Abstract
Pediatric donors may be at increased risk of psychological and social challenges following hematopoietic cell transplantation (HCT). Through a retrospective chart review, we evaluated the health-related quality of life (HRQL) of pediatric donors over time and examined facilitators and barriers to implementing a longitudinal psychosocial assessment. Fifty-one pediatric donors (M = 10.7 years, SD = 3.7) completed an HRQL questionnaire across six time points (T1 to T6) from prior to donation to 2 years after. Change in mean scores was assessed using a linear mixed-effect model for repeated measures design. Facilitators and barriers to implementation were examined. HRQL of pediatric donors improved between T1 and T6 with significant change in physical, emotional, and overall functioning. Facilitators to retention included the support of a clinical coordinator. Barriers to implementation included the absence of infrastructure to maintain contact with pediatric and their families. HRQL of pediatric donors of HCT improved steadily over time. Pattern of results suggests a need to further explore factors that contribute to change across time. Development of a longitudinal standardized assessment protocol that can be prospectively and feasibly implemented is integral to supporting the well-being of this group.
Similar content being viewed by others
Background
Hematopoietic cell transplantation (HCT) is a widely used and potentially curative medical treatment for patients with life-threatening malignant or non-malignant conditions (Henig & Zuckerman, 2014). With appropriate medical and psychological evaluation of a prospective donor, HCT donation is considered a medically safe procedure (Packman, 1999). Today, 26% of pediatric patients undergoing HCT receive stem cells from their sibling due to their genetic match (Packman, 1999; Wiener et al., 2007) and HCT from a fully matched sibling donor often offers the best HCT outcomes (Wiener et al., 2007) Further, 43% of pediatric patients undergoing HCT have a non-malignant disorder, an estimate that has changed over time (Khandelwal et al., 2017).
Pediatric donation can be a potentially lifesaving procedure (Pelletier et al., 2015; Pulsipher et al., 2005) Although safe, HCT donation is an intensive process for pediatric donors with the potential for medical and psychological consequences. These challenges are often compounded by family disruption due to life-threatening illness and medical intervention, as well as the donor recipient’s unpredictable post-HCT clinical course. Some pediatric donors may feel responsible for the success or failure of the HCT, or the complications that may arise (Klippenstein et al., 2021; Packman, 1999).
Extensive work has examined the physical and medical risks of HCT specific to pediatric sibling donors (Macleod et al., 2003). With appropriate donor screening, the medical risks are very small. Less is known about the psychological risks, which are often reported to exceed physical risks of donation (Pelletier et al., 2015). Yet, psychological needs of pediatric sibling donors are often overlooked (Pelletier et al., 2015; Wiener et al., 2007). For example, while pediatric HCT can strengthen family relationships (Packman et al., 2004), pediatric sibling donors are at an increased risk of experiencing anxiety, depression, low self-esteem, moderate post-traumatic stress symptoms, behavioral problems, and feelings of guilt and resentment (Gardner et al., 1977; Hoag et al., 2019; Klippenstein et al., 2021; Macleod et al., 2003; Packman et al., 2004; Wiener et al., 2008). A study interviewing pediatric sibling donors found that negative psychosocial impacts are often concentrated in siblings who: (1) felt they were not fully informed about the donation process and possibility of the recipient’s death; (2) experienced a lack of family and medical support; and (3) internalized their feelings (Macleod et al., 2003; Wiener et al., 2007). It is apparent through this work that HCT can have a significant impact on pediatric sibling donors. Importantly, a recent review of sibling donor experiences in pediatric HCT found that, while distressing, donation also facilitates personal growth, highlighting the potential for positive change after donation (Klippenstein et al., 2021).
Implementation of standardized guidelines is necessary to adequately support pediatric donors throughout the donation process and beyond (Bingen & Hoag, 2016). Pediatric sibling donors in particular have expressed the need for this support (Macleod et al., 2003; Packman et al., 2004; Wiener et al., 2007). To address these concerns, in 2010, the Bioethics Committee of the American Academy of Pediatrics (APP) released recommendations on the eligibility of pediatric donors and a standard of care (Pelletier et al., 2015; Diekema et al., 2010). APP emphasized the need to establish independent donor advocates, including the involvement of the donor in the decision making process, as well as on-going support for the donor and recipient throughout the donation process (Pelletier et al., 2015; Diekema et al., 2010). In 2019, Wiener and colleagues surveyed all North American and European transplant centres for their practices in donor surveillance (Wiener et al., 2019). The authors found that, despite APP’s recommendations, adherence to psychosocial follow-up assessment after donation remains poor (Wiener et al., 2019). To-date, a standardized assessment of pediatric donors does not exist. Without adequate and consistent screening, the needs of pediatric donors often remain unmet.
Current Research
In response to the lack of an established pediatric donor assessment, our team developed a screening program with an assessment protocol to evaluate the psychosocial functioning of pediatric sibling donors over the course of the HCT (Pelletier et al., 2015). The goal of this program is to identify areas of need and in turn offer relevant supports for the youth and family. This protocol is comprised of a comprehensive intake interview, including the sibling donor’s knowledge of the procedure, intentions for donation, coping with the HCT recipient’s illness, the perceived impact of the donation and illness on the sibling donor, and a diagnostic clinical interview guided by the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). A screening of the sibling donor’s health-related quality of life (HRQL) is also conducted as an index of their current psychosocial functioning. This assessment is conducted with the sibling donor independent of their parent(s) with the goal of minimizing bias and possible coercion, unless parent and/or youth preferred otherwise. This protocol was published previously (Pelletier et al., 2015).
The psychosocial screening protocol allows for an assessment of the HRQL of pediatric donors over the course of HCT and beyond. Information collected can offer important insights to the impact of HCT on pediatric donors and whether additional supports are required. The current research was carried out through two objectives described below:
-
1.
To evaluate the HRQL of pediatric donors over time, from T1 to T6, starting at the intake interview to 2 years following donation. Building on past research (Switzer et al., 2016; Zając-Spychała et al., 2020), we hypothesized that the HRQL of pediatric donors would improve over time. We also explored differences in HRQL for malignant compared to non-malignant conditions.
-
2.
To examine facilitators and barriers to implementing a longitudinal psychosocial assessment.
Methods
Study Design
This was a retrospective study design. Pediatric donors participated in the psychosocial assessment as part of a clinical protocol through the Hematology, Oncology, and Transplant Program at the local pediatric tertiary care hospital. Ethics approval was obtained by the local research ethics board for retrospective chart review (HREBA.CC-18–0157).
Pediatric Donors
Pediatric donors completed the psychosocial assessment as part of their clinical care at the pediatric hospital. Participation was consistent with the institution’s protocol for the psychosocial assessment of all pediatric donors. They were eligible to receive the assessment if they: (1) were over the age of 5 years; and (2) donated peripheral blood stem cells or bone marrow to their sibling. Only pediatric donors who could speak English and had no developmental or cognitive delays completed the assessment. It is important to note that youths were not excluded as potential donors based on these criteria.
Between 2013 and 2021, 55 pediatric donors completed the assessment at T1. Four pediatric donors were excluded from follow-up at T2 (2 cases with a recipient deceased before HCT, 1 case with a change in donor, and 1 case where the donor was identified to have cognitive delays). A total of 51 unique pediatric donors were included in the final sample. Of this sample, all were sibling donors with the exception that two youths donated to their parents (two fathers) instead. Further, two youths donated to two recipients at different times, resulting in a total of 53 donations assessed. Descriptive information for pediatric donors is reported in Table 1.
Procedure
When a youth has been identified as a potential donor, they undergo a medical clearance. They also participate in an intake interview with the program’s social worker and/or clinical psychologist to determine their suitability and willingness to donate. As a part of this baseline assessment process, pediatric donors completed a measure of HRQL (T1). They subsequently completed the measure again on the day of their stem cell collection (T2). Approximately one month following donation, pediatric donors returned to the outpatient clinic for a medical exam to ensure that there were no post-donation complications. There, they completed the same measure (T3). After these visits, pediatric donors were then contacted by a clinic coordinator post-donation at 6 months (T4), 1 year (T5), and 2 years later (T6) to complete the measure, which was mailed to them. The mailed package included a letter reiterating the nature of the assessment, instructions for completing the questionnaire, a questionnaire of HRQL, and a postage paid envelope for returning the questionnaire.
Measures
Pediatric Quality of Life Inventory (PedsQL)
HRQL of pediatric donors was assessed using the Pediatric Quality of Life Inventory 4.0 Generic Core Scale (PedsQL; Varni et al., 1999, 2002). This version of the PedsQL is a 23-item self-report questionnaire that measures the HRQL of healthy and ill individuals between 5 and 25 years of age. The PedsQL is comprised four subscales, including: Physical, Emotional, Social, and School Functioning. This measure has been shown to be reliable and valid across a wide range of populations including siblings of children with chronic illness (Switzer PhD et al., 2016). Pediatric donors rated the extent to which they experienced problems in their functioning in the past month, across the different domains (e.g., “It is hard for me to walk more than one block”) using a 4-point scale ranging from 1 (never) to 4 (almost always). Items were totaled to generate scores for each subscale, as well as a combined score reflecting overall HRQL. Scores range from 0 to 100, with higher scores reflecting better functioning.
Demographic Information
Demographic information of pediatric donors was identified through a review of their health records. Information regarding age and sex of pediatric donor, as well as age, sex, and diagnosis of the donor recipient, were collected for this study.
Facilitators and Barriers
We examined completion records by describing the number of pediatric donors that completed the psychosocial assessment across each time point. This served as an index of retention rate over time. Factors that contributed to, or interfered with the retention rate of pediatric donors (i.e., facilitators and barriers) were explored through review and deliberation among the clinical team.
Statistical Analysis
To assess pediatric donor HRQL over time (Aim 1), we conducted a linear mixed-effects model for repeated measures design across six time points (T1 to T6) and grouped by malignant and non-malignant disorders. Age and sex of pediatric donors were included as covariates. Mixed modeling controls for the potential lack of independence between recipient and pediatric donors who come from the same family, and allows for the estimation of least squared means for comparison of factor effects of correlated data. This is a widely used method of assessment for longitudinal HRQL and can handle missing data (Ibrahim & Molenberghs, 2009). Post hoc analyses were conducted using a Bonferroni correction to determine pairwise comparisons based on estimated marginal means. These analyses were conducted in SPSS 27.0 (IBM Corp, 2020).
To identify facilitators and/or barriers to implementing the pediatric donor psychosocial assessment protocol (Aim 2), we computed descriptive statistics (frequencies) to determine completion and retention rates of pediatric donors. We summarized facilitators and barriers to implementation that played a role in participation completion and retention as identified by the clinical team.
Results
Pediatric Donors and Recipient Characteristics
Pediatric donors were on average 10.7 years of age (SD = 3.7) at T1 with 31 males and 21 females. Sibling recipients of HCT (n = 49) were on average 9.1 years of age (SD = 6.1) at T2. Chart review did not reveal demographic characteristics (i.e., age) for parent recipients. Clinical characteristics of all donor recipients included those diagnosed with sickle cell disease (45.3%), leukemia (26.4%), and other diseases (26.4%). Sixteen donor recipients (30.2%) were diagnosed with a malignant disorder and five donor recipients deceased post-donation. For statistical completeness, descriptive statistics of pediatric donors and recipients can be found in Table 2.
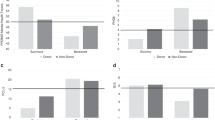
Aim 1: Longitudinal Assessment of HRQL
Descriptive statistics of HRQL are presented in Table 2. A summary of changes in HRQL mean scores over time is displayed in Table 3 and Fig. 1. Results showed that from T1 to T6, HRQL changed significantly in physical functioning (− 10.10 ± 2.77, t = − 3.64, p = 0.01), emotional functioning (− 19.98 ± 5.17, t = − 3.86, p = 0.001), and overall functioning (− 10.54 ± 2.84, t = − 3.72, p = 0.001). These changes in HRQL were not significant for social functioning (− 9.10 ± 4.47, t = − 2.04, p = 0.05) and school functioning (− 6.29 ± 4.77, t = − 1.32, p = 0.20).
Post hoc analysis showed that, for physical functioning, HRQL significantly improved between T1 and T6 (− 10.10 ± 2.77, p = 0.01), and between T2 and T6 (− 12.57 ± 3.40, p = 0.008). For emotional functioning, results showed that HRQL significantly improved from T1 to T4 (− 25.28 ± 5.97, p = 0.006), T1 to T5 (− 24.77 ± 5.67, p = 0.002) and T1 and T6 (− 19.98 ± 5.17, p = 0.008). For social functioning, results determined that HRQL significantly improved from T1 to T5 (− 16.59 ± 3.52, p < 0.001) and from T2 to T5 (− 13.96 ± 3.42, p = 0.002). For school functioning, results revealed that HRQL significantly improved between T1 and T5 (− 17.53 ± 4.56, p = 0.008) and between T2 and T5 (− 19.44 ± 4.97, p = 0.005). Finally, for overall functioning, results showed that HRQL significantly improved between T1 and T5 (− 15.76 ± 3.23, p = 0.09) and T1 and T6 (− 10.54 ± 2.84, p = 0.009). HRQL in overall functioning also improved between T2 and T5 (− 15.30 ± 3.31, p = 0.001) and T2 and T6 (− 10.08 ± 2.97, p = 0.02). Several non-significant trends emerged that are worth noting. A decline in HRQL was observed between T1 and T2 in physical and social functioning. Further, a decline in HRQL was observed between T5 and T6 in all forms of functioning, except for physical functioning.
Results also indicated there were no significant differences between malignancy and non-malignant disorders in changes in HRQL over time (see Table 2).
Aim 2: Facilitators and Barriers to Implementation
Completion rates of pediatric donor assessments over a 2-year period were initially high but declined over time: 78.4% (n = 40) at T2, 47.1% (n = 24) at T3, and 23.5% (n = 12), 25.5% (n = 13), 27.5% (n = 14) at T4, T5, and T6, respectively (see Fig. 2). Only 2 pediatric donors adhered to the entire assessment protocol across all six time points.
Facilitators to pediatric donor retention included the support of a clinic coordinator to organize, track, and initiate contact and mailing with the families. The involvement of the clinical team at T1 and T2 also supported completions, highlighting the utility of integrated clinical care and research (Wiener & Pao, 2012).
A major barrier identified was a lack of resources available to support contact efforts from T3 onwards. No standardized contact strategy existed. Moreover, reliance on mailing limited the clinic coordinator regard their reach to the families. Where possible, the clinical team provided a reminder to the family by telephone or email. This supplementary contact strategy was successful on occasion in terms of improving retention rates. Another barrier to facilitating retention was the delivery format. Questionnaires were implemented in pencil-and-paper format. No alternative formats (e.g., online survey) were available to patients. Moreover, questionnaires were mailed directly to the parents of pediatric donors, interfering with our ability to directly contact pediatric donors. Two families were also missed due to a combination of clinical coordinator error, changes in the data collection process, and changes in staffing, which contributed to the decline in completion rates.
Discussion
Based on a retrospective chart review, we examined the HRQL of pediatric donors across a two-year period to determine the longitudinal impact of HCT on pediatric donors. Results showed that pediatric donors’ HRQL generally improved over time. This change was steady, as significant differences in physical, emotional, and social functioning were found prior to donation and 1 to 2 years after donation with marginal differences observed shortly after donation. This change did not differ for those with malignant or non-malignant conditions. This finding supports our hypotheses and past research showing that, while the donation process is demanding, pediatric donors on the whole resume their functioning and can live well (Macleod et al., 2003). Some variability in domains of functioning was observed, highlighting a possible enduring consequence of HCT on social and school functioning for pediatric donors (Packman et al., 2004). Moreover, this finding likely reflects the complex nature of the HCT that impacts pediatric donors in different ways (Wiener et al., 2007). Overall, these trends align with those found applying a similar longitudinal protocol of psychosocial follow-up. Specifically, Switzer and colleagues found that approximately 20% of pediatric sibling donors experienced poor quality of life over three time points (4 weeks prior to donation, 4 weeks and 1 year after donation; Switzer et al., 2017).
At the time of initial assessment and donation, pediatric donor mean scores appear to be lower than that of the healthy pediatric population (Varni et al., 1999), particularly with respect to emotional functioning (Varni et al., 1999). This finding is in line with prior work showing that, for many pediatric donors, the psychological impact of their HCT donation supersede the physical ones (Wiener et al., 2007). It may be that pediatric donors worry for the health and well-being of their donor recipient as HCT is typically conducted when the recipient has a life-threatening condition. Altogether, the current work reinforces the need to provide psychosocial support to pediatric donors, including sibling donors, leading up to and during HCT, highlighting the critical demand for the establishment of a standardized assessment to reliably examine and intervene in this population.
A novel finding is that the HRQL of pediatric donors was observed trending towards a decline 1- and 2-years post-donation, although it is unclear whether these changes were meaningful as differences were not significant and based on a very small sample. It can be suggested that there may be a possible change that takes place for pediatric donors in the long-term, 1 year after donation and beyond. To discern these changes, it may be informative to consider the influence of pediatric donors and recipients, and their clinical characteristics, on outcomes. While no differences in HRQL were found for those diagnosed with malignant and non-malignant diseases, other challenges may contribute to HRQL, including grief and loss of a sibling passing and post-HCT complications (e.g., graft-versus-host disease). Of note, findings from this study were based on a sample of predominantly sibling donors. The psychosocial impact of HCT may therefore be largely related to the sibling relationship. In fact, there is extensive research exploring the psychosocial well-being of siblings of patients with malignant conditions outside the HCT procedure suggesting the HRQL of siblings may be impacted long-term (Abshire et al., 2017). However, it is possible that this impact is similar for donors to parent recipients when considered as part of the family context. Additional studies are necessary to specify the impact of donation to a parent versus a sibling on pediatric donors. Moreover, other studies comparing the HRQL of related and unrelated adult donors over time (pre-donation to 1-year post-donation) have found that the experience of related donors are unique and warrant tailored support, particularly in their recovery post-donation (Switzer et al., 2020). Future research should thus aim to understand the long-term impact on HRQL for pediatric donors.
Loss of participation was a major issue that contributed to missing data and reflected a potential barrier to the implementation of a long-term assessment protocol for pediatric donors. Multiple factors may contribute to loss of participation over time, including considerations internal to the pediatric donors, such as sociodemographic factors (Gustavson et al., 2012). System-level factors may also contribute to reduced participation such that many families relocate to our treatment centre for the transplant procedure and subsequently return to their home community and health care teams. This process of relocation unfortunately results in the natural loss of contact with many families in their follow-up. Finally, administration of the survey in pencil-and-paper format limited our ability to deliver the survey through other, perhaps more efficient methods (e.g., online). Importantly, some facilitators which can be employed in future efforts were noted. The support of a clinic coordinator to organize, track, and initiate contact and mailing with the families provides a necessary foundation. Research has described the use of a patient-reported outcome coordinator to improve HRQL response rates over time and reported improvements for early time points (Johnston et al., 2015). However, these improvements were not sustained for later data collection points and therefore other strategies should be considered. Finally, the involvement of the clinical team in the contact strategy enhanced retention, highlighting the utility of integrated clinical care and research (Johnston et al., 2015).
Results highlight potential challenges anticipated for pediatric donors well beyond their donation. This work informs future research that may explore the possible mechanisms that may influence changes in the HRQL of pediatric donors, which is necessary to determine how we can best enhance their HRQL in the long-term. Further, by establishing a standard of care (Wiener et al., 2015), this pediatric sibling donor assessment protocol can be implemented to systematically evaluate the psychosocial challenges of pediatric sibling donors in HCT over time to identify areas of need for intervention by the health care team. Priorities for treatment may be determined by evaluating how pediatric sibling donors report they are functioning across all domains of HRQL; for example, intervening in the domain of their lowest reported scores. Practically, it may be important to establish scheduled follow-up for the pediatric donors returning to a different treatment centre post-HCT. This would ensure that the psychological needs of the pediatric sibling donors are not overlooked.
There are limitations to address in future research and clinical practice. Our sample size was small and due to the retrospective nature of this study, sociodemographic variables were not available for review. Additionally, there was notable attrition from T1 to T6, which limits the generalizability of the findings. Based on the current protocol, no information regarding reasons for attrition from participants were gathered. Therefore, interpretation of our findings is therefore limited to the existing study sample. Future, prospective studies that include a larger and clinically diverse sample (e.g., malignant, non-malignant) and sociodemographic information of respondents may help to increase the generalizability of study findings. To further increase generalizability of this work, there is also a need to further evaluate the functioning of individuals with developmental and cognitive delays. Although the majority of the assessment were conducted and completed prior to the onset of the COVID-19 global pandemic, three participants were recruited between 2020 and 2021. Psychosocial outcomes as reported by these participants may be shaped by the impact of COVID-19 and thus warrants consideration when interpretating the data longitudinally. In addition, retention appears to be a major issue in the current approach to long-term follow-up, although this is not unusual for any longitudinal data collection. Using diverse, organized, and consistent contact strategies to reach pediatric donors may help to facilitate completion rates over time (Abshire et al., 2017), identify factors that may interfere with adherence, and minimize major barriers to implementation. For example, migrating the surveys from pencil-and-paper format to an online format or mobile health application (e.g., with push notification features) may help to increase reach to families that are from geographic regions distant from the pediatric hospital and allow for easier completion. Use of translated assessment tools in the preferred language of the family may allow families that are not fluent in English to engage in the assessment, as well as strengthen the cultural responsiveness of our assessment approach. Adhering to a rigorous process to ensure the ease of implementing this protocol will allow us to follow pediatric donors over time and in an accessible and equitable way. Finally, additional studies testing the implementation of this protocol, or facilitating the development of similar programs, in health care centers across North America may help to further establish standardization of care for this unique population in the HCT process.
Conclusion
In this retrospective and longitudinal study, we examined the HRQL of pediatric donors using a standardized protocol established through our program. We observed a steady and significant improvement in their HRQL prior to HCT and 1 to 2 years after donation. Nevertheless, pediatric donors experience poorer HRQL than their same-aged healthy peers (Switzer et al., 2017). We demonstrated the potential utility of implementing a standardized assessment tool to support the unique psychological needs of pediatric HCT pediatric donors. Establishing this standard of care is a critical requisite in supporting HCT pediatric donors in their ability to maximize their quality of life.
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Abshire, M., Dinglas, V. D., Cajita, M. I. A., Eakin, M. N., Needham, D. M., & Himmelfarb, C. D. (2017). Participant retention practices in longitudinal clinical research studies with high retention rates. BMC Medical Research Methodology, 17, 30. https://doi.org/10.1186/s12874-017-0310-z
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Arlington, VA: American Psychiatric Association.
Bingen, K., & Hoag, J. A. (2016). Pediatric hematopoietic stem cell transplantation: psychosocial assessment and care. Pediatric psychosocial oncology: Textbook for multidisciplinary care (pp. 219–242). Cham: Springer International Publishing. https://doi.org/10.1007/978-3-319-21374-3_13
Diekema, D. S., Fallat, M., Matheny Antommaria, A. H., Holzman, I. R., Katz, A. L., Leuthner, S. R., Ross, L. F., Webb, S. A., Baese, P. L., Levetown, M., Lyerly, A. D., Tsai, E., Berg, J. W., & Baker, A. (2010). Policy statement—Children as hematopoietic stem cell donors. Pediatrics, 125(2), 392–404. https://doi.org/10.1542/peds.2009-3078
Gardner, G. G., August, C. S., & Githens, J. (1977). Psychological issues in bone marrow transplantation. Pediatrics, 60, 625–631. https://doi.org/10.1542/peds.60.4.625
Gustavson, K., von Soest, T., Karevold, E., & Røysamb, E. (2012). Attrition and generalizability in longitudinal studies: Findings from a 15-year population-based study and a Monte Carlo simulation study. BMC Public Health, 12, 918. https://doi.org/10.1186/1471-2458-12-918
Henig, I., & Zuckerman, T. (2014). Hematopoietic stem cell transplantation-50 years of evolution and future perspectives. Rambam Maimonides Medical Journal, 5, e0028–e0028. https://doi.org/10.5041/RMMJ.10162
Hoag, J., Igler, E., Karst, J., Bingen, K., & Kupst, M. J. (2019). Decision-making, knowledge, and psychosocial outcomes in pediatric siblings identified to donate hematopoietic stem cells. Journal of Psychosocial Oncology, 37, 367–382. https://doi.org/10.1080/07347332.2018.1489443
IBM Corp. (2020). IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY: IBM Corp.
Ibrahim, J. G., & Molenberghs, G. (2009). Missing data methods in longitudinal studies: A review. Test (madr), 18, 1–43. https://doi.org/10.1007/s11749-009-0138-x
Johnston, D., Gerbing, R., Alonzo, T., Aplenc, R., Nagarajan, R., Schulte, F., Cullen, P., & Sung, L. (2015). Patient-reported outcome coordinator did not improve quality of life assessment response rates: A report from the children’s oncology group. PLoS ONE, 10, e0125290–e0125290. https://doi.org/10.1371/journal.pone.0125290
Khandelwal, P., Millard, H. R., Thiel, E., Abdel-Azim, H., Abraham, A. A., Auletta, J. J., Boulad, F., Brown, V. I., Camitta, B. M., Chan, K. W., Chaudhury, S., Cowan, M. J., Angel-Diaz, M., Gadalla, S. M., Gale, R. P., Hale, G., Kasow, K. A., Keating, A. K., Kitko, C. L., … Mehta, P. A. (2017). Hematopoietic stem cell transplantation activity in pediatric cancer between 2008 and 2014 in the united states: a center for international blood and marrow transplant research report. Biology of Blood and Bone Marrow Transplantation, 23, 1342–1349. https://doi.org/10.1016/j.bbmt.2017.04.018
Klippenstein, A. D. W., Piotrowski, C. C., Winkler, J., & West, C. H. (2021). Growth in the face of overwhelming pressure: A narrative review of sibling donor experiences in pediatric hematopoietic stem cell transplant. Journal of Child Health Care. https://doi.org/10.1177/13674935211043680
Macleod, K. D., Whitsett, S. F., Mash, E. J., & Pelletier, W. (2003). Pediatric sibling donors of successful and unsuccessful hematopoietic stem cell transplants (HSCT): A qualitative study of their psychosocial experience. Journal of Pediatric Psychology, 28, 223–231. https://doi.org/10.1093/jpepsy/jsg010
Packman, W. L. (1999). Psychosocial impact of pediatric BMT on siblings. Bone Marrow Transplantation, 24, 701–706. https://doi.org/10.1038/sj.bmt.1701997
Packman, W., Gong, K., VanZutphen, K., Shaffer, T., & Crittenden, M. (2004). Psychosocial adjustment of adolescent siblings of hematopoietic stem cell transplant patients. Journal of Pediatric Oncology Nursing, 21, 233–248. https://doi.org/10.1177/1043454203262698
Pelletier, W., Schulte, F., & Guilcher, G. M. T. (2015). Pediatric hematopoietic stem cell donors: Need for longitudinal medical and psychosocial surveillance. Pediatric Blood & Cancer, 62(5), 737–738.
Pulsipher, M. A., Levine, J. E., Hayashi, R. J., Chan, K. W., Anderson, P., Duerst, R., Osunkwo, I., Fisher, V., Hom, B., & Grupp, S. A. (2005). Safety and efficacy of allogeneic PBSC collection in normal pediatric donors: The pediatric blood and marrow transplant consortium experience (PBMTC) 1996–2003. Bone Marrow Transplantation, 35, 361–367. https://doi.org/10.1038/sj.bmt.1704743
Switzer, G. E., Bruce, J. G., Kiefer, D. M., Kobusingye, H., Abebe, K. Z., Drexler, R., Besser, R. M., Confer, D. L., Horowitz, M. M., King, R. J., Shaw, B. E., Riches, M., Hayes-Lattin, B., Linenberger, M., Bolwell, B., Rowley, S. D., Litzow, M. R., & Pulsipher, M. A. (2020). Health-related quality-of-life comparison of adult related and unrelated HSC donors: An RDSafe study. Biology of Blood and Bone Marrow Transplantation, 26, 2365–2371. https://doi.org/10.1016/j.bbmt.2020.08.016
Switzer, G. E., Bruce, J., Kiefer, D. M., Kobusingye, H., Drexler, A. A. S. R., Besser, R. M., Confer, D. L., Horowitz, M. M., King, R. J., Shaw, B. E., van Walraven, S. M., Wiener, L., Packman, J. D. W., Varni, J. W., & Pulsipher, M. A. (2016). Health-related quality of life among pediatric hematopoietic stem cell donors. Journal of Pediatrics, 178, 164-170.e1. https://doi.org/10.1016/j.jpeds.2016.07.009
Switzer, G. E., Bruce, J., Pastorek, G., Kiefer, D. M., Kobusingye, H., Drexler, R., Besser, R. A. M., Confer, D. L., Horowitz, M. M., King, R. J., Shaw, B. E., van Walraven, S. M., Wiener, L., Packman, W., Varni, J. W., & Pulsipher, M. A. (2017). Parent versus child donor perceptions of the bone marrow donation experience. Bone Marrow Transplantation, 52, 1338–1341. https://doi.org/10.1038/bmt.2017.124
Varni, J. W., Seid, M., Knight, T. S., Uzark, K., & Szer, I. S. (2002). The PedsQLTM 4.0 generic core scales: sensitivity, responsiveness, and impact on clinical decision-making. Journal of Behavioral Medicine, 25, 175–193. https://doi.org/10.1023/A:1014836921812
Varni, J. W., Seid, M., & Rode, C. A. (1999). The pedsql™: measurement model for the pediatric quality of life inventory. Medical Care, 37, 126–139. https://doi.org/10.1097/00005650-199902000-00003
Wiener, L., & Pao, M. (2012). Comprehensive and family-centered psychosocial care in pediatric oncology integration of clinical practice and research (pp. 7–17). Chichester, UK: Wiley Ltd. https://doi.org/10.1002/9781119941033.ch2
Wiener, L., Hoag, J. A., Pelletier, W., Shah, N. N., Shaw, B. E., Pulsipher, M. A., Bruce, J., Bader, P., Willasch, A. M., Dalissier, A., Guilcher, G., Anthias, C., Confer, D. L., Sees, J. A., Logan, B., & Switzer, G. E. (2019). Transplant center practices for psychosocial assessment and management of pediatric hematopoietic stem cell donors. Bone Marrow Transplantation, 54, 1780–1788. https://doi.org/10.1038/s41409-019-0515-3
Wiener, L., Kazak, A. E., Noll, R. B., Patenaude, A. F., & Kupst, M. J. (2015). Standards for the psychosocial care of children with cancer and their families an introduction to the special issue. Pediatric Blood & Cancer, 62, 419–424. https://doi.org/10.1002/pbc.25675
Wiener, L. S., Steffen-Smith, E., Battles, H. B., Wayne, A., Love, C. P., & Fry, T. (2008). Sibling stem cell donor experiences at a single institution. Psycho-Oncology, 17, 304–307. https://doi.org/10.1002/pon.1222
Wiener, L. S., Steffen-Smith, E., Fry, T., & Wayne, A. (2007). Hematopoeitic stem cell donation in children: a review of the sibling donor experience. Journal of Psychosocial Oncology, 25, 45–66.
Zając-Spychała, O., Pieczonka, A., Barańska, M., & Wachowiak, J. (2020). Long-term recipient health-related quality of life and donor-recipient relationship following sibling pediatric hematopoietic stem cell transplantation. Biology of Blood and Bone Marrow Transplantation, 26, 401–406. https://doi.org/10.1016/j.bbmt.2019.10.009
Funding
SHJH is supported by the Cumming School of Medicine Postdoctoral Scholarship, and the Arnie Charbonneau Cancer Institute. FSMS is supported by Alberta Children’s Hospital Research Institute, Arnie Charbonneau Cancer Institute, and the Button Family Initiative.
Author information
Authors and Affiliations
Contributions
FSMS initiated and contributed to study conceptualization, methodology, implementation of assessment protocol, formal analysis, writing, including the preparing the original draft and reviewing and editing the manuscript. WP contributed to study conceptualization, methodology, implementation of assessment protocol, and writing, including reviewing and editing the manuscript. GMTG contributed to study conceptualization, methodology, writing, including reviewing and editing. SHJH contributed to data synthesis, formal analysis, writing, including writing the original draft, and reviewing and editing. MYS contributed to data synthesis, formal analysis, writing, including reviewing and editing. MS contributed to data collection and synthesis, writing, including reviewing and editing. HZ contributed to data synthesis, writing, including reviewing and editing. MK contributed to implementation of assessment protocol, writing, including reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interest
Sharon H.J. Hou, Mehak Stokoe, Hailey Zwicker, Morgan Young-Speirs, Wendy Pelletier, Gregory M.T. Guilcher, Melanie Khu and Fiona S.M. Schulte declare that they have no conflict of interest
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. This study was approved by the Institutional Review Board as a retrospective review. The Institutional Review Board approved the waiver of informed consent (HREBA.CC-18–0157).
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hou, S.H.J., Stokoe, M., Zwicker, H. et al. Pediatric Hematopoietic Cell Transplantation: A Longitudinal Assessment of Health-Related Quality of Life of Pediatric Donors. J Clin Psychol Med Settings 30, 836–845 (2023). https://doi.org/10.1007/s10880-022-09933-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-022-09933-1