Abstract
Introduction
The genetic component, including genes and their variants, plays a significant role in the pathophysiology of arterial hypertension (AH). Thus, clinical, epidemiological and genetic studies have been carried out to improve the understanding of disease mechanisms, improve diagnostic quality and contribute to prevention.
Objective
To determine the association of risk factors, biochemical parameters and different ACE gene polymorphisms with AH.
Method
The case-control study was carried out in the population of Ouro Preto, Brazil. The subjects answered a questionnaire containing clinical and sociodemographic data. The ACE gene polymorphisms rs4291, rs4363 and rs4335 were evaluated by real time-polymerase chain reaction (real-time PCR) in 310 people (155 hypertensive and 155 normotensive patients), in addition to biochemical parameters. A multivariate logistic regression model was used to identify factors associated with AH. Analysis of continuous variables was performed using the Kruskal-Wallis test to assess significance between groups and Dunn’s post-test for multiple comparisons.
Results
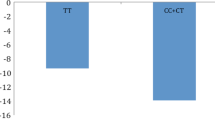
The results showed that AH was associated with age, education, smoking, obesity and high levels of triglycerides, sodium, glucose and uric acid. Regarding the biochemical parameters, in hypertensive patients, the rs4363 and rs4335 polymorphisms were associated with high levels of triglycerides, urea and glucose; the rs4291 polymorphism was associated with elevated urea and glucose levels. No association was detected between SNPs and HA.
Conclusion
AH was associated with socioeconomic status, lifestyle habits and biochemical parameters. ACE polymorphisms may have influenced the levels of triglycerides, urea and glucose in hypertensive patients.




Similar content being viewed by others
References
Gupta A, Patel RAG (2022) Peripheral arterial disease and hypertension. Curr Opin Cardiol. 5:403–412
Malachias MVB, Souza WKSB, Plavnik FL et al (2016) 7ª Dir Bras Hiperten arterial. Arq Bras Cardiol 107(3Supl3):1–83
Sousa AC, Reis RP, Pereira A et al (2018a) Genetic polymorphisms Associated with the onset of arterial hypertension in a Portuguese Population. Acta Med Port Oct 31(10):542–550
Menni C, Mangino M, Zhang F et al (2013) Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens 31(12):2356–2361
Inanır A, Yigit S, Tural S, Ozturk SD, Akkanet S, Habiboğlu A (2012) Significant association between insertion/deletion polymorphism of the angiotensin-convertig enzyme gene and ankylosing spondylitis. Mol Vis 18:2107–2113
National Library of Medicine (2022) ACE angiotensin I converting enzyme [Homo sapiens (human)]. National Center for Biotechnology Information. https://www.ncbi.nlm.nih.gov/gene/1636?_ga=2.257428098.864490725.1668028647-1628942924.1668028647. Accessed November 09, 2022
Bray MS, Hagberg JM, Pérusse L et al (2009) The human gene map for performance and health-related fitness phenotypes. Med Sci Sports Exercise 41(1):34–72
Mikrut K, Kupsz J, Koülik J et al (2016) Angiotensin-converting enzyme inhibitors reduce oxidative stress intensity in hyperglicemic conditions in rats independently from bradykinin receptor inhibitors. Croat Med J 57(4):371–380
Martínez-Rodríguez N, Posadas-Romero C, Villareal-Molina T et al (2013) Single nucleotide polymorphisms of the angiotensin-converting enzyme (ACE) gene are Associated with essential hypertension and increased ACE enzyme levels in mexican individuals. PLoS ONE. 5:65700
Martínez-Ríos MA, Alvarez-Léon E, Totomoch A et al (2014) Haplotypes of the angiotensin-converting enzyme (ACE) gene are associated with coronary artery disease but not with restenosis after coronary stenting. Exp Mol Pathol 97(1):166–170
Kulminski AM, Culminskaya IV, Ukraintseva SV et al (2010) Polymorphisms in the ACE and ADRB2 genes and risks of Aging-Associated phenotypes: the case of myocardial infarction. Rejuvenation Res 26 out 3(1):13–21
Zhu L, Zhang X, Fang Z et al (2020) Association between serum uric acid and pre-hypertension and hypertension among chinese adults. Soc Bra Cardiol 6(116):1072–1107
Bahramali E, Firouzabadi N, Rajabia M et al (2017) Association of renin–angiotensin–aldosterone system gene polymorphisms with left ventricular hypertrophy in patients with heart failure with preserved ejection fraction: a case–control study. Dev Immunol 4(3):1–7
Grimson S, Cox AJ, Pringle KG et al (2016) The prevalence of unique SNPs in the renin-angiotensin system highlights the need for pharmacogenetics in indigenous Australians. Clin Exp Pharmacol Physiol 2(43):157–160
Angunsri R, Sritharathikhun T, Suttirat S et al (2009) Association of angiotensin-converting enzyme gene promoter single nucleotide polymorphisms and haplotype with major depression in a northeastern thai population. JRAAS 10(3):181–184
Wetmore JB, Johansen KL, Sen S et al (2006) An angiotensin converting enzyme haplotype predicts survival in patients with end stage renal disease. Sprin-Verlag 5(120):201–210
Aggarwal P, Agarwal N, Das N et al (2015) Association of polymorphisms in angiotensin-converting enzyme gene with gestational diabetes mellitus in indian women. Int J Appl Basic Med Res 6(1):31–37
Stone NJ, Robinson J, Lichtenstein AH et al (2014) ACC/AHA cholesterol Guideline Panel. Treatment of blood cholesterol to reduce atherosclerotic cardiovascular disease risk in adults: synopsis of the 2013 ACC/AHA cholesterol guideline. Ann Intern Med 160(5):339–343
Menni C, Mangino M, Zhang et al (2013) Heritability analyses show visit-to-visit blood pressure variability reflects different pathological phenotypes in younger and older adults: evidence from UK twins. J Hypertens 31(12):2356–2361
Singh GM, Danaei G, Pelizzari PM et al (2012) The age associations of blood pressure, cholesterol, and glucose: analysis of health examination surveys from international populations. Circulation 125(18):2204–2211
Leng B, JIN Y, LI G et al (2015) Socioeconomic status andhypertension: ameta-analysis. J Hypertens 1(33):221–229
Nishida W, Ziersch A, Zanelatto C et al (2020) Education across the life-course and hypertension in adults from Southern Brazil. Ciên Saúde Coletiva 8(25):3063–3074
Mills KT, Bundy JD, Kelly TN et al (2016) Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation 134(6):441–450
Lan R, Bulsara MK, Pant PD et al (2021) Relationship between cigarette smoking and blood pressure in adults in Nepal: a population-based cross-sectional study. PLOS Glob Public Health 1(11):e0000045
Malta DC, Gonçalves RPF, Machado IE et al (2018) Prevalence of arterial hypertension according to different diagnostic criteria, National Health Survey. Rev Bra Epid 2(21):22–26
Duvivier BMFM, Bolijn JE, Koster A et al (2018) Reducing sitting time versus adding exercise: differential effects on biomarkers of endothelial dysfunction and metabolic risk. Sci Rep 8:8650–8657
Hall JEC, Silva JMAA, Wang ZME (2015) Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res 116:991–1006
Chen ML, Huang TP, Chen TW et al (2018) Interactions of genes and Sodium Intake on the development of hypertension: a cohort-based case-control study. Environ Res Pub Health 10(15):1–10
Freire RS, Reis VMCP, Brito AB et al (2020) Analysis of the interrelationships between factors influencing blood pressure in adults. Rev Saúde Pública 54:147
Sarwar MS, Adnan T, Hossain MD et al (2014) Evaluation of serum lipid Profi le in patients with hypertension living in a Coastal Region of Bangladesh. Drug Res 3(24):353–357
Choudhury KN, Mainuddin A, Wahiduzzaman M et al (2014) Serum lipid profile and its association with hypertension in Bangladesh. Vasc Health Risk Manage 1(10):327–332
Kanwar G, Jain N, Kirad S et al (2014) A study on serum lipid profile in hypertensive patients of Hadoti region. Impact: Ijranss 2(8):53–60
Nayak P, Panda S, Thatoi PK et al (2016) Evaluation of lipid Profile and Apolipoproteins in essential hypertensive patients. J Clin And Diagn Res 10(2):01–06
Pyadala N, Bobbiti RR, Borugadda R et al (2017) Assessment of lipid profile among hypertensive patients attending to a rural teaching hospital, Sangareddy. Int J Med Scien Pub Health 6(1):1–4
Hamrahian SM (2017) Management of hypertension in patients with chronic kidney disease. Curr Hypertens Rep 5(5):5–7
Teixeira JFG, Maíra RB, Fernanda M et al (2016) Hypertensives’ knowledge about High- Sodium Foods and their behavior. Arq Bras Cardiol 5(106):404–410
Qiu M, Shen W, Song X et al (2015) Effects of Prediabetes Mellitus alone or more hypertension on subsequent occurrence of Cardiovascular Disease and Diabetes Mellitus Longitudinal Study. Epidemiology 2(3):525–530
Mancia G, Bombelli M, Cuspidi C et al (2017) Cardiovascular risk associated with White-Coat hypertension. Hypertension 70(4):668–675
Soletsky B, Feig D (2012) Uric acid reduction rectifies prehypertension in obese adolescents. Clin Trial 5(40):1148–1156
Liu L, Gu Y, Li C et al (2016) Serum uric acid is an independent predictor for developing prehypertension: a population-based prospective cohort study. J Hum Hypertens 1(1):1–5
Cao Z, Cheng Y, Li S et al (2019) Mediation of the efect of serum uric acid on the risk of developing hypertension: a population-based cohort study. J Transl Med 202(17):1–10
Zheng H, Xu H, Cui B et al (2013) Association between polymorphism of the G-protein β3 subunit C825T and essential hypertension: an updated meta-analysis involving 36,802 subjects. Biol Res 46:265–273
Riet LT, Van EJHM, Roks AJM et al (2015) Renin–Angiotensin–Aldosterone Syst Alterations Hypertens Circul Res 116(6):960–975
Pahlavani M, Kalupahana NS, Ramalingam L et al (2017) Regulation and functions of the renin-angiotensin system in white and brown adipose tissue. Compr Physiol 7:1137–1150
Oliveira FF, Berreta JM, Chen ES et al (2016) Pharmacogenetic effects of angiotensin-converting enzyme inhibitors over age- related urea and creatinine variations in patients with dementia due to Alzheimer disease. Colom Med 7(2):76–80
Filha RS, Pinheiro SVBP, Cordeiro TM et al (2019) Evidence for a role of angiotensin converting enzyme 2 in proteinuria of idiopathic nephrotic syndrome. Biosci Rep 39(1):BSR20181361
Acknowledgements
We thank all patients who agreed to participate in this study. We are grateful for the assistance provided by Clinical Analysis Laboratory (LAPAC), Laboratory of Epidemiology of the School of Medicine, Laboratory of Epidemiology of the School of Pharmacy, Laboratory of Biochemistry and Clinical Research Laboratory of the Federal University of Ouro Preto.
Funding
This study was supported by Ouro Preto Municipal Health Department (18.295.295/0001-36), Federal University of Ouro Preto (UFOP) [Grant No. 23109.004080/2019-88], Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) [Finance Code 001], Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) [Grant No. 310905/2020-6, CNPq Research Productivity Scholarship] and Fundação de Amparo à Pesquisa do Estado de Minas Gerais [Grant No. APQ-03555-22].
Author information
Authors and Affiliations
Contributions
All of the authors discussed the results and approved the final manuscript. LCA carried out the experiments, contributed to data interpretation and wrote the manuscript. AAL, LFMT, WCV, NTS, TCA and VAB contributed to the experimental design, data interpretation and writing of the manuscript. WRC, ASM and LBM supported the experiments. GNS was the advisor, contributed to the experimental design and data interpretation as well as critically read the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no financial or proprietary interests in any material discussed in this article
Informed consent
Informed consent was obtained from all individual participants included in the study.
Ethical approval
This study was carried out in accordance with the principles of the Declaration of Helsinki. The study was approved by the Committees of Research Ethics of the University Federal of Ouro Preto (CAAE 22455119.0.0000.5150).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
da Agostini, L., Cunha, W.R., Silva, N.N.T. et al. Angiotensin-converting enzyme gene (ACE) polymorphisms are associated with dysregulation of biochemical parameters in hypertensive patients. Mol Biol Rep 50, 1487–1497 (2023). https://doi.org/10.1007/s11033-022-08128-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-08128-z