Abstract
Introduction
Neutrophil-to-lymphocyte ratio (NLR) is a surrogate for systemic inflammatory response and its elevation has been shown to be a poor prognostic factor in various malignancies. Stereotactic radiosurgery (SRS) can induce a leukocyte-predominant inflammatory response. This study investigates the prognostic impact of post-SRS NLR in patients with brain metastases (BM).
Methods
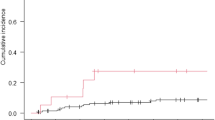
BM patients treated with SRS from 2003 to 2015 were retrospectively identified. NLR was calculated from the most recent full blood counts post-SRS. Overall survival (OS) and intracranial outcomes were calculated using the Kaplan–Meier method and cumulative incidence with competing risk for death, respectively.
Results
188 patients with 328 BM treated with SRS had calculable post-treatment NLR values. Of these, 51 (27.1%) had a NLR > 6. The overall median imaging follow-up was 13.2 (14.0 vs. 8.7 for NLR ≤ 6.0 vs. > 6.0) months. Baseline patient and treatment characteristics were well balanced, except for lower rate of ECOG performance status 0 in the NLR > 6 cohort (33.3 vs. 44.2%, p = 0.026). NLR > 6 was associated with worse 1- and 2-year OS: 59.9 vs. 72.9% and 24.6 vs. 43.8%, (p = 0.028). On multivariable analysis, NLR > 6 (HR: 1.53; 95% CI 1.03–2.26, p = 0.036) and presence of extracranial metastases (HR: 1.90; 95% CI 1.30–2.78; p < 0.001) were significant predictors for worse OS. No association was seen with NLR and intracranial outcomes.
Conclusion
Post-treatment NLR, a potential marker for post-SRS inflammatory response, is inversely associated with OS in patients with BM. If prospectively validated, NLR is a simple, systemic marker that can be easily used to guide subsequent management.

Similar content being viewed by others
References
Nayak L, Lee EQ, Wen PY (2012) Epidemiology of brain metastases. Curr Oncol Rep 14(1):48–54
Patel KR, Lawson DH, Kudchadkar RR et al (2015) Two heads better than one? Ipilimumab immunotherapy and radiation therapy for melanoma brain metastases. Neuro-oncology 17(10):1312–1321
Chowdhary M, Patel KR, Danish HH, Lawson DH, Khan MK (2016) BRAF inhibitors and radiotherapy for melanoma brain metastases: potential advantages and disadvantages of combination therapy. OncoTargets Ther 9:7149–7159
Kocher M, Soffietti R, Abacioglu U et al (2011) Adjuvant whole-brain radiotherapy versus observation after radiosurgery or surgical resection of one to three cerebral metastases: results of the EORTC 22952-26001 study. J Clin Oncol 29(2):134–141
Gaspar L, Scott C, Rotman M et al (1997) Recursive partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37(4):745–751
Sperduto CM, Watanabe Y, Mullan J et al (2008) A validation study of a new prognostic index for patients with brain metastases: the Graded Prognostic Assessment. J Neurosurg 109(Suppl):87–89
Sperduto PW, Berkey B, Gaspar LE, Mehta M, Curran W (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70(2):510–514
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100(1):57–70
Hanahan D, Weinberg RA (2011) Hallmarks of cancer: the next generation. Cell 144(5):646–674
Alagappan M, Pollom EL, von Eyben R et al (2018) Albumin and neutrophil-lymphocyte ratio (NLR) predict survival in patients with pancreatic adenocarcinoma treated with SBRT. Am J Clin Oncol 41(3):242–247
Hyder J, Boggs DH, Hanna A, Suntharalingam M, Chuong MD (2016) Changes in neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios during chemoradiation predict for survival and pathologic complete response in trimodality esophageal cancer patients. J Gastrointest Oncol 7(2):189–195
Shaverdian N, Veruttipong D, Wang J, Schaue D, Kupelian P, Lee P (2016) Pretreatment immune parameters predict for overall survival and toxicity in early-stage non-small-cell lung cancer patients treated with stereotactic body radiation therapy. Clin Lung Cancer 17(1):39–46
Louveau A, Smirnov I, Keyes TJ et al (2015) Structural and functional features of central nervous system lymphatic vessels. Nature 523(7560):337–341
Bambury RM, Teo MY, Power DG et al (2013) The association of pre-treatment neutrophil to lymphocyte ratio with overall survival in patients with glioblastoma multiforme. J Neurooncol 114(1):149–154
Mason M, Maurice C, McNamara MG et al (2017) Neutrophil-lymphocyte ratio dynamics during concurrent chemo-radiotherapy for glioblastoma is an independent predictor for overall survival. J Neurooncol 132(3):463–471
Patel KR, Prabhu RS, Kandula S et al (2014) Intracranial control and radiographic changes with adjuvant radiation therapy for resected brain metastases: whole brain radiotherapy versus stereotactic radiosurgery alone. J Neurooncol 120(3):657–663
Eaton BR, LaRiviere MJ, Kim S et al (2015) Hypofractionated radiosurgery has a better safety profile than single fraction radiosurgery for large resected brain metastases. J Neurooncol 123(1):103–111
Shaw E, Scott C, Souhami L et al (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 47(2):291–298
Patel KR, Chowdhary M, Switchenko JM et al (2016) BRAF inhibitor and stereotactic radiosurgery is associated with an increased risk of radiation necrosis. Melanoma Res 26(4):387–394
Keizman D, Ish-Shalom M, Huang P et al (2012) The association of pre-treatment neutrophil to lymphocyte ratio with response rate, progression free survival and overall survival of patients treated with sunitinib for metastatic renal cell carcinoma. Eur J Cancer 48(2):202–208
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
de Jager CP, Wever PC, Gemen EF et al (2012) The neutrophil-lymphocyte count ratio in patients with community-acquired pneumonia. PLoS ONE 7(10):e46561
Petrie HT, Klassen LW, Kay HD (1985) Inhibition of human cytotoxic T lymphocyte activity in vitro by autologous peripheral blood granulocytes. J Immunol 134(1):230–234
el-Hag A, Clark RA (1987) Immunosuppression by activated human neutrophils. Dependence on the myeloperoxidase system. J Immunol 139(7):2406–2413
McCourt M, Wang JH, Sookhai S, Redmond HP (1999) Proinflammatory mediators stimulate neutrophil-directed angiogenesis. Arch Surg 134(12):1325–1331
McCourt M, Wang JH, Sookhai S, Redmond HP (2001) Activated human neutrophils release hepatocyte growth factor/scatter factor. Eur J Surg Oncol 27(4):396–403
Jabłońska E, Kiluk M, Markiewicz W, Piotrowski L, Grabowska Z, Jabłoński J (2001) TNF-alpha, IL-6 and their soluble receptor serum levels and secretion by neutrophils in cancer patients. Arch Immunol Ther Exp 49(1):63–69
Shamamian P, Schwartz JD, Pocock BJ et al (2001) Activation of progelatinase A (MMP-2) by neutrophil elastase, cathepsin G, and proteinase-3: a role for inflammatory cells in tumor invasion and angiogenesis. J Cell Physiol 189(2):197–206
Scapini P, Nesi L, Morini M et al (2002) Generation of biologically active angiostatin kringle 1–3 by activated human neutrophils. J Immunol 168(11):5798–5804
Kitayama J, Yasuda K, Kawai K, Sunami E, Nagawa H (2010) Circulating lymphocyte is in an important determinant of the effectiveness of preoperative radiotherapy in advaced rectal cancer. Radiat Oncol 5:47
Sharabi AB, Nirschl CJ, Kochel CM et al (2015) Stereotactic radiation therapy augments antigen-specific PD-1-mediated antitumor immune responses via cross-presentation of tumor antigen. Cancer Immunol Res 3(4):345–355
Dovedi SJ, Adlard AL, Lipowska-Bhalla G et al (2014) Acquired resistance to fractionated radiotherapy can be overcome by concurrent PD-L1 blockade. Cancer Res 74(19):5458–5468
Shaverdian N, Wang J, Levin-Epstein R et al (2016) Pro-inflammatory state portends poor outcomes with stereotactic radiosurgery for brain metastases. Anticancer Res 36(10):5333–5337
Mitsuya K, Nakasu Y, Kurakane T, Hayashi N, Harada H, Nozaki K (2017) Elevated preoperative neutrophil-to-lymphocyte ratio as a predictor of worse survival after resection in patients with brain metastasis. J Neurosurg 127(2):433–437
Acknowledgements
Research reported in this publication was supported in part by the Biostatistics and Bioinformatics Shared Resource of Winship Cancer Institute of Emory University and National Institute of Health/National Cancer Institute under award number P30CA138292. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Chowdhary, M., Switchenko, J.M., Press, R.H. et al. Post-treatment neutrophil-to-lymphocyte ratio predicts for overall survival in brain metastases treated with stereotactic radiosurgery. J Neurooncol 139, 689–697 (2018). https://doi.org/10.1007/s11060-018-2914-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-018-2914-5