Abstract
Background and purpose
Currently, the antiangiogenic agent bevacizumab (BVZ) is used as a treatment option for high-grade glioma (HGG) patients. However, BVZ restores disruptions of the blood–brain barrier, which leads to the disappearance of contrast enhancement during radiological examinations and therefore complicates evaluations of treatment efficacy. This study aimed to investigate the radio-morphological features of recurrent lesions that newly appeared under BVZ therapy, as well as the utility of arterial spin labeling (ASL) perfusion imaging for evaluating treatment response and prognosis in HGG patients receiving BVZ.
Methods
Thirty-two patients (20 males, 12 females; age range, 35–84 years) with HGG who experienced a recurrence under BVZ therapy were enrolled. We measured the relative cerebral blood flow (rCBF) values of each recurrent lesion using ASL, and retrospectively investigated the correlation between rCBF values and prognosis.
Results
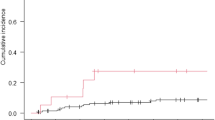
The optimal rCBF cut-off value for predicting prognosis was defined as 1.67 using receiver operating characteristic curve analysis. The patients in the rCBF < 1.67 group had significantly longer overall survival (OS) and post-progression survival (PPS) than those in the rCBF ≥ 1.67 group (OS: 34.0 months vs. 13.0 months, p = 0.03 and PPS: 13.0 months vs. 6.0 months, p < 0.001, respectively).
Conclusion
The ASL-derived rCBF values of recurrent lesions may serve as an effective imaging biomarker for prognosis in HGG patients undergoing BVZ therapy. Low rCBF values may indicate that BVZ efficacy is sustainable, which will influence BVZ treatment strategies in HGG patients.



Similar content being viewed by others
Data availability
The data used in this study are available to researchers on request. Requests for data can be sent to the corresponding author.
References
No authors listed (2017) Brain Tumor Registry of Japan (2005–2008). Neurol Med Chir (Tokyo) 57:9–102. https://doi.org/10.2176/nmc.sup.2017-0001
Henriksen OM, Del Mar Álvarez-Torres M, Figueiredo P et al (2022) High-Grade Glioma Treatment Response monitoring biomarkers: a position Statement on the evidence supporting the Use of Advanced MRI techniques in the Clinic, and the latest bench-to-Bedside developments. Part 1: perfusion and diffusion techniques. Front Oncol 12:810263. https://doi.org/10.3389/fonc.2022.810263
Seyedmirzaei H, Shobeiri P, Turgut M et al (2020) VEGF levels in patients with glioma: a systematic review and meta-analysis. Rev Neurosci 32:191–202. https://doi.org/10.1515/revneuro-2020-0062
Hegi ME, Diserens AC, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med 352:997–1003. https://doi.org/10.1056/NEJMoa043331
Hutterer M, Hattingen E, Palm C et al (2015) Current standards and new concepts in MRI and PET response assessment of antiangiogenic therapies in high-grade glioma patients. Neuro Oncol 17:784–800. https://doi.org/10.1093/neuonc/nou322
Lyu Y, Liu S, You H et al (2017) Evaluation of recurrent high-grade gliomas treated with bevacizumab: a preliminary report of 3D pseudocontinuous artery spin labeling. Magn Reson Imaging 46:565–573. https://doi.org/10.1002/jmri.25558
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972. https://doi.org/10.1200/JCO.2009.26.3541
Schmainda KM, Zhang Z, Prah M et al (2015) Dynamic susceptibility contrast MRI measures of relative cerebral blood volume as a prognostic marker for overall survival in recurrent glioblastoma: results from the ACRIN 6677/RTOG 0625 multicenter trial. Neuro Oncol 17:1148–1156. https://doi.org/10.1093/neuonc/nou364
Kickingereder P, Wiestler B, Burth S et al (2015) Relative cerebral blood volume is a potential predictive imaging biomarker of bevacizumab efficacy in recurrent glioblastoma. Neuro Oncol 17:1139–1147. https://doi.org/10.1093/neuonc/nov028
Beppu T, Sato Y, Sasaki T et al (2019) Comparisons between PET with 11 C-Methyl-L-Methionine and arterial spin labeling perfusion imaging in recurrent glioblastomas treated with Bevacizumab. Clin Nucl Med 44:186–193. https://doi.org/10.1097/RLU.0000000000002417
Golay X, Hendrikse J, Lim TC (2004) Perfusion imaging using arterial spin labeling. Top Magn Reson Imaging 15:10–27
Falk Delgado A, De Luca F, van Westen D et al (2018) Arterial spin labeling MR imaging for differentiation between high- and low-grade glioma-a meta-analysis. Neuro Oncol 20:1450–1461. https://doi.org/10.1093/neuonc/noy095
Yang S, Zhao B, Wang G et al (2016) Improving the Grading Accuracy of Astrocytic Neoplasms noninvasively by combining timing information with cerebral blood Flow: a Multi-TI arterial spin-labeling MR Imaging Study. AJNR Am J Neuroradiol 37:2209–2216. https://doi.org/10.3174/ajnr.A4907
Batalov AI, Afandiev RM, Zakharova NE et al (2022) 3D pseudo-continuous arterial spin labeling-MRI (3D PCASL-MRI) in the differential diagnosis between glioblastomas and primary central nervous system Lymphomas. Neuroradiology 64:1539–1545. https://doi.org/10.1007/s00234-021-02888-4
Xi YB, Kang XW, Wang N et al (2019) Differentiation of primary central nervous system Lymphoma from high-grade glioma and brain Metastasis using arterial spin labeling and dynamic contrast-enhanced magnetic resonance imaging. Eur J Radiol 112:59–64. https://doi.org/10.1016/j.ejrad.2019.01.008
Choi YJ, Kim HS, Jahng GH et al (2013) Pseudoprogression in patients with glioblastoma: added value of arterial spin labeling to dynamic susceptibility contrast perfusion MR imaging. Acta Radiol 54:448–454. https://doi.org/10.1177/0284185112474916
Manning P, Daghighi S, Rajaratnam MK et al (2020) Differentiation of Progressive Disease from pseudoprogression using 3D PCASL and DSC perfusion MRI in patients with glioblastoma. J Neurooncol 147:681–690. https://doi.org/10.1007/s11060-020-03475-y
Takano S, Kato Y, Yamamoto T et al (2012) Immunohistochemical detection of IDH1 mutation, p53, and internexin as prognostic factors of glial tumors. J Neurooncol 108:361–373. https://doi.org/10.1007/s11060-012-0837-0
Schmainda KM, Prah MA, Marques H et al (2021) Value of dynamic contrast perfusion MRI to predict early response to bevacizumab in newly diagnosed glioblastoma: results from ACRIN 6686 multicenter trial. Neuro Oncol 23:314–323. https://doi.org/10.1093/neuonc/noaa167
Zhang W, Kreisl T, Solomon J et al (2009) Acute effects of bevacizumab on glioblastoma vascularity assessed with DCE-MRI and relation to patient survival. Proc Intl Soc Magn Reson Med 17:282
Kickingereder P, Wiestler B, Graf M et al (2015) Evaluation of dynamic contrast-enhanced MRI derived microvascular permeability in recurrent glioblastoma treated with bevacizumab. J Neurooncol 121:373–380. https://doi.org/10.1007/s11060-014-1644-6
Essig M, Shiroishi MS, Nguyen TB et al (2013) Perfusion MRI: the five most frequently asked technical questions. AJR Am J Roentgenol 200:24–34. https://doi.org/10.2214/AJR.12.9543
Galldiks N, Rapp M, Stoffels G et al (2013) Earlier diagnosis of Progressive Disease during bevacizumab treatment using O-(2-18F-fluorethyl)-L-tyrosine positron emission tomography in comparison with magnetic resonance imaging. Mol Imaging 12:273–276
Galldiks N, Rapp M, Stoffels G et al (2013) Response assessment of bevacizumab in patients with recurrent malignant glioma using [18F] Fluoroethyl-L-tyrosine PET in comparison to MRI. Eur J Nucl Med Mol Imaging 40:22–33. https://doi.org/10.1007/s00259-012-2251-4
Schwarzenberg J, Czernin J, Cloughesy TF et al (2014) Treatment response evaluation using 18F-FDOPA PET in patients with recurrent malignant glioma on bevacizumab therapy. Clin Cancer Res 20:3550–3559. https://doi.org/10.1158/1078-0432.CCR-13-1440
Hughes KL, O’Neal CM, Andrews BJ et al (2021) A systematic review of the utility of amino acid PET in assessing treatment response to bevacizumab in recurrent high-grade glioma. Neurooncol Adv 3:vdab003. https://doi.org/10.1093/noajnl/vdab003
Gaddamanugu S, Shafaat O, Sotoudeh H et al (2022) Clinical applications of diffusion-weighted sequence in brain imaging: beyond Stroke. Neuroradiology 64:15–30. https://doi.org/10.1007/s00234-021-02819-3
Nguyen HS, Milbach N, Hurrell SL et al (2016) Progressing Bevacizumab-Induced Diffusion Restriction is Associated with Coagulative Necrosis surrounded by viable Tumor and decreased overall survival in patients with recurrent glioblastoma. AJNR Am J Neuroradiol 37:2201–2208. https://doi.org/10.3174/ajnr.A4898
Zakhari N, Taccone MS, Torres C et al (2018) Diagnostic accuracy of centrally restricted diffusion in the differentiation of treatment-related necrosis from Tumor Recurrence in High-Grade Gliomas. AJNR Am J Neuroradiol 39:260–264. https://doi.org/10.3174/ajnr.A5485
Rieger J, Bähr O, Müller K et al (2010) Bevacizumab-induced diffusion-restricted lesions in malignant glioma patients. J Neurooncol 99:49–56. https://doi.org/10.1007/s11060-009-0098-8
Farid N, Almeida-Freitas DB, White NS et al (2013) Restriction-Spectrum Imaging of Bevacizumab-Related Necrosis in a patient with GBM. Front Oncol 3:258. https://doi.org/10.3389/fonc.2013.00258
Mong S, Ellingson BM, Nghiemphu PL et al (2012) Persistent diffusion-restricted lesions in bevacizumab-treated malignant gliomas are associated with improved survival compared with matched controls. AJNR Am J Neuroradiol 33:1763–1770. https://doi.org/10.3174/ajnr.A3053
Cachia D, Elshafeey NA, Kamiya-Matsuoka C et al (2017) Radiographic patterns of progression with associated outcomes after bevacizumab therapy in glioblastoma patients. J Neurooncol 135:75–81. https://doi.org/10.1007/s11060-017-2550-5
Gupta A, Young RJ, Karimi S et al (2011) Isolated diffusion restriction precedes the development of enhancing Tumor in a subset of patients with glioblastoma. AJNR Am J Neuroradiol 32:1301–1306. https://doi.org/10.3174/ajnr.A2479
Acknowledgements
We thank Yudai Ohta and Kyohei Okuda for their technical support in data acquisition.
Funding
This study was supported by JSPS KAKENHI grant number JP20K08135 (A.K.).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analyses were performed by Atsushi Kambe, Shinichiro Kitao and Ryoya Ochiai. The first draft of the manuscript was written by Atsushi Kambe, and all authors commented on previous versions of the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
This retrospective study was approved by our Institutional Review Board, and the requirement for informed consent was waived because of the retrospective nature of this study (approval no. 23A018).
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kambe, A., Kitao, S., Ochiai, R. et al. The utility of arterial spin labeling imaging for predicting prognosis after a recurrence of high-grade glioma in patients under bevacizumab treatment. J Neurooncol 166, 175–183 (2024). https://doi.org/10.1007/s11060-023-04550-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04550-w