Abstract
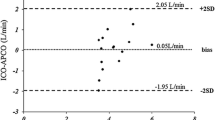
In this study a comparison of cardiac output (CO) measurements obtained with CardioQ transesophageal Doppler (TED) and pulmonary artery catheter (PAC) thermodilution (TD) technique was done in a systematic set-up, with induced changes in preload, afterload and heart rate. Twenty-five patients completed the study. Each patient were placed in the following successive positions: (1) supine, (2) head-down tilt, (3) head-up tilt, (4) supine, (5) supine with phenylephrine administration, (6) pace heart rate 80 beats per minute (bpm), (7) pace heart rate 110 bpm. The agreement of compared data was investigated by Bland–Altman plots, and to assess trending ability a four quadrants plot and a polar plot were constructed. Both methods showed an acceptable precision 6.4 % (PAC TD) and 12.8 % (TED). In comparison with PAC TD, the TED was associated with a mean bias in supine position of −0.30 l min−1 (95 % CI −0.88; 0.27), wide limits of agreement, a percentage error of 69.5 %, and a trending ability with a concordance rate of 92 %, angular bias of 1.1° and a radial sector size of 40.0° corresponding to an acceptable trending ability. In comparison with PAC TD, the CardioQ TED showed a low mean bias, wide limits of agreement and a larger percentage error than should be expected from the precision of the two methods. However, an acceptable trending ability was found. Thus, the CardioQ TED should not replace CO measurements done by PAC TD, but could be a valuable tool in guiding therapy.




Similar content being viewed by others
References
American Society of Anesthesiologists Task Force on Pulmonary Artery Catheterization. Practice guidelines for pulmonary artery catheterization an updated report by the American Society of Anesthesiologists Task Force on Pulmonary Artery Catheterization. Anesthesiology. 2003;99:988–1014.
Rhodes A, Cecconi M, Hamilton M, et al. Goal-directed therapy in high-risk surgical patients: a 15-year follow-up study. Intensiv Care Med. 2010;36:1327–32.
Gan TJ, Soppitt A, Maroof M, El-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PSA. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97:820–6.
Connors AF Jr, Speroff T, Dawson NV, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT investigators. JAMA. 1996;276:889–97.
Polanczyk CA, Rohde LE, Goldman L, et al. Right heart catheterization and cardiac complications in patients undergoing noncardiac surgery: an observational study. JAMA. 2001;286:309–14.
Sandham JD, Hull RD, Brant RF, et al. A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med. 2003;348:5–14.
Tuman KJ, McCarthy RJ, Spiess BD, et al. Effect of pulmonary artery catheterization on outcome in patients undergoing coronary artery surgery. Anesthesiology. 1989;70:199–206.
Pugsley J, Lerner AB. Cardiac output monitoring: is there a golden standard and how do newer technoligies compare? Semin Cardiothorac Vasc Anest. 2010;14:274–82.
Møller-Sørensen H, Hansen KL, Østergaard M, Andersen LW, Møller K. Lack of agreement and trending ability of the endotracheal cardiac output monitor compared with thermodilution. Acta Anaesthesiol Scand. 2012;56:433–40.
Møller-Sørensen H, Graeser K, Hansen KL, Zemtsovski M, Sander EM, Nilsson JC. Measurements of cardiac output obtained with transesophageal echocardiography and pulmonary artery thermodilution are not interchangeable. Acta Anaesthesiol Scand. 2014;58:80–8.
Dark PM, Singer M. The validity of trans-esophageal Doppler ultrasonography as a measure of cardiac output in critically ill adults. Intensiv Care Med. 2004;30:2060–6.
Odenstedt H, Aneman A, Oi Y, Svensson M, Stenqvist O, Lundin S. Descending aortic blood flow and cardiac output: a clinical and experimental study of continuous oesophageal echo-Doppler flowmetry. Acta Anaesthesiol Scand. 2001;45:180–7.
Perrino AC, Fleming J, LaMantia KR. Transesophageal Doppler cardiac output monitoring: performance during aortic reconstructive surgery. Anesth Analg. 1991;73:705–10.
Valtier B, Cholley BP, Belot JP, de La Coussaye JE, Mateo J, Payen DM. Noninvasive monitoring of cardiac output in critically ill patients using transesophageal Doppler. Am J Respir Crit Care Med. 1998;158:77–83.
Keyl C, Rodig G, Lemberger P, Hobbhahn J. A comparison of the use of transesophageal Doppler and thermodilution technique for cardiac output determination. Eur J Anaesth. 1997;13:136–42.
Critchley LAH, Huang L, Zhang J. Continuous cardiac output monitoring: what do validation studies tell us? Curr Anesthesiol Rep. 2014;4:242–50.
Squara P, Cecconi M, Rhodes A, Singer M, Chiche JD. Tracking changes in cardiac output: methodological considerations for the validation of monitoring devices. Intensiv Care Med. 2009;35:1801–8.
Critchley LA, Lee A, Ho AM. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111(5):1180–92.
Berthelsen PG, Nilsson LB. Researcher bias and generalization of results in bias and limits of agreement analyses: a commentary based on the review of 50 Acta Anaesthesiologica Scandinavica papers using the Altman–Bland approach. Acta Anaesthesiol Scand. 2006;50:1111–3.
Cecconi M, Rhodes A, Poloniecki J, et al. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies— with specific reference to the measurement of cardiac output. Crit Care Med. 2009;13:201.
Bundgaard-Nielsen M, Sorensen H, Dalsgaard M, Rasmussen P, Secher NH. Relationship between stroke volume, cardiac output and filling of the heart during tilt. Acta Anaesthesiol Scand. 2009;53:1324–8.
van Lieshout JJ, Harms MP, Pott F, Jenstrup M, Secher NH. Stroke volume of the heart and thoracic fluid content during head-up and head-down tilt in humans. Acta Anaesthesiol Scand. 2005;49:1287–92.
Harms MP, van Lieshout JJ, Jenstrup M, Pott F, Secher NH. Postural effects on cardiac output and mixed venous oxygen saturation in humans. Exp Physiol. 2003;88:611–6.
Nilsson LB, Nilsson JC, Skovgaard LT, Berthelsen PG. Thermodilution cardiac output—are three injections enough? Acta Anaesthesiol Scand. 2004;48:1322–7.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Bland JM, Altman DG. Measuring agreement in method comparison studies. Stat Methods Med Res. 1999;8:135–60.
Critchley LA, Yang XX, Lee A. Assessment of trending ability of cardiac output monitors by polar plot methodology. J Cardiothorac Vasc Anesth. 2011;25:536–46.
Critchley LA, Critchley JA. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J Clin Monit Comput. 1999;15:85–91.
Nishikawa T, Dohi S. Errors in the measurement of cardiac output by thermodilution. Can J Anaesth. 1993;40:142–53.
Lefrant JY, Bruelle P, Aya AG, et al. training is required to improve the reliability of esophageal Doppler to measure cardiac output in critically ill patients. Intensive Care Med. 1998;24:347–52.
Acknowledgments
This work was financially supported by the Department of Cardiothoracic Anesthesiology, Rigshospitalet, Denmark.
Authorship
All authors have approved to the submitted manuscript. hms: study design, data-analysis and interpretation, drafting the article; jc: patient recruitment, acquisition of data, revising article draft; klh: data-analysis and interpretation, revising article draft; mø: acquisition of data, revising article draft; jcn: data-interpretation, revising article draft.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None; Specifically no commercial funding was received. The CardioQ esophageal probes and the CardioQ-ODM were sponsored by NEOVITALIS ApS.
Take-home message
Transesophageal Doppler reliably tracks changes in cardiac output, but can not replace measurements of cardiac output obtained with PAC.
Rights and permissions
About this article
Cite this article
Møller-Sørensen, H., Cordtz, J., Østergaard, M. et al. Transesophageal Doppler reliably tracks changes in cardiac output in comparison with intermittent pulmonary artery thermodilution in cardiac surgery patients. J Clin Monit Comput 31, 135–142 (2017). https://doi.org/10.1007/s10877-015-9806-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9806-4