Abstract
Introduction
Stereotactic radiosurgery (SRS) has shown durable local control for the treatment of metastatic diseasespinal metastases. Multilevel disease or epidural or paraspinal involvement present challenges to achieving local control, and this study aims to analyze treatment outcomes for such lesions.
Methods
Patients treated at a single institution with SRS to the spine from 2010–2018 were retrospectively reviewed. Inclusion criteria required clinical follow-up with either a pain assessment or imaging study. Bulky spine metastasis was defined as consisting of multilevel disease or epidural or paraspinal tumor involvement.
Results
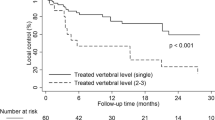
54 patients treated for 62 lesions met inclusion criteria. 42 treatments included at least two vertebrae, and 21 and 31 had paraspinal and epidural involvement, respectively. Treatment regimens had a median 24 Gy in 3 fractions to a volume of 37.75 cm3. Median follow-up was 14.36 months, with 5 instances (8%) of local failure. Median overall survival was 13.32 months. Pain improvement was achieved in 47 treatments (76%), and pain improved with treatment (p < 0.0001). Severe pain (HR = 3.08, p = 0.05), additional bone metastases (HR = 4.82, p = 0.05), and paraspinal involvement (HR = 3.93, p < 0.005) were predictive for worse overall survival. Kaplan–Meier analysis demonstrated that prior chemotherapy (p = 0.03) and additional bone metastases (p = 0.02) were predictive of worse overall survival. Grade < 3 toxicity was observed in 19 cases; no grade ≥ 3 side effects were observed.
Conclusions
SRS can effectively treat bulky metastases to the spine, resulting in improvement of pain with minimal toxicity. Severe pain independently predicts for worse overall survival, indicating that treatment prior to worsening of pain is strongly recommended



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Maranzano E et al (2009) 8 Gy single-dose radiotherapy is effective in metastatic spinal cord compression: results of a phase III randomized multicentre Italian trial. Radiother Oncol 93(2):174–179
Gerszten PC et al (2005) Combination kyphoplasty and spinal radiosurgery: a new treatment paradigm for pathological fractures. Journal of Neurosurgery: Spine 3(4):296–301
Sahgal A et al (2013) Probabilities of radiation myelopathy specific to stereotactic body radiation therapy to guide safe practice. Int J Radiat Oncol Biol Phys 85(2):341–347
Sahgal A et al (2010) Spinal cord tolerance for stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 77(2):548–553
Thibault I et al (2014) Spine stereotactic body radiotherapy for renal cell cancer spinal metastases: analysis of outcomes and risk of vertebral compression fracture. Journal of Neurosurgery: Spine 21(5):711–718
Sahgal A, Larson DA, Chang EL (2008) Stereotactic body radiosurgery for spinal metastases: a critical review. Int J Radiat Oncol Biol Phys 71(3):652–665
Gerszten PC et al (2007) Radiosurgery for spinal metastases: clinical experience in 500 cases from a single institution. Spine 32(2):193–199
Yamada Y et al (2008) High-dose, single-fraction image-guided intensity-modulated radiotherapy for metastatic spinal lesions. Int J Radiat Oncol Biol Phys 71(2):484–490
Moulding HD et al (2010) Local disease control after decompressive surgery and adjuvant high-dose single-fraction radiosurgery for spine metastases. Journal of Neurosurgery: Spine 13(1):87–93
Tao R et al (2016) Stereotactic body radiation therapy for spinal metastases in the postoperative setting: a secondary analysis of mature phase 1–2 trials. Int J Radiat Oncol Biol Phys 95(5):1405–1413
Nguyen Q-N et al (2010) Management of spinal metastases from renal cell carcinoma using stereotactic body radiotherapy. Int J Radiat Oncol Biol Phys 76(4):1185–1192
Maccauro, Giulio, et al. “Physiopathology of spine metastasis. International journal of surgical oncology 2011.
Sahgal A et al (2011) Stereotactic body radiotherapy for spinal metastases: current status, with a focus on its application in the postoperative patient: a review. Journal of Neurosurgery: Spine 14(2):151–166
Gibbs IC et al (2007) Image-guided robotic radiosurgery for spinal metastases. Radiother Oncol 82(2):185–190
Ryu S et al (2004) Patterns of failure after single-dose radiosurgery for spinal metastasis. J Neurosurg 101(3):402–405
Chang EL et al (2007) Phase I/II study of stereotactic body radiotherapy for spinal metastasis and its pattern of failure. Journal of Neurosurgery: Spine 7(2):151–160
Thibault I et al (2015) Salvage stereotactic body radiotherapy (SBRT) following in-field failure of initial SBRT for spinal metastases. Int J Radiat Oncol Biol Phys 93(2):353–360
Chan MW et al (2016) Patterns of epidural progression following postoperative spine stereotactic body radiotherapy: implications for clinical target volume delineation. Journal of Neurosurgery: Spine 24(4):652–659
Cox BW et al (2012) International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 83(5):e597–e605
Arjun S et al (2009) Stereotactic body radiotherapy is effective salvage therapy for patients with prior radiation of spinal metastases. Int J Radiat Oncol Biol Phys 74(3):723–731
Togawa, D., K. U. Lewandrowsky (2006) The pathophysiology of spinal metastases. Cancer in the Spine 17–23.
Kazmi F et al (2018) Spine Stereotactic Radiosurgery Offers Excellent Local Control in Patients with Bulky Spinal Disease. Int J Radiat Oncol Biol Phys 102(3):e268
Beeler WH et al (2019) Local control and toxicity of multilevel spine stereotactic body radiotherapy. Neurosurgery 86(2):164–174
Dunning EC, Butler JS, Morris S (2012) Complications in the management of metastatic spinal disease. World journal of orthopedics 3(8):114
Zeng KL et al (2018) Stereotactic Body Radiation Therapy (SBRT) for Spinal Metastases at the Extremes of the Spine: Imaging-Based Outcomes for Cervical and Sacral Metastases. Int J Radiat Oncol Biol Phys 102(3):e372
Boonstra AM et al (2016) Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Frontiers in psychology 7:1466
Koyfman SA et al (2012) Marginal recurrence requiring salvage radiotherapy after stereotactic body radiotherapy for spinal metastases. Int J Radiat Oncol Biol Phys 83(1):297–302
Puvanesarajah V et al (2015) Prognostic factors associated with pain palliation after spine stereotactic body radiation therapy. Journal of Neurosurgery: Spine 23(5):620–629
Switlyk MD et al (2015) Prognostic factors in patients with symptomatic spinal metastases and normal neurological function. Clin Oncol 27(4):213–221 PMID: 25624156
Leithner A et al (2008) Predictive value of seven preoperative prognostic scoring systems for spinal metastases. Eur Spine J 17(11):1488–1495
Tokuhashi Y et al (2005) A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine 30(19):2186–2191
Yahanda AT, Buchowski JM, Wegner AM (2019) Treatment, complications, and outcomes of metastatic disease of the spine: from Patchell to PROMIS. Annals of translational medicine 7(10):30
Ecker, Robert D., et al. (2005) “Diagnosis and treatment of vertebral column metastases”. Mayo Clinic Proceedings. 80(9).
Montazeri A (2009) Quality of life data as prognostic indicators of survival in cancer patients: an overview of the literature from 1982 to 2008. Health and quality of life outcomes 7(1):102
Maltoni, Marco, et al. “Prognostic factors in advanced cancer patients: evidence-based clinical recommendations—a study by the Steering Committee of the European Association for Palliative Care.” American Society of Clinical Oncology (ASCO), 2005.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Study conception and design was primarily conducted by RO.K, with the assistance of C.R.K. Data preparation, collection, and analysis were performed by RO.K. The first draft of the manuscript was written by RO.K. All authors contributed to the editing of the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The wife of Dr. Kowalchuk is a senior technical product manager at GE Healthcare.
Ethical approval
This study was exempt by the institutional review board and was conducted in accordance with their tenets for a retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary file1 (TIF 31 kb)
Supplemental Fig. 1 Predictive factors for overall survival are demonstrated, with severe pain and additional bone metastases demonstrating statistical significance (p=0.05) and prior palliative chemotherapy trending towards significance (p=0.06)
Rights and permissions
About this article
Cite this article
Kowalchuk, R.O., Waters, M.R., Richardson, K.M. et al. Stereotactic radiosurgery for the treatment of bulky spine metastases. J Neurooncol 148, 381–388 (2020). https://doi.org/10.1007/s11060-020-03534-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03534-4