Abstract
Background
Polycystic ovary syndrome (PCOS) is known as a multifactorial and multi-gene-mediated endocrine disorder among women of reproductive age. FoxO1 and FoxO3 are members of the forkhead transcriptional factors family that play a pivotal role in the function of ovaries. The current work is aimed at investigating the association between gene variants of FoxO1 and FoxO3 and the risk of PCOS in a sample of the Iranian population.
Methods and results
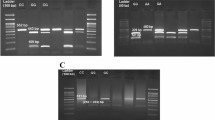
We recruited 200 women diagnosed with PCOS and 200 healthy women. Both polymerase PCR–RFLP and ARMS-PCR methods were used for genotyping. Sanger sequencing was recruited to confirm the genotyping results. The T allele of rs17592236 and the C allele of rs12585277 decreased PCOS risk by 29 and 28%, respectively. In contrast, the C allele of rs2253310 and G allele of rs2802292 increased the risk of PCOS by 1.39 and 1.63 folds, correspondingly. Bioinformatics results showed that some genes, including matrix metallopeptidase 9 (MMP-9), phosphoinositide-3-Kinase Regulatory Subunit 224 1 (PIK3R1), peroxisome proliferator-activated receptor Gamma (PPARG), and glycogen synthase 225 kinase-3 beta (GSK-3 beta) have significant interactions with FoxO1, suggesting that FoxO1 might have crucial roles in regulating different signaling pathways in ovarian cells.
Conclusion
We found that FoxO1 rs17592236C > T and rs12585277C > T had a protective role against PCOS, while FoxO3 rs2253310C > G and rs2802292G > T enhanced the risk of this metabolic disorder in our population. Additional studies on larger populations with varying races are needed to confirm these findings.
Graphical abstract




Similar content being viewed by others
Data availability
The data in this manuscript are available from the corresponding author upon reasonable request.
References
Pal L, Pathy S (2019) Polycystic ovarian syndrome. In: Norwitz ER, Zelop CM, Miller DA, Keefe DL (eds) Evidence-based obstetrics and gynecology. Wiley, Hoboken, pp 117–129
Muhas C et al (2021) An overview on polycystic ovary syndrome (PCOS). Technol Innov Pharm Res 6:19–30
Goodarzi MO et al (2011) Polycystic ovary syndrome: etiology, pathogenesis and diagnosis. Nat Rev Endocrinol 7(4):219–231
Hart R et al (2010) Serum antimullerian hormone (AMH) levels are elevated in adolescent girls with polycystic ovaries and the polycystic ovarian syndrome (PCOS). Fertil Steril 94(3):1118–1121
Eshre, R. and Group, A.-S.P.C.W (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome (PCOS). Hum Reprod (Oxf, Engl) 19(1):41–47
Azziz R et al (2006) Criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an androgen excess society guideline. J Clin Endocrinol Metab 91(11):4237–4245
Wolf WM et al (2018) Geographical prevalence of polycystic ovary syndrome as determined by region and race/ethnicity. Int J Environ Res Public Health 15(11):2589
Skiba MA et al (2018) Understanding variation in prevalence estimates of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update 24(6):694–709
Esmaeilzadeh S et al (2014) Polycystic ovary syndrome in Iranian adolescents. Int J Adolesc Med Health 26(4):559–565
Mani H et al (2015) Clinical characteristics of polycystic ovary syndrome: investigating differences in White and South Asian women. Clin Endocrinol 83(4):542–549
Valgeirsdottir H et al (2021) Polycystic ovary syndrome and risk of stillbirth: a nationwide register-based study. BJOG 128(13):2073–2082
Osibogun O et al (2020) Polycystic ovary syndrome and cardiometabolic risk: opportunities for cardiovascular disease prevention. Trends Cardiovasc Med 30(7):399–404
Azziz R (2018) Polycystic ovary syndrome. Obstet Gynecol 132(2):321–336
Cooney LG, Dokras A (2017) Depression and anxiety in polycystic ovary syndrome: etiology and treatment. Curr Psychiatry Rep 19(11):1–10
Chaudhary H et al (2021) The role of polymorphism in various potential genes on polycystic ovary syndrome susceptibility and pathogenesis. J Ovarian Res 14(1):1–21
Moran LJ et al (2009) Treatment of obesity in polycystic ovary syndrome: a position statement of the Androgen Excess and Polycystic Ovary Syndrome Society. Fertil Steril 92(6):1966–1982
Vink J et al (2006) Heritability of polycystic ovary syndrome in a Dutch twin-family study. J Clin Endocrinol Metab 91(6):2100–2104
Mykhalchenko K et al (2017) Genetics of polycystic ovary syndrome. Expert Rev Mol Diagn 17(7):723–733
Karakaya C et al (2022) Further delineation of familial polycystic ovary syndrome (PCOS) via whole-exome sequencing: PCOS-related rare FBN3 and FN1 gene variants are identified. J Obstet Gynaecol Res 48(5):1202–1211
Xu R, Wang Z (2021) Involvement of transcription factor FoxO1 in the pathogenesis of polycystic ovary syndrome. Front Physiol 12:649295
Lee S, Dong HH (2017) FoxO integration of insulin signaling with glucose and lipid metabolism. J Endocrinol 233(2):R67
Wang Z et al (2016) Post-translational modifications of FOXO family proteins. Mol Med Rep 14(6):4931–4941
Vickers NJ (2017) Animal communication: when i’m calling you, will you answer too? Curr Biol 27(14):R713–R715
Gong Y et al (2020) Growth hormone activates PI3K/Akt signaling and inhibits ROS accumulation and apoptosis in granulosa cells of patients with polycystic ovary syndrome. Reprod Biol Endocrinol 18(1):1–12
Obexer P et al (2007) FKHRL1-mediated expression of Noxa and Bim induces apoptosis via the mitochondria in neuroblastoma cells. Cell Death Differ 14(3):534–547
Mikaeili S et al (2016) Altered FoxO3 expression and apoptosis in granulosa cells of women with polycystic ovary syndrome. Arch Gynecol Obstet 294(1):185–192
ESHRE, T.R. and Group, A.-S.P.C.W (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril 81(1):19–25
Ghasemi M et al (2020) An association study of polymorphisms in the H19 imprinted gene in an Iranian population with the risk of polycystic ovary syndrome. Biol Reprod 103(5):978–985
Nasiri H et al (2005) Modified salting-out method: high-yield, high-quality genomic DNA extraction from whole blood using laundry detergent. J Clin Lab Anal 19(6):229–232
Sharma M et al (2020) PCOSKBR2: a database of genes, diseases, pathways, and networks associated with polycystic ovary syndrome. Sci Rep 10(1):1–11
Kanehisa M et al (2017) KEGG: new perspectives on genomes, pathways, diseases and drugs. Nucleic Acids Res 45(D1):D353–D361
Croft D et al (2010) Reactome: a database of reactions, pathways and biological processes. Nucl Acids Res 39(suppl_1):D691–D697
Shannon P et al (2003) Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res 13(11):2498–2504
Luddi A et al (2018) Matrix metalloproteinases and their inhibitors in human cumulus and granulosa cells as biomarkers for oocyte quality estimation. Fertil Steril 109(5):930-939 e933
Moss LAS et al (2012) Matrix metalloproteinases: changing roles in tumor progression and metastasis. Am J Pathol 181(6):1895–1899
Dambala K et al (2019) Biomarkers of endothelial dysfunction in women with polycystic ovary syndrome. Angiology 70(9):797–801
Gomes VA et al (2011) Imbalanced circulating matrix metalloproteinases in polycystic ovary syndrome. Mol Cell Biochem 353(1):251–257
Goldman S, Shalev E (2004) MMPS and TIMPS in ovarian physiology and pathophysiology. Front Biosci 9(4):2474–2483
Kettunen P et al (2015) Genetic variants of GSK3B are associated with biomarkers for Alzheimer’s disease and cognitive function. J Alzheimers Dis 44(4):1313–1322
Schaffer BA et al (2008) Association of GSK3B with Alzheimer disease and frontotemporal dementia. Arch Neurol 65(10):1368–1374
Ismail AB et al (2022) The expression profile of WNT/β-catanin signalling genes in human oocytes obtained from polycystic ovarian syndrome (PCOS) patients. Zygote 30:1–7
Chang W et al (2008) Adipocytes from women with polycystic ovary syndrome demonstrate altered phosphorylation and activity of glycogen synthase kinase 3. Fertil Steril 90(6):2291–2297
Genin EC et al (2014) Concise review: forkhead pathway in the control of adult neurogenesis. Stem Cells 32(6):1398–1407
van der Vos KE, Coffer PJ (2011) The extending network of FOXO transcriptional target genes. Antioxid Redox Signal 14(4):579–592
Tamura H et al (2009) Melatonin and the ovary: physiological and pathophysiological implications. Fertil Steril 92(1):328–343
Castrillon DH et al (2003) Suppression of ovarian follicle activation in mice by the transcription factor Foxo3a. Science 301(5630):215–218
Muller Y, et al (2007) Functional variants in FOXO1A are associated with type 2 diabetes and obesity in pima Indians. Diabetes 56
Li T et al (2011) Association analyses between the genetic polymorphisms of HNF4A and FOXO1 genes and Chinese Han patients with type 2 diabetes. Mol Cell Biochem 353(1):259–265
Hussain S et al (2021) No association between a genetic variant of FOXO3 and risk of type 2 diabetes mellitus in the elderly population of north India. Indian J Clin Biochem 36(3):330–336
Morris BJ et al (2016) Association analysis of FOXO3 longevity variants with blood pressure and essential hypertension. Am J Hypertens 29(11):1292–1300
Magno LAV et al (2011) Genetic variations in FOXO3A are associated with Bipolar Disorder without confering vulnerability for suicidal behavior. J Affect Disord 133(3):633–637
Wang S et al (2019) Micro-RNA-27a/b negatively regulates hepatic gluconeogenesis by targeting FOXO1. Am J Physiol-Endocrinol Metab 317(5):E911–E924
Yu H et al (2014) Predisposition to Behçet’s disease and VKH syndrome by genetic variants of miR-182. J Mol Med 92(9):961–967
Grossi V et al (2018) The longevity SNP rs2802292 uncovered: HSF1 activates stress-dependent expression of FOXO3 through an intronic enhancer. Nucleic Acids Res 46(11):5587–5600
Bae H et al (2018) Effects of FOXO3 polymorphisms on survival to extreme longevity in four centenarian studies. J Gerontol Ser A 73(11):1439–1447
Acknowledgements
The authors would like to thank the technical staff of the Cellular & Molecular Research Center, Zahedan University of Medical Sciences, for their support.
Funding
The current study received no funding.
Author information
Authors and Affiliations
Contributions
Conceptualization, SS; Clinical assessments: MG; writing-original draft preparation, AR, MHN, MS-M and SS; writing-review and editing, SS, MHN; supervision, SS, RS. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Ethical approval
The ethics committee of Mashhad University of Medical Sciences (Ethical code: IR.MUMS.REC.1400.375) approved the protocol of the current study.
Consent to publish
Not applicable.
Consent to participate
Informed consent was taken from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rakhshani Nejad, A., Sargazi, S., Ghasemi, M. et al. Association study to evaluate Foxo1 and Foxo3 gene polymorphisms in polycystic ovary syndrome: a preliminary case–control study and in silico analysis. Mol Biol Rep 50, 3569–3580 (2023). https://doi.org/10.1007/s11033-023-08292-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-023-08292-w