Abstract
Purpose
Previous research has systematically studied the effectiveness of Cognitive Behavioral Therapy (CBT)-based interventions in managing both mental and physical symptoms of chronic disease including depression, stress-related mental disorders (SMD), and chronic pain that are common causes of sick leave. However, a systematic review focusing on the effectiveness of CBT in facilitating RTW is lacking. This study compiles research on utilizing CBT-based interventions for helping employees on sick leave return to work.
Methods
Randomized controlled trials (RCT) published between 1 January 1990 and 27 June 2022 were searched in MEDLINE, EMBASE, The Cochrane Library, Scopus, PsycINFO, Web of Science, and PubMed. The primary outcome variables included a return to work (RTW) measure and sickness absences. The secondary outcomes include psychological conditions (mental illness, stress, anxiety, and depression) and physical condition (working ability, fatigue, and physical function).
Results
Thirty-four RCTs were included in the analysis. Fifteen RCTs with 1727 participants reported on sick leave. Results showed that participants who completed CBT intervention had reduced sick leave in days (mean reduction − 3.654; 95%CI − 5.253, − 2.046; p < 0.001) compared to the control group. Sixteen papers with 2298 participants reported that the intervention group RTW 1.5 days earlier (95%CI 1.019, 1.722; p < 0.05). CBT-based interventions were effective in managing fatigue, mental illness, and depression, and improving physical function while it showed no effects in managing stress, anxiety and working ability.
Conclusions
The findings indicate that CBT-based interventions are effective in reducing the length of sick leave and facilitating the RTW of employees in the intervention group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Sickness Absence Dictionary defines sick leave as contract employees or self-employees taking days off from their regular work to deal with their personal illness [1]; it is granted based on the different policies in each country. Long-term sick leave is defined as taking a long period of consecutive days off, and the number of days used for long-term sick leave is directly associated with the social insurance programmes in different nations [1]. In most countries including Sweden, Australia and Finland, long-term sick leave is defined as taking more than 60 consecutive days or 3 months off from work in 12 months [1].
Numerous reasons exist for sick leave beyond physical or mental medical conditions [1, 2]. Sick leave can be caused by factors including poor working environment and poor relationships between colleagues and supervisors at work, resulting in significantly economic loss. Among the 15 member states of the European Union in 2000, an average of 14.5% of people had taken at least 1 day of sick leave [3]. In Denmark, 3.6% of all work hours are lost due to sick leave [4]. Sick leave has resulted in a loss of 175 million working days in Britain in the year 2006 which is the equivalent of seven days for each working person [5], and it significantly contributes to low productivity, with every 1% increase in the rate of sickness leave resulting in a productivity loss of 0.66% [6].
Mental health disorders including depression and SMD are the leading causes of sick leave. In Sweden, mental health disorders accounted for 53% of sick leave causes in women and 42% of sick leave causes in men in the year 2019 [7]. The clinical features of depression (e.g. insomnia, anhedonia, feeling of worthlessness, fatigue, diminished concentration), and the poor psychological and behavioural characteristics present among SMD patients can contribute to poor working ability leading to sick leave [8]. The economic cost of mental health disorders in Europe is estimated to be $610 billion per year, with the majority arising from reduced employment and lost productivity [9]. Chronic musculoskeletal (MSK) pain is the second most common cause of sick leave [10]. Chronic MSK pain is defined in this study as pain that persists for more than three months and may occur anywhere in the body. It can be related to injuries to muscles, bones, ligaments, tendons, and/or nerves [11]. As an example, the productivity loss due to chronic lower back pain alone in the United States was up to 28 billion USD [12]. Chronic MSK pain is often related to muscle overuse, repetitive muscle inflammation from muscle strain, and heavy weight lifting [13]. Chronic MSK pain is relevant to all types of work, such as office work and building construction.
RTW interventions have been trialled to help employees on sick leave restore their physical and mental capacities and to avoid the recurrence of symptoms. Studies show that the symptomatic treatment of common mental disorders and MSK pain alone may be insufficient to reduce sick absence partly due to unadjusted working habits after RTW [14]. Recent studies have trialled various forms of cognitive behavioural therapy (CBT) to help employees return to work and adjust to working habits after RTW [15, 16]. There is strong evidence supporting the benefits of CBT as a treatment for a wide range of psychological conditions, such as anxiety and depression, which may help employees with sick leave to return to work early [17,18,19,20,21]. CBT works by training people to be aware of their thoughts and behaviours and to replace negative instinctive reactions to various daily life scenarios with more positive outlooks thereby allowing them to modulate their symptoms [22, 23]. The behavioural component employs various techniques, including reinforcement, classes and shaping, to improve employees’ functional status and help them develop positive relationships with work [24, 25]. The cognitive component helps individuals to identify and link their obstructive thoughts, problematic behaviours, and negative feelings together [23].
CBT is problem-oriented and focuses on improving the patient’s current cognition and thought processes [25]. Therefore, CBT is a useful intervention model for the management of chronic problems where there is no immediate cure [25]. Thus, CBT is a strong candidate when considering treatment options for people taking long-term sick leave because it can help manage the behaviours and thought processes underlying their reasons for taking the sick leave in the first place. Although CBT is primarily focused on the treatment of mental illnesses, applying the principles of CBT with a focus on positive reinforcement and behavioural changes may help improve resilience and the ability to cope with the pain, thereby increasing work satisfaction and reducing the mental burden of MSK-based reasons for long-term sick leave [26]. CBT is already the first-line treatment for a variety of psychological illnesses and can be utilised to great effect in the management of stress and burnout in the workplace [17, 27]. Thoughts and behaviours in the workplace contribute greatly to both the development and alleviation of stress, which can then lead to burnout [28]. CBT could be utilised to great effect in the control of these factors to help employees return to work and increase productivity.
The effectiveness of CBT in reducing the duration of sick leave has been investigated in various RCTs across different countries, albeit with inconsistent results. Previous RCTs have shown that CBT-based treatment can significantly reduce the length of MSK-related sick leaves and is effective in improving the physical and mental health of employees [20, 21, 29]. Other similar interventions have also been shown to have a significant effect on helping employees return to work after taking sick leaves due to mental conditions including stress and burnout [30, 31]. However, results from various studies are inconsistent with some RCTs showing that although CBT-based treatment led to improved outcomes compared to no treatment, there was no significant difference between the proposed treatment and care as usual [32,33,34,35]. In summary, low sample size, homogeneity of the sample population, and the differences in control groups may account for these inconsistencies among different studies. Although there are systematic reviews and meta-analyses investigating interventions supporting RTW among workers with different reasons for sick leave, a systematic review focusing on the effectiveness of CBT in facilitating RTW is lacking [36,37,38,39]. To fill in this research gap, this study aimed to conduct a systematic review and meta-analysis of RCTs to evaluate the effectiveness of CBT in helping employees with sick leave RTW and in reducing stress, anxiety, depression, fatigue, mental illness, and improving working ability and physical health.
Methodology
Literature Search
The study was registered at PROSPERO (Registration Number: CRD42021260666). The search was conducted in the following electronic databases: MEDLINE, EMBASE, The Cochrane Library (Cochrane Database of Systematic Reviews, Cochrane Central Register of Controlled Trials (CENTRAL), Cochrane Methodology Register), Scopus, PsycINFO, Web of Science, PubMed, and Chinese Zhi Wang. Then, the keywords were put in the Thesis and Dissertation to include the unpublished articles. Searches were confined to literature published from January 1, 1990 to June 27th 2022 by using the following key terms: (“ Employee OR employees OR worker OR workers OR staff OR personnel’ [All fields]) AND (“ Sick OR sick leave OR ill OR illness” [All fields]) AND (“ Return to work OR go back to work OR resume work OR part time OR full time OR casual OR temporary work” [All fields]) AND (“ Cognitive behaviour therapy OR CBT OR cognitive behaviour therapy” [All fields]) AND (“ Randomised controlled trials Or Randomised controlled trial OR Randomized controlled trials OR Randomized controlled trial OR RCT” [All fields].
Inclusion Criteria
The inclusion criteria for this systematic review and meta-analysis was developed based on the PICO approach [40]:
Participants: Participants were employees at a workplace and on sick leave or leave due to a workplace incident. All participants must be 18 years or above.
Intervention: The study design was RCT or RCT equivalent studies. The intervention must be based on CBT with both cognitive and behavioural therapy as compulsory components in combination with common CBT techniques including homework assignment, stress management, relapsing preventions, problem-solving strategies, and rehabilitation. The intervention can be a single CBT or CBT-based multiple programme intervention in combination with other managements including motivational interviews, and graded activity. CBT can be delivered individually or in groups in the form of face-to-face or online (online modules are included).
Control: Control group can be anything including non-CBT interventions such as care-as-usual, no treatment, graded activity, Qigong that refers to a traditional Chinese mind-body exercise to improve health by relieving stress, anxiety and improving physical health, work rehabilitation, and conventional care.
Outcome: The study outcome includes whether the employee return to work or not, and the number of days for sick leave. The secondary outcomes included stress, fatigue, mental illness, anxiety, depression, working ability and physical function.
The exclusion criteria for this review were:
Participants: People who were below the age of 18 OR participants and not employees or the employees were not on sick leave
Intervention: The intervention is not based on CBT.
Control: Papers will be excluded if there is no control group.
Outcome: The outcome is not whether the employee returned to work or sick leave.
Data Extraction
The titles and abstracts of non-duplicated papers that were selected during the search were independently screened by two authors to identify papers that potentially met the inclusion criteria. If there was any disagreement about the inclusion or exclusion of a paper between two authors, the paper was evaluated by a third author for a conclusive decision. Full texts of eligible studies that met the requirement of qualitative assessment were assessed for data extraction. Data extraction for study characteristics included country, publication year, study design (single-blinded, double-blinded, no blinded RCT), study population (proportion intervention and control employee participants), participant demographics (including age, the ratio of gender per group, number of employees with RTW in the post-intervention phase), type of interventions (characterization of the intervention group in addition to the control group), control group activity, duration of intervention, primary outcomes that were the number of people RTW and sick leave, secondary outcomes including psychological condition (mental illness, stress, anxiety, and depression) and physical condition (working ability, fatigue, and physical function), and quality assessment score. Missing data were requested from the corresponding author of the study. If sickness absences were measured in weeks, the number of days for sickness absences was calculated by multiplying the number of weeks by 5. The subgroup analysis included the delivery method of CBT (face to face vs. remote), an education level (< 9 years vs. 9–12 years vs. > 12 years), reasons for sick leave (MSK vs. psychological vs. others), combined with mood symptoms (no vs. yes), type of intervention (single CBT vs. combined CBT), duration of sessions (< 90 min vs. ≥ 90 min), treatment duration (< 16 weeks vs. ≥ 16 weeks), treatment form (individual session vs. group session vs. mixed), study design (non-RCT vs. RCT), and the components of CBT including (i) rehabilitation service utilization (no vs. yes), (ii) support from supervisor (no vs. yes), (iii) mood management (no vs. yes), (iv) stress management (no vs. yes), (v) homework assignment (no vs. yes), (vi) psychological education (no vs. yes), (vii) relapse prevention (no vs. yes), (viii) interpersonal strategies (no vs. yes).
Quality Assessment
Papers that met inclusion criteria were independently screened for risk by two authors. PEDro method was used for evaluating the risk assessment that was evidenced as a valid measure of the methodological quality of clinical trials [40]. PEDro scale consists of 10 ‘yes’ or ‘no’ questions. Every ‘yes’ to the question is worth 1 point. It categorizes the quality of papers into three-level: high quality with 8 points or above, moderate quality with 4–7 points, and low quality that has less than three points [41]. The criteria for the application of PEDro scale include random allocation of subjects, concealed randomization, the similarity of baseline information between groups, blinding to subjects, assessors, and researchers, attrition rate, maintenance of group allocations, use of intention-to-treat analysis, use of variability measures, and use of between-group comparison methods [40]. Low-quality papers (3 points) were automatically excluded.
Statistical Analysis
Outcome data extraction was conducted and extracted data contained information on data variable type, mean scores with SDs, and confidence interval. The primary outcome included an RTW measure (yes/no, categorical variable) and sickness absences (continuous variable). The secondary outcomes include psychological conditions (mental illness, stress, anxiety, and depression) and physical condition (working ability, fatigue, and physical function). RTW variable was presented in numbers and sample size per group. Continuous variables such as sickness absences, listed psychological and physical conditions were presented as mean and standard deviation.
The effect size for all outcome variables was measured by the random-effects model. A p-value of < 0.05 was considered statistically significant. Publication bias was assessed by Egger regression analysis. A P-value of less than 0.05 would suggest a publication bias, and further sensitivity analysis will be conducted to validate it.
I2 describing the variations across the study was calculated for the assessment of heterogeneity. An I2 > 50% meant a significant effect of CBT on the outcome variables. In such conditions, further subgroup analyses were conducted for outcome variables including sick leave and depression. The subgroup analysis was conducted in relation to variables including delivery method of CBT (face to face vs. remote), an education level (< 9 years vs. 9–12 years vs. > 12 years), reasons for sick leave (MSK vs. psychological vs. others), combined with mood symptoms (no vs. yes), type of intervention (single CBT vs. combined CBT), duration of sessions (< 90 min vs. ≥ 90 min), treatment duration (< 16 weeks vs. ≥ 16 weeks), treatment form (individual session vs. group session vs. mixed), study design (non-RCT vs. RCT), and the components of CBT including (i) rehabilitation service utilization (no vs. yes), (ii) support from supervisor (no vs. yes), (iii) mood management (no vs. yes), (iv) stress management (no vs. yes), (v) homework assignment (no vs. yes), (vi) psychological education (no vs. yes), (vii) relapse prevention (no vs. yes), (viii) interpersonal strategies (no vs. yes).
Results
Search Results
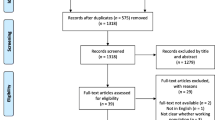
As seen in Fig. 1, 548 articles were identified by two assessors through the initial search and 43 articles were removed due to duplication. 471 articles were further excluded by screening abstracts and titles. The full text was retrieved for the remaining 34 articles, and they were assessed according to the inclusion and exclusion criteria. In the end, 30 RCTs or RCT equivalent studies were included in this systematic review and meta-analysis.
Characteristics of Included Studies
Individual analyses were performed for three studies that investigated the effectiveness of both individual CBTs and combined CBTs, and one study that investigated the effect of CBT on both individuals and work groups. Combined CBT refers to multimodal interventions that utilised CBT with a work-focused purpose in combination with other strategies including motivational interviews, functional capacity training modules and workplace-based interventions including occupational adjustment. Therefore, there were 34 effective comparing groups with a total of 6065 participants included. These studies were primarily done in developed countries including USA [42], Germany [43,44,45,46], Netherland [33, 34, 47,48,49,50,51], Denmark [30, 52, 53], Sweden [16, 19, 21, 31, 32, 54,55,56,57,58,59], Norway [35, 60], Canada [61, 62], Spain [20]. Out of the 34 studies, 21 studies were designed for patients on sick leave due to psychological reasons [16, 30,31,32,33,34, 42, 44, 45, 48, 50,51,52, 54, 55, 58,59,60], 12 studies for patients on sick leave due to MSK issues [19,20,21, 35, 43, 46, 47, 49, 53, 56, 57, 61, 62] and 1 study for patients due to other reasons such as unexplained fatigue [47]. 16 trials used CBT combine with other treatments/therapies [16, 30, 31, 35, 42, 43, 46, 49,50,51, 54, 55, 58,59,60,61,62] including motivational interviews, problem solving skills, education, and care as usual, while 18 trials used only CBT as an intervention [16, 19, 20, 32,33,34, 44, 45, 47, 48, 52, 53, 56,57,58] (Table1). 20 trials conducted individual based-CBT interventions [16, 20, 32,33,34, 42, 44, 45, 47, 50,51,52, 54, 58,59,60,61,62], 11 trials conducted group based-CBT interventions [19, 21, 30, 31, 33, 43, 48, 53, 55,56,57], and 3 trials delivered CBT through a mixed mode [35, 46, 49] with both individual and group sessions. Most CBTs were delivered face to face while 5 trials were delivered remotely [20, 32, 42, 51, 54] through strategies including online learning modules (Table1). 21 trials used usual care as control [16, 19,20,21, 32, 33, 35, 42, 45, 47, 48, 50, 51, 54,55,56, 58,59,60,61,62], 8 trials used no treatment [19, 30, 34, 44, 52, 53, 56, 57] and 5 used non-CBT intervention (conventional care [43, 46], Qigong [31], work rehabilitation [46], and graded activity [49]) (Table1).
Post- to Pre-treatment Effects of CBT-Based Intervention
Effects on Sick Leave in Reduced Days and People RTW in Number
Out of the 34 papers, 15 papers with 1727 participants investigated on reduction of sick leave, and the results showed that CBT-based intervention was more effective than the control condition in reducing sick leave in days with a mean reduction of − 3.649 (95% Cl − 5.253 to − 2.046; p < 0.001) and a moderate effect size of − 0.395 (95% Cl − 0.670 to − 0.120; p < 0.01). The heterogeneity of these studies was statistically significant (I2 = 92.991; p < 0.001) (Table2). Sixteen papers with 2298 participants reported on the number of people RTW. The results showed that CBT-based intervention was more effective than the control condition in facilitating people to RTW with a mean difference of 1.5 (95% Cl 1.019 to 1.722; p < 0.05). The heterogeneity of these studies was not statistically significant (I2 = 32.998, p > 0.05). The forest plots of the effect on sick leave in reduced days and numbers of people RTW are presented in Fig. 2a.
The subgroup analyses were performed to assess the effect of CBT on sick leave in reduced days. Table 3 suggested that CBT based intervention in the studies with the following characteristics had a significant effect on sick leave in reduced day: treatment delivered face-to-face (MD − 8.673, 95% CI − 15.550, − 1.797, p < 0.05), participants with higher education levels (> 12 years) (effect size − 0.923, 95% CI − 1.206, − 0.639, p < 0.001), utilization of rehabilitation services (MD − 10.095, 95% CI − 11.902, − 8.288, p < 0.001), stress management (MD − 3.498, 95% CI − 5.110, − 1.886, p < 0.001), and long treatment course (≥ 16 weeks) (MD 2.747, 95% CI − 4.169, − 1.326, p < 0.001). CBT-based intervention showed a better effect on sick leave in studies that included homework assignment (MD − 2.615, 95% CI − 4.017, − 1.213, p < 0.001), mood management (effect size − 0.926, 95% CI − 1.209, − 0.643), p < 0.001), long duration of sessions (≥ 90 min) (MD − 9.951, 95% CI − 17.633, − 2.269, p < 0.05), combined CBT (MD − 14.785, 95% CI − 22.898, − 6.672, p < 0.001) and those delivered in group sessions (effect size − 9.476, 95% CI − 11.247, − 7.704, p < 0.001).
Effect on Psychological Condition (Mental Illness, Stress, Anxiety, and Depression)
12 studies with a total sample of 1233 and 2078 participants were included in the random-effects meta-analysis for stress and anxiety respectively, while 5 studies with a total sample size of 1301 were analysed for mental illness. The result in Table 2 showed no significant difference between CBT-based intervention and control conditions for anxiety (MD − 0.380, 95% CI − 0.816, 0.057, p > 0.05). CBT-based interventions were more effective in managing stress in contrast to the control condition with a small effect size of − 0.123 (95% Cl − 0.243, − 0.003, p < 0.05). CBT-based interventions were also more effective in managing mental illness compared to the control condition with mean reduction of − 0.810 (95% Cl − 1.561, − 0.060; p < 0.05), with a small effect size of − 0.196 (95% Cl − 0.308, − 0.083, p < 0.01).
The effect on depression was analysed in 15 studies that had a total sample of 2870 participants. CBT-based interventions were more effective for depression management compared to the control condition with mean reduction of depression of -0.965 (95% Cl − 1.745, − 0.186, p < 0.05), and a small effect size of − 0.176 (95% Cl − 0.322, − 0.031, p < 0.05) (Table 2). The heterogeneity for these studies was statistically significant (I2 = 61.490; p < 0.01) (Table 2). Subgroup analyses also showed that CBT-based interventions with the following characteristics had a significant effect on depression symptoms (Table 4): participants with higher education levels (> 12 years) (MD − 0.349, 95% CI − 0.667, − 0.031, p < 0.05), rehabilitation services (MD − 0.132, 95% CI − 0.252, − 0.012, p < 0.05), stress management (MD − 0.222, 95% CI − 0.424, − 0.021, p < 0.05), homework assignments (MD − 0.382, 95% CI − 0.626, − 0.138, p < 0.01), psychological education (MD − 0.209, 95% CI − 0.384, − 0.034, p < 0.05), interpersonal skills (MD − 0.110, 95% CI − 0.213, − 0.007, p < 0.05), long treatment course (≥ 16 weeks) (MD − 0.210, 95% CI − 0.409, − 0.012, p < 0.05) and long duration of sessions (≥ 90 min) (MD − 0.153, CI 95% − 0.298, − 0.008, p < 0.05), treatment delivered in group sessions (MD − 0.197, 95% CI − 0.383, − 0.010, p < 0.05) in forms of combined CBT (effect size − 0.164, 95% CI − 0.267, − 0.061, p < 0.01). CBT-based interventions showed a better effect on depression when treatment was delivered remotely (MD − 0.892, 95% CI − 1.228, 0.556, p < 0.001). The forest plots of the effect on the psychological condition are presented in Fig. 2b.
Effect on Physical Condition (Working Ability, Fatigue, and Physical Function)
8 studies with 1112 participants were analysed for working ability. The result in Table 2 showed no significant difference between CBT-based intervention and control conditions for working ability (MD 0.164, 95% Cl − 0.221, 0.549, p > 0.05). 5 studies with 390 participants investigated fatigue while 3 studies with 364 participants investigated physical functioning. CBT-based interventions were more effective in managing fatigue and improving physical functioning when compared to the control condition with mean difference of − 4.271 (95% Cl − 7.795, − 0.747, p < 0.05) and 3.076 (95% Cl 0.218, 5.934, p < 0.05), respectively, with moderate effect sizes of − 0.376 (95% Cl − 1.058, 0.306, p < 0.05) for fatigue and 0.223 (95% Cl 0.016, 0.430, p < 0.05) for physical functioning. Forest plots of the effects of CBT-based intervention on the physical condition are presented in Fig. 2C.
Publication bias
The Egger test in Table 5 suggested publication bias is minimal for all outcome variables (p > 0.05). The overall results for all outcome variables were not significantly altered when any one study is removed, indicating that the results were not overly distorted by any paper.
Discussion
This meta-analysis aimed to determine whether CBT-based interventions are effective to increase the number of people who return to work, reduce sick leave days, and improve mood symptoms, working ability, and physical function in employees with sick leave. Our results confirm that CBT-based intervention significantly increased the number of people who RTW and improved physical function. The intervention group also had a reduced amount of sick leave time (days) as well as reduced mental illness, depression, stress, and fatigue symptoms. While previous studies mainly focused on the ability of CBT to treat certain conditions, this is one of the first meta-analyses to comprehensively examine the effectiveness that CBT has on multiple outcomes.
Our study found that CBT-based interventions significantly increased the number of participants who RTW and reduced the number of days spent on sick leave. Previous studies have also showcased the ability of CBT to facilitate RTW [20]. The improvements in sick leave duration and willingness to RTW seen in this study may be due to the enhanced mental health of participants. Our results indicate that individuals who have undergone CBT experienced decreased mental illness, depression, stress, and fatigue symptoms, which is consistent with another study conducted by Salomonsson et al. investigating the effects of CBT for patients on sick leave with common mental health disorders [63]. Several reasons exist as to why improving mental health with CBT leads to greater sick leave reduction. Firstly, the medical treatment of MSK pain and mental health disorders alone may be insufficient in reducing sick leave. To address this, CBT provides psychological-based treatment and work attitude adjustment in conjunction with the management of the physical causes of work absence [16]. CBT improves patient cognition and thought processes that underly their reasons for taking sick leave, allowing patients to cope with their circumstances [17]. This is supported by our study’s subgroup analysis findings that CBT was more effective in reducing sick leave when stress management was incorporated in the CBT process. By instilling positive attitudes towards work and reducing stress and burnout, individuals may be more eager to RTW after CBT, thus reducing sick leave duration. Equally, other studies have shown that CBT is effective in reducing stress and insomnia which can enhance energy levels and willingness to RTW [18]. CBT leads to a reduction in psychiatric symptoms and improvements in patient satisfaction [63]. Overall, the improvement of mental health due to CBT may lead to reduced sick leave duration since individuals are more likely to RTW faster if they are less stressed and fatigued.
Apart from stress management, our subgroup analyses further identified several factors that contributed to the effectiveness of CBT on reduced sick leave in days. Combined CBT that is work focused intervention in conjunction with other rehabilitations significantly reduced sick leave duration in comparison to CBT-only interventions, allowing employees to RTW faster. We speculate that despite CBT managing employees’ psychosocial complaints, it might not be directly correlated to work resumption as their working ability and subjective health were unaddressed. Meanwhile, combined CBT that utilised various intervention components not only focused on work problem solving bur also facilitated solving other health problems. The important components of combined CBT evidenced in our subgroup analysis were homework assignments and rehabilitation services. The importance of homework assignments could be explained by their effectiveness in managing symptoms between sessions and adapting to new skills. We speculate that since CBT was generally not a therapy delivered daily, homework assignments allowed individuals to practice their coping strategies between sessions and maintain their skills when they resumed to workplace. Our finding was consistent with a study conducted by Van der Klink et al. who investigated the effectiveness of CBT combined with stress management and homework assignment on sick leave in employees with mental health disorders [50]. Rehabilitation services could provide work-based education and physical training to allow employees to be mentally and physically prepared for RTW [35]. An example of rehabilitation would be low-intensity exercises for MSK-related injuries that allow employees to gradually regain their functional abilities with a reduced chance of further injury. Another example of rehabilitation services is the use of psychosocial strategies including relapsing preventions to support participants at the workplace [60]. The finding suggested that the work-focused components such as homework assignments and rehabilitation services focused on solving health problems that are frequently encountered at work, consequently allowing employees to restore self-esteem. Conversely, our subgroup analysis has also shown that there was no significant difference in reduced sick leave in days with the use of workplace-focused components including supervisor support and relapse prevention strategies. Firstly, we speculate that although supervisor support may provide appropriate workplace adjustments, employees may be reluctant to express their needs at the workplace due to self-stigma. This is consistent with a study conducted by Dalgaard et al. which demonstrated that only 10% of the participants wanted their supervisors and psychologists to participate in their direct workplace interventions [52]. Secondly, relapse prevention may reduce the frequency and duration of relapse episodes by developing positive attitudes and strategies when facing triggers in the workplace. However, its effectiveness may not be achieved if performed outside the workplace since there is a lack of context during the intervention. We speculate that the effectiveness of relapse prevention may be limited if it was delivered while employees were still on sick leave. Overall, it can be concluded that the effectiveness of CBT in facilitating RTW may be multifactorial and requires both workplace and health interventions. More research investigating the work-focused components of combined CBTs including relapse prevention and supervisor support would be required to evaluate their effectiveness.
An Update of the Recent Studies
A recent RCT conducted by Hoff et al. compared an integrated intervention (INT) with a non-integrated group and a care-as-usual (CAU) group [64]. The non-integrated method was referred to as Mental Healthcare (MHC) which was based on the conventional CBT while the INT integrated ‘healthcare and vocational rehabilitation’. The study suggested no difference in effect on the time to RTW between the MHC and the CAU group (98.3% Cl 0.88, 1.55, p = 0.196). This result is opposed to our findings that CBT-based interventions significantly reduced the number of days spent on sick leave. The insignificant difference in time to RTW in this RCT could be explained by many factors. Firstly, the staff only received a short period of training for standard CBT that may comprise the quality of treatment delivered to patients. Secondly, the insignificance may be related to the poor standard of the sessions since many studies have evidenced poor healthcare in primary care [65, 66]. Lastly, this RCT utilised standard CBT instead of work-focused CBT which has been found to be more effectively in facilitating RTW based on our findings. This RCT also found that the time to RTW in the MHC group was 0.79 times that in the INT group (98.3% Cl 0.6, 1.05, p = 0.044), suggesting an integrated intervention would be more effectively than a single intervention. Similarly, our review also suggested that combined CBT which is work focused intervention in conjunction with other rehabilitations significantly reduced sick leave duration in comparison to CBT-only interventions, allowing employees to RTW faster.
Additionally, certain forms of CBT-based intervention utilised in this study allowed sick leave days to be further reduced. These include ≥ 90 min session duration (where participants had 9.95 days of reduced sick leave on average compared to 0.7 days for sessions < 90 min) and ≥ 16 weeks treatment length, indicating that increasing intervention exposure time improves outcomes. However, this will require further research as there is currently a lack of studies that investigate the relationship between CBT duration and sick leave reduction. We also found that group-delivered CBT was more effective than individualised CBT in reducing sick days and depression. This could be explained by group CBT emphasising the influence of social factors on individual behaviour. Participants can access more opportunities for positive peer modelling and the normalisation of their symptoms through communication with group members [67]. CBT also reduced sick leave duration more when performed face-to-face compared to remote delivery (including via phone, internet, and online modules). We speculate that this may be due to the increased engagement and accountability of patients in face-to-face settings. Over the last two decades, hundreds of RCTs have showcased that internet-based CBT produces promising outcomes. However, the control groups were usually care-as-usual, preventing comparisons between different CBT delivery methods [68]. To address this, a 2018 meta-analysis compared the effectiveness of internet-based and face-to-face CBT for psychiatric and somatic disorders in 1418 participants from 20 included articles [68]. Overall effects were found to be equivalent between the two delivery methods [68]. Equally, a 2020 RCT found that internet-based CBT was non-inferior and cheaper than face-to-face CBT for anxiety improvement [69]. More research with larger sample sizes is required to establish further comparisons.
Several other key issues exist regarding the effectiveness of CBT. Our study found that working ability was not significantly improved by CBT despite reduced sick leave days, which increases the concern of presenteeism. Although individuals returned to work earlier, they may have had ongoing issues that prevented them from working at their full potential. Another problem is that sick leave was only reduced by 3.65 days on average, which needs to be considered in the context of the time and cost of implementing CBT [70].
Overall, while the findings of our study support the benefits of utilising CBT to improve mental health and enable earlier RTW, more research is required to determine the optimal timing and cost-effectiveness of CBT implementation.
Limitations, Strengths, and Implications
Despite the variety of papers considered in this study, there are several limitations. Firstly, there was high heterogeneity among the RCTs used which can be due to the fact that many of the outcomes being studied were measured on different scales by the authors of the RCTs that comprise the dataset for this study. Secondly, the outcome variables measured at different ending points may alter the validity of the result. Although we aimed to include the outcomes at the end point of the intervention, some outcomes were only measured a few months after the post-intervention which may alter the effectiveness of the intervention. In addition, although most RCTs included in this systematic review and meta-analysis were based on a CBT manual, the environmental settings and the focus of different CBT components varied. Therefore, the overall effectiveness of CBT on RTW would depend on the skills of practitioners, the dedication of patients to change, and whether it is also work-focused rather than only health-focused.
This study provides promising results for the utilisation of CBT in those unable to work due to MSK and psychiatric illnesses. By reducing sick leave, individuals can RTW sooner and increase the productivity of their workplaces [71]. The finding of decreased mental illness, depression, stress, and fatigue after CBT treatment has significant implications for the health of workers and the prevention of burnout [72]. More research is needed to assess the effectiveness of increasing CBT duration, comparing face-to-face and remote delivery methods, and whether CBT is better as a preventative measure used in the early stages of illness before sick leave commencement [73].
Conclusion
Our findings demonstrate that there was a significant reduction in the length of sick leave and improving the rate of RTW of employees. The subgroup analysis suggested that CBT-based intervention in the studies with the following characteristics had a better effect on sick leave in reduced days: treatment delivered face-to-face, utilization of rehabilitation services, stress management, homework assignment and long treatment course (≥ 16 weeks). We did not find any significant difference between the CBT-based interventions and the control in reducing anxiety, and working ability but CBT-based interventions were more effective in managing stress, fatigue, mental illness, physical function, and depression compared to the control condition. Subgroup analysis results demonstrate that CBT-based interventions with the following characteristics had a better effect on depression symptoms: participants with higher education levels (> 12 years, longer treatment courses (≥ 16 weeks), and treatment delivered in group sessions. CBT-based interventions showed a better effect on depression when they used the following components: rehabilitation services, homework assignments, and psychological education. Overall, CBT-based interventions are a good option for promoting RTW and reducing the length of sick leaves in employees.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Aas RW, Strupstad J. Sickness Absence Dictionary (SAD-1). 2017. p. 106.
MacEachen E, Clarke J, Franche R-L, Irvin E, Group W-bRtWLR. Systematic review of the qualitative literature on return to work after injury. Scandinavian Journal of Work, Environment & health. 2006: 257–269.
Scheil-Adlung X, Sandner L. The case for paid sick leave. World Health Report. 2010.
Thorsen SV, Flyvholm M-A, Bach E. Absence report 2017: descriptive analysis of wage earners’ sickness absence in Denmark based on register and questionnaire data, The National Research Center for the Working Environment. 2018.
Black CM. Working for a healthier tomorrow: Dame Carol Black’s review of the health of Britain’s working age population: The Stationery Office; 2008.
Grinza E, Rycx F. The impact of sickness absenteeism on firm productivity: new evidence from Belgian matched employer–employee panel data. Ind Relat: J Econ Soc. 2020;59(1):150–194.
Agency SSI. Social insurance in figures. Stockholm Sweden; 2020.
Beesdo K, Bittner A, Pine DS, Stein MB, Höfler M, Lieb R, et al. Incidence of social anxiety disorder and the consistent risk for secondary depression in the first three decades of life. Arch Gen Psychiatry. 2007;64(8):903–912.
OECD. Union E. Health at a glance: Europe 20182018.
Dellve L, Ahlstrom L, Jonsson A, Sandsjö L, Forsman M, Lindegård A, et al. Myofeedback training and intensive muscular strength training to decrease pain and improve work ability among female workers on long-term sick leave with neck pain: a randomized controlled trial. Int Arch Occup Environ Health. 2011;84(3):335–346.
Dieppe P. Chronic musculoskeletal pain. British Medical Journal. 2013; 346.
Campbell P, Wynne-Jones G, Muller S, Dunn KM. The influence of employment social support for risk and prognosis in nonspecific back pain: a systematic review and critical synthesis. Int Arch Occup Environ Health. 2013;86(2):119–137.
Alison BM. Work-related musculoskeletal disorders. Dental Nursing. 2016;12(2):80–83.
Finnes A, Enebrink P, Ghaderi A, Dahl J, Nager A, Öst L-G. Psychological treatments for return to work in individuals on sickness absence due to common mental disorders or musculoskeletal disorders: a systematic review and meta-analysis of randomized-controlled trials. Int Arch Occup Environ Health. 2019;92(3):273–293.
Winter L, Geldmacher J, Plücker-Boss K, Kahl KG. Integration of a return-to-work module in cognitive behavioral therapy in patients with major depressive disorder and long-term sick leave—a feasibility study. Front Psychiatry. 2020;11:512.
Salomonsson S, Santoft F, Lindaster E, Ejeby K, Ljtosson B, Ost LG, et al. Cognitive-behavioural therapy and return-to-work intervention for patients on sick leave due to common mental disorders: a randomised controlled trial. Occup Environ Med. 2017;74(12):905–912.
David D, Cristea I, Hofmann SG. Why cognitive behavioral therapy is the current gold standard of psychotherapy. Front Psychiatry. 2018;9:4.
Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The efficacy of cognitive behavioral therapy: a review of meta-analyses. Cognit Ther Res. 2012;36(5):427–440.
Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: are the effects dependent on gender? J Int Assoc Study Pain. 2001;91(1–2):65–78.
Leon L, Jover JA, Candelas G, Lajas C, Vadillo C, Blanco M, et al. Effectiveness of an early cognitive-behavioral treatment in patients with work disability due to musculoskeletal disorders. Arthritis Care Res. 2009;61(7):996–1003.
Marhold C, Linton SJ, Melin L. A cognitive-behavioral return-to-work program: effects on pain patients with a history of long-term versus short-term sick leave. J Int Assoc Study Pain. 2001;91(1–2):155–163.
Craske MG. Cognitive–behavioral therapy: American Psychological Association; 2010.
Grosse Holtforth M, Castonguay LG, Boswell JF, Wilson LA, Kakouros AA, Borkovec TD. Insight in Cognitive-Behavioral Therapy. American Psychological Association. 2007.
Morley S. Efficacy and effectiveness of cognitive behaviour therapy for chronic pain: progress and some challenges. J Int Assoc Study Pain. 2011;152(3):S99–106.
Fenn K, Byrne M. The key principles of cognitive behavioural therapy. InnovAiT. 2013;6(9):579–585.
Wainwright E, Wainwright D, Coghill N, Walsh J, Perry R. Resilience and return-to-work pain interventions: systematic review. Occup Med. 2019;69(3):163–176.
Lloyd J, Bond FW, Flaxman PE. The value of psychological flexibility: examining psychological mechanisms underpinning a cognitive behavioural therapy intervention for burnout. Work Stress. 2013;27(2):181–199.
Maguire N, Grellier B, Clayton K. The impact of CBT training and supervision on burnout, confidence and negative beliefs in a staff group working with homeless people. Housing, Care and Support. 2012.
Jensen IB, Bergström G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: Are the effects dependent on gender? Pain. 2001;91(1–2):65–78.
Willert MV, Thulstrup AM, Bonde JP. Effects of a stress management intervention on absenteeism and return to work–results from a randomized wait-list controlled trial. Scand J Work Environ Health. 2011;37(3):186–195.
Stenlund T, Ahlgren C, Lindahl B, Burell G, Steinholtz K, Edlund C, et al. Cognitively oriented behavioral rehabilitation in combination with Qigong for patients on long-term sick leave because of burnout: REST—a randomized clinical trial. Int J Behav Med. 2009;16(3):294.
Kaldo V, Lundin A, Hallgren M, Kraepelien M, Strid C, Ekblom Ö, et al. Effects of Internet-based cognitive behavioural therapy and physical exercise on sick leave and employment in primary care patients with depression: two subgroup analyses. Occup Environ Med. 2018;75(1):52–58.
De Vente W, Kamphuis JH, Emmelkamp PM, Blonk RW. Individual and group cognitive-behavioral treatment for work-related stress complaints and sickness absence: a randomized controlled trial. J Occup Health Psychol. 2008;13(3):214.
Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work Stress. 2006;20(2):129–144.
Haldorsen E, Kronholm K, Skouen J, Ursin H. Multimodal cognitive behavioral treatment of patients sicklisted for musculoskeletal pain: a randomized controlled study. Scand J Rheumatol. 1998;27(1):16–25.
Arends I, Bruinvels DJ, Rebergen DS, Nieuwenhuijsen K, Madan I, Neumeyer-Gromen A, et al. Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database Syst Rev. 2012;12:1.
Nieuwenhuijsen K, Verbeek JH, Neumeyer-Gromen A, Verhoeven AC, Bültmann U, Faber B. Interventions to improve return to work in depressed people. Cochrane Database Syst Rev. 2020;10:1.
Schaafsma FG, Whelan K, van der Beek AJ, van der Es-Lambeek LC, Ojajärvi A, Verbeek JH. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database Syst Rev. 2013;8:1.
Nazarov S, Manuwald U, Leonardi M, Silvaggi F, Foucaud J, Lamore K, et al. Chronic diseases and employment: which interventions support the maintenance of work and return to work among workers with chronic illnesses? A systematic review. Int J Environ Res Public Health. 2019;16(10):1864.
De Morton NA. The PEDro scale is a valid measure of the methodological quality of clinical trials: a demographic study. Australian J Physiother. 2009;55(2):129–133.
Ismail A, Moore C, Alshishani N, Yaseen K, Alshehri MA. Cognitive behavioural therapy and pain coping skills training for osteoarthritis knee pain management: a systematic review. J Phys Ther Sci. 2017;29(12):2228–2235.
Adler DA, Lerner D, Visco ZL, Greenhill A, Chang H, Cymerman E, et al. Improving work outcomes of dysthymia (persistent depressive disorder) in an employed population. Gen Hosp Psychiatry. 2015;37(4):352–359.
Bethge M, Herbold D, Trowitzsch L, Jacobi C. Work status and health-related quality of life following multimodal work hardening: a cluster randomised trial. J Back Musculoskelet Rehabil. 2011;24(3):161–172.
Glasscock DJ, Carstensen O, Dalgaard VL. Recovery from work-related stress: a randomized controlled trial of a stress management intervention in a clinical sample. Int Arch Occup Environ Health. 2018;91(6):675–687.
Kröger C, Bode K, Wunsch E-M, Kliem S, Grocholewski A, Finger F. Work-related treatment for major depressive disorder and incapacity to work: preliminary findings of a controlled, matched study. J Occup Health Psychol. 2015;20(2):248.
Schweikert B, Jacobi E, Seitz R, Cziske R, Ehlert A, Knab J, et al. Effectiveness and cost-effectiveness of adding a cognitive behavioral treatment to the rehabilitation of chronic low back pain. J Rheumatol. 2006;33(12):2519–2526.
Huibers MJ, Beurskens AJ, Van Schayck CP, Bazelmans E, Metsemakers JF, Knottnerus JA, et al. Efficacy of cognitive–behavioural therapy by general practitioners for unexplained fatigue among employees: randomised controlled trial. Br J Psychiatry. 2004;184(3):240–246.
Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB. Work-focused treatment of common mental disorders and return to work: a comparative outcome study. J Occup Health Psychol. 2012;17(2):220.
Van Den Hout JH, Vlaeyen JW, Heuts PH, Zijlema JH, Wijnen JA. Secondary prevention of work-related disability in nonspecific low back pain: does problem-solving therapy help? A randomized clinical trial. Clin J Pain. 2003;19(2):87–96.
van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med. 2003;60(6):429–437.
Volker D, Zijlstra-Vlasveld MC, Anema JR, Beekman AT, Brouwers EP, Emons WH, et al. Effectiveness of a blended web-based intervention on return to work for sick-listed employees with common mental disorders: results of a cluster randomized controlled trial. J Med Internet Res. 2015;17(5):e116.
Dalgaard VL, Aschbacher K, Andersen JH, Glasscock DJ, Willert MV, Carstensen O, et al. Return to work after work-related stress: a randomized controlled trial of a work-focused cognitive behavioral intervention. Scand J Work Environ Health. 2017;43(5):436–446.
Jørgensen MB, Faber A, Hansen JV, Holtermann A, Søgaard K. Effects on musculoskeletal pain, work ability and sickness absence in a 1-year randomised controlled trial among cleaners. BMC Public Health. 2011;11:1.
Eriksson MC, Kivi M, Hange D, Petersson E-L, Ariai N, Häggblad P, et al. Long-term effects of Internet-delivered cognitive behavioral therapy for depression in primary care–the PRIM-NET controlled trial. Scand J Prim Health Care. 2017;35(2):126–136.
Heiden M, Lyskov E, Nakata M, Sahlin K, Sahlin T, Barnekow-Bergkvist M. Evaluation of cognitive behavioural training and physical activity for patients with stress-related illnesses: a randomized controlled study. J Rehabil Med. 2007;39(5):366–373.
Jensen IB, Bergström G, Ljungquist T, Bodin L. A 3-year follow-up of a multidisciplinary rehabilitation programme for back and neck pain. Pain. 2005;115(3):273–283.
Linton SJ, Boersma K, Jansson M, Svärd L, Botvalde M. The effects of cognitive-behavioral and physical therapy preventive interventions on pain-related sick leave: a randomized controlled trial. Clin J Pain. 2005;21(2):109–119.
Salomonsson S, Santoft F, Lindsäter E, Ejeby K, Ingvar M, Ljótsson B, et al. Effects of cognitive behavioural therapy and return-to-work intervention for patients on sick leave due to stress-related disorders: results from a randomized trial. Scand J Psychol. 2020;61(2):281–289.
Salomonsson S, Santoft F, Lindsäter E, Ejeby K, Ljótsson B, Öst L-G, et al. Cognitive–behavioural therapy and return-to-work intervention for patients on sick leave due to common mental disorders: a randomised controlled trial. Occup Environ Med. 2017;74(12):905–912.
Reme SE, Grasdal AL, Løvvik C, Lie SA, Øverland S. Work-focused cognitive–behavioural therapy and individual job support to increase work participation in common mental disorders: a randomised controlled multicentre trial. Occup Environ Med. 2015;72(10):745–752.
Lambeek LC, Bosmans JE, Van Royen BJ, Van Tulder MW, Van Mechelen W, Anema JR. Effect of integrated care for sick listed patients with chronic low back pain: economic evaluation alongside a randomised controlled trial. BMJ (Clin Res Ed). 2010;341:c6414.
Schultz IZ, Crook J, Berkowitz J, Milner R, Meloche GR, Lewis ML. A prospective study of the effectiveness of early intervention with high-risk back-injured workers—a pilot study. J Occup Rehabil. 2008;18(2):140–151.
Salomonsson S, Santoft F, Lindsäter E, Ejeby K, Ljótsson B, Öst L-G, et al. Cognitive–behavioural therapy and return-to-work intervention for patients on sick leave due to common mental disorders: a randomised controlled trial. Occup Environ Med (London, England). 2017;74(12):905–912.
Hoff A, Poulsen RM, Fisker JP, Hjorthøj C, Nordentoft M, Christensen U, et al. Integrated mental healthcare and vocational rehabilitation for people on sick leave with anxiety or depression: 24-month follow-up of the randomized IBBIS trial. J Occup Rehabil. 2023. https://doi.org/10.1007/s10926-023-10094-7.
Sample P. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146:317–325.
Olsen L, Mortensen E, Bech P. Prevalence of major depression and stress indicators in the Danish general population. Acta Psychiatr Scand. 2004;109(2):96–103.
Sochting I. Cognitive Behavioral Group Therapy: Challenges and Opportunities. Wiley; 2014.
Carlbring P, Andersson G, Cuijpers P, Riper H, Hedman-Lagerlöf E. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: an updated systematic review and meta-analysis. Cogn Behav Ther. 2018;47(1):1–18.
Axelsson E, Andersson E, Ljótsson B, Björkander D, Hedman-Lagerlöf M, Hedman-Lagerlöf E. Effect of internet vs face-to-face cognitive behavior therapy for health anxiety: a randomized noninferiority clinical trial. JAMA Psychiat. 2020;77(9):915–924.
Okamura KH, Benjamin Wolk CL, Kang-Yi CD, Stewart R, Rubin RM, Weaver S, et al. The price per prospective consumer of providing therapist training and consultation in seven evidence-based treatments within a large public behavioral health system: an example cost-analysis metric. Front Public Health. 2017;5:356.
Kaldo V, Lundin A, Hallgren M, Kraepelien M, Strid C, Ekblom Ö, et al. Effects of internet-based cognitive behavioural therapy and physical exercise on sick leave and employment in primary care patients with depression: two subgroup analyses. Occup Environ Med (London, England). 2018;75(1):52–58.
Anclair M, Lappalainen R, Muotka J, Hiltunen AJ. Cognitive behavioural therapy and mindfulness for stress and burnout: a waiting list controlled pilot study comparing treatments for parents of children with chronic conditions. Scand J Caring Sci. 2018;32(1):389–396.
Hägglund P, Johansson P, Laun L. The impact of CBT on sick leave and health. Eval Rev. 2020;44(2–3):185–217.
Acknowledgements
Kelly Lin, School of Medicine and Dentistry, Griffith University, Australia for her contrition in double-checking the data extraction quality.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
JS designed and conceptualized the study. HX and JC conducted literature search and drafted the manuscript. The quality of studies was assessed by HX, JC and JS. Data extraction were performed by HX, JXC, RS, SJ. JS conducted data analysis and supervised the study. All authors commented on the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical Approval
The study was registered at PROSPERO (Registration Number: CRD42021260666).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, H., Cai, J., Sawhney, R. et al. The Effectiveness of Cognitive-Behavioral Therapy in Helping People on Sick Leave to Return to Work: A Systematic Review and Meta-analysis. J Occup Rehabil 34, 4–36 (2024). https://doi.org/10.1007/s10926-023-10116-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-023-10116-4