Abstract
Purpose
This phase 4, multicenter, open-labeled, single-sequence, crossover study in pediatric patients (ages 2 to 16) with primary immunodeficiency disease (PID) evaluated the pharmacokinetics, safety, and tolerability for subcutaneously (SC) administered 10 % caprylate/chromatography purified human immune globulin injection (IGIV-C, GAMUNEX®) compared with intravenously (IV) administered IGIV-C.
Methods
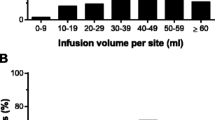
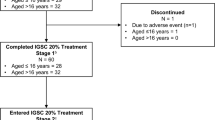
This study included a screening phase, run-in phase (where required), IV treatment phase, SC treatment phase, and end of study/early termination visit. Eligible patients receiving a stable dose of IGIV-C entered into the IV phase to receive two IV infusions of IGIV-C (200–600 mg/kg per infusion) every 3–4 weeks. The weekly SC dose of IGIV-C was calculated using a conversion factor of 1.37 times the prior IV dose.
Results
Twelve subjects between the ages of 2 and 16 years participated in the clinical study with the median age being 11 years old. The adjusted weekly mean AUC0-τ,IV was 216,873.7 h*mg/dL for the IV phase versus a mean AUC0-τ,SC of 230,830.0 h*mg/dL for the SC phase. The mean (range) C trough was 997.2 (784–1320) mg/dL in the IV phase and 1325.0 (1077–1690) mg/dL in the SC phase. During the SC phase, 100.0 % of the patients (n = 11) experienced treatment-emergent adverse events (TEAEs) that were local infusion reactions and 9 patients (81.8 %) had TEAEs that were non-infusion site reactions. The majority of TEAEs were mild or moderate in severity.
Conclusion
In pediatric patients with PID, SC-administered IGIV-C provides comparable overall serum exposure to total IgG to that produced by IV-administered IGIV-C. We have concluded that weekly SC administration of 10 % IGIV-C based on a dose conversion factor of 1.37 is safe and well-tolerated in pediatric patients with PID.
Trial Registration
ClinicalTrials.gov identifier: NCT01465958. https://clinicaltrials.gov/ct2/show/NCT01465958?term=NCT01465958.&rank=1


Similar content being viewed by others
References
Wood P, Stanworth S, Burton J, Jones A, Peckham DG, Green T, et al. Recognition, clinical diagnosis and management of patients with primary antibody deficiencies: a systematic review. Clin Exp Immunol. 2007;149(3):410–23.
Smith GN, Griffiths B, Mollison D, Mollison PL. Uptake of IgG after intramuscular and subcutaneous injection. Lancet. 1972;1(7762):1208–12.
Ochs HD, Fischer SH, Lee ML, Delson ES, Kingdon HS, Wedgwood RJ. Intravenous immunoglobulin home treatment for patients with primary immunodeficiency diseases. Lancet. 1986;1(8481):610–1.
Mankarious S, Lee M, Fischer S, Pyun KH, Ochs HD, Oxelius VA, et al. The half-lives of IgG subclasses and specific antibodies in patients with primary immunodeficiency who are receiving intravenously administered immunoglobulin. J Lab Clin Med. 1988;112(5):634–40.
Fischer SH, Ochs HD, Wedgwood RJ, Skvaril F, Morell A, Hill HR, et al. Survival of antigen-specific antibody following administration of intravenous immunoglobulin in patients with primary immunodeficiency diseases. Monogr Allergy. 1988;23:225–35.
Berger M. Principles of and advances in immunoglobulin replacement therapy for primary immunodeficiency. Immunol Allergy Clin N Am. 2008;28(2):413–37.
Wasserman RL. Progress in gammaglobulin therapy for immunodeficiency: from subcutaneous to intravenous infusions and back again. J Clin Immunol. 2012;32(6):1153–64.
Berger M. Incidence of infection is inversely related to steady-state (trough) serum IgG level in studies of subcutaneous IgG in PIDD. J Clin Immunol. 2011;31(5):924–6.
Berger M, Murphy E, Riley P, Bergman GE. Improved quality of life, immunoglobulin G levels, and infection rates in patients with primary immunodeficiency diseases during self-treatment with subcutaneous immunoglobulin G. South Med J. 2010;103(9):856–63.
Orange JS, Grossman WJ, Navickis RJ, Wilkes MM. Impact of trough IgG on pneumonia incidence in primary immunodeficiency: a meta-analysis of clinical studies. Clin Immunol. 2010;137(1):21–30.
Gardulf A, Hammarstrom L, Smith CI. Home treatment of hypogammaglobulinaemia with subcutaneous gammaglobulin by rapid infusion. Lancet. 1991;338(8760):162–6.
Gardulf A, Bjorvell H, Gustafson R, Hammarstrom L, Smith CIE. Safety of rapid subcutaneous gammaglobulin infusions in patients with primary antibody deficiency. Immunodeficiency. 1993;4(1-4):81–4.
Chapel HM, Spickett GP, Ericson D, Engl W, Eibl MM, Bjorkander J. The comparison of the efficacy and safety of intravenous versus subcutaneous immunoglobulin replacement therapy. J Clin Immunol. 2000;20(2):94–100.
Gardulf A, Nicolay U, Asensio O, Bernatowska E, Bock A, Carvalho BC, et al. Rapid subcutaneous IgG replacement therapy is effective and safe in children and adults with primary immunodeficiencies—a prospective, multi-national study. J Clin Immunol. 2006;26(2):177–85.
Ochs HD, Gupta S, Kiessling P, Nicolay U, Berger M, Subcutaneous Ig GSG. Safety and efficacy of self-administered subcutaneous immunoglobulin in patients with primary immunodeficiency diseases. J Clin Immunol. 2006;26(3):265–73.
Fasth A, Nystrom J. Safety and efficacy of subcutaneous human immunoglobulin in children with primary immunodeficiency. Acta Paediatr. 2007;96(10):1474–8.
Wasserman RL, Irani AM, Tracy J, Tsoukas C, Stark D, Levy R, et al. Pharmacokinetics and safety of subcutaneous immune globulin (human), 10% caprylate/chromatography purified in patients with primary immunodeficiency disease. Clin Exp Immunol. 2010;161(3):518–26.
Berger M, Pinciaro PJ, Althaus A, Ballow M, Chouksey A, Moy J, et al. Efficacy, pharmacokinetics, safety, and tolerability of Flebogamma 10% DIF, a high-purity human intravenous immunoglobulin, in primary immunodeficiency. J Clin Immunol. 2010;30(2):321–9.
Wasserman RL, Melamed I, Kobrynski L, Strausbaugh SD, Stein MR, Sharkhawy M, et al. Efficacy, safety, and pharmacokinetics of a 10% liquid immune globulin preparation (GAMMAGARD LIQUID, 10%) administered subcutaneously in subjects with primary immunodeficiency disease. J Clin Immunol. 2011;31(3):323–31.
Berger M, Rojavin M, Kiessling P, Zenker O. Pharmacokinetics of subcutaneous immunoglobulin and their use in dosing of replacement therapy in patients with primary immunodeficiencies. Clin Immunol. 2011;139(2):133–41.
Borte M, Pac M, Serban M, Gonzalez-Quevedo T, Grimbacher B, Jolles S, et al. Efficacy and safety of hizentra(R), a new 20% immunoglobulin preparation for subcutaneous administration, in pediatric patients with primary immunodeficiency. J Clin Immunol. 2011;31(5):752–61.
Borte M, Quinti I, Soresina A, Fernandez-Cruz E, Ritchie B, Schmidt DS, et al. Efficacy and safety of subcutaneous vivaglobin(R) replacement therapy in previously untreated patients with primary immunodeficiency: a prospective, multicenter study. J Clin Immunol. 2011;31(6):952–61.
Jolles S, Bernatowska E, de Gracia J, Borte M, Cristea V, Peter HH, et al. Efficacy and safety of Hizentra((R)) in patients with primary immunodeficiency after a dose-equivalent switch from intravenous or subcutaneous replacement therapy. Clin Immunol. 2011;141(1):90–102.
Jolles S, Borte M, Nelson Jr RP, Rojavin M, Bexon M, Lawo JP, et al. Long-term efficacy, safety, and tolerability of Hizentra(R) for treatment of primary immunodeficiency disease. Clin Immunol. 2014;150(2):161–9.
Kanegane H, Imai K, Yamada M, Takada H, Ariga T, Bexon M, et al. Efficacy and safety of IgPro20, a subcutaneous immunoglobulin, in Japanese patients with primary immunodeficiency diseases. J Clin Immunol. 2014;34(2):204–11.
Zampelli AR. Improving quality of life at home for pediatric patients and families with primary immune deficiencies using subcutaneous immune globulin infusions. Home Health Care Manag Pract. 2007;19(6):431–5.
Gardulf A, Nicolay U, Math D, Asensio O, Bernatowska E, Bock A, et al. Children and adults with primary antibody deficiencies gain quality of life by subcutaneous IgG self-infusions at home. J Allergy Clin Immunol. 2004;114(4):936–42.
Waniewski J, Gardulf A, Hammarstrom L. Bioavailability of gamma-globulin after subcutaneous infusions in patients with common variable immunodeficiency. J Clin Immunol. 1994;14(2):90–7.
Berger M. Subcutaneous administration of IgG. Immunol Allergy Clin North Am. 2008;28(4):779–802. viii.
Acknowledgments
Grifols, Bioscience Industrial Group, would like to acknowledge the investigators, the site personnel, and the patients who participated in this study. Also, Cristina Cruz (Grifols, Bioscience Industrial Group), who provided oversight for the in-house measles antibody testing; Susan Sorrells and Kim Hanna (Grifols, Bioscience Industrial Group) for their critical review of the manuscript; and Toya Lennon (Grifols, Bioscience Industrial Group) who provided study conduct oversight and review of the manuscript. This study was sponsored by Grifols Therapeutics Inc. Grifols manufactures GAMUNEX®-C. Medical writing assistance was provided under the direction of the authors by Latoya M. Mitchell, PhD, CMPP, of Grifols.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by all participating centers’ institutional review boards, and the investigators ensured that the study was conducted in full conformance with appropriate laws, regulations, and the 1964 Declaration of Helsinki. Written informed consent was obtained from each patient and/or legal guardian, and all patients provided assent.
Conflict of Interest
Junliang Chen and Rhonda Griffin are employees of Grifols, Bioscience Industrial Group. Drs. Heimall, Church, Melamed, and Kleiner served as primary investigators for this study. Dr. Church has received funding from BioProducts Laboratory, LTD; BD Biosciences, Inc; and Prometic Biotherapeutics. No other potential conflicts of interest were reported.
Rights and permissions
About this article
Cite this article
Heimall, J., Chen, J., Church, J.A. et al. Pharmacokinetics, Safety, and Tolerability of Subcutaneous Immune Globulin Injection (Human), 10 % Caprylate/Chromatography Purified (GAMUNEX®-C) in Pediatric Patients with Primary Immunodeficiency Disease. J Clin Immunol 36, 600–609 (2016). https://doi.org/10.1007/s10875-016-0311-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10875-016-0311-4