Abstract
Aims
Although skin manifestations are common in diabetic patients, its characteristics are poorly identified. This study explored the differentiation process of keratinocytes in type 2 diabetes mellitus (T2DM) in vivo.
Methods
Back skin of T2DM model KKAy/TaJcl mice (KKAy) and C57BL/6JJcl mice (control) aged 8 and 12 weeks was used. The mRNA expression of differentiation markers of keratinocytes was measured by quantitative real-time polymerase chain reaction (qRT-PCR). The expression of each marker in situ was examined immunohistochemically.
Results
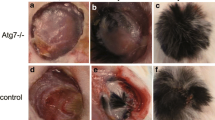
KKAy mice showed hyperglycemia versus control mice. The histological findings showed increased thickness and structural impairment of epidermal tissue in KKAy mice. The qRT-PCR revealed that the expression of integrin beta 1 and keratin 14 in KKAy and control mice was identical. However, the expression of involucrin at 8 weeks, keratin 10 at 12 weeks, and filaggrin and loricrin at 8 and 12 weeks was decreased in KKAy mice. Immunohistochemical findings showed that filaggrin was markedly decreased in KKAy mice, though Ki-67 remained unchanged.
Conclusion
The terminal differentiation process was impaired in the diabetic skin, while keratinocyte proliferation was preserved. Damaged terminal differentiation of keratinocytes may contribute to impairment of the skin barrier function in diabetic dermatoses.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
American Diabetes Association (2019) Cardiovascular disease and risk management: standards of medical care in diabetes-2019. Diabetes Care 42:S103–S123. https://doi.org/10.2337/dc19S010
American Diabetes Association (2019) Microvascular complications and foot care: standards of medical care in diabetes-2019. Diabetes Care 42:S124–S138. https://doi.org/10.2337/dc19-s011
Bertheim U, Engström-Laurent A, Hofer PÅ et al (2002) Loss of hyaluronan in the basement membrane zone of the skin correlates to the degree of stiff hands in diabetic patients. Acta Derm Venereol 82:329–334. https://doi.org/10.1080/000155502320624041
Brown SJ, McLean WHI (2012) One remarkable molecule: Filaggrin. J Invest Dermatol 132:751–762. https://doi.org/10.1038/jid.2011.393
Cai SCS, Chen H, Koh WP et al (2012) Filaggrin mutations are associated with recurrent skin infection in Singaporean Chinese patients with atopic dermatitis. Br J Dermatol 166:200–203. https://doi.org/10.1111/j.1365-2133.2011.10541.x
Candi E, Schmidt R, Melino G (2005) The cornified envelope: a model of cell death in the skin. Nat Rev Mol Cell Biol 6:328–340. https://doi.org/10.1038/nrm1619
Chatzigeorgiou A, Halapas A, Kalafatakis K, Kamper EF (2009) The use of animal models in the study of diabetes mellitus. In Vivo (Brooklyn) 23:245–258
Chen X, Lin W, Lu S et al (2010) Mechanistic study of endogenous skin lesions in diabetic rats. Exp Dermatol 19:1088–1095. https://doi.org/10.1111/j.1600-0625.2010.01137.x
Dash BC, Xu Z, Lin L et al (2018) Stem cells and engineered scaffolds for regenerative wound healing. Bioengineering 5:1–19. https://doi.org/10.3390/bioengineering5010023
Falanga V (2005) Wound healing and its impairment in the diabetic foot. Lancet 366:1736–1743. https://doi.org/10.1016/S0140-6736(05)67700-8
Ferringer T, MillerIII F (2002) Cutaneous manifestations of diabetes mellitus. Dermatol Clin 20:483–492. https://doi.org/10.1016/s0733-8635(02)00018-9
Gilhar A, Ullmann Y, Karry R et al (2004) Ageing in human epidermis: the role of apoptosis, Fas and telomerase. Br J Dermatol 150:56–63. https://doi.org/10.1111/j.1365-2133.2004.05715.x
Li C, Hou S, Liu S et al (2017) The albumin-exendin-4 recombinant protein E2HSA improves glycemic control and β-cell function in spontaneous diabetic KKAy mice. BMC Pharmacol Toxicol 18:1–9. https://doi.org/10.1186/s40360-017-0143-8
Lima AL, Illing T, Schliemann S, Elsner P (2017) Cutaneous manifestations of diabetes mellitus: a review. Am J Clin Dermatol 18:541–553. https://doi.org/10.1007/s40257-017-0275-z
Miyai M, Hamada M, Moriguchi T et al (2016) Transcription factor MafB coordinates epidermal keratinocyte differentiation. J Invest Dermatol 136:1848–1857. https://doi.org/10.1016/j.jid.2016.05.088
Muller LMAJ, Gorter KJ, Hak E et al (2005) Increased risk of common infections in patients with type 1 and type 2 diabetes mellitus. Clin Infect Dis 41:281–288. https://doi.org/10.1086/431587
Nakai K, Yoneda K, Ishihara Y et al (2011) Lipid peroxidation-induced VEGF expression in the skin of KKAy obese mice. Exp Dermatol 20:388–393. https://doi.org/10.1111/j.1600-0625.2010.01223.x
Neufang G, Furstenberger G, Heidt M et al (2001) Abnormal differentiation of epidermis in transgenic mice constitutively expressing cyclooxygenase-2 in skin. Proc Natl Acad Sci U S A 98:7629–7634. https://doi.org/10.1073/pnas.121574098
Okano J, Kojima H, Katagi M et al (2016) Hyperglycemia induces skin barrier dysfunctions with impairment of epidermal integrity in non-wounded skin of type 1 diabetic mice. PLoS ONE 11:1–22. https://doi.org/10.1371/journal.pone.0166215
Park HY, Kim JH, Jung M et al (2011) A long-standing hyperglycaemic condition impairs skin barrier by accelerating skin ageing process. Exp Dermatol 20:969–974. https://doi.org/10.1111/j.1600-0625.2011.01364.x
Rodgers KE, Ellefson DD, Espinoza T et al (2006) Expression of intracellular filament, collagen, and collagenase genes in diabetic and normal skin after injury. Wound Repair Regen 14:298–305. https://doi.org/10.1111/j.1743-6109.2006.00124.x
Sakai S, Endo Y, Ozawa N et al (2003) Characteristics of the epidermis and stratum corneum of hairless mice with experimentally induced diabetes mellitus. J Invest Dermatol 120:79–85. https://doi.org/10.1046/j.1523-1747.2003.12006.x
Sandilands A, Sutherland C, Irvine AD, McLean WHI (2009) Filaggrin in the frontline: role in skin barrier function and disease. J Cell Sci 122:1285–1294. https://doi.org/10.1242/jcs.033969
Schneider CA, Rasband WS, Eliceiri KW (2012) NIH Image to ImageJ: 25 years of image analysis. Nat Methods 9(7):671–675. https://doi.org/10.1038/nmeth.2089
Taylor KR, Costanzo AE, Jameson JM (2011) Dysfunctional γδ T cells contribute to impaired keratinocyte homeostasis in mouse models of obesity. J Invest Dermatol 131:2409–2418. https://doi.org/10.1038/jid.2011.241
Uchida K (2017) HNE as an inducer of COX-2. Free Radic Biol Med 111:169–172. https://doi.org/10.1016/j.freeradbiomed.2017.02.004
Yoneda K, Nakagawa T, Lawrence OT et al (2012) Interaction of the profilaggrin N-terminal domain with loricrin in human cultured keratinocytes and epidermis. J Invest Dermatol 132:1206–1214. https://doi.org/10.1038/jid.2011.460
Acknowledgements
We give special thanks to Sayaka Nomura for excellent technical assistance. This study was supported by grants-in-aid from Fujita Health University.
Funding
This study was supported by grants-in-aid from Fujita Health University to AS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
TY and SH are employees of Nippon Menard Cosmetics Co., Ltd. Other authors do not have any financial or non-financial conflict of interest.
Ethical approval
The mice were handled ethically according to the Regulations for the Management of Laboratory Animals at Fujita Health University. The experimental protocol for the ethical use of these animals was approved by the Animal Care and Use Committee at Fujita Health University (Permit No.: M0271).
Consent to participate
All the authors have made a significant contribution to this manuscript, have seen and approved the final manuscript.
Consent for publication
All the authors have agreed to its submission to the “Molecular Biology Reports”.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takayanagi, T., Hirai, H., Asada, Y. et al. Terminal differentiation of keratinocytes was damaged in type 2 diabetic mice. Mol Biol Rep 49, 5875–5882 (2022). https://doi.org/10.1007/s11033-022-07367-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07367-4