Abstract
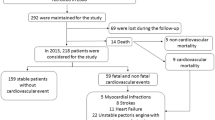
Calcific mitral valve stenosis (MVS) is a common disease characterized by extensive remodeling of the extracellular matrix via matrix metalloproteinases (MMPs). The mechanism of calcification due to extensive matrix remodeling remains unclear. In this study, we investigated the relationship between MMP-3, tissue inhibitors of metalloproteinases (TIMPs) as well as pro-inflammatory cytokines and the phenomenon of calcification in MVS. 212 patients having rheumatic mitral stenosis (RMS) and 155 healthy control subjects were recruited in the Cardiology Department of La Rabta Hospital University. Levels of MMP-3, TIMPs, IL-6 and TNF-α were measured by ELISA sandwich assay, hs-CRP was measured by immunoturbidimetry. Plasma levels of MMP-3, TIMP-1 and MMP-3/TIMP-2 ratio were lower only in RMS women in comparison to the control group. Calcification degree correlated positively with MMP-3 in women and men. In addition, calcification was correlated positively with MMP-3/TIMPs ratio in women patients. The inflammatory parameters were positively associated with extracellular matrix turnover biomarkers in men patients. In patients, the level of MMP-3 was increased in men and women with a calcification score ≥ 5. In addition, MMP-3 level predicted the occurrence of calcification. At ROC curves analysis, the cut-off MMP-3 level was in women was 9.21 ng/ml (sensitivity 51.1%, specificity 89.3%) and in men was 12.84 ng/ml (sensitivity 78.6%, specificity 77.8%). The high levels of MMP-3 and the biomarkers of inflammation contribute to valvular remodeling and calcification of the mitral valve.





Similar content being viewed by others
References
Narin N, Kütükçüler N, Ozyürek R, Bakiler AR, Parlar A, Arcasoy M (1995) Lymphocyte subsets and plasma IL-1 alpha, IL-2 and TNF-alpha concentrations in acute rheumatic fever and chronic rheumatic heart disease. Clin Immunol Immunopathol 77:172–176
Ben Ameur Y, Zairi I, Kamoun K, Ben sassi M, Longo S, Battikh K, Slimane ML (2010) Tricuspid dysfunction as a result of rheumatic disease. Tunis Med 88:820–828
Bilik MZ, Kaplan İ, Polat N, Akil MA, Akyüz A, Acet H, Yüksel M, İnci Ü, Kayan F, Toprak N (2016) Serum Levels of IL-17 and IL-23 in patients with rheumatic mitral stenosis. Medicine (Baltimore) 95:e3562
Alyan O, Metin F, Kacmaz F, Ozdemir O, Maden O, Topaloglu S, Demir AD, Karahan Z, Karadede A, Ilkay E (2009) High levels of high sensitivity C-reactive protein predict the progression of chronic rheumatic mitral stenosis. J Thromb Thrombolysis 28:63–69
Chang CJ, Hsu LA, Chiang CW, Ko YS, See LC, Shen YC, Ko YL, Kou CT, Lee YS, Pang JH (2003) Percutaneous transvenous mitral valvulotomy normalizes elevated circulating levels of tumor necrosis factor-alpha and interleukin-6 in mitral stenosis with heart failure. Am J Cardiol 91:1018–1020
Cagli KE, Aras D, Topaloglu S, Geyik B, Ayaz S, Cagirci G, Kisacik HL, Korkmaz S (2010) Plasma levels of tumor necrosis factor-alpha and its receptors in patients with mitral stenosis and sinus rhythm undergoing percutaneous balloon valvuloplasty. Heart Vessels 25:131–137
Edep ME, Shirani J, Wolf P, Brown DL (2000) Matrix metalloproteinase expression in nonrheumatic aortic stenosis. Cardiovasc Pathol 9:281–286
Soini Y, Satta J, Maatta M, Autio-Harmainen H (2001) Expression of MMP-2, MMP-9, MTI-MMP, TIMP-1, and TIMP-2 mRNA in valvular lesions of the heart. J Pathol 194:225–231
Nagase H, Woessner JF (1999) Matrix metalloproteinases. J Biol Chem 274:21491–21494
Fondard O, Detaint D, Iung B, Choqueux C, Adle-Biassette H, Jarraya M, Hvass U, Couetil JP, Henin D, Michel JB, Vahanian A, Jacob MP (2005) Extracellular matrix remodelling in human aortic valve disease: the role of matrix metalloproteinases and their tissue inhibitors. Eur Heart J 26:1333–1341
Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios IF (1988) Percutaneous balloon dilatation of the mitral valve: an analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J 60:299–308
Yetkin E, Erbay AR, Ileri M, Turhan H, Balci M, Cehreli S, Yetkin G, Demirkan D (2001) Levels of circulating adhesion molecules in rheumatic mitral stenosis. Am J Cardiol 88:1209–1211
Krasuski RA, Bush A, Kay JE, Mayes CE Jr, Wang A, Fleming J, Pierce C, Kisslo KB, Harrison JK, Bashore TM (2003) C-reactive protein elevation independently influences the procedural success of percutaneous balloon mitral valve commissurotomy. Am Heart J 146:1099–1104
Thubrikar MJ, Aouad J, Nolan SP (1986) Patterns of calcific deposits in operatively excised stenotic or purely regurgitant aortic valves and their relationship to mechanical stress. Am J Cardiol 58:304–308
Loof TG, Goldmann O, Gessner A, Herwald H, Medina E (2010) Aberrant inflammatory response to Streptococcus pyogenes in mice lacking myeloid differentiation factor 88. Am J Pathol 76:754–763
Irwin MW, Mak S, Mann DL, Qu R, Penninger JM, Yan A, Dawood F, Wen WH, Shou Z, Liu P (1999) Tissue expression and immunolocalization of tumor necrosis factor-alpha in postinfarction dysfunctional myocardium. Circulation 99:1492–1498
Baysal E, Burak C, Cay S, Aksu T, Altıntaş B, Yaylak B, Sevük U, Bilge Ö (2015) The neutrophil to lymphocyte ratio is associated with severity of rheumatic mitral valve stenosis. J Blood Med 6:151–156
Fukumoto Y, Shimokawa H, Ito A, Kadokami T, Yonemitsu Y, Aikawa M, Owada MK, Egashira K, Sueishi K, Nagai R, Yazaki Y, Takeshita A (1997) Inflammatory cytokines cause coronary arteriosclerosis like changes and alterations in the smooth-muscle phenotypes in pigs. J Cardiovasc Pharmacol 29:222–231
Galkina E, Ley K (2009) Immune and inflammatory mechanisms of atherosclerosis. Annu Rev Immunol 27:165–197
Diwan A, Dibbs Z, Nemoto S, DeFreitas G, Carabello BA, Sivasubramanian N, Wilson EM, Spinale FG, Mann DL (2004) Targeted overexpression of noncleavable and secreted forms of tumor necrosis factor provokes disparate cardiac phenotypes. Circulation 109:262–268
Fabunmi RP, Baker AH, Murray EJ, Booth RF, Newby AC (1996) Divergent regulation by growth factors and cytokines of 95 kDa and 72 kDa gelatinases and tissue inhibitors or metalloproteinases-1,-2, and-3 in rabbit aortic smooth muscle cells. Biochem J 315:335–342
Dreger SA, Taylor PM, Allen SP, Yacoub MH (2002) Profile and localization of matrix metalloproteinases (MMPs) and their tissue inhibitors (TIMPs) in human heart valves. J Heart Valve Dis 11: 875–880
Corcoran ML, Stetler-Stevenson WG (1995) Tissue inhibitor of metalloproteinase-2 stimulates fibroblast proliferation via a CAMP-dependent mechanism. J Biol Chem 270:13453–13459
Kim L, Kim DK, Yang WI, Shin DH, Jung IM, Park HK, Chang BC (2008) Overexpression of transforming growth factor-1 in the valvular fibrosis of chronic rheumatic heart disease. J Korean Med Sci 23:41–48
Kwak HJ, Park MJ, Cho H, Park CM, Moon SI, Lee HC, Park IC, Kim MS, Rhee CH, Hong SI (2006) Transforming growth factor-beta1 induces tissue inhibitor of metalloproteinase-1 expression via activation of extracellular signal-regulated kinase and Sp1 in human fibrosarcoma cells. Mol Cancer Res 4:209–220
O’Brien KD (2006) Pathogenesis of calcific aortic valve disease: a disease process comes of age (and a good deal more). Arterioscler Thromb Vasc Biol 26:1721–1728
Nadra I, Mason JC, Philippidis P, Florey O, Smythe CD, McCarthy GM, Landis RC, Haskard DO (2005) Proinflammatory activation of macrophages by basic calcium phosphate crystals via protein kinase C and MAP kinase pathways: a vicious cycle of inflammation and arterial calcification? Circ Res 96:1248–1256
Almholt K, Johnsen M (2003) Stromal cell involvement in cancer. Recent Results Cancer Res 162:31–42 24
Nagase H, Suzuki K, Morodomi T, Enghild JJ, Salvesen G (1992) Activation mechanisms of the precursors of matrix metalloproteinases 1, 2 and 3. Matrix Suppl 1:237–244
Eriksen HA, Satta J, Risteli J, Veijola M, Vare P, Soini Y (2006) Type I and type III collagen synthesis and composition in the valve matrix in aortic valve stenosis. Atherosclerosis 189:91–98
Newman KM, Jean-Claude J, Li H, Scholes JV, Ogata Y, Nagase H, Tilson MD (1994) Cellular localization of matrix metalloproteinases in the abdominal aortic aneurysm will. J Vaso Surg 20:814–820
Otto CM (2008) Calcific aortic stenosis—time to look more closely at the valve. N Engl J Med 359:1395–1398
Ogier C, Creidy R, Boucraut J, Soloway PD, Khrestchatisky M, Rivera S (2005) Astrocyte reactivity to Fas activation is attenuated in TIMP-1 deficient mice, an in vitro study. BMC Neurosci 29:68
Reynolds JL, Joannides AJ, Skepper JN, McNair R, Schurgers LJ, Proudfoot D, Jahnen-Dechent W, Weissberg PL, Shanahan CM (2004) Human vascular smooth muscle cells undergo vesicle- mediated calcification in response to changes in extracellular calcium and phosphate concentrations: a potential mechanism for accelerated vascular calcification in ESRD. J Am Soc Nephrol 15:2857–2867
Shanahan CM, Crouthamel MH, Kapustin A, Giachelli CM (2011) Arterial calcification in chronic kidney disease: key roles for calcium and phosphate. Circ Res 109:697–711
Canver CC, Gregory RD, Cooler SD, Voytovich MC (2000) Association of osteopontin with calcification in human mitral valves. J Cardiovasc Surg (Torino) 41(2):171–174
Acknowledgements
We thank all the personnel of Biochemistry and Cardiology departments for their collaboration throughout this study.
Funding
The study was supported by a grant from the “Ministry of High Education, Scientific Research and Technologies of Tunisia”.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Ethics Committee of Rabta Hospital and informed consent was obtained from all participants to this study. This work was carried out in accordance with the Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Rights and permissions
About this article
Cite this article
Aloui, S., Zidi, W., Ouali, S. et al. Association of matrix metalloproteinase 3 and endogenous inhibitors with inflammatory markers in mitral valve disease and calcification. Mol Biol Rep 45, 2135–2143 (2018). https://doi.org/10.1007/s11033-018-4372-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-018-4372-8