Abstract
The accuracy of glucose test strip in critically care has been questioned. We investigated the accuracy of glucose test strip in critically ill children. Patients, aged from 1 month to 18 years admitted in pediatric intensive care unit. Demographic data, hemodynamic parameters, and perfusion index (PI) were recorded. Glucose test strips were performed from finger stick blood [capillary blood glucose (CBG)] and from whole blood [whole blood glucose (WBG)] along with laboratory plasma blood glucose (PBG) from either arterial or venous blood samples. The accuracy of glucose test strips was defined according to ISO 15197 and Clarke error grid (CEG). One hundred and eighty one blood samplings including 117 arterial blood (CBG, WBGa, PBGa) and 64 venous blood (CBG, WBGv, PBGv) were obtained. The accuracy of WBGa was 98.3 and 95.2 % when compared to the accuracy of CBG (88.7 and 83.3 %. The accuracy of WBGv was 92.2 % and 87.0 when compared to the accuracy of CBG which was 79.7 and 72.9 % (ISO 15197: 2003 and 2013, respectively). Bland–Altman plot demonstrated bias and precision of 7.4 ± 17.7 mg/dL in acceptable PI group compared to 30.2 ± 23.4 mg/dL in low PI group (PI ≤ 0.3). The CBG test strip must be interpreted carefully in critically ill children. A low PI was associated with poor CBG strip accuracy. WBG test strip from arterial blood was more appropriate for glucose monitoring in children with peripheral hypoperfusion.
Similar content being viewed by others
1 Introduction
Hyperglycemia and hypoglycemia are risk factors for increasing morbidity and mortality in critically ill children. The optimal glucose control in these patients is important. The glucose test strip from finger stick blood representing capillary blood glucose (CBG) has been used as the standard point of care (POC) for glucose measurement. However, the accuracy of this glucose measurement has been questioned especially in critically ill patients, and might have a low level of accuracy [1, 2]. Studies have shown overestimation of glucose level by CBG, therefore, it is not recommended to use in the intensive care unit [2]. Arterial blood samples appear to be more accurate for measuring blood glucose level, therefore, laboratory blood glucose measurement from arterial blood was considered to be the reference value [3]. Study in adults post cardiac surgery demonstrated whole blood glucose (WBG) levels correlated most closely with laboratory plasma blood glucose (PBG) levels in patients receiving intensive intravenous insulin therapy after cardiac surgery [4]. The decreased peripheral perfusion in critically ill patients may be a factor associated with inaccuracy of CBG [5]. Thus, the purpose of the present study was to determine the accuracy of bedside glucose measurements using glucose test strip from finger stick (CBG), venous whole blood samples, and arterial whole blood samples compared to the standard laboratory PBG in critically ill children.
2 Methods
This was a cross-sectional study in an 8-bed pediatric intensive care unit (PICU) of a 1,000-bed Tertiary Care University Hospital. We included patients, age from 1 month to 18 years who required blood glucose monitoring during 1-year period from July 1, 2011 to June 30, 2012. This study was approved by the Institution’s Ethics Committee with guardians’ informed consent. The patients’ age, sex, indications for admission in PICU were obtained.
2.1 Measurements
2.1.1 Glucose measurements
In all patients, blood samples from either artery or vein were collected in sodium fluoride tube in order to inhibit glycolysis and sent for laboratory PBG using hexokinase method. These glucose measurements were used as a standard values for reference. Blood glucose with glucose test strips read by Accu-Chek® was measured simultaneously from these blood samples represented as WBG and also from capillary blood using finger stick represented as CBG. This glucometry device was routinely used in PICU and maintenance was standardized. For comparison, we divided glucose samples into two groups consisting of arterial blood (PBGa, WBGa, and CBG) and venous blood (PBGv, WBGv, and CBG). The glucose measurements were compared for their accuracy.
2.1.2 Perfusion index (PI) measurement
PI measurement was assessed with Masimo Radical® based on signal extraction technology (SET) by placing the sensor on the same digit just before the finger stick glucose was obtained. In pulse oximetry, PI is a scalar value derived from magnitude of the pulsations displayed on the plethysmographic wave form by calculation from the ratio of the amount of infrared signal light absorbed by pulsating arterial flow (pulsatile component) to the amount of infrared signal light absorbed by skin, other tissues, and venous blood (non-pulsatile component) [6]. The upper and lower limits of PI for Masimo Radical SET reported by the manufacturer are 0.02–20.00. Poor tissue perfusion or peripheral hypoperfusion leads to a reduction of PI [7]. Values were considered marginal if below 0.3, acceptable between 0.3 and 1.0, and optimal above 1.
2.1.3 Parameters indicated perfusion
PI, blood pressure, pulse rate, temperature, oxygen saturation, shock, skin changes (mottling and/or cyanosis), capillary refill time, ventilator support, hematocrit, and pH were obtained on the same time of each blood sample.
2.2 Statistical analysis
Continuous variables were described as median and interquartile range (IQR). Categorical variables were described as ratio. Mann–Whitney U tests were use to compare continuous variable in each group. McStat statistical software was used to analyze data. Bland–Altman method was used for assessing agreement between each pair of blood glucose measurement. A bias and precision were calculated from Bland–Altman graph [8]. A p value <0.05 was considered to be statistically significant.
According to the international standardization organization (ISO) 15917:2003, the relative number of blood glucose difference within ±15, ±10, and ±5 mg/dL (at blood glucose levels <75 mg/dL) and ±20, ±15, ±10, and ±5 % (at blood glucose levels ≥75 mg/dL) from the reference measurement (PBG) were calculated. The number of differences within ±15 mg/dL at blood glucose levels <75 mg/dL and within ±20 % at blood glucose levels ≥75 mg/dL were used for assessment of the overall accuracy of glucose test strips from CBG and WBG [9]. Recently, according to the new ISO 15197:2013, the relative number of blood glucose difference within ±15, ±10, and ±5 mg/dL (at blood glucose levels <100 mg/dL) and ±15, ±10, and ±5 % (at blood glucose levels ≥100 mg/dL) from the reference measurement (PBG) were also calculated. The number of differences within ±15 mg/dL at blood glucose levels <100 mg/dL and within ±15 % at blood glucose levels ≥100 mg/dL were used for assessment of the overall accuracy of glucose test strips from CBG and WBG [10]. The acceptable percentage of all results within bias limits is 95 %.
Clarke error grid [11] was used to assess clinical accuracy of blood glucose values obtained from CBG and WBG against the reference values from PBG. For arterial blood, the clinical accuracy of WBGa and PBGa was compared to the clinical accuracy of CBG and PBGa. For venous blood, clinical accuracy of WBGv and PBGv was compared to the clinical accuracy of CBG and PBGv. The absolute bias was calculated by the difference between the sensor glucose levels (WBG or CBG) and the reference glucose values (PBG). Then, the absolute relative bias (ARB) was calculated by the following equation: ARB = absolute bias/reference glucose * 100. CEG divides into five zones as the following.
-
Zone A are those values within 20 % of the reference glucose levels or paired glucose levels <70 mg/dL.
-
Zone B contains points that are outside of 20 % but would not lead to inappropriate treatment.
-
Zone C are those points leading to unnecessary treatment.
-
Zone D are those points indicating a potentially dangerous failure to detect hypoglycemia or hyperglycemia.
-
Zone E are those points that would confuse treatment of hypoglycemia for hyperglycemia and vice versa.
3 Results
There were 86 patients (50 males) with median age of 58.5 months, IQR 12–154. Most patients were admitted in PICU due to (1) post operative care (45 %) including neurological patients (20 %), cardiovascular patients (8 %), oncologic patients (7 %), gastro-intestinal patients (5 %), and others (5 %); (2) close monitoring (17 %) including respiratory system (6 %), cardiovascular system (6 %), and neurological system (5 %); (3) septic shock (14 %); (4) respiratory failure (12 %); (5) heart failure (6 %); and (6) miscellaneous (4 %). A total of 181 blood glucose assays for PBG were sent to the laboratory including arterial blood (PBGa, n = 117 samples) and venous blood (PBGv, n = 64 samples) with simultaneous WBG and CBG by glucose test strip. The median PBGa, WBGa, and CBG were not significantly different (130 mg/dL, IQR 112–164; 124 mg/dL, IQR 108–156; and 121 mg/dL, IQR 106–148, respectively). The median absolute bias (6 mg/dL, IQR 2–12) and ARB (3.9 %, IQR 1.8–8.1) of WBGa were significantly lower than those of CBG (9 mg/dL, IQR 3–18 and 5.9 %, IQR 2–12.3, respectively, p = 0.02). Overall, from arterial blood samples (N = 115, excluded two samples which glucose level was <75 mg/dL), the accuracy of WBGa was 98.3 % (ISO 15197: 2003) and 95.2 % (ISO 15197: 2013) when compared to the accuracy of CBG which was 88.7 % (ISO 15197: 2003) and 83.3 % (ISO 15197: 2013) (Tables 1, 2). The samples <100 mg/dL were excluded for the evaluation of the accuracy by ISO 15197:2013, since the samples were quite low. Subgroup analysis in arterial blood samples was categorized into two groups, consisting of 102 blood samples obtained during acceptable PI (>0.3) and 15 blood samples obtained during low PI (≤0.3). The accuracy of CBG was higher in subgroup with normal PI when compare to that with low PI (Tables 1, 2). The median PBGv, WBGv, and CBG were also not significantly different (118 mg/dL, IQR 102–165; 116 mg/dL, IQR 104–168; and 113 mg/dL, IQR 100–157, respectively). The median absolute bias (7 mg/dL, IQR 4–13) and ARB (5.5 %, IQR 2.6–8.5) of WBGv were significantly lower than those of CBG (11 mg/dL, IQR 4–22 and 8.2 %, IQR 3–16.5, respectively), p = 0.04. Overall, from venous blood samples (N = 54, excluded ten samples which glucose level was <100 mg/dL), the accuracy of WBGv was 92.2 % (ISO 15197: 2003) and 87.0 % (ISO 15197: 2013) when compared to the accuracy of CBG which was 79.7 % (ISO 15197: 2003) and 72.9 % (ISO 15197: 2013) (Tables 1, 2). Subgroup analysis in venous blood samples was categorized into two groups, consisting of 56 blood samples obtained during acceptable PI (>0.3) and eight blood samples obtained during low PI (≤0.3). The accuracy of CBG was higher in subgroup with normal PI when compare to that with low PI (Tables 1, 2).
Using Bland–Altman plot, the overall difference between PBGa and CBG had bias (mean) and precision (standard deviation) of 10.3 ± 20.0 mg/dL compared to the difference between PBGa and WBGa (4.8 ± 22.7 mg/dL) (Fig. 1). Interestingly, each pair of blood samples between PBGa and CBG from children with low PI (mean and precision = 30.2 ± 23.4 mg/dL) tended to be scatter from the bias line rather than those from children with normal PI (mean and precision = 7.4 ± 17.7 mg/dL) whereas this observation was not found in blood samples between PBGa and WBGa (mean and precision of 3.1 ± 16.1 in children with low PI and 5.1 ± 12.2 in children with acceptable PI). The overall difference between PBGv and CBG had bias and precision of 3.7 ± 23.6 mg/dL compared to the difference between PBGv and WBGv (0.9 ± 12.5 mg/dL) (Fig. 2). Interestingly, each pair of blood samples between PBGv and CBG from children with low PI (mean and precision = −8.5 ± 37.1 mg/dL) tended to scatter from the bias line rather than those from children with normal PI (mean and precision = 5.4 ± 21.0 mg/dL) whereas this observation was not found in blood samples between PBGv and WBGv (mean and precision of 2.9 ± 8.9 from children with low PI and 1.4 ± 12.6 from children with normal PI).
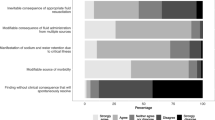
Clarke error grid graph demonstrated that all CBG and WBG either from arterial or venous blood samples were in zone A and B. However, the percentage in zone A of WBG was greater than that of CBG (Figs. 3, 4). Moreover, the points in zone B were more in samples from patients with low PI.
Clark error grid graph plotted between PBG from arterial blood samples (PBGa) [reference blood glucose (RFBG)] and glucose test strips from capillary blood sample using finger stick (CBG) [sensor blood glucose (SBG)] (A) and between PBGa (RFBG) and glucose test strips from whole arterial blood sample (WBGa) (SBG) (B). Zone A: [ARB ≤ 20] or [both reference glucose levels and measured glucose levels < 70 mg/dL]. Zone B: not in zone A, C, D, E. Zone C: [130 ≤ RFBG ≤ 180 and SBG < line equation 1] or [RFBG > 70 and SBG > 180 and SBG > line equation 2]. Zone D: [RFBG < 70 and 70 < SBG < 180 mg/dL] or [RFBG > 240 and 70 < SBG < 180 mg/dL]. Zone E: [RFBG ≤ 70 and SBG ≥ 180 mg/dL] or [RFBG ≥ 180 and SBG ≤ 70 mg/dL]. ARB = absolute bias [SBG − RFBG]/RFBG * 100. Line equation 1 = [7/5] * [RFBG − 130]; line equation 2 = RFBG + 110. Filled circle: Paired glucose samples from children with normal pulsatility index in zone A. Open diamond: Paired glucose samples from children with low pulsatility index (PI ≤ 0.3) in zone A. Filled square: Paired glucose samples from children with normal pulsatility index in zone B. Filled diamond: Paired glucose samples from children with low pulsatility index (PI ≤ 0.3) in zone B
Clark error grid graph plotted between PBG from venous blood samples (PBGv; RFBG) and glucose test strips from capillary blood sample using finger stick (CBG; SBG) (A) and between PBGv (RFBG) and glucose test strips from whole venous blood sample (WBGa) (SBG) (B). Zone A: [ARE ≤ 20] or [both reference glucose levels and measured glucose levels <70 mg/dL]. Zone B: not in zone A, C, D, E. Zone C: [130 ≤ RFBG ≤ 180 and SBG < line equation 1] or [RFBG > 70 and SBG > 180 and SBG > line equation 2]. Zone D: [RFBG < 70 and 70 < SBG < 180 mg/dL] or [RFBG > 240 and 70 < SBG < 180 mg/dL]. Zone E: [RFBG ≤ 70 and SBG ≥ 180 mg/dL] or [RFBG ≥ 180 and SBG ≤ 70 mg/dL]. ARB = absolute bias [SBG − RFBG]/RFBG * 100. Line equation 1 = [7/5] * [RFBG − 130]; line equation 2 = RFBG + 110. Filled circle: Paired glucose samples from children with normal pulsatility index in zone A. Open diamond: Paired glucose samples from children with low pulsatility index (PI ≤ 0.3) in zone A. Filled square: Paired glucose samples from children with normal pulsatility index in zone B. Filled diamond: Paired glucose samples from children with low pulsatility index (PI ≤ 0.3) in zone B
Using logistic regression analysis for parameters indicated perfusion including PI, blood pressure, pulse rate, temperature, oxygen saturation, shock, skin changes (mottling and/or cyanosis), capillary refill time, ventilator support, hematocrit, and pH, found only PI ≤ 0.3 was the factor determining the disagreement between PBGa and CBG, p < 0.001; and between PBGv and CBG, p < 0.008 (Table 3).
4 Discussion
In general, WBG concentrations are approximately 15 % lower than PBG [12]. However, the Roche Accu-Chek was calibrated to deliver plasma-like value even using whole blood for glucose test strip [13]. This ensured comparability of results between glucose test strip (whole blood) and laboratory (plasma) glucose measurements. In this study, the authors used the laboratory plasma glucose as the standard reference.
Meynaar et al. [14] reported that WBG measurement from arterial blood using glucose test strip (Accu-Chek®) could be used accurately in critically ill adult patients instead of laboratory PBG. Critchell et al. [2] reported inaccuracy of glucose test strip (Accu-Chek) from capillary blood using finger stick in the intensive care setting. In contrast, Karon et al. [4] reported WBG levels as measured by serum calibrated Accu-Chek correlated well with laboratory PBG levels in patients post cardiac surgery. In this study included critically ill pediatric patients, 88.9 and 79.7 % of CBG values using Accu-Chek test strip from finger stick differed from simultaneous laboratory arterial or venous plasma blood samples within 20 %, respectively, whereas 98.3 and 92.2 % of WBG levels using Accu-Chek test strip from either arterial or venous blood differed from simultaneous laboratory PBG levels from the same blood samples within 20 %, respectively. ISO 15917:2003 states that 95 % of the individual glucose results should fall within 15 mg/dL at glucose level ≤75 mg/dL and within ±20 % at glucose levels >75 mg/dL for minimum acceptable accuracy [9]. Recently, ISO 15197:2013 states that 95 % of the individual glucose results should fall within 15 mg/dL at glucose level <100 mg/dL and within ±15 % at glucose levels ≥100 mg/dL [10]. Importantly, the glucose test strip from whole venous blood was accurate only 92.2–87.0 % according to ISO 15197:2003 and ISO 15197:2013, respectively. The glucose test strip from whole arterial blood had a high percentage of accuracy (98.3 % according to ISO 15197:2003 and 95.2 % according to ISO 15197:2013). This finding was the in the same direction as reported by Meynaar et al. [14]. From this data it is concluded that only glucose test strips from arterial blood samples (WBGa) meets the ISO criteria. This demonstrated that the accuracy between glucose test strips from capillary blood using finger stick in critically ill pediatric patients was not reliable in some situations. The accuracy glucose test strips from capillary blood using finger stick (CBG) was low especially samples from children with low PI. Only CBG in patients with normal PI when compared to arterial blood met the criteria of ISO 15197:2003 but did not meet the criteria of ISO 15197:2013. This study demonstrated that low perfusion index was the only factor associated with the inaccuracy between CBG and PBGa. Subgroup analysis demonstrated bias between CBG and PBGa in patients with low PI (≤0.3) was higher than bias between CBG and PBGa in patients with acceptable PI (≥0.3). As previous reports [5, 15], this study’s results suggested that the glucose test strip from capillary blood using finger stick could underestimate or overestimate glucose levels when compared to laboratory PBG levels in unpredictable fashion especially in the low perfusion state. In this situation, bedside glucose test strip on arterial or venous blood could be used instead of glucose test strip on capillary blood to avoid this inaccuracy. We suggested using PI as a simple screening tool for low perfusion state. If PI is ≤0.3, CBG using finger stick blood should be avoided.
Although CBG and WBGv in critically ill pediatric patients was not accurate enough to meet ISO 15197, however, according to CEG graph, none of these samples was in zone C, D, and E which means there was no inaccurate glucose levels leading to unnecessary treatment, undetected potential hazard hypoglycemia/hyperglycemia, or inappropriate treatment of hypoglycemia for hyperglycemia and vice versa.
Glucose test strips from venous blood samples seemed to be less accurate than from arterial blood samples. If possible, we suggested using glucose test strip test from arterial blood rather than venous blood. In this study, glucose measurement performed with glucose test strip from arterial or venous blood was more reliable than that from a capillary sample, especially in a child with poor peripheral perfusion. Although CBG using glucose test strip from finger stick blood is still the standard point-of-care for monitoring glucose level in critically ill children, but glucose test strip from arterial blood should be considered in children with evidence of peripheral hypoperfusion including shock and low PI. Since the invasive arterial line or central venous line is commonly placed in critically ill children with shock requiring vasoactive medications, so blood glucose can be measured by using glucose test strip from these samples rather than capillary blood as a POC test. Glucose test strips from venous blood might be interpreted carefully since the accuracy of this method was less than the accuracy of glucose test strips from arterial blood. In case that there are both arterial and venous lines, the authors recommended using arterial blood samples.
5 Conclusions
Bedside glucose test strip from finger stick (CBG) should be interpreted carefully in critically ill children with peripheral hypoperfusion. A low perfusion index (PI ≤ 0.3) was associated with poor CBG accuracy. Glucose test strip from arterial blood was more appropriate for glucose monitoring in critically ill children with peripheral hypoperfusion.
References
Mebis L, Gunst J, Langouche L, Vanhorebeek I, Van den Berghe G. Indication and practical use of intensive insulin therapy in the critically ill. Curr Opin Crit Care. 2007;13:392–8.
Critchell CD, Savarese V, Callahan A, Aboud C, Jabbour S, Marik P. Accuracy of bedside capillary blood glucose measurements in critically ill patients. Intensive Care Med. 2007;33:2079–84.
Cengiz E, Tamborlane WV. A tale of two compartments: interstitial versus blood glucose monitoring. Diabetes Technol Ther. 2009;11:S11–6.
Karon BS, Gandhi GY, Nuttall GA, Bryant SC, Schaff HV, McMahon MM, et al. Accuracy of roche accu-chek inform whole blood capillary, arterial, and venous glucose values in patients receiving intensive intravenous insulin therapy after cardiac surgery. Am J Clin Pathol. 2007;127:919–26.
Desachy A, Vuagnat AC, Ghazali AD, Baudin OT, Longuet OH, Calvat SN, et al. Accuracy of bedside glucometry in critically ill patients: influence of clinical characteristics and perfusion index. Mayo Clin Proc. 2008;83:400–5.
De Felice C, Goldstein MR, Parrini S, Verrotti A, Criscuolo M, Latini G. Early dynamic changes in pulse oximetry signals in preterm newborns with histologic chorioamnionitis. Pediatr Crit Care Med. 2006;7:138–42.
Lima AP, Beelen P, Bakker J. Use of a peripheral perfusion index derived from the pulse oximetry signal as a noninvasive indicator of perfusion. Crit Care Med. 2002;30:1210–3.
Bland JM, Altman DG. Statistical method for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
ISO 15197. In vitro diagnostic test systems—requirements for blood-glucose monitoring systems for self-testing in managing diabetes mellitus. Geneva, Switzerland: International Organization for Standardization; 2003.
ISO 15197. In vitro diagnostic test systems—requirements for blood-glucose monitoring systems for self-testing in managing diabetes mellitus. Geneva, Switzerland: International Organization for Standardization; 2013.
Clark WL, Cox D, Gonder-Frederick LA, Carter WL, Pohl SL. Evaluating clinical accuracy of systems for self-monitoring of blood glucose. Diabetes Care. 1987;10:662–8.
Colagiuri S, Sandbaek A, Carstensen B, Christensen J, Glumer C, Lauritzen T, et al. Comparability of venous and capillary glucose measurements in blood. Diabet Med. 2003;20:953–6.
Meex C, Poncin J, Chapelle JP, Cavalier E. Analytical validation of the new plasma calibrated accu-chek test strips (roche diagnostics). Clin Chem Lab Med. 2006;44:1376–8.
Meynaar IA, van Spreuwel M, Tangkau PL, Dawson L, Sleeswijk Visser S, Rijks L, et al. Accuracy of accuchek glucose measurement in intensive care patients. Crit Care Med. 2009;37:2691–6.
Kanji S, Buffie J, Hutton B, Bunting PS, Singh A, McDonald K, et al. Reliability of point-of-care testing for glucose measurement in critically ill adults. Crit Care Med. 2005;33:2778–85.
Acknowledgments
We are grateful to the patients’ parents who allow their children to participate in the study and the many pediatric residents and nurses that taking care of these patients.
Conflict of interest
None.
Ethical standard
This study was approved by the Institution’s Ethics Committee with guardians’ informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khositseth, A., Pharadornuwat, O., Lertbunrian, R. et al. Accuracy of bedside glucometry in critically ill children with peripheral hypoperfusion. J Clin Monit Comput 29, 145–152 (2015). https://doi.org/10.1007/s10877-014-9579-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9579-1