Abstract
Background
Adverse radiation effect (ARE) following stereotactic radiosurgery (SRS) for brain metastases is challenging to distinguish from tumor progression. This study characterizes the clinical implications of radiologic uncertainty (RU).
Methods
Cases reviewed retrospectively at a single-institutional, multi-disciplinary SRS Tumor Board between 2015–2022 for RU following SRS were identified. Treatment history, diagnostic or therapeutic interventions performed upon RU resolution, and development of neurologic deficits surrounding intervention were obtained from the medical record. Differences in lesion volume and maximum diameter at RU onset versus resolution were compared with paired t-tests. Median time from RU onset to resolution was estimated using the Kaplan–Meier method. Univariate and multivariate associations between clinical characteristics and time to RU resolution were assessed with Cox proportional-hazards regression.
Results
Among 128 lesions with RU, 23.5% had undergone ≥ 2 courses of radiation. Median maximum diameter (20 vs. 16 mm, p < 0.001) and volume (2.7 vs. 1.5 cc, p < 0.001) were larger upon RU resolution versus onset. RU resolution took > 6 and > 12 months in 25% and 7% of cases, respectively. Higher total EQD2 prior to RU onset (HR = 0.45, p = 0.03) and use of MR perfusion (HR = 0.56, p = 0.001) correlated with shorter time to resolution; larger volume (HR = 1.05, p = 0.006) portended longer time to resolution. Most lesions (57%) were diagnosed as ARE. Most patients (58%) underwent an intervention upon RU resolution; of these, 38% developed a neurologic deficit surrounding intervention.
Conclusions
RU resolution took > 6 months in > 25% of cases. RU may lead to suboptimal outcomes and symptom burden. Improved characterization of post-SRS RU is needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases are common, occurring in up to 30 to 40% of patients with cancer [1]. Their incidence is expected to rise as more effective systemic therapies and high-quality imaging become increasingly available [2]. In recent years, stereotactic radiosurgery (SRS) has supplanted whole-brain radiation as a preferred treatment modality for patients with limited brain metastases due to its ability to spare neurocognitive function without compromising local control or overall survival [3,4,5]. Indications for SRS continue to expand, with observational data suggesting that SRS may be feasible in patients with up to 10 brain metastases [6]. Multiple phase III clinical trials exploring quality of life and survival outcomes further are currently underway (NCT04804644, NCT03075072).
Adverse radiation effect (ARE), which may entail necrosis, is a late complication of intracranial radiotherapy that typically occurs within 6 to 18 months after treatment [7]. Estimates of its incidence vary from 0% up to 30% [8] due to variations in its definition and challenges associated with pathologic confirmation. Radiologically, ARE typically appears as a ring-enhancing lesion with surrounding T2/FLAIR hyperintensity on magnetic resonance imaging (MRI) and can manifest clinically as headache, nausea, somatosensory deficits, or vision changes, among other symptoms [9]. These features make it difficult to distinguish from tumor progression, which often exhibits similar radiologic and clinical characteristics. Moreover, contrast-enhancing MRI lesions can represent a mixture of both ARE and recurrent tumor, further complicating their differentiation. Apart from surgical resection and laser interstitial thermal therapy (LITT), management of these entities can vary significantly, ranging from corticosteroids or bevacizumab for ARE to systemic therapy or reirradiation for recurrent tumor. ARE also resolves spontaneously without intervention in up to 50% of cases [10] and is therefore often managed with observation alone when asymptomatic. Accurate diagnosis of ARE versus tumor progression is therefore of critical importance.
Pathologic assessment is the gold standard in diagnosing ARE versus tumor progression; however, this is rarely performed in practice to avoid operative morbidity. Optimal techniques to distinguish ARE from tumor progression in a non-invasive manner have not yet been established. Studies have explored morphologic MRI [11], MR perfusion [12], MR spectroscopy [13], and positron emission tomography (PET) [14] as potential diagnostic tools, yet many of these techniques are currently limited by poor performance or infeasibility in the routine clinical setting. Instead, radiologic uncertainty (RU) between ARE and progressive tumor is typically monitored for change over time with serial MRIs before a presumed diagnosis is declared and a definitive intervention is recommended. This process can take months, during which time patients may experience lesion growth with edema and mass effect resulting in progressive symptoms and ultimately requiring more intensive therapy. While generally acknowledged, no studies to date have described the ramifications of this diagnostic delay after RU. We sought to characterize the management and clinical implications of RU after SRS for brain metastases among patients presented at a single center, high-volume, multidisciplinary SRS Tumor Board.
Materials and methods
Study design and participants
This study was approved by our Institutional Review Board. This was a retrospective cohort study of patients reviewed at the University of California San Francisco (UCSF) multi-disciplinary SRS Tumor Board for RU of ARE versus tumor progression at a site of prior SRS between April 2015 and December 2022. All patients were required to have undergone SRS for brain metastases. Exclusion criteria included incomplete medical records after initial RU and/or loss to follow-up before RU resolution.
Definitions of RU and RU resolution
The date of RU was defined as the date of the MRI on which a lesion indeterminate for tumor progression versus ARE (i.e., RU) was first described. The date of RU resolution was determined based on review of the medical record and defined as the date of surgical resection for diagnostic purposes in the face of uncertainty about ARE versus tumor progression or the date of definitive intervention after a presumed diagnosis of ARE versus tumor progression was reached, including surgical resection, re-irradiation, initiation of/change in systemic therapy, enrollment on hospice or a clinical trial, or initiation of steroids to treat ARE. If no intervention was performed, RU resolution was designated as the date on which the lesion showed improvement or stability in size as described in clinical notes and radiology reports.
Patient, tumor, and treatment characteristics
Patient, tumor, and treatment characteristics were obtained from the medical record. Specifically, histology of primary disease, history of prior surgical resection at the site of RU, history of prior permanent seed implant brachytherapy at the site of RU, symptoms at the time of RU, use of steroids or bevacizumab at the time of RU, imaging modalities used to resolve RU, final diagnosis of either ARE or tumor progression, interventions performed at the time of RU resolution, and development of neurological deficits surrounding definitive intervention were recorded. Note that a diagnosis could be reached either radiologically or based on pathology; thus, for lesions diagnosed based on imaging, the diagnosis may not have reflected the true lesion etiology. Lesions diagnosed as a mixture of ARE and tumor were classified as tumor progression. Dosimetric data from all prior courses of radiotherapy to sites of RU were obtained by evaluation of UCSF and outside radiation records.
Assessment of lesions at most recent course of SRS, time of initial RU, and time of RU resolution
For each patient, MRIs from three timepoints were imported from our institutional picture archiving and communication system (PACS) into MIM (version 7.1.4). Timepoints included a) the date of the most recent SRS course (planning SRS MRI), b) the date on which the question of RU was raised, and c) the date of RU resolution or the closest date prior to RU resolution. The contrast-enhancing lesion of interest was manually contoured on the T1 post-contrast MRI sequence at each timepoint for each patient. The maximum diameter and volume of the contrast-enhancing lesion at each timepoint were calculated in MIM. The T2/FLAIR MRI sequence was used to assess for the presence of edema causing mass effect (i.e., compression, distortion, or displacement or brain parenchyma or ventricles or sulcal effacement) on the dates of RU and RU resolution.
Statistical analysis
Descriptive statistics were used to summarize patient, tumor, and treatment characteristics at baseline. Differences in median lesion volume (cc) and maximum diameter (mm) at the time of RU versus RU resolution were evaluated with paired samples t-tests. The difference in the frequency of edema causing mass effect between RU and RU resolution within the cohort was evaluated with McNemar’s test. The Kaplan–Meier method was used to estimate the median time from completion of the most recent SRS course to the date of RU and the time from RU to the date of RU resolution (months). Associations between clinical characteristics and time to RU resolution were assessed with univariate and multivariate Cox proportional hazards regression. P-values < 0.05 were considered statistically significant. All statistics were performed in R version (version 4.2.2; available at http://www.r-project.org/).
Results
Lesion and treatment characteristics
We identified 128 lesions with RU in 123 patients who were presented at the institutional SRS Tumor Board for RU of ARE versus tumor progression at a prior site of SRS for brain metastasis between April 2015 and December 2022. Complete radiation records were available for 125 lesions. Imaging from the most recent course of SRS, initial RU, and RU resolution was available in 126, 128, and 126 cases, respectively. Baseline lesion characteristics are summarized in Table 1. Primary histology was non-small cell lung cancer in 32.8% of lesions and the most common location was in the frontal lobes (29.7%). The median total prescription EQD2 for all radiation courses prior to RU onset was 43.4 Gy. A metastasis had been previously resected at the site of RU in 28.9% of cases and permanent seed implant brachytherapy had been performed at the site of RU in 3.9% of cases. At the time of RU, 66.4% of patients were on systemic therapy; most were on either targeted therapy (39.1%) and/or immunotherapy (21.9%).
Lesion characteristics at time of initial RU and RU resolution
The median time from the most recent prior course of SRS to RU was 10.6 months. There was no significant difference in the time to RU among lesions ultimately diagnosed as ARE compared with progressive tumor (10 vs. 11 months, p = 0.6). Almost half (43.8%) of lesions were associated with symptoms at the time of RU; 41 (32.0%) and 5 (3.9%) required steroids and/or bevacizumab, respectively. The median maximum lesion diameter (20.0 mm vs. 16.0 mm, p < 0.001) and median lesion volume (2.7 cc vs. 1.5 cc, p < 0.001) were both significantly larger at the time of RU resolution compared with initial RU. A significantly larger proportion of lesions were also noted to result in edema causing mass effect on imaging at RU resolution compared with initial RU (38.3% vs. 21.9%, p = 0.001. Lesions with RU on T1 post-contrast MRI at RU onset, 18 and 30 months after RU onset, and RU resolution from two representative patients are demonstrated in Fig. 1.
Lesions with RU for representative patients diagnosed with ARE and tumor progression. Lesions with RU on T1 post-gadolinium MRI at A) RU onset, B) 18 months after RU onset, C) 30 months after RU onset, and D) RU resolution for representative patients diagnosed with ARE (top panel) and tumor progression (bottom panel)
Time to RU resolution
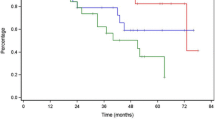
The distribution of times to resolution of RU among all lesions in our cohort is demonstrated in Fig. 2. The median time to RU resolution from the initial date of RU was 3.3 months (IQR: 2.3–6.0). Resolution of RU took between 0 and 3 months in 44.5% of cases; however, it took more than 6 months in 25% of cases and more than 12 months in 7.0% of cases.
Univariate and multivariate associations between patient, treatment, and RU lesion characteristics are shown in Table 2. On univariate analysis, lesions that received a total EQD2 > 100 Gy had significantly shorter time to RU resolution compared to those that received a total EQD2 ≤ 50 Gy (HR = 0.45, p = 0.03), but there was no difference in the time to RU resolution between those treated to 50–100 Gy compared to ≤ 50 Gy (HR = 0.96, p = 0.86). Larger lesion volume (HR = 1.05, p = 0.006) and diameter (HR = 1.02, p = 0.01) at the time of RU were associated with longer time to RU resolution. Cases where MR perfusion imaging was used to aid in the resolution of RU had significantly shorter time to RU resolution compared to those that did not (HR = 0.6, p = 0.001). Both lesion volume at the time of RU (HR = 1.04, p = 0.01) and use of MR perfusion imaging (HR = 0.60, p = 0.006) remained significantly associated with time to RU resolution on multivariate analysis. RU lesion diameter was not included in the multivariate analysis due collinearity with lesion volume.
Diagnosis and management
Data on lesion diagnosis (determined either radiologically or pathologically) and definitive management are shown in Table 3. ARE was diagnosed in 57.0% of lesions, while 42.2% of lesions were diagnosed as progressive tumor. One lesion was ultimately found to be a cavernous malformation upon resection 2.5 years after SRS. A diagnosis was reached radiographically in 73.4% of cases and based on surgical pathology in 26.6%. Of those that were resected, the presumed preoperative diagnosis aligned with surgical pathology in 88.2% of cases (three lesions thought to represent tumor were ultimately diagnosed as ARE and one lesion thought to represent tumor was diagnosed as a cavernous malformation). Management of the nine lesions that had previously been treated to an EQD2 ≥ 100 Gy involved surgery in 44.4% of cases. Surveillance between the time of initial RU and RU resolution involved MR perfusion imaging in 52.2% of cases and PET imaging in 11.7% of cases. Lesions in which MR perfusion was used were larger at the time of initial RU (7.9 cc vs. 4.1 cc, p = 0.01) and were more often located in the temporal lobes (24.1% vs. 8.9%, p = 0.08) compared to those in which MR perfusion was not used. Of the 34 lesions treated with surgery at the time of intervention, 16 had been imaged with MR perfusion between RU and RU resolution. The interpretation of MR perfusion (i.e., ARE versus tumor progression) was consistent with pathologic findings at surgery in 75% of cases.
At the time of RU resolution, 58.5% of patients underwent an intervention, including radiation (17.2%), surgery (18.0%), or a combination of the two (8.6%). Of these, 37.8% developed a neurologic deficit surrounding intervention. Most patients developed these deficits leading up to the intervention due to continued progression of either ARE or tumor; however, two patients developed new deficits immediately after the intervention (one who underwent surgery and another who underwent repeat SRS). The types and frequencies of the neurologic deficits experienced by patients in this cohort are illustrated in Fig. 3. The most common neurologic deficits were weakness, aphasia, and ataxia. Two patients died shortly after RU resolution. One patient, in whom RU resolution took 2.4 months, died from intractable cerebral edema secondary to radiation necrosis. The other patient was ultimately diagnosed with recurrent tumor 6.5 months after initial RU, during which time the lesion grew from 7.35 cc to 30.16 cc. This patient died due to progression of intracranial disease.
Discussion
While tumor progression and ARE are often radiographically and clinically indistinguishable, their management can be vastly different. Current diagnostic methods are non-specific in this setting despite efforts from the Response Assessment in Neuro-Oncology (RANO) group to standardize treatment response reporting [15]. When RU between progressive disease and ARE arises, patients are frequently monitored clinically and with serial imaging until a diagnosis can be reached. The implications of this RU are crucial to understand as the incidence of brain metastases rises and SRS plays a larger role in their treatment. In this study, we described the management and outcomes among patients with brain metastases presented at our multidisciplinary SRS Tumor Board for RU after SRS. Our findings illustrate the implications of RU and underscore the need for improved diagnostic techniques in this patient population.
While resolution of RU occurred within 3 months of initial RU for most lesions in our study, a large subset was subject to substantial diagnostic delays. Notably, RU resolution took more than 6 months in 25% of our cohort. Differentiation of tumor progression from ARE is notoriously difficult for several reasons. ARE encompasses a heterogeneous group of responses to intracranial radiotherapy ranging from transient, early inflammation, or “pseudoprogression,” to irreversible and sometimes progressive brain necrosis [16]. These entities exhibit marked variation in imaging features, making it challenging to define a characteristic “ARE radiologic signature” that can be applied across patients. Two-thirds of our cohort were receiving systemic therapy at the time of RU, which can influence treated lesions’ appearance on MRI. Treatment effect can also differ depending on class of systemic agent, with several studies demonstrating an increased risk of ARE with capecitabine [10] and tyrosine kinase inhibitors [17]. Moreover, intracranial lesions often exhibit dynamic evolution on imaging after SRS; up to a third will enlarge after treatment [18]. While this typically occurs within 18 months of radiation [10], cases have been reported up to a decade later [19]. This variability is reflected in our cohort, in which the time from SRS to RU development among patients ultimately diagnosed with ARE ranged from 1.1 to 156 months. Finally, the risk factors for development of ARE are incompletely understood and thus have poor specificity for treatment effect. Certainly, they include treatment-related parameters such as radiation dose, volume [20], and concurrent use of systemic therapy [10, 17], but also comprise primary tumor histology [21], age [22], tumor location and microenvironment [16, 23], intrinsic radiosensitivity [24], or most likely, a combination of these factors.
It took less time to resolve RU for lesions that had received multiple prior courses of radiotherapy (i.e., had been treated to a cumulative EQD2 ≥ 100 Gy). Cumulative radiation dose and volume of irradiated brain tissue, specifically V10 Gy and V12 Gy [20], have previously been described as risk factors for ARE. For instance, a review of 435 patients with 2,200 brain metastases treated with Gamma Knife SRS found that prior SRS to the same lesion was the most important predictor of ARE. Specifically, previous radiosurgery was associated with a 20% 1-year risk of symptomatic ARE, compared with only 3% among those with no prior treatment [10]. Our findings imply that radiation treatment history is often considered in diagnostic decision-making between RU and tumor progression. This may influence management in several ways. Progressive or symptomatic lesions may be pushed towards earlier surgery to obtain a pathologic diagnosis given the risks associated with both observation and further radiation. Indeed, 44% of the lesions previously treated to a total EQD2 ≥ 100 Gy in our study were diagnosed surgically, compared with 18% in the larger cohort. Alternatively, asymptomatic lesions that have been treated with multiple prior courses of radiotherapy may be quickly attributed to ARE.
Lesion diameter and volume at the time of RU were also associated with time to resolution of RU. One strategy for distinguishing treatment effect from progressive disease is comparison of the MRI with RU to the original radiation plan. Out-of-field or marginal lesion growth (i.e., growth outside of the area previously treated to 10–12 Gy) is concerning for recurrent tumor, while enlargement within the high-dose treatment area is more convincing for ARE. Small lesions are typically clearly distinguishable as in- or out-of-field, leading to prompt diagnosis and intervention, if appropriate. Alternatively, larger lesions often demonstrate heterogeneous growth [25], requiring observation over multiple imaging cycles before a definitive pattern of evolution can be appreciated. Moreover, larger lesions are more likely to contain a mixture of ARE, progressive disease, and necrotic tumor, further complicating their characterization [26, 27]. We also found that use of MR perfusion imaging portended a shorter time to resolution of RU. MR perfusion is often employed to help distinguish ARE from tumor progression [12, 28]; however, it is not without limitations, particularly for small lesions. This is illustrated in our study, where findings on MR perfusion only correlated with surgical pathology in 75% of cases.
Interestingly, there were a number of clinically relevant factors that were not associated with time to RU resolution. Perhaps most importantly, there was no difference in time to RU resolution between lesions ultimately deemed to represent ARE versus progressive disease, emphasizing the diagnostic challenge central to this study. In the same vein, the presence of symptoms at the time of RU did not correlate with more rapid resolution, likely because ARE can mimic tumor progression clinically [9]. Symptomatic ARE is initially managed with corticosteroids and sometimes bevacizumab, both of which can mitigate the clinical and radiographic signs of radionecrosis [29,30,31]. In clinical practice, these therapies frequently serve a diagnostic purpose as well, as one would expect recurrent tumor to remain stable and ARE to rapidly regress after their administration. Despite this, we did not find that lesions treated with steroids or bevacizumab at the time of RU were resolved more quickly. This may have been because these therapies are also used to relieve symptoms of recurrent brain metastases, and both are also associated with reversal of radiographic findings of tumor progression [8, 32]. Interpretation of imaging after administration of steroids or bevacizumab is therefore complex, and our findings suggest that they may not always facilitate differentiation of progressive disease from ARE.
Strikingly, almost 40% of patients who underwent a definitive intervention upon RU resolution developed a new neurologic deficit surrounding intervention. These included symptoms such as weakness, aphasia, visual deficits, and cognitive changes, all of which can have a profound impact on functional status and quality of life. While we are unable to determine whether these could have been prevented with earlier diagnosis, most deficits developed due to continued progression of ARE or tumor, and it is reasonable to assume that they could have been mitigated or avoided altogether with earlier intervention. Indeed, we found that median lesion size increased by 25% and median lesion volume almost doubled between RU and consensus diagnosis. This was accompanied by a significantly higher proportion of patients experiencing edema causing mass effect at the time of resolution. Larger lesion size is also a known risk factor for treatment-related complications after surgery [33, 34] and radiotherapy [9], which occurred in two patients who underwent definitive intervention at the time of RU resolution. Two patients in our cohort died shortly after resolution of RU. One developed intractable intracranial edema due to radiation necrosis, ultimately leading to their death 2.4 months after initial RU. Another patient died from progressive disease 6.5 months after RU, during which time their tumor quadrupled in size. While these represent extreme examples, our findings suggest that a large proportion of patients develop serious, potentially irreversible deficits due to diagnostic delay. Even with timely intervention, diagnostic uncertainty raises the potential for inappropriate treatment, such as re-reirradiation or withdrawal of effective systemic therapy in a patient who has ARE but is thought to have recurrent tumor. It is important to note that resolution of RU is often based on imaging alone without pathologic confirmation [16], as was the case in 73% of lesions in this study. Thus, there is a real possibility of misdiagnosis. This is highlighted in our cohort, where the presumed preoperative diagnosis among lesions that were surgically resected only aligned with pathologic findings in 88% of cases. This can lead to treatment error, unnecessary toxicity, and compromised outcomes.
RU is a well-recognized problem in the field of Neuro-Oncology [8, 15, 16], and efforts to develop more effective diagnostic tools to distinguish ARE from tumor progression are currently underway [35]. LITT, a minimally invasive surgical technique that uses heat to ablate tissue, can play both diagnostic and therapeutic roles in the management of RU. Indications for LITT have rapidly expanded in recent years and now include both treatment of in-field metastatic recurrences and ARE [36]. LITT has also demonstrated superior efficacy to bevacizumab for symptomatic radiation necrosis in retrospective series [37, 38]. Nevertheless, LITT may not always be feasible, particularly in lesions located in eloquent brain regions. Non-invasive diagnostic techniques have also been explored to address RU. These have included using standard MRI sequences such as T1/T2 matching [11], apparent diffusion coefficient ratios [39], and time-dependent changes in lesion morphology after contrast administration [40], although these are infrequently used in the clinical setting. As discussed above, MR perfusion is often employed when conventional MRI sequences are inconclusive, and multiple groups have explored using standard cutoffs for metrics such as relative cerebral blood volume or peak height to distinguish recurrent tumor from treatment effect [12, 28]. MR spectroscopy [41,42,43], which analyzes tissue metabolites is another MR technique that has been employed to improve diagnostic certainty in this situation. Historically, single-photon emission computed tomography (SPECT)44, which detects the distribution of radioactive tracers such as thallium-201 or technetium-99, was the nuclear medicine technique of choice for the study of indeterminate brain lesions. More recently, amino acid PET imaging has been employed in this scenario and has demonstrated high diagnostic accuracy in identifying tumor progression [45, 46]. Indeed, RANO cites level 2 evidence for amino acid PET in this setting, although most studies have comprised retrospective, single-center analyses without histopathologic confirmation [47]. While a variety of amino acid radiotracers have been examined, including 11C-MET, 18F-DOPA, 18F-FET, and 18F-fluciclovine, their regular use is currently limited by availability, cost, and regulatory approval [48]. Notably, only 11.7% of lesions in our study were assessed with nuclear imaging, highlighting its limited use even within a large, academic institution. Most recently, machine learning-based analyses of radiomics signatures have been increasingly explored in patients with RU after intracranial radiation [49]. This approach extracts radiographic features from a variety of imaging sequences and modalities to build predictive models that can aid in diagnosis and management. These models frequently outperform radiologists in identifying radiation necrosis [50, 51]; however, further validation is needed in large, heterogeneous populations across multiple sites before they can be incorporated into clinical practice. Ultimately, RANO guidelines state that there is insufficient evidence to support any one of these modalities [15]. Instead, use of clinical judgment with a combination of these techniques is recommended, potentially across several imaging cycles if a diagnosis cannot be reached at any one timepoint.
This study has several limitations, one of which is its lack of histopathologic confirmation at the time of resolution for the majority of lesions. Our findings describe factors associated with time to RU resolution, which may or may not have been based on a correct diagnosis in patients diagnosed radiographically. Nevertheless, our results reflect the reality of RU resolution in the clinical setting and describe the consequences of current management practices. Other limitations are related to this study’s retrospective nature. Patient-specific factors such as lack of social support or transportation barriers that may have contributed to prolonged diagnosis were not captured in this study. Similarly, assessment of patient symptoms upon RU and intervention was based on the medical record, which may have introduced bias in our results. However, complete radiation records and imaging at each timepoint were available for the vast majority of lesions, which allowed the study authors to independently measure lesion volumes over time rather than relying on radiology reports.
To our knowledge, we present the first analysis of the consequences of RU between ARE and tumor progression among patients who have undergone SRS for brain metastases. In a multidisciplinary setting at a large, academic medical center, a quarter of patients experienced delays in management of at least 6 months, during which time lesions enlarged and more often led to intracranial edema. Clinical factors such as radiation history, lesion size, and use of MR perfusion influenced time to RU resolution; however, these may be subject to error when used for diagnostic purposes. Finally, a striking number of patients developed neurologic deficits surrounding intervention, including two patients who died due to lesion progression. Oncology care teams will increasingly be faced with this diagnostic dilemma as survival among patients with brain metastases continues to improve. Our findings highlight the critical need for more effective, clinically feasible diagnostic tools in this population.
Data availability
The data analyzed in this study are available upon request to the corresponding author.
References
Gondi V, Bauman G, Bradfield L et al (2022) Radiation Therapy for Brain Metastases: An ASTRO Clinical Practice Guideline. Pract Radiat Oncol 12(4):265–282. https://doi.org/10.1016/j.prro.2022.02.003
Suh JH (2010) Stereotactic radiosurgery for the treatment of brain metastases. N Engl J Med 362:1119–1127. https://doi.org/10.1056/NEJMct0806951
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases a randomized clinical trial. JAMA - J Am Med Assoc 316(4):401–409. https://doi.org/10.1001/jama.2016.9839
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044. https://doi.org/10.1016/S1470-2045(09)70263-3
Aoyama H, Shirato H, Tago M et al (2006) Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: A randomized controlled trial. JAMA - J Am Med Assoc 295(21):2483–2491. https://doi.org/10.1001/jama.295.21.2483
Yamamoto M, Serizawa T, Shuto T et al (2014) Stereotactic radiosurgery for patients with multiple brain metastases (JLGK0901): a multi-institutional prospective observational study. Lancet Oncol 15(4):387–395. https://doi.org/10.1016/S1470-2045(14)70061-0
Eisele S, Dietrich J (2015) Cerebral radiation necrosis: diagnostic challenge and clinical management. Rev Neurol 1(61):225–232
Aizer AA, Lamba N, Ahluwalia MS et al (2022) Brain metastases: A Society for Neuro-Oncology (SNO) consensus review on current management and future directions. Neuro Oncol 24(10):1613–1646. https://doi.org/10.1093/neuonc/noac118
Minniti, G., Clarke, E., Lanzetta, G. et al (2021) Stereotactic radiosurgery for brain metastases: analysisof outcome and risk of brain radionecrosis. Radiat Oncol 6:48 . https://doi.org/10.1186/1748-717X-6-48
Sneed PK, Mendez J, Vemer-Van Den Hoek JGM et al (2015) Adverse radiation effect after stereotactic radiosurgery for brain metastases: Incidence, time course, and risk factors. J Neurosurg. 123(2):373–386. https://doi.org/10.3171/2014.10.JNS141610
Kano H, Kondziolka D, Lobato-Polo J, Zorro O, Flickinger JC, Lunsford LD (2010) T1/T2 matching to differentiate tumor growth from radiation effects after stereotactic radiosurgery. Neurosurgery 66(3):486–491. https://doi.org/10.1227/01.NEU.0000360391.35749.A5
Mitsuya K, Nakasu Y, Horiguchi S et al (2010) Perfusion weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. J Neurooncol 99(1):81–88. https://doi.org/10.1007/s11060-009-0106-z
Kamada K, Houkin K, Abe H, Sawamura Y, Kashiwaba T (1997) Differentiation of cerebral radiation necrosis from tumor recurrence by proton magnetic resonance spectroscopy. Neurol Med Chir 37:250–256
Li H, Deng L, Bai HX et al (2018) Diagnostic Accuracy of Amino Acid and FDG-PET in Differentiating Brain Metastasis Recurrence from Radionecrosis after Radiotherapy: A Systematic Review and Meta-Analysis. Am J Neuroradiol 39(2):280–288. https://doi.org/10.3174/ajnr.A5472
Lin NU, Lee EQ, Aoyama H et al (2015) Response assessment criteria for brain metastases: Proposal from the RANO group. Lancet Oncol 16(6):e270–e278. https://doi.org/10.1016/S1470-2045(15)70057-4
Winter SF, Loebel F, Loeffler J et al (2019) Treatment-induced brain tissue necrosis: A clinical challenge in neuro-oncology. Neuro Oncol 21(9):1118–1130. https://doi.org/10.1093/neuonc/noz048
Kim JM, Miller JA, Kotecha R et al (2017) The risk of radiation necrosis following stereotactic radiosurgery with concurrent systemic therapies. J Neurooncol 133(2):357–368. https://doi.org/10.1007/s11060-017-2442-8
Patel TR, McHugh BJ, Bi WL, Minja FJ, Knisely JPS, Chiang VL (2011) A comprehensive review of MR imaging changes following radiosurgery to 500 brain metastases. Am J Neuroradiol 32(10):1885–1892. https://doi.org/10.3174/ajnr.A2668
Tofilon PJ, Fike JR (2000) The radioresponse of the central nervous system: A dynamic process. Radiat Res 153(4):357–370. https://doi.org/10.1667/0033-7587(2000)153[0357:TROTCN]2.0.CO;2
Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, Breneman JC (2010) Irradiated Volume as a Predictor of Brain Radionecrosis After Linear Accelerator Stereotactic Radiosurgery. Int J Radiat Oncol Biol Phys 77(4):996–1001. https://doi.org/10.1016/j.ijrobp.2009.06.006
Miller JA, Bennett EE, Xiao R et al (2016) Association Between Radiation Necrosis and Tumor Biology After Stereotactic Radiosurgery for Brain Metastasis. Int J Radiat Oncol Biol Phys 96(5):1060–1069. https://doi.org/10.1016/j.ijrobp.2016.08.039
Kerschbaumer J, Demetz M, Krigers A, Nevinny-Stickel M, Thomé C, Freyschlag CF (2021) Risk factors for radiation necrosis in patients undergoing cranial stereotactic radiosurgery. Cancers (Basel) 13(19):1–8. https://doi.org/10.3390/cancers13194736
Jarosz-Biej M, Smolarczyk R, Cichoń T, Kułach N (2019) Tumor microenvironment as a “game changer” in cancer radiotherapy. Int J Mol Sci 20(13):18–20. https://doi.org/10.3390/ijms20133212
Raaphorst GP, Malone S, Alsbeih G, Souhani L, Szumacher E, Girard A (2002) Skin fibroblasts in vitro radiosensitivity can predict for late complications following AVM radiosurgery. Radiother Oncol 64(2):153–156. https://doi.org/10.1016/S0167-8140(02)00076-2
Wen J, Tan AP, Yong HRC, Wong YLJ (2018) Delayed radiation necrosis and evolution of its imaging features over time: An illustrative case report. J Oncol Pract 14(12):754–756. https://doi.org/10.1200/JOP.18.00488
Dequesada IM, Quisling RG, Yachnis A, Friedman WA (2008) Can standard magnetic resonance imaging reliably distinguish recurrent tumor from radiation necrosis after radiosurgery for brain metastases? A radiographic-pathological study. Neurosurgery 63(5):898–903. https://doi.org/10.1227/01.NEU.0000333263.31870.31
Mullins ME, Barest GD, Schaefer PW, Hochberg FH, Gonzalez RG, Lev MH (2005) Radiation necrosis versus glioma recurrence: Conventional MR imaging clues to diagnosis. Am J Neuroradiol 26(8):1967–1972
Barajas RF, Chang JS, Sneed PK, Segal MR, McDermott MW, Cha S (2009) Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following gamma knife radiosurgery using dynamic susceptibility- weighted contrast-enhanced perfusion MR imaging. Am J Neuroradiol 30(2):367–372. https://doi.org/10.3174/ajnr.A1362
Tye K, Engelhard HH, Slavin KV et al (2014) An analysis of radiation necrosis of the central nervous system treated with bevacizumab. J Neurooncol 117(2):321–327. https://doi.org/10.1007/s11060-014-1391-8
Rahmathulla G, Marko NF, Weil RJ (2013) Cerebral radiation necrosis: A review of the pathobiology, diagnosis and management considerations. J Clin Neurosci 20(4):485–502. https://doi.org/10.1016/j.jocn.2012.09.011
Yoritsune E, Furuse M, Kuwabara H et al (2014) Inflammation as well as angiogenesis may participate in the pathophysiology of brain radiation necrosis. J Radiat Res 55(4):803–811. https://doi.org/10.1093/jrr/rru017
Berghoff AS, Breckwoldt MO, Riedemann L et al (2020) Bevacizumab-based treatment as salvage therapy in patients with recurrent symptomatic brain metastases. Neuro-Oncology Adv 2(1):1–9. https://doi.org/10.1093/noajnl/vdaa038
Ferroli P, Broggi M, Schiavolin S et al (2015) Predicting functional impairment in brain tumor surgery: The Big Five and the Milan Complexity Scale. Neurosurg Focus 39(6):1–10. https://doi.org/10.3171/2015.9.FOCUS15339
McPherson CM, Warnick RE (2004) Results of contemporary surgical management of radiation necrosis using frameless stereotaxis and intraoperative magnetic resonance imaging. J Neurooncol 68(1):41–47. https://doi.org/10.1023/B:NEON.0000024744.16031.e9
Mayo ZS, Halima A, Broughman JR et al (2023) Radiation necrosis or tumor progression? A review of the radiographic modalities used in the diagnosis of cerebral radiation necrosis. J Neurooncol 161(1):23–31. https://doi.org/10.1007/s11060-022-04225-y
Holste KG, Orringer DA (2020) Laser interstitial thermal therapy. Neuro-Oncology Adv 2(1):1–6. https://doi.org/10.1093/noajnl/vdz035
Sujijantarat N, Hong CS, Owusu KA et al (2020) Laser interstitial thermal therapy (LITT) vs. bevacizumab for radiation necrosis in previously irradiated brain metastases. J Neurooncol. 148(3):641–649. https://doi.org/10.1007/s11060-020-03570-0
Chan M, Tatter S, Chiang V et al (2023) Neuro-Oncology Advances proven radiation necrosis in radiographically recurrent 5(March):1-12
Hein PA, Eskey CJ, Dunn JF, Hug EB (2004) Diffusion-Weighted Imaging in the Follow-up of Treated High-Grade Gliomas: Tumor Recurrence versus Radiation Injury. Am J Neuroradiol 25(2):201–209
Wagner S, Lanfermann H, Eichner G, Gufler H (2017) Radiation injury versus malignancy after stereotactic radiosurgery for brain metastases: Impact of time-dependent changes in lesion morphology on MRI. Neuro Oncol 19(4):586–594. https://doi.org/10.1093/neuonc/now193
Sundgren PC (2009) MR spectroscopy in radiation injury. Am J Neuroradiol 30(8):1469–1476. https://doi.org/10.3174/ajnr.A1580
Rock JP, Scarpace L, Hearshen D et al (2004) Associations among Magnetic Resonance Spectroscopy, Apparent Diffusion Coefficients, and Image-guided Histopathology with Special Attention to Radiation Necrosis. Neurosurgery 54(5):1111–1119. https://doi.org/10.1227/01.NEU.0000119328.56431.A7
Wang ZJ, Ohliger MA, Larson PEZ et al (2019) Hyperpolarized 13C MRI: State of the art and future directions. Radiology 291(2):273–284. https://doi.org/10.1148/radiol.2019182391
Furuse M, Nonoguchi N, Yamada K et al (2019) Radiological diagnosis of brain radiation necrosis after cranial irradiation for brain tumor: A systematic review. Radiat Oncol 14(1):1–15. https://doi.org/10.1186/s13014-019-1228-x
Cicone F, Minniti G, Romano A et al (2015) Accuracy of F-DOPA PET and perfusion-MRI for differentiating radionecrotic from progressive brain metastases after radiosurgery. Eur J Nucl Med Mol Imaging 42(1):103–111. https://doi.org/10.1007/s00259-014-2886-4
Tomura N, Kokubun M, Saginoya T, Mizuno Y, Kikuchi Y (2017) Differentiation between Treatment-Induced Necrosis and Recurrent Tumors in Patients with Metastatic Brain Tumors: Comparison among 11C-Methionine-PET, FDG-PET, MR Permeability Imaging, and MRI-ADC - Preliminary Results. Am J Neuroradiol 38(8):1520–1527
Galldiks N, Langen KJ, Albert NL et al (2019) PET imaging in patients with brain metastasis—report of the RANO/PET group. Neuro Oncol 21(5):584–595. https://doi.org/10.1093/neuonc/noz003
Heinzel A, Müller D, Yekta-Michael SS et al (2017) O-(2–18F-fluoroethyl)-L-tyrosine PET for evaluation of brain metastasis recurrence after radiotherapy: An effectiveness and cost-effectiveness analysis. Neuro Oncol 19(9):1271–1278. https://doi.org/10.1093/neuonc/now310
Nowakowski A, Lahijanian Z, Panet-Raymond V et al (2022) Radiomics as an emerging tool in the management of brain metastases. Neuro-Oncology Adv 4(1):1–16. https://doi.org/10.1093/noajnl/vdac141
Hettal L, Stefani A, Salleron J et al (2020) Radiomics method for the differential diagnosis of radionecrosis versus progression after fractionated stereotactic body radiotherapy for brain oligometastasis. Radiat Res 193(5):471–480. https://doi.org/10.1667/RR15517.1
Peng L, Parekh V, Huang P et al (2018) Distinguishing true progression from radionecrosis after stereotactic radiation therapy for brain metastases with machine learning and radiomics. Int J Radiat Oncol Biol Phys 102(4):1236–1243. https://doi.org/10.1016/j.ijrobp.2018.05.041
Acknowledgements
None
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Concept and design: MS, SB Acquisition, analysis, or interpretation of data: All authors Drafting and reviewing of the manuscript: All authors Statistical analysis: MS, SB Administrative, technical, or material support: SB, PT, PKS
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the UCSF IRB, No. 18–26489.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Tumor is difficult to distinguish from treatment effect after stereotactic radiosurgery (SRS).
• Resolution of radiologic uncertainty (RU) after SRS took > 6 months in 25% of brain metastases.
• Many patients developed new neurologic deficits by the time of RU resolution.
Importance of the study
Stereotactic radiosurgery (SRS) is frequently used to treat brain metastases but may lead to adverse radiation effect (ARE) in up to 30% of cases. ARE is challenging to distinguish from tumor progression on imaging, and radiologic uncertainty (RU) is often resolved with monitoring of serial MRIs before a diagnosis is reached or a definitive intervention is performed. During this time, lesions may enlarge and cause progressive symptoms, ultimately requiring more intensive treatment. While generally acknowledged, no studies have described the consequences of this delay in RU resolution. This study characterizes the management and clinical implications of RU after SRS for brain metastases at a single, high-volume institution. We demonstrate that a significant proportion of patients experience prolonged delays in diagnosis and/or intervention after RU, many of whom develop new neurologic deficits by the time of resolution. Our findings highlight the critical need for improved diagnostic tools in this population.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salans, M., Ni, L., Morin, O. et al. Adverse radiation effect versus tumor progression following stereotactic radiosurgery for brain metastases: Implications of radiologic uncertainty. J Neurooncol 166, 535–546 (2024). https://doi.org/10.1007/s11060-024-04578-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-024-04578-6