Abstract
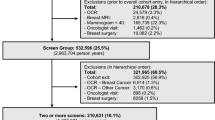
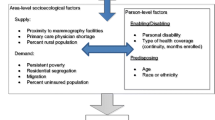
Not all women 50–74 years received biennial mammography and the situation is worse in rural areas. Accountable care organizations (ACO) emphasize coordinated care, use of electronic health system, and preventive quality measures and these practices may improve their patients’ breast cancer screening rate. Using medical record data of 8,347 women patients aged 50–74 years from eight rural ACO clinics in Nebraska, this study examined patient-, provider-, and county-level barriers and facilitators for breast cancer screening. A generalized estimating equations model was used to account for the correlation among patients from the same provider and county. The multi-level logistic regression results suggest that uninsured non-Hispanic Black patients were less likely to meet the biennial mammography screening guideline. Patients whose preferred language being English, having a preventive visit in the past 12 months, having one or more chronic conditions were more likely to meet the biennial mammography screening guideline. Patients with a primary care provider (PCP) that was male, without a medical doctor degree were less likely to screen biennially. Patients with a PCP that reviewed performance report quarterly, or manually checked patients’ mammography screening status during visits were more likely to screen biennially. Interestingly, patients whose PCP reported being reminded by a care coordination team were less likely to screen biennially. Patients living in counties with more PCPs were also more likely to screen biennially. The study findings suggest that efforts targeting individual and practice-level barriers could be most effective in improving mammography screening for these rural ACO patients.
Similar content being viewed by others
References
U.S. Preventive Services Task Force. (2016). Breast cancer screening final recommendations. Retrieved April 30, 2016 from http://screeningforbreastcancer.org/.
U.S. Cancer Statistics Working Group. (2015). United States Cancer Statistics: 1999–2012 Incidence and Mortality Web-based Report. (No. 2016). Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute.
Mandelblatt, J. S., Cronin, K. A., Bailey, S., et al. (2009). Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Annals of Internal Medicine, 151(10), 738–747.
Office of Disease Prevention and Health Promotion. (2016). Cancer. Retrieved April 9, 2016 from https://www.healthypeople.gov/2020/topics-objectives/topic/cancer/objectives.
Doescher, M. P., & Jackson, J. E. (2009). Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. Journal of Public Health Management and Practice, 15(3), 200–209. doi:10.1097/PHH.0b013e3181a117da.
Centers for Medicare and Medicaid Services. (2015). Accountable Care Organizations (ACO). Retrieved April 30, 2016 from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/index.html.
National Committee for Quality Assurance (NCQA). (2014). HEDIS 2015 technical specifications for ACO measurement. Washington, D.C.: National Committee for Quality Assurance (NCQA).
Nyweide, D. J., Lee, W., Cuerdon, T. T., Pham, H. H., Cox, M., Rajkumar, R., & Conway, P. H. (2015). Association of Pioneer accountable care organizations versus traditional Medicare fee for service with spending, utilization, and patient experience. JAMA: The Journal of the American Medical Association, 313(21), 2152–2161.
Schwartz, A. L., Chernew, M. E., Landon, B. E., & McWilliams, J. M. (2015). Changes in low-value services in year 1 of the Medicare Pioneer Accountable Care Organization Program. JAMA Internal Medicine, 175(11), 1815–1825.
Greene, J., Hibbard, J. H., & Overton, V. (2015). Large performance incentives had the greatest impact on providers whose quality metrics were lowest at baseline. Health Affairs, 34(4), 673–680. doi:10.1377/hlthaff.2014.0998.
McWilliams, J. M., Chernew, M. E., Landon, B. E., & Schwartz, A. L. (2015). Performance differences in year 1 of Pioneer Accountable Care Organizations. New England Journal of Medicine, 372(20), 1927–1936.
Salako, A., Zhu, X., MacKinney, A. C., Ullrich, F., & Mueller, K. (2015). Characteristics of rural Accountable Care Organizations (ACOs)—A survey of Medicare ACOs with rural presence. Rural Health Research & Policy Centers, & Rural Policy Research Institute, RUPRI Center for Rural Health Policy Analysis, University of Iowa College of Public Health, Department of Health Management and Policy.
Schueler, K. M., Chu, P. W., & Smith-Bindman, R. (2008). Factors associated with mammography utilization: a systematic quantitative review of the literature. Journal of Women’s Health, 17(9), 1477–1498.
Fox, S. A., Heritage, J., Stockdale, S. E., Asch, S. M., Duan, N., & Reise, S. P. (2009). Cancer screening adherence: Does physician–patient communication matter? Patient Education and Counseling, 75(2), 178–184.
Wilkinson, C., Champion, J. D., & Sabharwal, K. (2013). Promoting preventive health screening through the use of a clinical reminder tool: An accountable care organization quality improvement initiative. Journal for Healthcare Quality, 35(5), 7–19.
Office of Disease Prevention and Health Promotion. (2016). Social determinants of health. Retrieved April 10, 2016 from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health.
Litaker, D., & Tomolo, A. (2007). Association of contextual factors and breast cancer screening: finding new targets to promote early detection. Journal of Women’s Health, 16(1), 36–45.
Meersman, S. C., Breen, N., Pickle, L. W., Meissner, H. I., & Simon, P. (2009). Access to mammography screening in a large urban population: A multi-level analysis. Cancer Causes & Control, 20(8), 1469–1482.
Pagan, J. A., Asch, D. A., Brown, C. J., Guerra, C. E., & Armstrong, K. (2008). Lack of community insurance and mammography screening rates among insured and uninsured women. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 26(11), 1865–1870. doi:10.1200/JCO.2007.14.5664.
Schootman, M., Jeffe, D. B., Baker, E. A., & Walker, M. S. (2006). Effect of area poverty rate on cancer screening across US communities. Journal of Epidemiology and Community Health, 60(3), 202–207.
Fan, L., Mohile, S., Zhang, N., Fiscella, K., & Noyes, K. (2012). Self-reported cancer screening among elderly Medicare beneficiaries: A rural-urban comparison. The Journal of Rural Health, 28(3), 312–319.
Pruitt, S. L., Shim, M. J., Mullen, P. D., Vernon, S. W., & Amick, B. C. 3rd (2009). Association of area socioeconomic status and breast, cervical, and colorectal cancer screening: a systematic review. Cancer Epidemiology, Biomarkers & Prevention, 18(10), 2579–2599. doi:10.1158/1055-9965.EPI-09-0135.
United States Department of Agriculture Economic Research Service. (2013). Urban Influence Code. Retrieved September, 2016 from http://www.ers.usda.gov/data-products/urban-influence-codes.aspx.
Young, L., Kim, J., Wang, H., & Chen, L. (2015). Examining factors influencing colorectal cancer screening of rural Nebraskans using data from clinics participating in an accountable care organization: A study protocol. F1000Research 4:298. doi:10.12688/f1000research.6782.1.
Area Health Resources Files (AHRF). (2015–2016). Rockville, MD: US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce.
Environmental Systems Research Institute (ESRI). (2014). ArcGIS, ver. 10.1, Redlands, CA: Environmental Systems Research Institute (ESRI).
Ornstein, S. M., Nietert, P. J., Jenkins, R. G., & Litvin, C. B. (2013). The prevalence of chronic diseases and multimorbidity in primary care practice: A PPRNet report. Journal of the American Board of Family Medicine: JABFM, 26(5), 518–524. doi:10.3122/jabfm.2013.05.130012.
U.S. Food and Drug Administration. (2016). Mammography facilities. Retrieved April 30, 2016, from http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfMQSA/mqsa.cfm.
Dailey, A. B., Brumback, B. A., Livingston, M. D., Jones, B. A., Curbow, B. A., & Xu, X. (2011). Area-level socioeconomic position and repeat mammography screening use: Results from the 2005 National Health Interview Survey. Cancer Epidemiology, Biomarkers & Prevention: A Publication of the American Association for Cancer Research, 20(11), 2331–2344. doi:10.1158/1055-9965.EPI-11-0528.
Franks, P., & Clancy, C. M. (1993). Physician gender bias in clinical decision making: Screening for cancer in primary care. Medical Care, 31(3), 213–218.
Lurie, N., Slater, J., McGovern, P., Ekstrum, J., Quam, L., & Margolis, K. (1993). Preventive care for women—does the sex of the physician matter? New England Journal of Medicine, 329(7), 478–482.
Brooks, D. J. (2016). Differences in patient screening mammography rates associated with internist gender and level of training and change following the 2009 US Preventive Services Task Force Guidelines. Journal of the National Comprehensive Cancer Network, 14(6), 749–753.
Flocke, S. A., & Gilchrist, V. (2005). Physician and patient gender concordance and the delivery of comprehensive clinical preventive services. Medical Care, 43(5), 486–492.
Roter, D. L., Hall, J. A., & Aoki, Y. (2002). Physician gender effects in medical communication: a meta-analytic review. JAMA, 288(6), 756–764.
Martínez-González, N. A., Djalali, S., Tandjung, R., et al. (2014). Substitution of physicians by nurses in primary care: A systematic review and meta-analysis. BMC Health Services Research, 14(1), 1.
Horrocks, S., Anderson, E., & Salisbury, C. (2002). Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ, 324(7341), 819–823.
Hayes, K., & Bloniarz, K. (2013). Assessing payment adequacy: Physician and other health professional services. Washington, D.C: Medicare Payment Advisory Commission (MedPAC).
Kim, J., Young, L., Bekmuratova, S., Schober, D., Wang, H., Roy, S., Bhuyan, S., Schumaker, A., & Chen, L. (2017). Promoting colorectal cancer screening through a new model of delivering rural primary care in the United States: A qualitative study. Rural and Remote Health, 17(1), 4187. doi:10.22605/RRH4187. Retrieved from http://www.rrh.org.au/articles/subviewnew.asp?ArticleID=4187.
Sarfaty, M. (2008). How to increase colorectal cancer screening rates in practice: A primary care clinician’s evidence-based toolbox and guide. Atlanta: The American Cancer Society, The National Colorectal Cancer Roundtable and Thomas Jefferson University.
Wang, H., Qiu, F., Gregg, A., Chen, B., Kim, J., Young, L., Wan, N., & Chen, L. (2017). Barriers and facilitators of colorectal cancer screening for patients of rural accountable care organizations clinics: A multi-level analysis. Journal of Rural Health. doi:10.1111/jrh.12248.
Economic Research Service. (2017). Racial and ethnic diversity is increasing in rural America. Retrieved February 22, 2017, from http://www.ers.usda.gov/briefi ng/population/.
Acknowledgements
This publication was partially supported by the Fred & Pamela Buffett Cancer Center Support Grant from the National Cancer Institute under award number P30 CA036727. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. This study was also supported through “Pilot Grant for Cancer Prevention and Control’ by the College of Public Health at the University of Nebraska Medical Center. We also would like to express our appreciation to South East Rural Physician Alliance - Accountable Care Organization (SERPA-ACO) for their support for data collection and survey administration
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, H., Gregg, A., Qiu, F. et al. Breast Cancer Screening for Patients of Rural Accountable Care Organization Clinics: A Multi-Level Analysis of Barriers and Facilitators. J Community Health 43, 248–258 (2018). https://doi.org/10.1007/s10900-017-0412-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-017-0412-x