striatal ups and downs: Their roles in vulnerability to addictions in humans. Neuroscience & Biobehavioral Reviews, 37(9), 1999–2014. https://doi.org/10.1016/j.neubiorev.2013.01.018
Lin, X., Zhou, H., Dong, G., & Du, X. (2015). Impaired risk evaluation in people with Internet gaming disorder: FMRI evidence from a probability discounting task. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 56, 142–148. https://doi.org/10.1016/j.pnpbp.2014.08.016
Liu, L., Xue, G., Potenza, M. N., Zhang, J.-T., Yao, Y.-W., Xia, C.-C., Lan, J., Ma, S.-S., & Fang, X.-Y. (2017). Dissociable neural processes during risky decision-making in individuals with Internet-gaming disorder. NeuroImage: Clinical, 14(November 2016), 741–749. https://doi.org/10.1016/j.nicl.2017.03.010
Lopez-Guzman, S., Konova, A. B., & Glimcher, P. W. (2019). Computational psychiatry of impulsivity and risk: How risk and time preferences interact in health and disease. Philosophical Transactions of the Royal Society b: Biological Sciences, 374(1766), 20180135. https://doi.org/10.1098/rstb.2018.0135
Luijten, M., Machielsen, M. W. J., Veltman, D. J., Hester, R., de Haan, L., & Franken, I. H. A. (2014). Systematic review of ERP and fMRI studies investigating inhibitory control and error processing in people with substance dependence and behavioural addictions. Journal of Psychiatry & Neuroscience : JPN, 39(3), 149–169. https://doi.org/10.1503/jpn.130052
Luijten, M., Schellekens, A. F., Kuehn, S., Machielse, M. W. J., & Sescousse, G. (2017). Disruption of reward processing in addiction an image-based meta-analysis of functional magnetic resonance imaging studies. JAMA PSYCHIATRY, 74(4), 387–398. https://doi.org/10.1001/jamapsychiatry.2016.3084
Mellers, B. A., Schwartz, A., & Weber, E. U. (1997). Do risk attitudes reflect in the eye of the beholder? In Choice, Decision, and Measurement: Essays in Honor of R. Duncan Luce (pp. 57–71). https://doi.org/10.4324/9781315789408-5
Miedl, S. F., Fehr, T., Herrmann, M., & Meyer, G. (2014). Risk assessment and reward processing in problem gambling investigated by event-related potentials and fMRI-constrained source analysis. BMC Psychiatry, 14(1), 229. https://doi.org/10.1186/s12888-014-0229-4
Miedl, S. F., Fehr, T., Meyer, G., & Herrmann, M. (2010). Neurobiological correlates of problem gambling in a quasi-realistic blackjack scenario as revealed by fMRI. Psychiatry Research: Neuroimaging, 181(3), 165–173. https://doi.org/10.1016/j.pscychresns.2009.11.008
Mohr, P. N. C., Biele, G., & Heekeren, H. R. (2010). Neural processing of risk. Journal of Neuroscience, 30(19), 6613–6619. https://doi.org/10.1523/JNEUROSCI.0003-10.2010
Murray, E. A., & Rudebeck, P. H. (2018). Specializations for reward-guided decision-making in the primate ventral prefrontal cortex. Nature Reviews Neuroscience, 19(7), 404–417. https://doi.org/10.1038/s41583-018-0013-4
Olsen, C. M. (2011). Natural rewards, neuroplasticity, and non-drug addictions. Neuropharmacology, 61(7), 1109–1122. https://doi.org/10.1016/j.neuropharm.2011.03.010
Park, S. Q., Kahnt, T., Rieskamp, J., & Heekeren, H. R. (2011). Neurobiology of value integration: When value impacts valuation. Journal of Neuroscience, 31(25), 9307–9314. https://doi.org/10.1523/JNEUROSCI.4973-10.2011
Paulus, M. P., Rogalsky, C., Simmons, A., Feinstein, J. S., & Stein, M. B. (2003). Increased activation in the right insula during risk-taking decision making is related to harm avoidance and neuroticism. NeuroImage, 19(4), 1439–1448. https://doi.org/10.1016/S1053-8119(03)00251-9
Phan, K. L., Wager, T., Taylor, S. F., & Liberzon, I. (2002). Functional neuroanatomy of emotion: A meta-analysis of emotion activation studies in PET and fMRI. NeuroImage, 16(2), 331–348. https://doi.org/10.1006/nimg.2002.1087
Poldrack, R. A., Baker, C. I., Durnez, J., Gorgolewski, K. J., Matthews, P. M., Munafò, M. R., Nichols, T. E., Poline, J. B., Vul, E., & Yarkoni, T. (2017). Scanning the horizon: Towards transparent and reproducible neuroimaging research. Nature Reviews Neuroscience, 18(2), 115–126. https://doi.org/10.1038/nrn.2016.167
Potenza, M. N. (2006). Should addictive disorders include non-substance-related conditions? Addiction, 101(s1), 142–151. https://doi.org/10.1111/j.1360-0443.2006.01591.x
Potenza, M. N. (2008). The neurobiology of pathological gambling and drug addiction: An overview and new findings. Philosophical Transactions of the Royal Society b: Biological Sciences, 363(1507), 3181–3189. https://doi.org/10.1098/rstb.2008.0100
Potenza, M. N., Balodis, I. M., Franco, C. A., Bullock, S., Xu, J., Chung, T., & Grant, J. E. (2013). Neurobiological considerations in understanding behavioral treatments for pathological gambling. Psychology of Addictive Behaviors, 27(2), 380–392. https://doi.org/10.1037/a0032389
Poudel, R., Riedel, M. C., Salo, T., Flannery, J. S., Hill-Bowen, L. D., Eickhoff, S. B., Laird, A. R., & Sutherland, M. T. (2020). Common and distinct brain activity associated with risky and ambiguous decision-making. Drug and Alcohol Dependence, 209(October 2019). https://doi.org/10.1016/j.drugalcdep.2020.107884
Power, Y., Goodyear, B., & Crockford, D. (2012). Neural correlates of pathological gamblers preference for immediate rewards during the Iowa gambling task: An fMRI Study. Journal of Gambling Studies, 28(4), 623–636. https://doi.org/10.1007/s10899-011-9278-5
Preuschoff, K., Bossaerts, P., & Quartz, S. R. (2006). Neural differentiation of expected reward and risk in human subcortical structures. Neuron, 51(3), 381–390. https://doi.org/10.1016/j.neuron.2006.06.024
Reske, M., Stewart, J. L., Flagan, T. M., & Paulus, M. P. (2015). Attenuated neural processing of risk in young adults at risk for stimulant dependence. PLoS ONE, 10(6), e0127010. https://doi.org/10.1371/journal.pone.0127010
Roy, A. K., Gotimer, K., Kelly, A. M. C., Castellanos, F. X., Milham, M. P., & Ernst, M. (2011). Uncovering putative neural markers of risk avoidance. Neuropsychologia, 49(5), 937–944. https://doi.org/10.1016/j.neuropsychologia.2011.02.038
Rudebeck, P. H., Putnam, P. T., Daniels, T. E., Yang, T., Mitz, A. R., Rhodes, S. E. V., & Murray, E. A. (2014). A role for primate subgenual cingulate cortex in sustaining autonomic arousal. Proceedings of the National Academy of Sciences, 111(14), 5391–5396. https://doi.org/10.1073/pnas.1317695111
Schmidt, L., Skvortsova, V., Kullen, C., Weber, B., & Plassmann, H. (2017). How context alters value: The brain’s valuation and affective regulation system link price cues to experienced taste pleasantness. Scientific Reports, 7(1), 8098. https://doi.org/10.1038/s41598-017-08080-0
Schonberg, T., Fox, C. R., & Poldrack, R. A. (2011). Mind the gap: Bridging economic and naturalistic risk-taking with cognitive neuroscience. Trends in Cognitive Sciences, 15(1), 11–19. https://doi.org/10.1016/j.tics.2010.10.002
Schultz, W. (2011). Potential vulnerabilities of neuronal reward, risk, and decision mechanisms to addictive drugs. Neuron, 69(4), 603–617. https://doi.org/10.1016/j.neuron.2011.02.014
Seok, J.-W., Lee, K. H., Sohn, S., & Sohn, J.-H. (2015). Neural substrates of risky decision making in individuals with Internet addiction. The Australian and New Zealand Journal of Psychiatry, 49(10), 923–932. https://doi.org/10.1177/0004867415598009
Stalnaker, T. A., Cooch, N. K., & Schoenbaum, G. (2015). What the orbitofrontal cortex does not do. Nature Neuroscience, 18(5), 620–627. https://doi.org/10.1038/nn.3982
Suckling, J., & Nestor, L. J. (2017). The neurobiology of addiction: The perspective from magnetic resonance imaging present and future. Addiction, 112(2), 360–369. https://doi.org/10.1111/add.13474
Szucs, D., & Ioannidis, J. P. (2020). Sample size evolution in neuroimaging research: An evaluation of highly-cited studies (1990–2012) and of latest practices (2017–2018) in high-impact journals. NeuroImage, 221(July), 117164. https://doi.org/10.1016/j.neuroimage.2020.117164
Tanabe, J., Thompson, L., Claus, E., Dalwani, M., Hutchison, K., & Banich, M. T. (2007). Prefrontal cortex activity is reduced in gambling and nongambling substance users during decision-making. Human Brain Mapping, 28(12), 1276–1286. https://doi.org/10.1002/hbm.20344
Vaidya, J. G., Block, R. I., O’Leary, D. S., Ponto, L. B., Ghoneim, M. M., & Bechara, A. (2012). Effects of chronic marijuana use on brain activity during monetary decision-making. Neuropsychopharmacology : Official Publication of the American College of Neuropsychopharmacology, 37(3), 618–629. https://doi.org/10.1038/npp.2011.227
Vogt, B. A., Vogt, L., Farber, N. B., & Bush, G. (2005). Architecture and neurocytology of monkey cingulate gyrus. The Journal of Comparative Neurology, 485(3), 218–239. https://doi.org/10.1002/cne.20512
Wang, L., Yang, G., Zheng, Y., Li, Z., Qi, Y., Li, Q., & Liu, X. (2021). Enhanced neural responses in specific phases of reward processing in individuals with Internet gaming disorder. Journal of Behavioral Addictions, 10(1), 99–111. https://doi.org/10.1556/2006.2021.00003
Wang, Y., Wu, L., Wang, L., Zhang, Y., Du, X., & Dong, G. (2017). Impaired decision-making and impulse control in Internet gaming addicts: Evidence from the comparison with recreational Internet game users. Addiction Biology, 22(6), 1610–1621. https://doi.org/10.1111/adb.12458
West, R. (2001). Theories of addiction. Addiction, 96(1), 3–13. https://doi.org/10.1046/j.1360-0443.2001.96131.x
Wilson, R. C., Takahashi, Y. K., Schoenbaum, G., & Niv, Y. (2014). Orbitofrontal cortex as a cognitive map of task space. Neuron, 81(2), 267–279. https://doi.org/10.1016/j.neuron.2013.11.005
Yamamoto, D. J., Banich, M. T., Regner, M. F., Sakai, J. T., & Tanabe, J. (2017). Behavioral approach and orbitofrontal cortical activity during decision-making in substance dependence. Drug and Alcohol Dependence, 180(1), 234–240. https://doi.org/10.1016/j.drugalcdep.2017.08.024
Yamamoto, D. J., Reynolds, J., Krmpotich, T., Banich, M. T., Thompson, L., & Tanabe, J. (2014). Temporal profile of fronto-striatal-limbic activity during implicit decisions in drug dependence. Drug and Alcohol Dependence, 136(4), 108–114. https://doi.org/10.1016/j.drugalcdep.2013.12.024
Yu, L. Q., Kan, I. P., & Kable, J. W. (2020). Beyond a rod through the skull: A systematic review of lesion studies of the human ventromedial frontal lobe. Cognitive Neuropsychology, 37(1–2), 97–141. https://doi.org/10.1080/02643294.2019.1690981
Zilverstand, A., Huang, A. S., Alia-Klein, N., & Goldstein, R. Z. (2018). Neuroimaging impaired response inhibition and salience attribution in human drug addiction: A systematic review. Neuron, 98(5), 886–903. https://doi.org/10.1016/j.neuron.2018.03.048
Acknowledgements
This work was supported by the International Research Training Group The Neuroscience of Modulating Aggression and Impulsivity in Psychopathology (IRTG-2150) of the German Research Foundation (DFG).
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the International Research Training Group The Neuroscience of Modulating Aggression and Impulsivity in Psychopathology (IRTG-2150) of the German Research Foundation (DFG).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest/Competing Interests
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hüpen, P., Habel, U., Votinov, M. et al. A Systematic Review on Common and Distinct Neural Correlates of Risk-taking in Substance-related and Non-substance Related Addictions. Neuropsychol Rev 33, 492–513 (2023). https://doi.org/10.1007/s11065-022-09552-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-022-09552-5