Abstract
Positive end-expiratory pressure (PEEP) can be titrated by electrical impedance tomography (EIT). The aim of the present study was to examine the performance of different EIT measures during PEEP trials with the aim of identifying “optimum” PEEP and to provide possible interpretations of largely diverging results. After recruitment (maximum plateau pressure 35 cmH2O), decremental PEEP trial with steps of 2 cmH2O and duration of 2 min per step was performed. Ventilation gain and loss, the global inhomogeneity (GI) index, trend of end-expiratory lung impedance (EELI) and regional compliance (Creg) for estimation of overdistension and collapse were calculated. Largely diverging results of PEEP selection among the measures were defined as differences ≥ 4 PEEP steps (i.e. ≥ 8 cmH2O). In 30 ARDS patients we examined so far, 3 patients showed significant differences in PEEP selections. Overdistension and collapse estimation based on Creg tended to select lower PEEP while the GI index and EELI trend suggested higher PEEP settings. Regional inspiration times were heterogeneous indicating that the assumption of a uniform driving pressure in the calculation of Creg may not be valid. Judging by the predominant ventilation distribution in the most dependent regions, these patients were non-recruitable with the applied recruitment method or pressure levels. The existence of differences in the recommended PEEP among the analyzed EIT measures might be an indicator of non-recruitable lungs and heterogeneous airway resistances. In these extreme cases, the largely diverging results may prompt the attending clinician to develop individual ventilation strategies.
Clinical Trial Registration Registration number NCT03112512, https://clinicaltrials.gov/ Registered 13 April 2017.
Similar content being viewed by others
1 Background
Titration of positive end-expiratory pressure (PEEP) is important for patients under mechanical ventilation to prevent the alveoli from collapse [1]. Optimal PEEP level is still controversial since the introduction of PEEP may influence the lung volume, ventilation distribution, as well as cardiac output. An optimal PEEP level should be selected in such a way that it balances alveolar recruitment against overdistention and at the same time it does not impair the hemodynamics. Computed tomography as the gold standard for lung volume imaging cannot be used in this indication due to radiation exposure in a non-dynamic diagnostic fashion. Many bedside approaches to titrate PEEP have been proposed, including measures of lung mechanics [2] or oxygenation [3]. All of these measures allow only global assessment and do not take regional pulmonary heterogeneity into account. As atelectasis and overdistension may simultaneously occur at the same PEEP levels, regional information is warranted.
Electrical impedance tomography (EIT) is a non-invasive imaging technique that allows individual, real-time, bedside imaging of the lungs [4]. Recent studies highlighted the potential use of EIT in PEEP titration [5,6,7,8,9,10]. Many EIT-based measures have been proposed to guide PEEP titration [11]. Ventilation gain and loss [5, 6], the global inhomogeneity (GI) index [12, 13], trend of end-expiratory lung impedance (EELI) [14, 15] and overdistension and collapse estimation with regional compliance (Creg) [16, 17] are the most widely used measures. In a recent prospective study, we found that PEEP titration based on EIT measures improved oxygenation, compliance, driving pressure, and weaning success rate [18]. Although these measures evaluate different aspects of ventilation distribution, in most of the cases, the selection of optimal PEEP based on these measures does not differ very much [19]. Nevertheless, we observed that in some patients, the “optimum” values of PEEP selected from different EIT measures differ.
The aim of the present study was to examine when and why the EIT-derived measures differed from each other. We evaluated offline four different commonly used EIT-derived measures and compared the PEEP selected correspondingly.
2 Methods
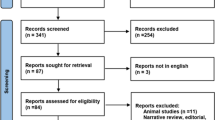
The study was approved by the FEMH Ethics Committee in Taiwan (FEMH-105117-E). The present study involves data from our ongoing registry for EIT-guided PEEP titration (clinical trial registration number NCT03112512, https://clinicaltrials.gov/, registered on the 13th of April 2017). Written informed consent was obtained from all patients or their legal representatives prior to the study.
Moderate to severe acute respiratory distress syndrome (ARDS) patients (diagnosed according to the Berlin definition [20]) were randomized to the EIT group and examined (arterial oxygen partial pressure to fractional inspired oxygen ratio, PaO2/FiO2 < 200 mmHg). Exclusion criteria were the presence of spontaneous breathing, unstable hemodynamics, confirmed or suspected intracranial hypertension, refractory shock, pneumothorax and total ICU stay less than 3 days. Additional exclusion criteria related to the EIT application were age < 18 years, pregnancy and lactation period, and any contraindication to the use of EIT (i.e., pacemaker, automatic implantable cardioverter defibrillator, and implantable pumps).
An EIT electrode belt with 16 electrodes and a width of 40 mm was placed around the thorax in the fifth intercostal space, and one reference electrode was placed at the patients’ abdomen (PulmoVista 500, Dräger Medical, Lübeck, Germany). EIT images were continuously recorded at 20 Hz and stored. Respiratory data from the ventilator were transferred to the EIT device via MEDIBUS connection. The EIT data were reconstructed with the baseline referring to the lowest impedance value measured before PEEP titration started. The data were filtered using a Butterworth 4th degree low-pass filter with a cut-off frequency of 50/min to eliminate impedance changes synchronous with the heart beat.
An incremental PEEP trial was performed starting at a pressure of 5–8 cmH2O with steps of 2 cmH2O till the plateau pressure reached 35 cmH2O for 2 min or unstable blood pressure was observed [21]. Haemodynamic was monitored with IntelliVue MX800 (Philips Medizin Systeme Böblingen GmbH, Böblingen, Germany). In case of blood pressure decrease, a bolus of 500-1000 ml normal saline would be administrated. Dopamine or norepinephrine would be administrated or the recruitment maneuver terminated if the blood pressure was further decreasing. Then a decremental PEEP trial with steps of 2 cmH2O and duration of 2 min per step followed. EIT data analyses were performed offline with MATLAB7.2 (The MathWorks Inc., Natick, USA). Ventilation distribution was quantified by subtracting the end-expiration from the end-inspiration image, which represents the variation during tidal breathing [22]. Resulting tidal images of ten consecutive breaths at the end of each PEEP step were averaged to increase the signal-to-noise ratio. The averaged image is denoted as tidal variation (TV) at the respective PEEP level. In order to indentify the lung regions, TV from all the PEEP steps were combined. Pixels from the combined image with values higher than 20% of the maximum pixel value were defined as lung regions [23]. Therefore, for every PEEP step, the same lung regions were used. Four EIT measures listed below were calculated to assess the PEEP effects on ventilation.
2.1 Differences in TV
TV was normalized with tidal volume given by the ventilator in milliliters. The normalized TV at each PEEP step was subtracted from the normalized TV of the next PEEP step (ΔTV). Consequently, the calculated ΔTV images depicted consecutive regional changes in tidal volume at each PEEP reduction. Regional positive values described the volume gain and negative values its loss within the pulmonary cross-section.
The GI index: this index indicated the degree of homogeneity of ventilation distribution and was calculated according to the following formula [24]:
where DI denotes the value of the differential impedance in the TV images; DIxy is the pixel in the identified lung area; DIlung are all pixels in the lung area under observation. An optimal PEEP should have the lowest GI.
Trend in the EELI levels: end-expiratory impedance values were calculated for every breath. The starting EELI level at each PEEP level was defined as the second breath of each PEEP. If the EELI values of the rest of the breaths at the same PEEP were significantly lower compared to the starting one (confirmed by one-tailed Student’s t test), then we considered this to indicate a loss of end-expiratory lung volume [25]. The PEEP prior to this one was considered “optimal”.
Overdistension and collapse estimation: with the assumption of a uniform driving pressure within the lungs, Creg was estimated by pixel-wise dividing impedance changes in the lung regions with driving pressure given by the ventilator. Then, cumulated overdistension and collapse percentages were estimated based on the decrease of Creg curve during decremental PEEP titration, either towards higher or lower PEEP levels [16]. The overdistension defined by the regional compliance method assumed that the Creg change would first increase along decremental PEEP. After reaching to its maximum, the Creg would decrease. The regions were defined as overdistended at PEEP levels before reaching the maximum compliance. Similar idea applies for collapse estimation. The best compromise was defined with the lowest sum of collapse and overdistension percentages.
Based on the last three described parameters “optimum” PEEP levels were determined. Extremely large differences among the measures were defined as representing equal or more than 4 PEEP steps (i.e., ≥ 8 cmH2O).
Further, we calculated the inspiration time of each pixel in the lung regions to evaluate the possible heterogeneity of airway resistance [22]. The EIT images were divided into four anteroposterior segments of equal height and denoted as ROI1, ROI2, ROI3 and ROI4, from anterior to posterior, respectively. Percentages of ventilation and volume distributions were calculated in each ROI.
2.2 Statistical analysis
The normality of data was confirmed with Lilliefors test and the data are presented as means and standard deviations. The differences in PEEP selection among various EIT-based methods were compared with one-way analysis of variance using MATLAB. A p value < 0.05 was considered statistically significant. Since the patients were not prospectively recruited for the present study, no sample size analysis was performed. Power analysis was not performed due to the nature of the study design.
3 Results
In total 30 moderate to severe ARDS patients were assigned to the EIT group till October 2018 (age 55.8 ± 15.7 years; 8:22 female:male; height 164.6 ± 7.5 cm; weight 63.5 ± 10.1 kg; APACHE II 26.1 ± 7.3; PaO2/FiO2 108.8 ± 34.1 mmHg; mean ± SD). Among these patients, 3 patients showed significant differences in PEEP selection with EIT measures (for demographics of these 3 patients and baseline parameters please refer to Table 1). Figure 1 shows the box plot comparing PEEP selections with different EIT methods (3 patients who exhibited difference ≥ 8 cmH2O were excluded). The differences among various methods were not significant (p > 0.05).
Box plots comparing PEEP selection with various methods in 27 studied ARDS patients (three patients who had differences > 8 cmH2O were not included in this diagram). Left: the end-expiratory lung impedance (EELI) trend; middle: the global inhomogeneity (GI) index; right: overdistension and collapse estimation based on regional respiratory system compliance. The boxes mark the quartiles; the whiskers extend from the box out to the most extreme data values within 1.59 of the interquartile range of the sample; the red + represent possible outliers
Figure 2 shows the comparison with largely diverging results among the EIT measures in one example patient. Ventilation gain occurred mainly in the gravity-dependent regions at higher PEEP levels compared to lower levels (Fig. 2, top, blue regions), while ventilation loss occurred in the non-dependent regions (Fig. 2, top, orange regions). Even at PEEP as high as 26 cmH2O, tidal ventilation increased in the dependent regions compared to PEEP of 24 cmH2O (please note that demonstration of the differences in tidal variation were higher minus lower PEEP levels). EELI trend indicated that end-expiratory lung volume (EELV) already started to decrease at PEEP of 22 cmH2O (Fig. 2, green dashed lines). The GI index reached the lowest value at the highest PEEP level (red circle) and the best compromise between overdistension and collapse based on Creg was found at 16 cmH2O (Fig. 2 bottom). Although ventilation loss occurred at low PEEP levels (e.g. 10, 8, 6 cm H2O), estimated overdistension was 0% at those PEEP levels.
Comparison of the EIT measures in patient 1. Top: differences in tidal variation (ΔTV) images. TV at higher PEEP steps were subtracted from the next lower PEEP steps (i.e., PEEP 26–24, 24–22, 22–20 cmH2O, etc.). Blue regions correspond to volume gain and orange regions to volume loss. Same scale is used for all these differential images. Middle: the global inhomogeneity (GI) index (red circles) represent the degree of ventilation distribution inhomogeneity and horizontal dashed lines mark the EELI values at the beginning of individual PEEP levels. Bottom: overdistension (stars) and collapse (triangles) estimation based on regional respiratory system compliance. Global impedance curves were rescaled and in arbitrary unit. Please note that demonstration of ΔTV were higher minus lower PEEP levels
In Fig. 3, comparisons are shown for ΔTV between PEEP 10 and 8 and between 12 and 10 cmH2O (Fig. 3 left). Further, ΔCreg between those PEEP levels (Fig. 3 middle), and inspiration time maps at PEEP 8 and 12 cmH2O (Fig. 3 right) are presented. Tidal volume loss and gain had a clear gravity-dependent pattern. However, only ΔCreg between PEEP 12 and 10 showed a similar pattern. Creg was higher at PEEP 10 (red regions, top middle image), even for regions with ventilation loss (orange regions, top left image). Inspiration time maps indicated that the inspiration time was very different among pixels at PEEP of 8 cmH2O (top right), while at PEEP of 12 cmH2O, the regional inspiration time was more homogeneous (bottom right). Coefficient of variation was 29.8% for regional inspiration time at PEEP of 8 cmH2O and 11.5% at PEEP of 12 cmH2O.
Comparisons among tidal volume distribution differences (ΔTV) (left), regional compliance differences (ΔCreg) (middle), and inspiration time maps (right) of patient 1. Left: differences between PEEP 10 and 8 cmH2O (top), as well as between PEEP 12 and 10 cmH2O (bottom) are shown. Impedance changes were normalized to global tidal volume in milliliters. Regions with tidal volume loss and gain were denoted with orange and light blue colors, respectively. Middle: differences between PEEP 10 and 8 cmH2O (top), as well as between PEEP 12 and 10 cmH2O (bottom). Regions with compliance increase and decrease were denoted with red and blue colors, respectively. Right: inspiration time in seconds at PEEP of 8 cmH2O (top) and 12 cmH2O (bottom)
Creg changes along with decremental PEEP in the most non-dependent lung regions are plotted in Fig. 4. Global as well as local maxima were observed in some lung regions (thick lines). (Similar curves were found in other lung regions, which are not plotted in this figure for clarity.)
TV in ROI4 changed from 5.5 to 4.0% during PEEP titration (from the highest PEEP 26 cmH2O to the lowest PEEP 6 cmH2O, respectively). Ventilation distributions in ROI4 were low throughout the whole PEEP titration process.
Like in patient 1, also in the other 2 patients exhibiting large difference among determined “optimum” PEEP, ventilation gain occurred mainly in the gravity-dependent regions, while ventilation loss occurred in the non-dependent regions. EELI trend indicated that EELV already started to decrease at PEEP of 20 cmH2O. The GI index reached the lowest value at PEEP of 20 cmH2O (patient 2) or 22 cmH2O (patient 3). The best compromise between overdistension and collapse based on Creg was found at 10 cmH2O. TV in ROI4 changed from 9.5 to 5.4% in patient 2 and from 5.7 to 3.4% in patient 3 (highest to lowest PEEP, respectively). The results regarding overdistension and collapse based on Creg were strongly dependent on the starting and ending values of PEEP steps (Fig. 5). If the PEEP titration ended at PEEP of 14 cmH2O, the “optimal” PEEP would be 16 cmH2O (Fig. 5 middle). If the titration started at PEEP of 14 cmH2O, the “optimal” PEEP would be 12 cmH2O (Fig. 5 bottom). The lung fraction percentages of overdistension and collapse were also different at the same PEEP, depending on the starting and ending values of the PEEP titration process.
The lung fraction percentages of overdistension and collapse based on regional respiratory system compliance may be different, depending on the starting and ending PEEP values (patient 2 for example). Top: PEEP titration from 22 to 6 cmH2O with “optimal” PEEP of 10 cmH2O (green arrow). Middle: PEEP titration from 22 to 14 cmH2O with “optimal” PEEP of 16 cmH2O. Bottom: PEEP titration from 14 to 6 cmH2O with “optimal” PEEP of 12 cmH2O. Global impedance curves were rescaled and in arbitrary unit
4 Discussion
In the present study, we examined several EIT-based PEEP titration measures in 30 moderate to severe ARDS patients. In most of the cases (90%) the PEEP values rendered by the different EIT measures were not significantly different. In 3 extreme cases, the differences in optimal PEEP selection among these measures were larger than 4 PEEP steps (8 cmH2O). We have further investigated other EIT-derived measures to figure out two questions: why this happened and how should we interpret the results, namely, how to exploit this information for an adequate PEEP setting.
4.1 Why this happened?
EIT data contain spatial and temporal information that help the user understand the lung status from different angles (e.g. [26, 27]). Four EIT measures compared in the present study captured different aspects, which were not completely independent. ΔTV visualizes the ventilation gain and loss, while the GI index quantifies the ventilation distribution. Trend in EELI directly reflects the changes in EELV, which is correlated to recruitment/derecruitment. Derecruited regions correspond to ventilation loss. Overdistension and collapse estimation based on Creg capture similar information as ΔTV, but it includes the information on driving pressure as well. Therefore, in most cases, these measures proposed similar “optimal” PEEP settings. Since various EIT measures reflect various physiological phenomena, when the “optimal PEEP” levels selected by these EIT measures were the same, this selected PEEP could be the ideal one in respect to these physiological phenomena.
In the extreme cases we observed, overdistension and collapse estimation based on Creg tended to select lower PEEP while the GI index and the EELI trend suggested higher PEEP settings to be optimal (e.g. Fig. 2). The EELI trend might be misleading during a decremental PEEP with fast steps of only a few minutes duration. There would not be enough time to reach a constant EELV level. If overdistension and collapse estimation based on Creg is applied, it is assumed that the driving pressure is the same over the lung regions and that the Creg curves have single global maximum. Ideally at the end of inspiration and expiration under pressure control ventilation mode, flow within the lung should be zero and thus the driving pressure the same in all lung regions. In Fig. 3 however, it can be observed that Creg was higher at PEEP 10 compared to PEEP 8, even for regions with ventilation loss, which cannot be explained if the Creg calculation was correct. It was confirmed that the regional inspiration time was very heterogeneous in this patient, which indicated that airway resistances and driving pressure were probably heterogeneous as well. Intrinsic PEEP might be a reason for heterogeneous driving pressure within the lung, which was not assessed in the present study. Creg of a pixel may be a mixture of compliances from much smaller regions, which might explain why local maxima could be observed in some pixels (Fig. 4). This is also the reason why the results of overdistension and collapse estimation were so sensitive to the starting and ending values of PEEP during the decremental PEEP trial in certain cases (e.g. Fig. 5). It is less likely that a decremental PEEP trial would stop at high PEEP of 14 cmH2O but our example demonstrated the possible bias in the application of this measure. We suspected that when no global maximum of Creg is reached during a PEEP-trial, then the calculations of optimal settings are hampered.
Ventilation distribution in ROI4 did not change much (in average from 6.9 to 4.3%), which indicated that only a small portion of lung regions in the most dependent regions collapsed during PEEP titration. On the other hand, the low percentage of ventilation distribution also suggested that even at the highest PEEP level, lung regions in ROI4 were not recruited. These patients might be classified as non-recruitable with the described recruitment method and/or the used pressure levels. It would be interesting to see how much EELI changed in ROI4 during PEEP changes, which could be another indicator of recruitment. However, due to the abovementioned reasons EELI changed during a short PEEP step might not be reliable. Due to the volume gain at high PEEP levels and not significant volume loss at the same time (e.g. Fig. 2), the GI index was low at high PEEP levels. The main issue related to the GI index is the lung region identification. In non-recruitable patients, the lung region estimations were incorrect, which led to inaccurate GI values. The “optimal” PEEP levels proposed by the GI index or EELI trends were higher than commonly used levels, which would normally not be considered by the attending physicians.
4.2 How to interpret the results and set the PEEP subsequently?
We suspected that the occasional differences in optimum PEEP values derived from EIT measures and presented in three patients in this paper could be a good indicator of non-recruitable lungs and heterogeneous airway resistances. Further studies need to be conducted to examine this hypothesis. There are other EIT measures that may provide information for individual PEEP titration as well, e.g. silent spaces, which are defined as hypoventilated areas showing impedance changes < 10% of the maximal impedance change within predefined lung areas [28]. Unlike GI index and Creg, which cover both overdistension and collapsed regions, silent spaces focus on evaluating lung recruitability. Considering the way how these EIT measures assess hypoventilated areas, the weighted (scaling) factors are different. The hypoventilated areas were compared to median value of impedance change in the GI calculation, while in the Creg calculation, they were weighted to driving pressure. For the silent spaces, they were compared to the maximum of impedance change. A recent survey indicated that the GI index and silent spaces are two highly rated EIT measures [29]. The calculation of both GI index and silent spaces required lung regions identification. The lung regions used in the Spadaro study were based on CT scans derived from a database of patients with different chest circumferences and matched to the test subjects. If individual CT images are used for reconstruction (whenever available), the correlation between silent space and pressure–volume curves might be improved (r2 reported was 0.54 [28]).
Heterogeneities may be present in the lungs outside the measurement plane, which are not fully covered by EIT [30]. This effect may potentially impact the findings regarding the identification of the “optimum” PEEP. Nevertheless, we suggest combining these EIT-based measures to guide PEEP titrations. As we previously discussed, these measures capture information of the respiratory system from different aspects. Should the suggested PEEP be similar, we are confident in the optimal PEEP level. Should the suggested PEEP be very different as presented in the three cases in this study, we might increase the pressure during the recruitment procedure within an acceptable range and closely monitor the ventilation redistribution in the most dependent regions [8], as well as cardiopulmonary functions. A weighted combination of different EIT measures might be a good way to titrate PEEP as well, which was not possible to be explored with the current patient data. Alternatively, clinicians might choose other options (e.g. prone position) when they consider the patient as non-recruitable [31].
5 Conclusions
“Optimal” PEEP selected by various EIT-based measures may significantly differ in some ARDS patients (~ 10%). The existence of differences among the analyzed EIT measures and the recommended “optimum” PEEP selection might be an indicator of non-recruitable lungs and heterogeneous airway resistances.
Availability of data and material
The data and material are available upon reasonable request.
Abbreviations
- APACHE:
-
Acute physiology and chronic health evaluation
- ARDS:
-
Acute respiratory distress syndrome
- Creg:
-
Regional respiratory system compliance
- EELI:
-
End-expiratory lung impedance
- EIT:
-
Electrical impedance tomography
- FiO2:
-
Fractional inspired oxygen
- ICU:
-
Intensive care unit
- PaO2:
-
Arterial oxygen partial pressure
- PEEP:
-
Positive end-expiratory pressure
- ROI:
-
Region of interest
- TV:
-
Tidal variation
References
Hess DR. Recruitment maneuvers and PEEP titration. Respir Care. 2015;60:1688–704.
Suarez-Sipmann F, Bohm SH, Tusman G, Pesch T, Thamm O, Reissmann H, Reske A, Magnusson A, Hedenstierna G. Use of dynamic compliance for open lung positive end-expiratory pressure titration in an experimental study. Crit Care Med. 2007;35:214–21.
Toth I, Leiner T, Mikor A, Szakmany T, Bogar L, Molnar Z. Hemodynamic and respiratory changes during lung recruitment and descending optimal positive end-expiratory pressure titration in patients with acute respiratory distress syndrome. Crit Care Med. 2007;35:787–93.
Gong B, Krueger-Ziolek S, Moeller K, Schullcke B, Zhao Z. Electrical impedance tomography: functional lung imaging on its way to clinical practice? Expert Rev Respir Med. 2015;9:721–37.
Luepschen H, Meier T, Grossherr M, Leibecke T, Karsten J, Leonhardt S. Protective ventilation using electrical impedance tomography. Physiol Meas. 2007;28:S247–60.
Meier T, Luepschen H, Karsten J, Leibecke T, Grossherr M, Gehring H, Leonhardt S. Assessment of regional lung recruitment and derecruitment during a PEEP trial based on electrical impedance tomography. Intensive Care Med. 2008;34:543–50.
Dargaville PA, Rimensberger PC, Frerichs I. Regional tidal ventilation and compliance during a stepwise vital capacity manoeuvre. Intensive Care Med. 2010;36:1953–61.
Wolf GK, Gomez-Laberge C, Rettig JS, Vargas SO, Smallwood CD, Prabhu SP, Vitali SH, Zurakowski D, Arnold JH. Mechanical ventilation guided by electrical impedance tomography in experimental acute lung injury. Crit Care Med. 2013;41:1296–304.
Liu S, Tan L, Moller K, Frerichs I, Yu T, Liu L, Huang Y, Guo F, Xu J, Yang Y, et al. Identification of regional overdistension, recruitment and cyclic alveolar collapse with electrical impedance tomography in an experimental ARDS model. Crit Care. 2016;20:119.
Franchineau G, Brechot N, Lebreton G, Hekimian G, Nieszkowska A, Trouillet JL, Leprince P, Chastre J, Luyt CE, Combes A, et al. Bedside contribution of electrical impedance tomography to set positive end-expiratory pressure for ECMO-treated severe ARDS patients. Am J Respir Crit Care Med. 2017;196:447–57.
Frerichs I, Amato MB, van Kaam AH, Tingay DG, Zhao Z, Grychtol B, Bodenstein M, Gagnon H, Bohm SH, Teschner E, et al. Chest electrical impedance tomography examination, data analysis, terminology, clinical use and recommendations: consensus statement of the TRanslational EIT developmeNt stuDy group. Thorax. 2017;72:83–93.
Zhao Z, Steinmann D, Frerichs I, Guttmann J, Möller K. PEEP titration guided by ventilation homogeneity: a feasibility study using electrical impedance tomography. Crit Care. 2010;14:R8.
Hochhausen N, Biener I, Rossaint R, Follmann A, Bleilevens C, Braunschweig T, Leonhardt S, Czaplik M. Optimizing PEEP by electrical impedance tomography in a porcine animal model of ARDS. Respir Care. 2017;62:340–9.
Erlandsson K, Odenstedt H, Lundin S, Stenqvist O. Positive end-expiratory pressure optimization using electric impedance tomography in morbidly obese patients during laparoscopic gastric bypass surgery. Acta Anaesthesiol Scand. 2006;50:833–9.
Eronia N, Mauri T, Maffezzini E, Gatti S, Bronco A, Alban L, Binda F, Sasso T, Marenghi C, Grasselli G, et al. Bedside selection of positive end-expiratory pressure by electrical impedance tomography in hypoxemic patients: a feasibility study. Ann Intensive Care. 2017;7:76.
Costa EL, Borges JB, Melo A, Suarez-Sipmann F, Toufen C Jr, Bohm SH, Amato MB. Bedside estimation of recruitable alveolar collapse and hyperdistension by electrical impedance tomography. Intensive Care Med. 2009;35:1132–7.
Heines SJH, Strauch U, van de Poll MCG, Roekaerts P, Bergmans D. Clinical implementation of electric impedance tomography in the treatment of ARDS: a single centre experience. J Clin Monit Comput. 2018;33:291–300.
Zhao Z, Chang MY, Gow CH, Zhang JH, Hsu YL, Frerichs I, Chang HT, Moller K. Positive end-expiratory pressure titration with electrical impedance tomography and pressure-volume curve in severe acute respiratory distress syndrome. Ann Intensive Care. 2019;9:7.
Blankman P, Hasan D, Erik G, Gommers D. Detection of ‘best’ positive end-expiratory pressure derived from electrical impedance tomography parameters during a decremental positive end-expiratory pressure trial. Crit Care. 2014;18:R95.
Definition Task Force ARDS, Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Santos CL, Samary Cdos S, Fiorio Junior PL, Santos BL, Schanaider A. Pulmonar recruitment in acute respiratory distress syndrome. What is the best strategy? Rev Col Bras Cir. 2015;42:125–9.
Zhao Z, Yun PJ, Kuo YL, Fu F, Dai M, Frerichs I, Moller K. Comparison of different functional EIT approaches to quantify tidal ventilation distribution. Physiol Meas. 2018;39:01NT01.
Pulletz S, van Genderingen HR, Schmitz G, Zick G, Schadler D, Scholz J, Weiler N, Frerichs I. Comparison of different methods to define regions of interest for evaluation of regional lung ventilation by EIT. Physiol Meas. 2006;27:S115–27.
Zhao Z, Möller K, Steinmann D, Frerichs I, Guttmann J. Evaluation of an electrical impedance tomography-based global inhomogeneity index for pulmonary ventilation distribution. Intensive Care Med. 2009;35:1900–6.
Hinz J, Hahn G, Neumann P, Sydow M, Mohrenweiser P, Hellige G, Burchardi H. End-expiratory lung impedance change enables bedside monitoring of end-expiratory lung volume change. Intensive Care Med. 2003;29:37–43.
Vogt B, Pulletz S, Elke G, Zhao Z, Zabel P, Weiler N, Frerichs I. Spatial and temporal heterogeneity of regional lung ventilation determined by electrical impedance tomography during pulmonary function testing. J Appl Physiol. 2012;113:1154–61.
Hsu YL, Tien AJ, Chang MY, Chang HT, Moller K, Frerichs I, Zhao Z. Regional ventilation redistribution measured by electrical impedance tomography during spontaneous breathing trial with automatic tube compensation. Physiol Meas. 2017;38:1193–203.
Spadaro S, Mauri T, Bohm SH, Scaramuzzo G, Turrini C, Waldmann AD, Ragazzi R, Pesenti A, Volta CA. Variation of poorly ventilated lung units (silent spaces) measured by electrical impedance tomography to dynamically assess recruitment. Crit Care. 2018;22:26.
Frerichs I, Becher T. Chest electrical impedance tomography measures in neonatology and paediatrics-a survey on clinical usefulness. Physiol Meas. 2019;40:054001.
Schullcke B, Krueger-Ziolek S, Gong B, Jorres RA, Mueller-Lisse U, Moeller K. Ventilation inhomogeneity in obstructive lung diseases measured by electrical impedance tomography: a simulation study. J Clin Monit Comput. 2018;32:753–61.
Yun L, He HW, Moller K, Frerichs I, Liu D, Zhao Z. Assessment of lung recruitment by electrical impedance tomography and oxygenation in ARDS patients. Medicine (Baltimore). 2016;95:e3820.
Funding
This work was financially supported by the project Far Eastern Memorial Hospital (FEMH-2016-C-012 and FEMH-2017-C-055).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Zhanqi Zhao receives a consulting fee from Dräger Medical. Inéz Frerichs reports funding by the European Union’s 7th Framework Program for Research and Technological Development (WELCOME, Grant No. 611223), the European Union’s Framework Program for Research and Innovation Horizon2020 (CRADL, Grant No. 668259 and WELMO, Grant No. 825572) and reimbursement of speaking fees, congress and travel costs by Dräger Medical. Other authors declare no conflict of interest.
Ethical approval
The study was approved by the FEMH Ethics Committee in Taiwan (FEMH-105117-E). The present study involves data from our ongoing registry for EIT guiding PEEP titration (clinical trial registration number NCT03112512, https://clinicaltrials.gov/, registered 13 April 2017).
Informed consent
Written informed consent was obtained from all patients or their legal representatives prior to the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhao, Z., Lee, LC., Chang, MY. et al. The incidence and interpretation of large differences in EIT-based measures for PEEP titration in ARDS patients. J Clin Monit Comput 34, 1005–1013 (2020). https://doi.org/10.1007/s10877-019-00396-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00396-8