Abstract
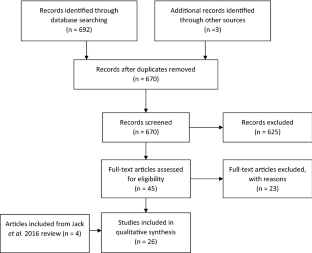
Community Health Worker (CHW) interventions have shown potential to reduce inequities for underserved populations. However, there is a lack of support for CHW integration in the delivery of health care. This may be of particular importance in rural areas in the Unites States where access to care remains problematic. This review aims to describe CHW interventions and their outcomes in rural populations in the US. Peer reviewed literature was searched in PubMed and PsycINFO for articles published in English from 2015 to February 2021. Title and abstract screening was performed followed by full text screening. Quality of the included studies was assessed using the Downs and Black score. A total of 26 studies met inclusion criteria. The largest proportion were pre-post program evaluation or cohort studies (46.2%). Many described CHW training (69%). Almost a third (30%) indicated the CHW was integrated within the health care team. Interventions aimed to provide health education (46%), links to community resources (27%), or both (27%). Chronic conditions were the concern for most interventions (38.5%) followed by women’s health (34.6%). Nearly all studies reported positive improvement in measured outcomes. In addition, studies examining cost reported positive return on investment. This review offers a broad overview of CHW interventions in rural settings in the United States. It provides evidence that CHW can improve access to care in rural settings and may represent a cost-effective investment for the healthcare system.
Similar content being viewed by others
Data Availability
All data is from the published literature.
Code Availability
not applicable.
References
Bolin, J. N., Bellamy, G. R., Ferdinand, A. O., et al. (2015). Rural healthy people 2020: new decade, same challenges. The Journal of Rural Health, 31(3), 326–333.
Cardarelli, R., Bausch, G., Murdock, J., & Chyatte, M. R. (2018). Return-on-Investment (ROI) analyses of an inpatient lay health worker model on 30-day readmission rates in a rural community hospital. The Journal of Rural Health, 34(4), 411–422.
Cardarelli, R., Horsley, M., Ray, L., et al. (2018). Reducing 30-day readmission rates in a high-risk population using a lay-health worker model in Appalachia Kentucky. Health Education Research, 33(1), 73–80.
Center for Disease Control and Prevention. (2020). About Rural Health. Centers for Disease Control and Prevention. https://www.cdc.gov/ruralhealth/about.html
Cramer, M. E., Mollard, E. K., Ford, A. L., Kupzyk, K. A., & Wilson, F. A. (2018). The feasibility and promise of mobile technology with community health worker reinforcement to reduce rural preterm birth. Public Health Nursing, 35(6), 508–516.
Crespo, R., Christiansen, M., Tieman, K., & Wittberg, R. (2020). An emerging model for community health worker-based chronic care management for patients with high health care costs in rural Appalachia. Preventing Chronic Disease, 17, E13.
Downs, S. H., & Black, N. (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology & Community Health, 52(6), 377–384.
Falk, D., Falk, D., Cubbin, C., et al. (2018). Increasing breast and cervical cancer screening in rural and border texas with friend to friend plus patient navigation. Journal of Cancer Education, 33(4), 798–805.
Falk, D., Foley, K., Weaver, K. E., Jones, B., & Cubbin, C. (2020). An Evaluation of Breast and Cervical Cancer Screening Outcomes in an Education and Patient Navigation Program in Rural and Border Texas. Journal of Cancer Education, 10, Epub ahead of print.
Fawcett, K., Neff, R., Freese Decker, C., & Faber, J. (2018). Achieving IHIʼs triple aim by utilizing core health program with community health workers in rural communities. Family & Community Health, 41(4), 255–264.
Felix, H. C., Ali, M., Bird, T. M., Cottoms, N., & Stewart, M. K. (2019). Are community health workers more effective in identifying persons in need of home and community-based long-term services than standard-passive approaches. Home Health Care Services Quarterly, 38(3), 194–208.
Felix, H. C., Mays, G. P., Stewart, M. K., Cottoms, N., & Olson, M. (2011). Medicaid savings resulted when community health workers matched those with needs to home and community care. Health Affairs, 30(7), 1366–1374.
Feltner, F., Thompson, S., Baker, W., & Slone, M. (2017). Community health workers improving diabetes outcomes in a rural Appalachian population. Social Work in Health Care, 56(2), 115–123.
Glenn, L. E., Nichols, M., Enriquez, M., & Jenkins, C. (2020). Impact of a community-based approach to patient engagement in rural, low-income adults with type 2 diabetes. Public Health Nursing, 37(2), 178–187.
Hopper, L. N., Blackman, K. F., Page, R. A., et al. (2017). Seeds of HOPE: incorporating community-based strategies to implement a weight-loss and empowerment intervention in Eastern North Carolina. North Carolina Medical Journal, 78(4), 230–236.
Hunter, J. B., de Zapien, J. G., Papenfuss, M., Fernandez, M. L., Meister, J., & Giuliano, A. R. (2004). The impact of a “Promotora” on increasing routine chronic disease prevention among women aged 40 and older at the US-Mexico Border. Health Education & Behavior, 31(4), 18–28.
Jack, H. E., Arabadjis, S. D., Sun, L., Sullivan, E. E., & Phillips, R. S. (2016). Impact of community health workers on use of healthcare services in the United States: a systematic review. Journal of General Internal Medicine, 32(3), 325–344.
Kitzman, P., Hudson, K., Sylvia, V., Feltner, F., & Lovins, J. (2017). Care coordination for community transitions for individuals post-stroke returning to low-resource rural communities. Journal of Community Health, 42(3), 565–572.
Krantz, M. J., Coronel, S. M., Whitley, E. M., Dale, R., Yost, J., & Estacio, R. O. (2013). Effectiveness of a community health worker cardiovascular risk reduction program in public health and health care settings. American Journal of Public Health, 103(1), e19–e27.
Krok-Schoen, J. L., Oliveri, J. M., Young, G. S., Katz, M. L., Tatum, C. M., & Paskett, E. D. (2015). Evaluating the stage of change model to a cervical cancer screening intervention among Ohio Appalachian women. Women and Health, 56(4), 468–4886.
Logan, R. I., & Castañeda, H. (2020). Addressing health disparities in the rural United States: advocacy as caregiving among community health workers and Promotores de Salud. International Journal of Environmental Research and Public Health, 17(24), 10.
Luque, J., Tarasenko, Y., Reyes-Garcia, C., et al. (2017). Salud es Vida: a Cervical Cancer Screening Intervention for Rural Latina Immigrant Women. Journal of Cancer Education, 32(4), 690–699.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, T. P. (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLOS Medicine, 6(7), e1000097
NACHW. (2021). CHW Networks and Training Programs. NACHW. https://nachw.org/membership/chw-networks-and-certification-programs/
Nkonki, L., Tugendhaft, A., & Hofman, K. (2017). A systematic review of economic evaluations of CHW interventions aimed at improving child health outcomes. Human Resources for Health, 15(1), 19.
Postma, J. M., Smalley, K., Ybarra, V., & Kieckhefer, G. (2011). The Feasibility and acceptability of a home-visitation, asthma education program in a rural, Latino a population. The Journal of Asthma, 48(2), 139–146.
Probst, J., Zahnd, W., & Breneman, C. (2019). Declines in pediatric mortality fall short for rural US children. Health Affairs, 38(12), 2069–2076.
Reed, P. H., & Hulton, L. J. (2017). Community health workers in collaboration with case managers to improve quality of life for patients with heart failure. Professional Case Management, 22(3), 144–148.
Riedy, C. A., Weinstein, P., Mancl, L., Garson, G., Huebner, C. E., Milgrom, P., Grembowski, D., Shepherd-Banigan, M., Smolen, D., & Sutherland, M. (2015). Dental attendance among low-income women and their children following a brief motivational counseling intervention: a community randomized trial. Social Science & Medicine, 1982(144), 9–18.
Roland, K. B., Milliken, E. L., Rohan, E. A., et al. (2017). Use of Community health workers and patient navigators to improve cancer outcomes among patients served by federally qualified health centers: a systematic literature review. Health Equity, 1(1), 61–76.
Rural Health Information Hub. (2020). Substance Use and Misuse in Rural Areas. Rural Health Information Hub. https://www.ruralhealthinfo.org/topics/substance-use#:~:text=Though%20often%20perceived%20to%20be,in%20towns%20of%20every%20size.
Ryabov, I. (2014). Cost-effectiveness of community health workers in controlling diabetes epidemic on the US–Mexico border. Public Health, 128(7), 636–642.
Samuel-Hodge, C. D., Gizlice, Z., Allgood, S. D., et al. (2020). Strengthening community-clinical linkages to reduce cardiovascular disease risk in rural NC: feasibility phase of the CHANGE study. BMC Public Health, 20(1), 264.
Schleiff, M. J., Peters, D. H., & Surkan, P. J. (2020). Comparative case analysis of the role of community health workers in rural and low-income populations of west Virginia and the United States. The Journal of Ambulatory Care Management, 43(3), 205–220.
Smith, L., Atherly, A., Campbell, J., Flattery, N., Coronel, S., & Krantz, M. (2019). Cost-effectiveness of a statewide public health intervention to reduce cardiovascular disease risk. BMC Public Health, 19(1), 1234.
Suther, S., Battle, A. M., Battle-Jones, F., & Seaborn, C. (2016). Utilizing health ambassadors to improve type 2 diabetes and cardiovascular disease outcomes in Gadsden County, Florida. Evaluation and Program Planning, 55, 17–26.
Thompson, B., Carosso, E. A., Jhingan, E., et al. (2017). Results of a randomized controlled trial to increase cervical cancer screening among rural Latinas. Cancer, 123(4), 666–674.
Trump, L. J., & Mendenhall, T. J. (2017). Community health workers in diabetes care: a systematic review of randomized controlled trials. Families Systems & Health, 35(3), 320–340.
Turner, B. J., Liang, Y., Rodriguez, N., et al. (2018). Randomized trial of a low-literacy chronic pain self-management program: analysis of secondary pain and psychological outcome measures. The Journal of Pain, 19(12), 1471–1479. https://doi.org/10.1016/j.jpain.2018.06.010
Vilchis, H., Onstad, L. E., Benavidez, R., et al. (2019). Una Mano Amiga: pilot test of a patient navigator program for Southwest New Mexico. Journal of Cancer Education, 34(1), 173–179.
Weaver, A., & Lapidos, A. (2018). Mental health interventions with community health workers in the United States: a systematic review. Journal of Health Care for the Poor and Underserved, 29(1), 159–180.
Yaemsiri, S., Alfier, J. M., Moy, E., et al. (2019). Healthy people 2020: rural areas lag in achieving targets for major causes of death. Health Affairs (Project Hope), 38(12), 2027–2031.
Acknowledgements
The authors thank Teri Lynn Herbert for her expert assistance in finalizing the database search strategies.
Funding
There was no funding for this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization of the study; the first author performed the initial literature search and rating, the second author served as second rater, all authors contributed to subsequent analysis; the first author produced the initial draft, all authors critically revised the work and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflicts of interests to disclose.
Ethical Approval
Because the study is based on previously published information, no institutional review board approval is needed.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix
Search strategies
PubMed: ((Rural OR “rural health”) AND (“continuum of care” OR “Access to care” OR “health systems” OR “Women’s health” OR “disease prevention” OR “patient education” OR “managed care” OR “program cost” OR “health care system” OR "cost–benefit" OR "cost-effectiveness" OR "ED visit" OR “fees” OR "emergency department visit" OR "emergency room visit" OR "ER visit" OR "urgent care use" OR "urgent care visit" OR cost OR expenditure OR expense OR finance OR hospitalization OR payment OR profit OR readmission OR “Return on investment” OR savings OR utilization OR “insurance, health” [MeSH Terms] OR "costs and cost analysis"[MeSH Terms] OR "Medicaid/economics"[MeSH Terms] OR "Medicaid/utilization"[MeSH Terms] OR "Models, econometric"[MeSH Terms]) AND ("Abuse Counselor" OR "Birth attendant" OR "Case coordinator" OR "Community coordinator" OR "Community health advocate" OR "Community health aide" OR "Community health educator" OR "Community health representative" OR "Community health worker" OR "Community liaison" OR "Community organizer" OR "Community social worker" OR "Doula" OR "Family advocate" OR "Family support worker" OR "Health adviser" OR "Health advisor" OR "Health advocate" OR "Health agent" OR "Health assistant" OR "Health attendant" OR “health care volunteer” OR "Health coach" OR "Health Communicator" OR "Health Educator" OR "Home Care Worker" OR "Home health aide" OR "Home Visitor" OR "Intake specialist" OR "Lay attendant" OR "Lay health advisor" OR “Lay health adviser” OR "Lay health worker" OR "Lay personnel" OR "Medical representative" OR "Mental Health Worker" OR "Nutrition educator" OR "Outreach Coordinator" OR "Outreach Educator" OR "Outreach Worker" OR "Parent Aide" OR "Parent Liaison" OR "Patient navigator" OR "Peer advocate" OR "Peer coach" OR "Peer leader" OR "Promotora” OR "Recovery coach" OR Paraprofessional OR "community health workers"[MeSH Terms] OR "health educators"[MeSH Terms] OR "patient navigation"[MeSH Terms] OR "home health aides"[MeSH Terms])).
PsycINFO: (Rural OR “rural health”) AND (“continuum of care” OR “Access to care” OR “health systems” OR “Women’s health” OR “disease prevention” OR “patient education” OR “managed care” OR “program cost” OR “health care system” OR "cost–benefit" OR "cost-effectiveness" OR "ED visit" OR “fees” OR "emergency department visit" OR "emergency room visit" OR "ER visit" OR "urgent care use" OR "urgent care visit" OR cost OR expenditure OR expense OR finance OR hospitalization OR payment OR profit OR readmission OR “Return on investment” OR savings OR utilization) AND ("Abuse Counselor" OR "Birth attendant" OR "Case coordinator" OR "Community coordinator" OR "Community health advocate" OR "Community health aide" OR "Community health educator" OR "Community health representative" OR "Community health worker" OR "Community liaison" OR "Community organizer" OR "Community social worker" OR "Doula" OR "Family advocate" OR "Family support worker" OR "Health adviser" OR "Health advisor" OR "Health advocate" OR "Health agent" OR "Health assistant" OR "Health attendant" OR “health care volunteer” OR "Health coach" OR "Health Communicator" OR "Health Educator" OR "Home Care Worker" OR "Home health aide" OR "Home Visitor" OR "Intake specialist" OR "Lay attendant" OR "Lay health advisor" OR “Lay health adviser” OR "Lay health worker" OR "Lay personnel" OR "Medical representative" OR "Mental Health Worker" OR "Nutrition educator" OR "Outreach Coordinator" OR "Outreach Educator" OR "Outreach Worker" OR "Parent Aide" OR "Parent Liaison" OR "Patient navigator" OR "Peer advocate" OR "Peer coach" OR "Peer leader" OR "Promotora” OR "Recovery coach" OR Paraprofessional).
Rights and permissions
About this article
Cite this article
Berini, C.R., Bonilha, H.S. & Simpson, A.N. Impact of Community Health Workers on Access to Care for Rural Populations in the United States: A Systematic Review. J Community Health 47, 539–553 (2022). https://doi.org/10.1007/s10900-021-01052-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-021-01052-6




