Abstract
Purpose
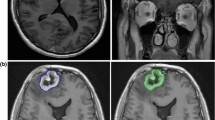
The differentiation between adverse radiation effects (ARE) and tumor recurrence or progression (TRP) is a major decision-making point in the follow-up of patients with brain tumors. The advent of immunotherapy, targeted therapy and radiosurgery has made this distinction difficult to achieve in several clinical situations. Contrast clearance analysis (CCA) is a useful technique that can inform clinical decisions but has so far only been histologically validated in the context of high-grade gliomas.
Methods
This is a series of 7 patients, treated between 2018 and 2023, for various brain pathologies including brain metastasis, atypical meningioma, and high-grade glioma. MRI with contrast clearance analysis was used to inform clinical decisions and patients underwent surgical resection as indicated. The histopathology findings were compared with the CCA findings in all cases.
Results
All seven patients had been treated with gamma knife radiosurgery and were followed up with periodic MR imaging. All patients underwent CCA when the necessity to distinguish tumor recurrence from radiation necrosis arose, and subsequently underwent surgery as indicated. Concordance of CCA findings with histological findings was found in all cases (100%).
Conclusions
Based on prior studies on GBM and the surgical findings in our series, delayed contrast extravasation MRI findings correlate well with histopathology across a wide spectrum of brain tumor pathologies. CCA can provide a quick diagnosis and have a direct impact on patients’ treatment and outcomes.





Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ARE:
-
Adverse radiation effect
- BEV:
-
Bevacizumab
- CCA:
-
Contrast clearance analysis
- GKRS:
-
Gamma Knife Radiosurgery
- IDL:
-
Isodose line
- IMRT:
-
Intensity modulated radiotherapy
- TRP:
-
Tumor recurrence/progression
References
Langer CJ, Mehta MP (2005) Current management of brain metastases, with a focus on systemic options. J Clin Oncol 23:6207–6219. https://doi.org/10.1200/JCO.2005.03.145
Yu Y, Chen H, Tian Z, Zhang Q, Shui Y, Shen L, Hu Q, Huang Z, Zhu S, Jiang H, Wei Q (2023) Improved survival outcome with not-delayed radiotherapy and immediate PD-1/PD-L1 inhibitor for non-small-cell lung cancer patients with brain metastases. J Neurooncol 165:127–137. https://doi.org/10.1007/s11060-023-04459-4
Zach L, Guez D, Last D, Daniels D, Grober Y, Nissim O, Hoffmann C, Nass D, Talianski A, Spiegelmann R, Tsarfaty G, Salomon S, Hadani M, Kanner A, Blumenthal DT, Bukstein F, Yalon M, Zauberman J, Roth J, Shoshan Y, Fridman E, Wygoda M, Limon D, Tzuk T, Cohen ZR, Mardor Y (2015) Delayed contrast extravasation MRI: a new paradigm in neuro-oncology. Neuro Oncol 17:457–465. https://doi.org/10.1093/neuonc/nou230
Ellingson BM, Chung C, Pope WB, Boxerman JL, Kaufmann TJ (2017) Pseudoprogression, radionecrosis, inflammation or true tumor progression? Challenges associated with Glioblastoma response assessment in an evolving therapeutic landscape. J Neurooncol 134:495–504. https://doi.org/10.1007/s11060-017-2375-2
Manning P, Daghighi S, Rajaratnam MK, Parthiban S, Bahrami N, Dale AM, Bolar D, Piccioni DE, McDonald CR, Farid N (2020) Differentiation of progressive disease from pseudoprogression using 3D PCASL and DSC perfusion MRI in patients with glioblastoma. J Neurooncol 147:681–690. https://doi.org/10.1007/s11060-020-03475-y
Thomas AA, Arevalo-Perez J, Kaley T, Lyo J, Peck KK, Shi W, Zhang Z, Young RJ (2015) Dynamic contrast enhanced T1 MRI perfusion differentiates pseudoprogression from recurrent glioblastoma. J Neurooncol 125:183–190. https://doi.org/10.1007/s11060-015-1893-z
Umemura Y, Wang D, Peck KK, Flynn J, Zhang Z, Fatovic R, Anderson ES, Beal K, Shoushtari AN, Kaley T, Young RJ (2020) DCE-MRI perfusion predicts pseudoprogression in metastatic melanoma treated with immunotherapy. J Neurooncol 146:339–346. https://doi.org/10.1007/s11060-019-03379-6
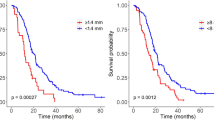
Bodensohn R, Forbrig R, Quach S, Reis J, Boulesteix AL, Mansmann U, Hadi I, Fleischmann DF, Mucke J, Holzgreve A, Albert NL, Ruf V, Dorostkar M, Corradini S, Herms J, Belka C, Thon N, Niyazi M (2022) MRI-based contrast clearance analysis shows high differentiation accuracy between radiation-induced reactions and progressive disease after cranial radiotherapy. ESMO Open 7:100424. https://doi.org/10.1016/j.esmoop.2022.100424
Lim DH, Kim SY, Na YC, Cho JM (2023) Navigation guided Biopsy is as effective as Frame-based stereotactic biopsy. J Pers Med 13. https://doi.org/10.3390/jpm13050708
Mohamedkhan S, Hindocha S, de Boisanger J, Millard T, Welsh L, Rich P, MacKinnon AD, Williams N, Sharma B, Rosenfelder N, Minchom A (2024) Contrast Clearance Analysis (CCA) to assess viable Tumour following stereotactic radiosurgery (SRS) to Brain Metastasis in Non-small Cell Lung Cancer (NSCLC). Cancers (Basel) 16. https://doi.org/10.3390/cancers16061218
Zach L, Guez D, Last D, Daniels D, Grober Y, Nissim O, Hoffmann C, Nass D, Talianski A, Spiegelmann R, Cohen ZR, Mardor Y (2012) Delayed contrast extravasation MRI for depicting tumor and non-tumoral tissues in primary and metastatic brain tumors. PLoS ONE 7:e52008. https://doi.org/10.1371/journal.pone.0052008
Rachinger W, Stoecklein VM, Terpolilli NA, Haug AR, Ertl L, Poschl J, Schuller U, Schichor C, Thon N, Tonn JC (2015) Increased 68Ga-DOTATATE uptake in PET imaging discriminates meningioma and tumor-free tissue. J Nucl Med 56:347–353. https://doi.org/10.2967/jnumed.114.149120
Chen WC, Perlow HK, Choudhury A, Nguyen MP, Mirchia K, Youngblood MW, Lucas CG, Palmer JD, Magill ST, Raleigh DR (2022) Radiotherapy for meningiomas. J Neurooncol 160:505–515. https://doi.org/10.1007/s11060-022-04171-9
Funding
No funding for this work was provided.
Author information
Authors and Affiliations
Contributions
Victor Goulenko– conceptualization, data acquisition, data analysis, writing, review. Venkatesh S Madhugiri– conceptualization, data acquisition, data analysis, writing, review. Amade Bregdy - data acquisition, data analysis, writing, review. Matthew Recker– data analysis, writing, review. Jingxin Qiu– data acquisition, data analysis, writing, review. Lindsey Lipinsky– data acquisition, data analysis, writing, review. Andrew Fabiano– data acquisition, data analysis, writing, review. Robert Fenstermaker– data acquisition, data analysis, writing, review. Robert Plunkett– data acquisition, data analysis, writing, review. Dheerendra Prasad– conceptualization, data acquisition, data analysis, writing, review.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Institutional Review Board of Roswell Park Comprehensive Cancer Center.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goulenko, V., Madhugiri, V.S., Bregy, A. et al. Histopathological correlation of brain tumor recurrence vs. radiation effect post-radiosurgery as detected by MRI contrast clearance analysis: a validation study. J Neurooncol (2024). https://doi.org/10.1007/s11060-024-04697-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11060-024-04697-0