Abstract
Background
Diabetes is among the leading causes of reproductive system failure and infertility in both women and men. Inflammation and oxidative stress have a main role in the development of diabetes. Eugenol or clove oil is a phenolic monoterpenoid with antioxidant and anti-inflammatory properties. Here, the effects of eugenol on diabetes features and ovarian function were investigated.
Methods and results
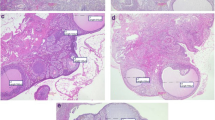
Streptozotocin-induced diabetes rats were treated with 12 and 24 mg/kg of eugenol for 4 weeks. The biochemical and histological assay was done to evaluate the effects of eugenol on ovary and pancreas function, liver injury, oxidative status, sex hormones, lipid profile, and mRNA levels of cyclooxygenase-2 (COX-2) and peroxisome proliferator-activated receptor alpha (PPAR-α) genes. Streptozotocin increased levels of serum glucose, total cholesterol, triglyceride, low-density lipoprotein, aspartate transaminase, alanine transaminase, alkaline phosphatase, malondialdehyde, pancreas necrosis and inflammation, COX-2 expression, ovarian cystic, and anovulation. It decreased the levels of insulin, high-density lipoprotein, Superoxide dismutase, estradiol, progesterone, testosterone, luteinizing hormone, follicle-stimulating hormone, and PPAR-α expression. Eugenol administration ameliorated diabetes features through the improvement of lipid profile, oxidative status, insulin and glucose levels, sex hormone levels, liver markers, COX-2 and PPAR-α expression, and pancreas histology. It had no effect on ovarian cystic and follicular development.
Conclusions
Therefore, eugenol may be useful for ameliorating some adverse features of diabetes and used as an adjunct treatment or protective agent accompany by other chemicals in diabetes patients.



Similar content being viewed by others
Data availability
All datasets generated during the present study are available from the corresponding author on request.
References
Brownlee M (2005) The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54:1615–1625. https://doi.org/10.2337/diabetes.54.6.1615
Erbas O, Pala HG, Pala EE, Oltulu F, Aktug H, Yavasoglu A, Taskiran D (2014) Ovarian failure in diabetic rat model: nuclear factor-kappaB, oxidative stress, and pentraxin-3. Taiwan J Obstet Gynecol 53:498–503. https://doi.org/10.1016/j.tjog.2013.11.008
Pala HG, Pala EE, Artunc Ulkumen B, Aktug H, Yavasoglu A, Korkmaz HA, Erbas O (2014) The protective effect of granulocyte colony-stimulating factor on endometrium and ovary in a rat model of diabetes mellitus. Gynecol Obstet Invest 78:94–100. https://doi.org/10.1159/000363239
Erbas O, Pala HG, Pala EE, Artunc Ulkumen B, Akman L, Akman T, Oltulu F, Aktug H, Yavasoglu A (2015) Therapeutic effect of sunitinib on diabetes mellitus related ovarian injury: an experimental rat model study. Gynecol Endocrinol 31:388–391. https://doi.org/10.3109/09513590.2015.1005593
Brand JS, Onland-Moret NC, Eijkemans MJ, Tjonneland A, Roswall N, Overvad K et al (2015) Diabetes and onset of natural menopause: results from the European prospective investigation into cancer and nutrition. Hum Reprod (Oxford, England) 30(6):1491–1498. https://doi.org/10.1093/humrep/dev054
Hasani-Ranjbar S, Larijani B (2014) Medicinal plants as potential new target drugs in endocrine disorders review article. Iran J Public Health 43:24–34
Shahwan M, Alhumaydhi F, Ashraf GM, Hasan PMZ, Shamsi A (2022) Role of polyphenols in combating Type 2 diabetes and insulin resistance. Int J Biol Macromol 206:567–579. https://doi.org/10.1016/j.ijbiomac.2022.03.004
Km A, Arefeen A, Shamsi A, Alhumaydhi FA, Naseem I (2021) Insight into the in vitro antiglycation and in vivo antidiabetic effects of thiamine: implications of vitamin B1 in controlling diabetes. ACS Omega 6(19):12605–12614. https://doi.org/10.1021/acsomega.1c00631
Lopes AA, Fonsecau FN, Rocha TM, Freitas LB, Araújo EVO, Wong DVT et al (2018) Eugenol as a promising molecule for the treatment of dermatitis: antioxidant and anti-inflammatory activities and its nanoformulation. Oxid Med Cell Longev 2018:8194849. https://doi.org/10.1155/2018/8194849
Manikandan P, Vinothini G, Vidya Priyadarsini R, Prathiba D, Nagini S (2011) Eugenol inhibits cell proliferation via NF-κB suppression in a rat model of gastric carcinogenesis induced by MNNG. Invest New Drugs 29(1):110–117. https://doi.org/10.1007/s10637-009-9345-2
Callejas NA, Casado M, Bosca L, Martín-Sanz P (1999) Requirement of nuclear factor kappa B for the constitutive expression of nitric oxide synthase-2 and cyclooxygenase- 2 in rat trophoblasts. J Cell Sci 112:3147–3155. https://doi.org/10.1242/jcs.112.18.3147
Marnett LJ (2000) Cyclooxygenase mechanisms. Curr Opin Chem Biol 4(5):545–552. https://doi.org/10.1016/s1367-5931(00)00130-7
Poynter ME, Daynes RA (1998) Peroxisome proliferator-activated receptor alpha activation modulates cellular redox status, represses nuclear factor-kappa B signaling, and reduces inflammatory cytokine production in aging. J Biol Chem 273:32833–32841. https://doi.org/10.1074/jbc.273.49.32833
Committee for the update of the guide for the care and use of laboratory animals (1996) Guide for the care and use of laboratory animals. National Academy Press, Washington
Kokabiyan Z, Yaghmaei P, Behnamedin Jameie S, Hajebrahimi Z (2022) Therapeutic effects of eugenol in polycystic ovarian rats induced by estradiol valerate: a histopathological and a biochemical study. International Journal of Fertility and Sterility. https://doi.org/10.22074/IJFS.2021.537724.1176
- Williams CJ, Erickson GF (2003) Morphology and physiology of the ovary. Endotext (Chapter 2). pp 51–58
Junod A, Lambert AE, Stauffacher W, Renold AE (1969) Diabetogenic action of streptozotocin: relationship of dose to metabolic response. J Clin Invest 48:2129–2139. https://doi.org/10.1172/JCI106180
Parhofer KG (2015) Interaction between glucose and lipid metabolism: more than diabetic dyslipidemia. Diabetes Metab J 39(5):353–362. https://doi.org/10.4093/dmj.2015.39.5.353
JrE W, Scism-Bacon JL, Glass LC (2006) Oxidative stress in type 2 diabetes: the role of fasting and postprandial glycaemia. Int J Clin Pract 60(3):308–314. https://doi.org/10.1111/j.1368-5031.2006.00825.x
Oguntibeju OO (2019) Type 2 diabetes mellitus, oxidative stress and inflammation: examining the links. Int J Physiol Pathophysiol Pharmacol 11(3):45–63
Gilani SJ, Bin-Jumah MN, Al-Abbasi FA, Nadeem MS, Afzal M, Sayyed N, Kazmi I (2021) Fustin ameliorates hyperglycemia in streptozotocin induced type-2 diabetes via modulating glutathione/superoxide dismutase/catalase expressions, suppress lipid peroxidation and regulates histopathological changes. Saudi J Biol Sci 28(12):6963–6971. https://doi.org/10.1016/j.sjbs.2021.07.070
Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, Nascimbeni F, Roverato A, Guaraldi G, Lonardo A (2016) Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol 31(5):936–944. https://doi.org/10.1111/jgh.13264
Islam S, Rahman S, Haque T, Sumon AH, Ahmed AM, Ali N (2020) Prevalence of elevated liver enzymes and its association with type 2 diabetes: a cross-sectional study in Bangladeshi adults. Endocrinol Diabetes Metab 3(2):e00116. https://doi.org/10.1002/edm2.116
Duckworth WC, Hamel FG, Peavy DE (1988) Hepatic metabolism of insulin. Am J Med 85(5):71–76. https://doi.org/10.1016/0002-9343(88)90399-3
Elkrief L, Rautou PE, Sarin S, Valla D, Paradis V, Moreau R (2016) Diabetes mellitus in patients with cirrhosis: clinical implications and management. Liver Int 36(7):936–948. https://doi.org/10.1111/liv.13115
Davila JA, Morgan RO, Shaib Y, McGlynn KA, El-Serag HB (2005) Diabetes increases the risk of hepatocellular carcinoma in the United States: a population based case control study. Gut 54:533–539. https://doi.org/10.1136/gut.2004.052167
Manna P, Das J, Ghosh J, Sil PC (2010) Contribution of type 1 diabetes to rat liver dysfunction and cellular damage via activation of NOS, PARP, IkappaBalpha/NF-kappaB, MAPKs, and mitochondria-dependent pathways: prophylactic role of arjunolic acid. Free Radic Biol Med 48:1465–1484. https://doi.org/10.1016/j.freeradbiomed.2010.02.025
Palsamy P, Sivakumar S, Subramanian S (2010) Resveratrol attenuates hyperglycemia-mediated oxidative stress, proinflammatory cytokines and protects hepatocytes ultrastructure in streptozotocin-nicotinamide-induced experimental diabetic rats. Chem Biol Interact 186:200–210. https://doi.org/10.1016/j.cbi.2010.03.028
Marchesini G, Brizi M, Bianchi G, Tomassetti S, Bugianesi E, Lenzi M, McCullough AJ, Natale S, Forlani G, Melchionda N (2001) Nonalcoholic fatty liver disease: a feature of the metabolic syndrome. Diabetes 50:1844–1850. https://doi.org/10.2337/diabetes.50.8.1844
Pelusi B, Gambineri A, Pasquali R (2004) Type 2 diabetes and the polycystic ovary syndrome. Minerva Ginecol 56(1):41–51
Pala HG, Pala EE, Ulkumen BA, Aktug H, Yavasoglu A, Korkmaz HA, Erbas O (2014) The protective effect of granulocyte colony-stimulating factor on endometrium and ovary in a rat model of diabetes mellitus. Gynecol Obstet Invest 78:94–100. https://doi.org/10.1159/000363239
Nayki U, Onk D, Balci G, Nayki C, Onk A, Gunay M (2016) The effects of diabetes mellitus on ovarian injury and reserve: an experimental study. Gynecol Obstet Invest 81:424–429. https://doi.org/10.1159/000442287
Oktay K, Newton H, Mullan J, Gosden RG (1998) Development of human primordial follicles to antral stages in SCID/hpg mice stimulated with follicle stimulating hormone. Hum Reprod 13(5):1133–1138. https://doi.org/10.1093/humrep/13.5.1133
Edson MA, Nagaraja AK, Matzuk MM (2009) The mammalian ovary from genesis to revelation. Endocr Rev 30:624–712. https://doi.org/10.1210/er.2009-0012
Wang Y, Wang Y (2022) Accelerated ovarian aging among type 2 diabetes patients and its association with adverse lipid profile. Front Endocrinol 13:780979. https://doi.org/10.3389/fendo.2022.780979
Wang X, Xian T, Jia X, Zhang L, Liu L, Man F et al (2017) A cross-sectional study on the associations of insulin resistance with sex hormone, abnormal lipid metabolism in T2DM and IGT patients. Medicine 96:e7378. https://doi.org/10.1097/MD.0000000000007378
Natah TM, Abdul- Adheem Wtwt M, Al-Saadi HK, Al-Saadi AH, Farhood HF (2013) Study the levels of adiponectin, FSH, LH and Sex hormones in Type 2 diabetes (NIDDM). J Biol Agric Healthcare 3(2):172–181
Blades RA, Bryant KR, Whitehead SA (1985) Feedback effects of steroids and gonadotrophin control in adult rats with streptozotocin-induced diabetes mellitus. Diabetes Tologia 28:348–354. https://doi.org/10.1007/BF00283142
Wang Q, Ferreira DLS, Nelson SM, Sattar N, Ala-Korpela M, Lawlor DA (2018) Metabolic characterization of menopause: cross-sectional and longitudinal evidence. BMC Med 16(1):17. https://doi.org/10.1186/s12916-018-1008-8
Miao C, Chen H, Li Y, Guo Y, Xu F, Chen Q, Zhang Y, Hu M, Chen G (2021) Curcumin and its analog alleviate diabetes-induced damages by regulating inflammation and oxidative stress in brain of diabetic rats. Diabetol Metab Syndr. https://doi.org/10.1186/s13098-021-00638-3
Hu Y, Chen Y, Ding L, He X, Takahashi Y, Gao Y, Shen W, Cheng R, Chen Q, Qi X, Boulton ME, Ma J (2013) Pathogenic role of diabetes-induced PPAR-α down-regulation in microvascular dysfunction. Proc Natl Acad Sci USA 110(38):15401–15406. https://doi.org/10.1073/pnas.1307211110
Srinivasan S, Sathish G, Jayanthi M, Muthukumaran J, Muruganathan U, Ramachandran V (2014) Ameliorating effect of eugenol on hyperglycemia by attenuating the key enzymes of glucose metabolism in streptozotocin induced diabetic rats. Mol Cell Biochem 385:159–168. https://doi.org/10.1007/s11010-013-1824-2
Jeong KJ, Kim DY, Quan HY, Jo HK, Kim GW, Chung SH (2014) Effects of eugenol on hepatic glucose production and AMPK signaling pathway in hepatocytes and C57BL/6J mice. Fitoterapia 93:150–162. https://doi.org/10.1016/j.fitote.2013.12.023
Al-Trad B, Alkhateeb H, Alsmadi W, Al- Zoubi M (2019) Eugenol ameliorates insulin resistance, oxidative stress and inflammation in high fat-diet/streptozotocin-induced diabetic rat. Life Sci 216:183–188. https://doi.org/10.1016/j.lfs.2018.11.034
Moghimian M, Aalami S, Abtahi-Evari SH, Soltani M (2018) Effect of Syzygium aromaticum (clove) extract on morphine withdrawal side effect in male reproductive system should be addressed. Physiol Pharmacol 22:109–117
Poli V, Challa C (2019) A comparative study of eugenol and Ocimum sanctum Linn. leaf extract on the antifertility effect in female albino rats. J Chin Med Assoc 82(3):231–234. https://doi.org/10.1097/JCMA.0000000000000034
Acknowledgements
Partial financial support was received from Islamic Azad University, Science and Research Branch, for conducting this study.
Funding
Partial financial support was received from Islamic Azad University, Science and Research Branch, for conducting this study.
Author information
Authors and Affiliations
Contributions
ZK, PY, SBJ, and ZH contributed to conception and designed the experiments. ZK performed experiments and collected data. ZK, PY, SBJ, and ZH discussed the results and strategy; PY, SBJ, and ZH supervised, directed, and managed the study. ZH was the major contributor in writing the manuscript. ZK, PY, SBJ, and ZH final approved of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to declare.
Ethical approval
The study was approved by the Animal Care and Use Committee of Islamic Azad University (Ethical permission number: IR.IAU.SRB.REC.1396.51).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kokabiyan, Z., Yaghmaei, P., Jameie, S.B. et al. Effect of eugenol on lipid profile, oxidative stress, sex hormone, liver injury, ovarian failure, and expression of COX-2 and PPAR-α genes in a rat model of diabetes. Mol Biol Rep 50, 3669–3679 (2023). https://doi.org/10.1007/s11033-022-08108-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-08108-3