Abstract
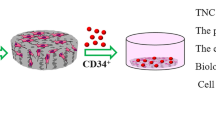
Mesenchymal stem cells (MSCs) and Hematopoietic stem cells (HSCs) are two types of bone marrow stem cells that can proliferate and differentiate into different cell lineages. HSCs interact with MSCs under protective conditions, called niche. Numerous studies have indicated supportive effects of MSCs on HSCs proliferation and differentiation. Furthermore, HSCs have many clinical applications and could treat different hematologic and non-hematologic diseases. For this purpose, there is a need to perform in vitro studies to optimize their expansion. Therefore, various methods including co-culture with MSCs are used to address the limitations of HSCs culture. Some parameters that might be effective for improving the MSC/ HSC co-culture systems. Manipulating culture condition to enhance MSC paracrine activity, scaffolds, hypoxia, culture medium additives, and the use of various MSC sources, have been examined in different studies. In this article, we investigated the potential factors for optimizing HSCs/ MSCs co-culture. It might be helpful to apply a suitable approach for providing high-quality HSCs and improving their therapeutic applications.


Similar content being viewed by others
Abbreviations
- MSCs:
-
Mesenchymal stem cells
- HSCs:
-
Hematopoietic stem cells
- UCB:
-
Umbilical cord blood
- WJ:
-
Wharton jelly
- Flt3L:
-
FMS-like tyrosine kinase-3 ligand
- SCF:
-
Stem cell factor
- G-CSF:
-
Granulocyte colony-stimulating factor
- GM-CSF:
-
Granulocyte–macrophage colony-stimulating factor
- TPO:
-
Thrombopoietin
- Angs:
-
Angiopoietins
- Wnt:
-
Wingless-related integration
- LT-HSCs:
-
Long-term hematopoietic stem cells
- ST-HSCs:
-
Short-term hematopoietic stem cells
- IGFBP1:
-
Insulin-like growth factor-binding protein-1
- NS:
-
Nucleostemin
- Nfix:
-
Nuclear factor I/X
- CFU:
-
Colony forming unit
- CAFC:
-
Cobblestone area forming cells
- DNMT1:
-
DNA methyl-transferase
- LTC-IC:
-
Long-term culture- initiating cell
- EPCR:
-
Endothelial protein C receptor
- VLA-4, 5:
-
Very late antigen-4, 5
- CXCR4:
-
C-X-C chemokine receptor 4
- GVHD:
-
Graft versus host disease
- bFGF:
-
Basic fibroblast growth factor
- LIF:
-
Leukemia inhibitory factor
- SDF:
-
Stromal-derived factor
- TGFβ-RII:
-
Transforming growth factor-beta receptor II
- MVs:
-
Microvesicles
- miRNAs:
-
MicroRNAs
- ROS:
-
Reactive oxygen species
- WJ-MSCs:
-
Wharton jelly-derived mesenchymal stem cells
- ESCs:
-
Embryonic stem cells
- BM-MSCs:
-
Bone marrow-derived MSCs
- CXCL12:
-
C-X-C chemokine ligand 12
- UC:
-
Umbilical cord
- CFU-Meg:
-
Megakaryocyte colony-forming unit
- LFA:
-
Lymphocyte function-associated antigen
- HOXB4:
-
Homeobox protein B 4
- HOXA9:
-
Homeobox protein A 9
- BMI1:
-
Polycomb complex protein BMI-1
- PCL:
-
Polycaprolactone
- FN:
-
Fibronectin
- PDMS:
-
Polymethyl siloxane
- PEG:
-
Polyethylene glycol
- VEGF:
-
Vascular endothelial growth factor
- TEPA:
-
Tetraethylenepentamine
- SR1:
-
Aryl hydrocarbon receptor antagonist
- UM171:
-
Pyrimidoindole derivatives
- P18IN003, P18IN011:
-
P18 inhibitory molecules in the cell cycle
- CHIR99021:
-
Type of glycogen synthase kinase 3β inhibitor
- BIO:
-
Another kind of glycogen synthase kinase 3β inhibitor
- NR-101:
-
A small non-peptidyl agonist molecule of c-MPL
- 5azaD / TSA:
-
5-Aza-2-deoxycytidine / trichostatin A
- GAR:
-
Garcinol; a plant-derived histone acetyltransferase
- AhR:
-
Aryl hydrocarbon receptor
- TMEM183A:
-
Transmembrane protein 183A
- PROCR:
-
Protein C receptor
- mTOR:
-
Mammalian target of rapamycin
- PTEN:
-
Phosphatase and tensin homolog
- PI3K:
-
Phosphoinositide 3-kinase
- GSK3β:
-
Glycogen synthase kinase 3 beta
- STAT5:
-
Signal transducer and activator of transcription 5
- HIF-1α:
-
Hypoxia-inducible factor-1α
- HAT:
-
Histone acetyltransferase
- VPA:
-
Valproic acid
- HDAC:
-
Histone deacetylase
- DEAB:
-
Diethylaminobenzaldehyde
- zVADfmk/zLLYfmk:
-
Caspase and calpain inhibitors
- ALDH:
-
Aldehyde dehydrogenase
- 5-HT:
-
5-Hydroxytryptamine
References
Amiri F, Kiani AA, Bahadori M et al (2021) Co-culture of mesenchymal stem cell spheres with hematopoietic stem cells under hypoxia: a cost-effective method to maintain self-renewal and homing marker expression. Mol Biol Rep 49(2):931–941
Kokkaliaris KD, Scadden DT (2020) Cell interactions in the bone marrow microenvironment affecting myeloid malignancies. Blood Adv 415:3795–3803
Nakahara F, Borger DK, Wei Q et al (2019) Engineering a haematopoietic stem cell niche by revitalizing mesenchymal stromal cells. Nat Cell Biol 215:560–567
Mushahary D, Spittler A, Ce K et al (2018) Isolation, cultivation, and characterization of human mesenchymal stem cells. Cytometry A 931:19–31
Schmelzer E, McKeel DT, Gerlach JC (2019) Characterization of human mesenchymal stem cells from different tissues and their membrane encasement for prospective transplantation therapies. Biomed Res Int 5:1–13
Pittenger MF, Mackay AM, Beck SC et al (1999) Multilineage potential of adult human mesenchymal stem cells. Science 284:143–147
Al-Anazi K (2020) The future role of mesenchymal stem cells in tissue repair and medical therapeutics: realities and expectations. J Reg Med Biol Res 12:1–5
Pittenger MF, Discher DE, Péault BM et al (2019) Mesenchymal stem cell perspective: cell biology to clinical progress. NPJ Regen Med 2(4):22–37
Noort W, Scherjon S, Kleijburg-Van Der Keur C et al (2003) Mesenchymal stem cells in human second-trimester bone marrow, liver, lung, and spleen exhibit a similar immunophenotype but a heterogeneous multilineage differentiation potential. Haematologica 888:845–852
Meng X, Ichim TE, Zhong J et al (2007) Endometrial regenerative cells: a novel stem cell population. J Transl Med 51:1–10
Goodarzi A, Valikhani M, Amiri F et al (2022) The mechanisms of mutual relationship between malignant hematologic cells and mesenchymal stem cells: does it contradict the nursing role of mesenchymal stem cells? Cell Commun Signal 20:21–34
Saleh M, Shams Asanjan K, Movassaghpour Akbari A et al (2015) The Effect of Mesenchymal Stem Cells on Hematopoetic Stem Cells Differentiation. Sci J Iran Blood Transfus Organ 123:292–302
Amiri F, Molaei S, Bahadori M et al (2016) Autophagy-modulated human bone marrow-derived mesenchymal stem cells accelerate liver restoration in mouse models of acute liver failure. Iran Biomed J 203:135
Orkin SH, Zon LI (2008) SnapShot: hematopoiesis. Cell 132(4):712
Mangel M, Bonsall MB (2013) Stem cell biology is population biology: differentiation of hematopoietic multipotent progenitors to common lymphoid and myeloid progenitors. Theor Biol Med Model 10:5
Wilson A, Trumpp A (2006) Bone-marrow haematopoietic-stem-cell niches. Nat Rev Immunol 62:93–106
Gomariz A, Isringhausen S, Helbling PM et al (2020) Imaging and spatial analysis of hematopoietic stem cell niches. Ann NY Acad Sci 14661:5–16
Hurwitz SN, Jung SK, Kurre P (2020) Hematopoietic stem and progenitor cell signaling in the niche. Leukemia 34:3136–3148
Molaei S, Amiri F, Salimi R et al (2022) Therapeutic effects of mesenchymal stem cells-conditioned medium derived from suspension cultivation or silymarin on liver failure mice. Mol Biol Rep 49(11):10315–10325
Zhang P, Zhang C, Li J et al (2019) The physical microenvironment of hematopoietic stem cells and its emerging roles in engineering applications. Stem Cell Res Ther 10:1–13
Futrega K, Atkinson K, Lott WB et al (2017) Spheroid coculture of hematopoietic stem/progenitor cells and monolayer expanded mesenchymal stem/stromal cells in polydimethylsiloxane microwells modestly improves in vitro hematopoietic stem/progenitor cell expansion. Tissue Eng Part C Methods 23:200–218
Huang X, Zhu B, Wang X et al (2016) Three-dimensional co-culture of mesenchymal stromal cells and differentiated osteoblasts on human bio-derived bone scaffolds supports active multi-lineage hematopoiesis in vitro: Functional implication of the biomimetic HSC niche. Int J Mol Med 38:1141–1151
Khong D, Li M, Singleton A et al (2018) Stromalized microreactor supports murine hematopoietic progenitor enrichment. Biomed Microdevices 20:1–9
Mayle A, Luo M, Jeong M et al (2013) Flow cytometry analysis of murine hematopoietic stem cells. Cytometry A 83:27–37
Robinson SN, Ng J, Niu T et al (2006) Superior ex vivo cord blood expansion following co-culture with bone marrow-derived mesenchymal stem cells. Bone Marrow Transplant 37:359–366
Ahmadnejad M, Amirizadeh N, Mehrasa R et al (2017) Elevated expression of DNMT1 is associated with increased expansion and proliferation of hematopoietic stem cells co-cultured with human MSCs. Blood Res 52:25
Romanov YA, Volgina NE, Balashova EE et al (2017) Human umbilical cord mesenchymal stromal cells support viability of umbilical cord blood hematopoietic stem cells but not the “stemness” of their progeny in co-culture. Bull Exp Biol Med 163:523–527
Corselli M, Chin CJ, Parekh C et al (2013) Perivascular support of human hematopoietic stem/progenitor cells. Blood 121(15):2891–2901
Walenda T, Bork S, Horn P et al (2010) Co-culture with mesenchymal stromal cells increases proliferation and maintenance of haematopoietic progenitor cells. J Cell Mol Med 14(1–2):337–350
Oubari F, Amirizade N, Mohammadpour H et al (2015) The important role of FLT3-L in ex vivo expansion of hematopoietic stem cells following co-culture with mesenchymal stem cells. Cell J 17(2):201–210
Ajami M, Soleimani M, Abroun S et al (2019) Comparison of cord blood CD34+ stem cell expansion in coculture with mesenchymal stem cells overexpressing SDF-1 and soluble/membrane isoforms of SCF. J Cell Biochem 120:15297–15309
Cook MM, Doran MR, Kollar K et al (2013) Engraftment outcomes after HPC co-culture with mesenchymal stromal cells and osteoblasts. J Clin Med 2:115–135
Crippa S, Santi L, Berti M et al (2021) Role of ex vivo Expanded Mesenchymal Stromal Cells in Determining Hematopoietic Stem Cell Transplantation Outcome. Front Cell Dev Biol 9:663316
Li T, Chengxin Luo Ch, Zhang J et al (2021) Efficacy and safety of mesenchymal stem cells co-infusion in allogeneic hematopoietic stem cell transplantation: a systematic review and meta-analysis. Stem Cell Res & Ther 12:246
Abbasi-Malati Z, Roushandeh AM, Kuwahara Y et al (2018) Mesenchymal stem cells on horizon: a new arsenal of therapeutic agents. Stem Cell Rev Rep 14:484–499
Aqmasheh S (2017) Effects of mesenchymal stem cell derivatives on hematopoiesis and hematopoietic stem cells. Adv pharm bull 7:165
Qiu G, Zheng G, Ge M et al (2018) Mesenchymal stem cell-derived extracellular vesicles affect disease outcomes via transfer of microRNAs. Stem Cell Res Ther 9:1–9
Sagaradze G, Grigorieva O, Nimiritsky P et al (2019) Conditioned medium from human mesenchymal stromal cells: towards the clinical translation. Int J Mol Sci 20:1656
Lazar-Karsten P, Dorn I, Meyer G et al (2011) The influence of extracellular matrix proteins and mesenchymal stem cells on erythropoietic cell maturation. Vox Sang 1011:65–76
Andrade PZ, dos Santos F, Almeida-Porada G et al (2010) Systematic delineation of optimal cytokine concentrations to expand hematopoietic stem/progenitor cells in co-culture with mesenchymal stem cells. Mol Biosyst 6:1207–1215
Schuster JA, Stupnikov MR, Ma G et al (2012) Expansion of hematopoietic stem cells for transplantation: current perspectives. Exp Hematol Oncol 1:1–6
Noort WA, Kruisselbrink AB, Anker PS et al (2002) Mesenchymal stem cells promote engraftment of human umbilical cord blood–derived CD34+ cells in NOD/SCID mice. Exp Hemato 30:870878
Akhkand SS, Amirizadeh N, Nikougoftar M et al (2016) Evaluation of umbilical cord blood CD34+ hematopoietic stem cells expansion with inhibition of TGF-β receptorII in co-culture with bone marrow mesenchymal stromal cells. Tissue Cell 484:305–311
Asgarpour K, Shojaei Z, Amiri F et al (2020) Exosomal microRNAs derived from mesenchymal stem cells: cell-to-cell messages. Cell Commun Signal 18:1–16
De Luca L, Trino S, Laurenzana I (2016) MiRNAs and piRNAs from bone marrow mesenchymal stem cell extracellular vesicles induce cell survival and inhibit cell differentiation of cord blood hematopoietic stem cells: a new insight in transplantation. Oncotarget 7:6676
Jing D, Fonseca AV, Alakel N et al (2010) Hematopoietic stem cells in coculture with mesenchymal stromal cells-modeling the niche compartments in vitro. Haematologica 95:542–550
Miyoshi H, Shimizu Y, Yasui Y et al (2020) Expansion of mouse primitive hematopoietic cells in three-dimensional cultures on chemically fixed stromal cell layers. Cytotechnology 72(741–750):45
Jozaki T, Aoki K, Mizumoto H et al (2010) In vitro reconstruction of a three-dimensional mouse hematopoietic microenvironment in the pore of polyurethane foam. Cytotechnology 62:531–537
Aggarwal R, Lu J, Pompili VJ et al (2012) Hematopoietic stem cells: transcriptional regulation, ex vivo expansion and clinical application. Curr Mol Med 12:3449
Robinson SN, Simmons PJ, Yang H et al (2011) Mesenchymal stem cells in ex vivo cord blood expansion. Best Pract Res Clin Haematol 24:83–92
De Lima M, Mcniece I, Robinson SN et al (2012) Cord-blood engraftment with ex vivo mesenchymal-cell coculture. N Engl J Med 367:23052315
Mousavi SH, Abroun S, Soleimani M et al (2018) 3-Dimensional nano-fibre scaffold for ex vivo expansion of cord blood haematopoietic stem cells. Artif Cells Nanomed Biotechnol 46:740–748
Mousavi SH, Abroun S, Soleimani M et al (2015) Expansion of human cord blood hematopoietic stem/progenitor cells in three-dimensional Nano scaffold coated with Fibronectin. Int J Hematol Oncol Stem Cell Res 9:72
Raic A, Rödling L, Kalbacher H et al (2014) Biomimetic macroporous PEG hydrogels as 3D scaffolds for the multiplication of human hematopoietic stem and progenitor cells. Biomaterials 35:929–940
Hermitte F, Brunet de la Grange P, Belloc F et al (2006) Very low O2 concentration [0.1%] favors G0 return of dividing CD34+ cells. Stem cells 24:65–73
Zhang CC, Sadek HA (2014) Hypoxia and metabolic properties of hematopoietic stem cells. Anti-oxide Redox Signal 20:1891–1901
Suda T, Takubo K, Semenza GL (2011) Metabolic regulation of hematopoietic stem cells in the hypoxic niche. Cell Stem Cell 9:298–310
Jang YY, Sharkis SJ (2007) A low level of reactive oxygen species selects for primitive hematopoietic stem cells that may reside in the low-oxygenic niche. Blood 110:3056–3063
Zhao D, Liu L, Chen Q et al (2018) Hypoxia with Wharton’s jelly mesenchymal stem cell coculture maintains stemness of umbilical cord blood-derived CD34+ cells. Stem Cell Res Ther 9:1–11
Ezashi T, Das P, Roberts RM (2005) Low O2 tensions and the prevention of differentiation of hES cells. Proc Natl Acad Sci 102:4783–4788
Mohammadali F, Abroun S, Atashi A (2018) Mild hypoxia and human bone marrow mesenchymal stem cells synergistically enhance expansion and homing capacity of human cord blood CD34+ stem cells. Iran J Basic Med Sci 21:709
Amiri F, Halabian R, Dehgan Harati M et al (2015) Positive selection of Wharton’s jelly-derived CD105+ cells by MACS technique and their subsequent cultivation under suspension culture condition: A simple, versatile culturing method to enhance the multipotentiality of mesenchymal stem cells. Hematol 20:208–216
Anzalone R, Iacono ML, Corrao S et al (2010) New emerging potentials for human Wharton’s jelly mesenchymal stem cells: immunological features and hepatocyte-like differentiative capacity. Stem Cells Dev 194:423–438
Nilsson SK, Johnston HM, Whitty GA et al (2005) Osteo pontin, a key component of the hematopoietic stem cell niche and regulator of primitive hematopoietic progenitor cells. Blood 106:1232–1239
Raio L, Cromi A, Ghezzi F et al (2005) Hyaluronan content of Wharton’s jelly in healthy and down syndrome fetuses. Matrix Biol 24:166–174
Li Q, Zhao D, Chen Q et al (2019) Wharton’s jelly mesenchymal stem cell-based or umbilical vein endothelial cell-based serum-free coculture with cytokines supports the ex vivo expansion/maintenance of cord blood hematopoietic stem/progenitor cells. Stem Cell Res Ther 101:1–9
Lo Iacono M, Russo E, Anzalone R et al (2018) Wharton’s jelly mesenchymal stromal cells support the expansion of cord blood–derived CD34+ cells mimicking a hematopoietic niche in a direct cell–cell contact culture system. Cell Transplant 27(1):117–129
Raffo D, Maglioco A, Fernandez Sasso D (2021) A protocol for umbilical cord tissue cryopreservation as a source of mesenchymal stem cells. Mol Biol Rep 48(2):1559–1565
Dai Y, Cui X, Zhang G et al (2022) Development of a novel feeding regime for large scale production of human umbilical cord mesenchymal stem/stromal cells. Cytotechnology 74:351–369
Wu KH, Tsai C, Wu HP et al (2013) Human application of ex vivo expanded umbilical cord-derived mesenchymal stem cells: enhance hematopoiesis after cord blood transplantation. Cell Trans 22:2041–2051
Xu M, Zhang B, Liu Y et al (2014) The immunologic and hematopoietic profiles of mesenchymal stem cells derived from different sections of human umbilical cord. Acta Biochim Biophys Sin 46:1056–1065
Tipnis S, Viswanathan C (2010) Umbilical cord matrix derived mesenchymal stem cells can change the cord blood transplant scenario. Int J Stem Cells 3:103
Yang S, Wei Y, Sun R et al (2020) Umbilical cord blood-derived mesenchymal stromal cells promote myeloid-derived suppressor cell proliferation by secreting HLA-G to reduce acute graft-versus-host disease after hematopoietic stem cell transplantation. Cito Ther 22:718–733
Gao L, Chen X, ZhAng X et al (2006) Human umbilical cord blood-derived stromal cell, a new resource of feeder layer to expand human umbilical cord blood CD34+ cells in vitro. Blood Cells Mol Dis 36:322–328
Chen Y, Liang Y, Luo X et al (2020) Oxidative resistance of leukemic stem cells and oxidative damage to hematopoietic stem cells under pro-oxidative therapy. Cell Death Dis 11:1–12
Hu L, Zhang Y, Miao W et al (2019) Reactive oxygen species and Nrf2: functional and transcriptional regulators of hematopoiesis. Oxid Med Cell Longev 2019:5153268
Baur JA, Sinclair DA (2006) Therapeutic potential of resveratrol: the in vivo evidence. Nat Rev Drug Discov 5:493–506
Heinz N, Ehrnström B, Schambach A et al (2015) Comparison of different cytokine conditions reveals resveratrol as a new molecule for ex vivo cultivation of cord blood-derived hematopoietic stem cells. Stem Cells Transl Med 4:1064–1072
Tang C, Zhang W, Cai H et al (2019) Resveratrol improves ex vivo expansion of CB-CD34+ cells via downregulating intracellular reactive oxygen species level. J Cell Biochem 120:7778–7787
Vaidya A, Kale V, Poonawala M et al (2018) Mesenchymal stromal cells enhance the hematopoietic stem cell-supportive activity of resveratrol. Regen Med 13:409–425
Zaker F, Nasiri N, Oodi A et al (2013) Evaluation of umbilical cord blood CD34+ hematopoietic stem cell expansion in co-culture with bone marrow mesenchymal stem cells in the presence of TEPA. Hematology 18:39–45
Zhang Y, Gao Y (2016) Novel chemical attempts at ex vivo hematopoietic stem cell expansion. Int J Hematol 103:519–529
Singh KP, Casado FL, Opanashuk LA et al (2009) The aryl hydrocarbon receptor has a normal function in the regulation of hematopoietic and other stem/progenitor cell populations. Biochem Pharmacol 77:577–587
Fares I, Chagraoui J, Gareau Y et al (2014) Cord blood expansion Pyrimidoindole derivatives are agonists of human hematopoietic stem cell self-renewal. Science 345:1509–1512
Gao Y, Yang P, Shen H et al (2015) Small molecule inhibitors targeting INK4 protein p18[INK4C] enhance ex vivo expansion of haematopoietic stem cells. Nat Commun 6:6328
Chen C, Liu Y, Liu R et al (2008) TSC-mTOR maintains quiescence and function of hematopoietic stem cells by repressing mitochondrial biogenesis and reactive oxygen species. J Exp Med 205:2397–2408
Ying QL, Wray J, Nichols J et al (2008) The ground state of embryonic stem cell self-renewal. Nature 453:519–523
Ko KH, Holmes T, Palladinetti P et al (2011) GSK-3β inhibition promotes engraftment of ex vivo-expanded hematopoietic stem cells and modulates gene expression. Stem Cells 29:108–118
Araki H, Yoshinaga K, Boccuni P et al (2007) Chromatin-modifying agents permit human hematopoietic stem cells to undergo multiple cell divisions while retaining their repopulating potential. Blood 109:3570–3578
Nishino T, Wang C, Mochizuki-Kashio M et al (2011) Ex vivo expansion of human hematopoietic stem cells by garcinol, a potent inhibitor of histone acetyltransferase. PLoS ONE 6:e24298
De Felice L, Tataelli C, Mascolo MG et al (2005) Histone deacetylase inhibitor valproic acid enhances the cytokine-induced expansion of human hematopoietic stem cells. Cancer Res 65:1505–1513
Chute JP, Muramoto GG, Whitesides J et al (2006) Inhibition of aldehyde dehydrogenase and retinoid signaling induces the expansion of human hematopoietic stem cells. Proc Natl Acad Sci USA 103:1707–1712
Yang M, Li K, Ng PC et al (2007) Promoting effects of serotonin on hematopoiesis: ex vivo expansion of cord blood CD34+ stem/progenitor cells, proliferation of bone marrow stromal cells, and antiapoptotic. Stem Cells 25:1800–1806
Ms V, Kale VP, Limaye LS (2010) Expansion of cord blood CD34 cells in presence of zVADfmk and zLLYfmk improved their in vitro functionality and in vivo engraftment in NOD/SCID mouse. PLoS ONE 58:e12221
Ogilvy S, Metcalf D, Print CG et al (1999) Constitutive Bcl-2 expression throughout the hematopoietic compartment affects multiple lineages and enhances progenitor cell survival. Proc Natl Acad Sci USA 96:14943–14948
Driscoll J, Patel T (2019) The mesenchymal stem cell secretome as a cellular regenerative therapy for liver disease. J gastroenterol 54:763–773
Jiang H, Wang H, Liu T (2018) Co-cultured the MSCs and cardiomyocytes can promote the growth of cardiomyocytes. Cytotechnology 70:793–806
Bazinet A, Popradi G (2019) A general practitioner’s guide to hematopoietic stem-cell transplantation. Curr Oncol 26:187
Takagaki S, Yamashita R, Hashimoto N et al (2019) Galactosyl carbohydrate residues on hematopoietic stem/progenitor cells are essential for homing and engraftment to the bone marrow. Sci Rep 9:1–11
Feng Q, Chai C, Jiang XS et al (2006) Expansion of engrafting human hematopoietic stem/progenitor cells in three-dimensional scaffolds with surface immobilized fibronectin. J Biomed Mater Res A 78:781–791
Acknowledgements
This work was founded by the Hamadan University of Medical Sciences, Code: IR.UMSHA.REC.1400.183, [grant number: 140004012854]. Special thanks to Delaram Yaghoubzadeh.
Funding
This work was founded by the Hamadan University of Medical Sciences [grant No. 140004012854].
Author information
Authors and Affiliations
Contributions
Mandana Shirdareh has written the first draft of the manuscript. Mohammad Pouya Samiee and Armita Safari have participated to write the first manuscript and figure preparation. Fatemeh Amiri has reviewed the text. All authors commented on previous versions of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors contributed in this review clearly state that there is no conflict of interest either in authorship or financial benefits.
Ethical approval
This is a review article. The research ethic committee of Hamadan University of Medical Sciences has confirmed that no ethical approval is required.
Consent to participate
Not applicable.
Consent to Publication
All authors reviewed the manuscript and consent to publish.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shirdare, M., Amiri, F., Samiee, M.P. et al. Influential factors for optimizing and strengthening mesenchymal stem cells and hematopoietic stem cells co-culture. Mol Biol Rep 51, 189 (2024). https://doi.org/10.1007/s11033-023-09041-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11033-023-09041-9