Abstract
To improve and increase drug permeation efficiency and hydrogel stability, a gelatin/shellac (Gel/SL) hydrogel was prepared for use in transdermal patches. Gallic acid (Gal) was selected as a model active pharmaceutical ingredient (API). Gel/SL hydrogels were prepared with various amounts of SL (0–30% w/w SL). The swelling and permeation behavior of Gel/SL hydrogels were studied. The rigidity and hydrophobic aliphatic groups of SL affect the swelling characteristics of hydrogels, and the percentage of swelling decreases with increasing SL ratio. The permeation characteristic experiments were carried out at pH 7.4 and 37 °C for 48 h. To enhance the amount of Gal permeation, an external voltage (0–3 V) was applied. The amount of Gal permeation into tissue from Gel/SL hydrogels increased rapidly at the initial state before reaching time equilibrium, TEP (< 8 h). When a voltage was applied, the amount of Gal permeation increased due to the stronger electrorepulsive force, micro pathway generation and transappendageal route expansion. To improve the mechanical properties of the hydrogel, Gel/SL was prepared with various amounts of crosslinking agent. The physical properties and mechanical properties of the hydrogels were studied. The hardness and tensile strength were improved when the amount of crosslink agent increased due to the higher number of hydrogel strands. The amount of permeated Gal increases with decreasing amounts of crosslinking agent due to the higher free volume in the matrix. The % cell viability (of fibroblast cells) was higher than 80%. Thus, these Gel/SL hydrogels could serve as an alternative hydrogel for user-friendly and controllable transdermal patch applications.
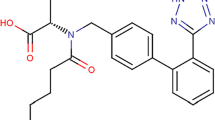
Graphical Abstract











Similar content being viewed by others
References
Olatunji O, Richard O (2015) Processing and characterization of natural polymers. Springer International Publishing AG
Akash MSH, Rehman K, Chen S (2015) Natural and synthetic polymers as drug carriers for delivery of therapeutic proteins. Polym Rev 55:371–406
Kandavilli S, Nair V, Panchagnula R (2002) Polymers in transdermal drug delivery systems. Pharm Technol 26(5):62–81
Ahmed EM (2015) Hydrogel: Preparation, characterization, and applications: a review. J Adv Res 6:105–121
Gulrez SKH, Al-A S, Phillips GO (2011) Hydrogels: methods of preparation, characterisation and applications. Intech Published
Ganji F, Vasheghani-F S, Vasheghani-F E (2010) Theoretical description of hydrogel swelling: a review. Iran Polym J 19(5):375–398
Rastogi V, Rastogi P (2012) Transdermal drug delivery system: an overview. Asian J Pharm 6(3):161–170
Bala P, Jathar S, Kale S, Pal K (2015) Transdermal drug delivery system (TDDS): a multifaceted approach for drug delivery. J Pharm Res 8(12):1805–1835
Jeong WY, Kwon M, Choi HE, Kim KS (2021) Recent advances in transdermal drug delivery systems: a review. Biomater. Res. 25(24):1–15
Alkilani AZ, Alkilani MTC, Donnelly RF (2015) Transdermal drug delivery: innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics 7:438–470
Wang F-F, Chen Y, Huang Y-Y, Cheng C-M (2021) Transdermal drug delivery systems for fighting common viral infectious diseases. Drug Deliv Transl Res 11:1498–1508
Sachan R, Bajpai M (2013) Transdermal drug delivery system: a review. Int J Res Dev Pharm L Sci 3(1):748–765
Tanwar H, Sachdeva R (2016) Transdermal drug delivery system: a review. IJPSR 7(6):2274–2290
Patel D, Chaudhary SA, Parmar B, Bhura N (2012) Transdermal drug delivery system: a review. J Pharm Innov 1(4):66–75
Yue K, Santiago GT-D, Alvarez MM, Tamayol A, Annabi N, Khademhosseini A (2015) Synthesis, properties, and biomedical applications of gelatin methacryloyl (GelMA) hydrogels. Biomaterials 73:254–271
Koshy ST, Desai RM, Joly P, Li J, Bagrodia RK, Lewin SA, Joshi NS, Mooney DJ (2016) Click-crosslinked injectable gelatin hydrogels. Adv Healthcare Mater 5(5):541–547
Salamon A, Vlierberghe SV, Nieuwenhove IV, Baudisch F, Graulus G-J, Benecke V, Alberti K, Neumann H-G, Rychly J, Martins JC, Dubruel P, Peters K (2014) Gelatin-based hydrogels promote chondrogenic differentiation of human adipose tissue-derived mesenchymal stem cells in vitro. Materials 7:1342–1359
García-Astrain C, Guaresti O, González K, Santamaria-Echart A, Eceiza A, Corcuera MC, Gabilondo N (2016) Click gelatin hydrogels: characterization and drug release behavior. Mater Lett 182:134–137
Kikkawa YS, Nakagawa T, Nakagawa L, Tabata Y, Tsubouchi H, Ido A, Ito J (2014) Growth factor-eluting cochlear implant electrode: impact on residual auditory function, insertional trauma, and fibrosis. J Transl Med 12:280
Rattana M, Paradee N, Paradee A, Niamlang S (2015) Porcine and fish gelatin hydrogels for controlled release of salicylic acid and 5-sulfosalicylic acid. Int J Drug Dev Res 7(1):107–117
Xue M, Hu H, Jiang Y, Liu J, He H, Ye X (2012) biodegradable polymer-coated, gelatin hydrogel/bioceramics ternary composites for antitubercular drug delivery and tissue regeneration. J Nanomater 2012:1–8
Ooi SY, Ahmad I, Cairul IMAM (2016) Cellulose nanocrystals extracted from rice husks as a reinforcing material in gelatin hydrogels for use in controlled drug delivery systems. Ind Crops Prod 93:227–234
Al-Gousous J, Penning M, Langguth P (2015) Molecular insights into shellac film coats from different aqueous shellac salt solutions and effect on disintegration of enteric-coated soft gelatin capsules. Int J Pharm 484:283–291
Pearnchob N, Dashevsky A, Bodmeier R (2004) Improvement in the disintegration of shellac-coated soft gelatin capsules in simulated intestinal fluid. JCR 94:313–321
Soradech S, Nunthanid J, Limmatvapirat S, Luangtana-anan M (2012) An approach for the enhancement of the mechanical properties and film coating efficiency of shellac by the formation of composite films based on shellac and gelatin. J Food Eng 108:94–102
Phaechamud T, Choncheewa C (2016) Double-layered matrix of shellac wax-lutrol in controlled dual drug release. AAPS PharmSciTech 17(6):1326–1335
Nayeem N, SMB A, Salem H, AHEl-Alfqy S (2016) Gallic acid: a promising lead molecule for drug development. J App Pharm 8(2):1–4
Cassano R, Mellace S, Picci N (2015) New Gallic acid based hydrogel for phloretin intestinal release. IJPRD 7(05):001–009
Borges A, Saavedra MJ, Simoes M (2012) The activity of ferulic and gallic acids in biofilm prevention and control of pathogenic bacteria. Biofouling 28(7):755–767
Sorrentino E, Succi M, Tipaldi L, Pannella G, Maiuro L, Maiuro M, Coppola R, Tremonte P (2018) Antimicrobial activity of gallic acid against food-related Pseudomonas strains and its use as biocontrol tool to improve the shelf life of fresh black truffles. Int J Food Microbiol 266:183–189
Buapool D, Mongkol N, Chantimal J, Roytrakul S, Srisook E, Srisook K (2013) Molecular mechanism of anti-inflammatory activity of Pluchea indica leaves in macrophages RAW 264.7 and its action in animal models of inflammation. J Ethnopharmacol 146:495–504
Bouillaguet S, Shaw L, Gonzalez L, Wataha C, Krejci I (2002) Long-term cytotoxicity of resin-based dental restorative materials. J Oral Rehabil 29:7–13
Juntanon K, Niamlang S, Niamlang R, Sirivat A (2008) Electrically controlled release of sulfosalicylic acid from crosslinked poly(vinyl alcohol) hydrogel. Int J Pharm 356:1–11
Phaechamud T, Mahadlek J, Chuenbarn T (2016) In situ forming gel comprising bleached shellac loaded with antimicrobial drugs for periodontitis treatment. Mater Des 89:294–303
Niamlang S, Buranut T, Niansiri A, Sirivat A (2013) Controlled aloin release from crosslinked polyacrylamide hydrogels: effects of mesh size, electric field strength and a conductive polymer. Materials 6:4787–4800
Dash S, Murthy PN, Nath L, Chowdhury P (2010) Kinetic Modeling on drug release from controlled drug delivery systems. Acta Pol Pharm 67(3):217–223
Niamlang S, Paradee N, Sirivat A (2018) Hybrid transdermal drug delivery patch made from poly(p-phenylene vinylene)/natural rubber latex and controlled by an electric field. Polym Int 67(6):747–754
Siepmann J, Peppas NA (2011) Higuchi equation: derivation, applications, use and misuse. Int J Pharm 418:6–12
Niamlang S, Sirivat A (2009) Electrically controlled release of salicylic acid from poly(p-phenylene vinylene)/polyacrylamide hydrogels. Int J Pharm 371:126–133
Thorngkham P, Paradee N, Niamlang S, Sirivat A (2015) Permeation study of indomethacin from polycarbazole/natural rubber blend film for electric field controlled transdermal delivery. J Pharm Sci 104(5):1795–1803
Chansai P, Sirivat A, Niamlang S, Chotpattananont D, Viravaidya-Pasuwat K (2009) Controlled transdermal iontophoresis of sulfosalicylic acid from polypyrrole/poly(acrylic acid) hydrogel. Int J Pharm 381:25–33
Phaechamud T, Chanyaboonsub N, Setthajindalert O (2016) Doxycycline hyclate-loaded bleached shellac in situ forming microparticle for intraperiodontal pocket local delivery. Eur J Pharm Sci 93:360–370
Srichan T, Phaechamud T (2016) Designing solvent exchange-induced in situ forming gel from aqueous insoluble polymers as matrix base for periodontitis treatment. AAPS PharmSciTech 18(1):194–201
Sittiwong J, Niamlang S, Paradee N, Sirivat A (2012) Electric field-controlled benzoic acid and sulphanilamide delivery from poly (vinyl alcohol) hydrogel. AAPS PharmSciTech 13(4):1407–1415
Ruangmak K, Paradee N, Niamlang S, Sakunpongpitiporn P, Sirivat A (2022) Electrically controlled transdermal delivery of naproxen and indomethacin from porous cis-1,4-polyisoprene matrix. J Biomed Mater Res 110(2):478–488
Choncheewa C, Phaechamud T (2012) Characterization and drug behavior in shellac wax—poloxamer matrix tablets fabricated with mold Technique. J Met Mater Miner 22(2):67–74
Suksaeree J, Karnsopa P, Wannaphruek N, Prasomkij J, Panrat K, Pichayakorn W (2018) Transdermal delivery of nicotine using pectin isolated from durian fruit-hulls-based polymer blends as a matrix layer. J Polym Environ 26:3216–3225
Wannaphatchaiyong S, Suksaeree J, Waiprib R, Kaewpuang A, Saelee W, Saelee W (2019) Gelatin/Gelatinized sago starch biomembranes as a drug delivery system using rubber latex as plasticizer. J Polym Environ 27:2380–2394
Ghaem B, Sadeghi M, Bardajee GR (2020) Synthesis of nano-polymer supported on nano-hydrogel chitosan base and its application for DOX delivery. J Polym Environ 28:2457–2468
Bera H, Abbasi YF, Hoong AK, Be LP, Wuan TJ, Guo H, Cun D, Yang M, Seen LY, Woan LL, Ying SQ (2021) Functionalized food-grade biopolymer-nanosilica based hybrid hydrogels as sustained delivery devices of rutin. J Polym Environ 29:260–270
Kaewchingduang R, Paradee N, Sirivat A, Niamlang S (2019) Effects of conductive polyazulene and plasticizer embedded in deproteinized natural rubber transdermal patch on electrically controlled naproxen release-permeation. Int J Pharm 561:296–304
Paradee N, Sirivat A, Niamlang S, Prissanaroon-Ouajai W (2012) Effects of crosslinking ratio, model drugs, and electric field strength on electrically controlled release for alginate-based hydrogel. J Mater Sci: Mater Med 23:999–1010
Banpean A, Paradee N, Sirivat A, Niamlang S (2018) Deproteinized natural rubber as an electrically controllable transdermal drug-delivery patch. J Polym Environ 26:3745–3753
Acknowledgements
The authors would like to thank the Advance Material Research Group of RMUTT, Rajamangala University of Technology Thanyaburi (RMUTT), Thailand.
Funding
This project was supported by Reinventing University Project (given to Rajamangala University of Technology Thanyaburi (RMUTT), Thailand) 2022, Office of the Ministry of Higher Education, Science, Research and Innovation, Thailand Science Research and Innovation.
Author information
Authors and Affiliations
Contributions
SC, experiment, wrote the manuscript and data analysis. SN, Ideation, experimental setting and analysis, wrote manuscript and corresponding author.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chungyampin, S., Niamlang, S. Electrical Stimuli-Responsive Gelatin/Shellac Gel Blends for Use as Controllable Transdermal Delivery Patches. J Polym Environ 31, 3248–3258 (2023). https://doi.org/10.1007/s10924-023-02808-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10924-023-02808-y