Abstract
Purpose
Microsurgery is the mainstay of treatment for large vestibular schwannomas (VS), but the benefits of radiosurgery remain incompletely defined. Here, we aim to use automated volumetric analysis software to quantify the degree of brain stem deformity to predict long-term outcomes of patients with large VS following GKRS.
Methods
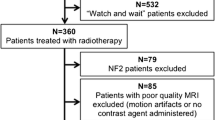
Between 2003 and 2020, 39 patients with large VS (volume > 8 cc) undergoing GKRS with a margin dose of 10–12 Gy were analyzed. The reconstruction 3D MRI was used to evaluate the extent of deformity for predicting the long-term outcome of patients.
Results
Their mean tumor volume was 13.7 ± 6.3 cc, and their mean follow-up after GKRS was 86.7 ± 65.3 months. Favorable clinical outcome was observed in 26 (66.7%) patients, while 13 (33.3%) patients had treatment failure. Patients with small tumor volumes, low vital structure deformity indice [(TV/(BSV + CerV) and (TV + EV)/(BSV + CerV)], and long distance of tumor to the central line were more likely to have favorable clinical outcome after GKRS. Significant prognostic value was with tumor shrinkage ratio (< 50%) were CV, CV/TV, TV/CerV, (TV + EV)/(BSV + CerV), and the distance of tumor to the central line. In cox regression, favorable clinical outcome was correlated with the Charlson comorbidity index and cochlear dosage (both p < 0.05). In multivariant analysis, tumor regression was highly correlated with the CV/TV ratio (p < 0.001).
Conclusions
The brainstem deformity ratio is likely a useful index to assess the clinical and tumor regression outcomes. Clinical outcomes are multifactorial and the tumor regression was highly correlated with the ratio of cystic components.


Similar content being viewed by others
Data Availability
Not applicable.
Abbreviations
- VS:
-
vestibular schwannomas
- GKRS:
-
gamma knife radiosurgery
- Gy:
-
gray
- MRI:
-
Magnetic Resonance Imaging
- VP:
-
ventriculoperitoneal
- SRS:
-
stereotactic radiosurgery
- 3D:
-
3-dimension
- TOF:
-
time of flight
- Gd:
-
Gadolinium
- TV:
-
tumor volume
- BSV:
-
brainstem volume
- CerV:
-
cerebellum volume
- CV:
-
cystic volume
- EV:
-
edema volume
- VV:
-
ventricle volume
- TSR:
-
tumor shrinkage ratio
References
Lee DY, Lerner DK, Naples JG, Brant JA, Bigelow DC, Lee JYK, Alonso-Basanta M, Ruckenstein MJ (2019) Vestibular Schwannoma Tumor size is Associated with Acute vestibular symptoms after Gamma Knife Therapy. Otol Neurotol 40:1088–1093. https://doi.org/10.1097/MAO.0000000000002312
Chung WY, Pan DH, Lee CC, Wu HM, Liu KD, Yen YS, Guo WY, Shiau CY, Shih YH (2010) Large vestibular schwannomas treated by Gamma Knife surgery: long-term outcomes. J Neurosurg 113 Suppl:112–121. https://doi.org/10.3171/2010.8.GKS10954
Pan HC, Sheehan J, Sheu ML, Chiu WT, Yang DY (2012) Intracapsular decompression or radical resection followed by Gamma Knife surgery for patients harboring a large vestibular schwannoma. J Neurosurg 117 Suppl:69–77. https://doi.org/10.3171/2012.6.GKS12697
Klijn S, Verheul JB, Beute GN, Leenstra S, Mulder JJ, Kunst HP, Hanssens PE (2016) Gamma Knife radiosurgery for vestibular schwannomas: evaluation of tumor control and its predictors in a large patient cohort in the Netherlands. J Neurosurg 124:1619–1626. https://doi.org/10.3171/2015.4.JNS142415
Huang CW, Tu HT, Chuang CY, Chang CS, Chou HH, Lee MT, Huang CF (2018) Gamma Knife radiosurgery for large vestibular schwannomas greater than 3 cm in diameter. J Neurosurg 128:1380–1387. https://doi.org/10.3171/2016.12.JNS161530
Langenhuizen P, Zinger S, Hanssens PEJ, Kunst HPM, Mulder JJS, Leenstra S, de With PHN, Verheul JB (2018) Influence of pretreatment growth rate on Gamma Knife treatment response for vestibular schwannoma: a volumetric analysis. J Neurosurg 1–8. https://doi.org/10.3171/2018.6.JNS18516
Watanabe S, Yamamoto M, Kawabe T, Koiso T, Aiyama H, Kasuya H, Barfod BE (2019) Long-term follow-up results of stereotactic radiosurgery for vestibular schwannomas larger than 8 cc. Acta Neurochir (Wien) 161:1457–1465. https://doi.org/10.1007/s00701-019-03951-z
Yang HC, Wu CC, Lee CC, Huang HE, Lee WK, Chung WY, Wu HM, Guo WY, Wu YT, Lu CF (2021) Prediction of pseudoprogression and long-term outcome of vestibular schwannoma after Gamma Knife radiosurgery based on preradiosurgical MR radiomics. Radiother Oncol 155:123–130. https://doi.org/10.1016/j.radonc.2020.10.041
Inoue HK (2005) Low-dose radiosurgery for large vestibular schwannomas: long-term results of functional preservation. J Neurosurg 102 Suppl:111–113
van de Langenberg R, Hanssens PE, Verheul JB, van Overbeeke JJ, Nelemans PJ, Dohmen AJ, de Bondt BJ, Stokroos RJ (2011) Management of large vestibular schwannoma. Part II. Primary Gamma Knife surgery: radiological and clinical aspects. J Neurosurg 115:885–893. https://doi.org/10.3171/2011.6.JNS101963
Yeole U, Prabhuraj AR, Arivazhagan A, Narasingarao KVL, Vazhayil V, Bhat D, Srinivas D, Govindswamy B, Sampath S (2022) Gamma Knife Radiosurgery for large vestibular Schwannoma more than 10 cm (3): a single-center indian study. J Neurol Surg B Skull Base 83:e343–e352. https://doi.org/10.1055/s-0041-1729977
Kondziolka D, Lunsford LD, McLaughlin MR, Flickinger JC (1998) Long-term outcomes after radiosurgery for acoustic neuromas. N Engl J Med 339:1426–1433. https://doi.org/10.1056/nejm199811123392003
Kondziolka D, Lunsford LD, Flickinger JC (2003) Acoustic tumors: operation versus radiation–making sense of opposing viewpoints. Part II. Acoustic neuromas: sorting out management options. Clin Neurosurg 50:313–328
Milligan BD, Pollock BE, Foote RL, Link MJ (2012) Long-term tumor control and cranial nerve outcomes following gamma knife surgery for larger-volume vestibular schwannomas. J Neurosurg 116:598–604. https://doi.org/10.3171/2011.11.JNS11811
Yang HC, Kano H, Awan NR, Lunsford LD, Niranjan A, Flickinger JC, Novotny J Jr, Bhatnagar JP, Kondziolka D (2011) Gamma Knife radiosurgery for larger-volume vestibular schwannomas. Clinical article. J Neurosurg 114:801–807. https://doi.org/10.3171/2010.8.JNS10674
Williams BJ, Xu Z, Salvetti DJ, McNeill IT, Larner J, Sheehan JP (2013) Gamma Knife surgery for large vestibular schwannomas: a single-center retrospective case-matched comparison assessing the effect of lesion size. J Neurosurg 119:463–471. https://doi.org/10.3171/2013.4.JNS122195
Frischer JM, Gruber E, Schoffmann V, Ertl A, Hoftberger R, Mallouhi A, Wolfsberger S, Arnoldner C, Eisner W, Knosp E, Kitz K, Gatterbauer B (2018) Long-term outcome after Gamma Knife radiosurgery for acoustic neuroma of all Koos grades: a single-center study. J Neurosurg 1–10. https://doi.org/10.3171/2017.8.JNS171281
Ruess D, Pohlmann L, Grau S, Hamisch C, Hoevels M, Treuer H, Baues C, Kocher M, Ruge M (2020) Outcome and toxicity analysis of single dose stereotactic radiosurgery in vestibular schwannoma based on the Koos grading system. Sci Rep 10:9309. https://doi.org/10.1038/s41598-020-66213-4
van de Langenberg R, Hanssens PE, van Overbeeke JJ, Verheul JB, Nelemans PJ, de Bondt BJ, Stokroos RJ (2011) Management of large vestibular schwannoma. Part I. Planned subtotal resection followed by Gamma Knife surgery: radiological and clinical aspects. J Neurosurg 115:875–884. https://doi.org/10.3171/2011.6.JNS101958
Gurgel RK, Dogru S, Amdur RL, Monfared A (2012) Facial nerve outcomes after surgery for large vestibular schwannomas: do surgical approach and extent of resection matter? Neurosurg Focus 33:E16. https://doi.org/10.3171/2012.7.Focus12199
Iwai Y, Ishibashi K, Watanabe Y, Uemura G, Yamanaka K (2015) Functional preservation after planned partial resection followed by Gamma Knife Radiosurgery for large vestibular Schwannomas. World Neurosurg 84:292–300. https://doi.org/10.1016/j.wneu.2015.03.012
Tosi U, Lavieri MET, An A, Maayan O, Guadix SW, DeRosa AP, Christos PJ, Pannullo S, Stieg PE, Brandmaier A, Knisely JPS, Ramakrishna R (2021) Outcomes of stereotactic radiosurgery for large vestibular schwannomas: a systematic review and meta-analysis. Neurooncol Pract 8:405–416. https://doi.org/10.1093/nop/npab011
Lefranc M, Da Roz LM, Balossier A, Thomassin JM, Roche PH, Regis J (2018) Place of Gamma Knife Stereotactic Radiosurgery in Grade 4 vestibular Schwannoma based on Case Series of 86 patients with long-term Follow-Up. World Neurosurg 114:e1192–e1198. https://doi.org/10.1016/j.wneu.2018.03.175
Hasegawa T, Fujitani S, Katsumata S, Kida Y, Yoshimoto M, Koike J (2005) Stereotactic radiosurgery for vestibular schwannomas: analysis of 317 patients followed more than 5 years. Neurosurgery 57: 257–265; discussion 257–265 doi:https://doi.org/10.1227/01.neu.0000166542.00512.84
Sun S, Liu A (2012) Long-term follow-up studies of Gamma Knife surgery with a low margin dose for vestibular schwannoma. J Neurosurg 117 Suppl:57–62. https://doi.org/10.3171/2012.7.GKS12783
Dumot C, Pikis S, Mantziaris G, Xu Z, Anand RK, Nabeel AM, Sheehan D, Sheehan K, Reda WA, Tawadros SR, Abdel Karim K, El-Shehaby AMN, Emad Eldin RM, Peker S, Samanci Y, Kaisman-Elbaz T, Speckter H, Hernández W, Isidor J, Tripathi M, Madan R, Zacharia BE, Daggubati LC, Moreno NM, Álvarez RM, Langlois AM, Mathieu D, Deibert CP, Sudhakar VR, Cifarelli CP, Icaza DA, Cifarelli DT, Wei Z, Niranjan A, Barnett GH, Lunsford LD, Bowden GN, Sheehan JP (2022) Stereotactic radiosurgery for Koos grade IV vestibular schwannoma in young patients: a multi-institutional study. J Neurooncol. https://doi.org/10.1007/s11060-022-04134-0
Foote KD, Friedman WA, Buatti JM, Meeks SL, Bova FJ, Kubilis PS (2001) Analysis of risk factors associated with radiosurgery for vestibular schwannoma. J Neurosurg 95:440–449. https://doi.org/10.3171/jns.2001.95.3.0440
Ganz JC, Reda WA, Abdelkarim K (2009) Adverse radiation effects after Gamma Knife surgery in relation to dose and volume. Acta Neurochir (Wien) 151:9–19. https://doi.org/10.1007/s00701-008-0174-4
Lunsford LD, Niranjan A, Flickinger JC, Maitz A, Kondziolka D (2005) Radiosurgery of vestibular schwannomas: summary of experience in 829 cases. J Neurosurg 102 Suppl:195–199
Sharma MS, Kondziolka D, Khan A, Kano H, Niranjan A, Flickinger JC, Lunsford LD (2008) Radiation tolerance limits of the brainstem. Neurosurgery 63:728–732 discussion 732 – 723. https://doi.org/10.1227/01.NEU.0000325726.72815.22
Arvold ND, Pinnell NE, Mahadevan A, Connelly S, Silverman R, Weiss SE, Kelly PJ, Alexander BM (2016) Steroid and anticonvulsant prophylaxis for stereotactic radiosurgery: large variation in physician recommendations. Pract Radiat Oncol 6:e89–e96. https://doi.org/10.1016/j.prro.2015.11.004
Shaw EG, Robbins ME (2006) The management of radiation-induced brain injury. Cancer Treat Res 128:7–22. https://doi.org/10.1007/0-387-25354-8_2
Huang SH, Chuang CC, Wang CC, Wei KC, Chen HC, Hsu PW (2022) Risk factors for peritumoral edema after radiosurgery for intracranial benign meningiomas: a long-term follow-up in a single institution. Neurosurg Focus 53:E7. https://doi.org/10.3171/2022.8.FOCUS22377
Myrseth E, Møller P, Pedersen PH, Vassbotn FS, Wentzel-Larsen T, Lund-Johansen M (2005) Vestibular schwannomas: clinical results and quality of life after microsurgery or gamma knife radiosurgery. Neurosurgery 56: 927–935; discussion 927–935 doi:https://doi.org/10.1055/s-2005-916493
Nakaya K, Niranjan A, Kondziolka D, Kano H, Khan AA, Nettel B, Koebbe C, Pirris S, Flickinger JC, Lunsford LD (2010) Gamma knife radiosurgery for benign tumors with symptoms from brainstem compression. Int J Radiat Oncol Biol Phys 77:988–995. https://doi.org/10.1016/j.ijrobp.2009.06.089
Wangerid T, Bartek J Jr, Svensson M, Förander P (2014) Long-term quality of life and tumour control following gamma knife radiosurgery for vestibular schwannoma. Acta Neurochir (Wien) 156:389–396. https://doi.org/10.1007/s00701-013-1924-5
Inoue HK, Nishi H, Shibazaki T, Ono N (2004) Hearing preservation after radiosurgery combined with or without microsurgery for large vestibular schwannomas: preliminary results. Radiosurgery. Karger Publishers, pp 107–114
Boari N, Bailo M, Gagliardi F, Franzin A, Gemma M, del Vecchio A, Bolognesi A, Picozzi P, Mortini P (2014) Gamma Knife radiosurgery for vestibular schwannoma: clinical results at long-term follow-up in a series of 379 patients. J Neurosurg 121 Suppl:123–142. https://doi.org/10.3171/2014.8.GKS141506
Chihara Y, Ito K, Sugasawa K, Shin M (2007) Neurological complications after acoustic neurinoma radiosurgery: revised risk factors based on long-term follow-up. Acta Otolaryngol Suppl 65–70. https://doi.org/10.1080/03655230701596467
Shirato H, Sakamoto T, Takeichi N, Aoyama H, Suzuki K, Kagei K, Nishioka T, Fukuda S, Sawamura Y, Miyasaka K (2000) Fractionated stereotactic radiotherapy for vestibular schwannoma (VS): comparison between cystic-type and solid-type VS. Int J Radiat Oncol Biol Phys 48:1395–1401. https://doi.org/10.1016/s0360-3016(00)00731-8
Delsanti C, Régis J (2004) [Cystic vestibular schwannomas]. Neurochirurgie 50:401–406
Wu CC, Guo WY, Chung WY, Wu HM, Lin CJ, Lee CC, Liu KD, Yang HC (2017) Magnetic resonance imaging characteristics and the prediction of outcome of vestibular schwannomas following Gamma Knife radiosurgery. J Neurosurg 127:1384–1391. https://doi.org/10.3171/2016.9.JNS161510
Park CK, Kim DC, Park SH, Kim JE, Paek SH, Kim DG, Jung HW (2006) Microhemorrhage, a possible mechanism for cyst formation in vestibular schwannomas. J Neurosurg 105:576–580. https://doi.org/10.3171/jns.2006.105.4.576
Rutten I, Baumert BG, Seidel L, Kotolenko S, Collignon J, Kaschten B, Albert A, Martin D, Deneufbourg JM, Demanez JP, Stevenaert A (2007) Long-term follow-up reveals low toxicity of radiosurgery for vestibular schwannoma. Radiother Oncol 82:83–89. https://doi.org/10.1016/j.radonc.2006.11.019
Acknowledgements
The author would like to thank to the Biostatistics Task Force of Taichung Veterans General Hospital for their kind assistance in the statistical analysis.
Funding
This work was supported by the grant of TCVGH-PU1088103, TCVGH-1117303 C, and TCVGH-1117303D from Taichung Veterans General Hospital.
Author information
Authors and Affiliations
Contributions
HCC and WCY collected the data and drafted the manuscript. MLS, LYP and CCS participated in the study design. LYP and MHS participated in the data collection. MLS and JS participated in the study design and in the statistical analysis. KCS participated in the techniques of automatically calculation in volumetry study. JS participated in the study design and helped drafting the manuscript. HCP participated in the study design and coordination and helped to draft the manuscript. All authors read and approved the final manuscripts.
Corresponding author
Ethics declarations
Institute review board statement
This study was approved by the Ethical Committee of Taichung Veterans General Hospital (No. CE21156A).
Conflict of Interest
The authors declare no conflicts of interest in this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chang, HC., You, W.C., Shen, CC. et al. Using the deformity index of vital structures to predict outcome of patients with large vestibular schwannomas after Gamma Knife radiosurgery. J Neurooncol 162, 179–189 (2023). https://doi.org/10.1007/s11060-023-04280-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-023-04280-z