Abstract
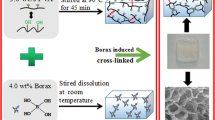
Injectable hydrogels have attracted considerable attention in regenerative medicine since their controllable properties. However, there are quite a few challenges in regulating an ideal hydrogel’s features for target tissue; overcoming them needs reliable fabrication techniques. In the present work, a novel in situ forming hydrogel based on aldehyde-modified xanthan gum (AXG) and gelatin (Gel) has been developed by taking advantage of Schiff’s base reaction and optimized for the tissue engineering applications. First, the AXG with three different oxidation degrees has been successfully synthesized using sodium periodate. Later on, AXG and Gel were blended with different volume ratios. The prepared scaffolds were characterized by FTIR, SEM, rheometer, and compression analysis. In addition, the hydrogels gelation time, injectability, self-healing, and swelling ratios were studied. The results indicated that all hydrogels exhibited suitable morphological as well as physical characteristics for biomedical applications. Because of its high compression strength and modulus, high storage modulus, and suitable swelling behavior, the X1/G2 hydrogel sample was selected as the optimal scaffold. In vitro cell viability shows ≥ 90% cell viability, and MG-63 cells lingered at the surface of the hydrogel, indicating that hydrogels can provide a suitable substrate for cell viability and cell adhesion by in vitro cell culture assay. This study illustrated that the synthesized hydrogels could be reputable scaffolds for biomedical and tissue engineering applications; however, more studies are needed.
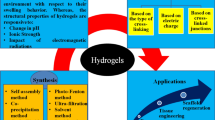
Graphical abstract
Novel polysaccharide-based hydrogels formed by Schiff’s base reaction of aldehyde and amine groups, displaying suitable physicomechanical and biological properties for biomedical and tissue engineering applications.










Similar content being viewed by others
References
Kim Y-M, Potta T, Park K-H, Song S-C (2017) Temperature responsive chemical crosslinkable UV pretreated hydrogel for application to injectable tissue regeneration system via differentiations of encapsulated hMSCs. Biomaterials 112:248–256. https://doi.org/10.1016/j.biomaterials.2016.10.025
Han YL, Yang Y, Liu S, Wu J, Chen Y, Lu TJ, Xu F (2013) Directed self-assembly of microscale hydrogels by electrostatic interaction. Biofabrication 5(3):035004. https://doi.org/10.1088/1758-5082/5/3/035004
Wei Z, Yang JH, Liu ZQ, Xu F, Zhou JX, Zrínyi M, Osada Y, Chen YM (2015) Novel biocompatible polysaccharide-based self-healing hydrogel. Adv Func Mater 25(9):1352–1359. https://doi.org/10.1002/adfm.201401502
Zheng B-D, Ye J, Yang Y-C, Huang Y-Y, Xiao M-T (2022) Self-healing polysaccharide-based injectable hydrogels with antibacterial activity for wound healing. Carbohydr Polym 275:118770. https://doi.org/10.1016/j.carbpol.2021.118770
Huang J, Deng Y, Ren J, Chen G, Wang G, Wang F, Wu X (2018) Novel in situ forming hydrogel based on xanthan and chitosan re-gelifying in liquids for local drug delivery. Carbohyd Polym 186:54–63. https://doi.org/10.1016/j.carbpol.2018.01.025
Khodadadi Yazdia M, Zarrintaj P, Khodadadi A et al (2021) Polysaccharide-based electroconductive hydrogels: Structure, properties and applications in biomedical engineering. Carbohydr Polym. https://doi.org/10.1016/j.carbpol.2021.118998
Mo C, Li X, Chen Y (2021) Advances in Injectable and Self-healing Polysaccharide Hydrogel Based on the Schiff Base Reaction. Macromol Rapid Commun 42(10):2100025. https://doi.org/10.1002/marc.202100025
Hassler RA, Doherty DH (1990) Genetic engineering of polysaccharide structure: production of variants of xanthan gum in Xanthomonas campestris. Biotechnol Prog 6(3):182–187. https://doi.org/10.1021/bp00003a003
Kumar A, Rao KM, Han SS (2018) Application of xanthan gum as polysaccharide in tissue engineering: a review. Carbohyd Polym 180:128–144. https://doi.org/10.1016/j.carbpol.2017.10.009
Zhong L, Oostrom M, Truex MJ, Vermeu VR, Szecsody JE (2013) Rheological behavior of xanthan gum solution related to shear thinning fluid delivery for subsurface remediation. J Hazard Mater 244:160–170. https://doi.org/10.1016/j.jhazmat.2012.11.028
Petri DF (2015) Xanthan gum: a versatile biopolymer for biomedical and technological applications. J Appl Polym Sci 132(23):1548. https://doi.org/10.1002/app.42035
Guo J, Gea L, Li X, Mu C, Li D (2014) Periodate oxidation of xanthan gum and its crosslinking effects on gelatin-based edible films. Food Hydrocolloids 39:243–250. https://doi.org/10.1016/j.foodhyd.2014.01.026
Gomez CG, Rinaudo M, Villar MA (2007) Oxidation of sodium alginate and characterization of the oxidized derivatives. Carbohyd Polym 67(3):296–304. https://doi.org/10.1016/j.carbpol.2006.05.025
Wei Z, Gerecht S (2018) A self-healing hydrogel as an injectable instructive carrier for cellular morphogenesis. Biomaterials 185:86–96. https://doi.org/10.1016/j.biomaterials.2018.09.003
Ge L, Xu Y, Li X, Yuan L, Tan H, Li D, Mu C (2018) Fabrication of antibacterial collagen-based composite wound dressing. ACS Sustain Chem Eng 6(7):9153–9166. https://doi.org/10.1021/acssuschemeng.8b01482
Salazar G.M., Sanoh NC, and Penaloza DJP (2019) Synthesis and characterization of a novel polysaccharide-based self-healing hydrogel. KIMIKA, 29(2), 44–48. Available from https://kimika.pfcs.org.ph/index.php/kimika/article/view/264
Zhao W, Jin X, Cong Y, Liu Y, Fu J (2013) Degradable natural polymer hydrogels for articular cartilage tissue engineering. J Chem Technol Biotechnol 88(3):327–339. https://doi.org/10.1002/jctb.3970
Vahedi M, Barzin J, Shokrolahi F, Shorollahi P (2018) Self-healing, injectable gelatin hydrogels cross-linked by dynamic schiff base linkages support cell adhesion and sustained release of antibacterial drugs. Macromol Mater Eng 303(9):1800200. https://doi.org/10.1002/mame.201800200
Das S, Dalei G (2023) In situ forming dialdehyde xanthan gum-gelatin Schiff-base hydrogels as potent controlled release fertilizers. Sci Total Environ 2023:162660–162716. https://doi.org/10.1016/j.scitotenv.2023.162660
Khorshidi S, Karkhaneh A, Bonakdar S, Omidian M (2020) High-strength functionalized pectin/fibroin hydrogel with tunable properties: a structure–property relationship study. J Appl Polym Sci 137(28):48859. https://doi.org/10.1002/app.48859
Yao Y, Wang P, Li X et al (2020) A di-self-crosslinking hyaluronan-based hydrogel combined with type I collagen to construct a biomimetic injectable cartilage-filling scaffold. Acta Biomater 111:197–207. https://doi.org/10.1016/j.actbio.2020.05.007
Han Y, Zeng Q, Li H, Chang J (2013) The calcium silicate/alginate composite: preparation and evaluation of its behavior as bioactive injectable hydrogels. Acta Biomater 9(11):9107–9117. https://doi.org/10.1016/j.actbio.2013.06.022
Standardization., IOf (1992) ISO/EN 10993‐5: Biological evaluation of medical devices. Part 5. Test for cytotoxicity: In Vitro Methods. 8.2. Tests on Extracts.
Zhang S, Huang D, Lin H, Xiao Y, Zhang X (2020) Cellulose nanocrystal reinforced collagen-based nanocomposite hydrogel with self-healing and stress-relaxation properties for cell delivery. Biomacromol 21(6):2400–2408. https://doi.org/10.1021/acs.biomac.0c00345
Basu S, Pacelli S, Paul A (2020) Self-healing DNA-based injectable hydrogels with reversible covalent linkages for controlled drug delivery. Acta Biomater 105:159–169. https://doi.org/10.1016/j.actbio.2020.01.021
Chena H, Cheng J, Ran L et al (2018) An injectable self-healing hydrogel with adhesive and antibacterial properties effectively promotes wound healing. Carbohyd Polym 201:522–531. https://doi.org/10.1016/j.carbpol.2018.08.090
Xu J, Liu Y, Hsu S-h (2019) Hydrogels based on Schiff base linkages for biomedical applications. Molecules 24(16):3005. https://doi.org/10.3390/molecules24163005
Emami Z, Ehsani M, Zandi M, Foudazi R (2018) Controlling alginate oxidation conditions for making alginate-gelatin hydrogels. Carbohyd Polym 198:509–517. https://doi.org/10.1016/j.carbpol.2018.06.080
Peivandi A, Jackson K, He L et al (2021) Inducing microscale structural order in phage nanofilament hydrogels with globular proteins. ACS Biomater Sci Eng. https://doi.org/10.1021/acsbiomaterials.1c01112
Majchera MJ, Babar A, Lofts A et al (2021) In situ-gelling starch nanoparticle (SNP)/O-carboxymethyl chitosan (CMCh) nanoparticle network hydrogels for the intranasal delivery of an antipsychotic peptide. J Controll Release 330:738–752. https://doi.org/10.1016/j.jconrel.2020.12.050
Khorshidi S, Karkhaneh A (2016) A self-crosslinking tri-component hydrogel based on functionalized polysaccharides and gelatin for tissue engineering applications. Mater Lett 164:468–471. https://doi.org/10.1016/j.matlet.2015.11.041
Qian L (2018) Cellulose-based composite hydrogels: preparation, structures, and applications, in Cellulose-Based Hydrogels. Springer International Publishing AG New York. p. 1–50. doi: https://doi.org/10.1007/978-3-319-76573-0_23-1
Ngwabebhoh FA, Zandraa O, Patwa R, Saha N, Capakova Z, Saha P (2021) Self-crosslinked chitosan/dialdehyde xanthan gum blended hypromellose hydrogel for the controlled delivery of ampicillin, minocycline and rifampicin. Int J Biol Macromol 167:1468–1478. https://doi.org/10.1016/j.ijbiomac.2020.11.100
Tao Y, Liu S, Zhanf Y, Chi Z, Xu J (2018) A pH-responsive polymer based on dynamic imine bonds as a drug delivery material with pseudo target release behavior. Polym Chem 9(7):878–884. https://doi.org/10.1039/C7PY02108A
Iftime MM, Morariu S, Marin L (2017) Salicyl-imine-chitosan hydrogels: Supramolecular architecturing as a crosslinking method toward multifunctional hydrogels. Carbohyd Polym 165:39–50. https://doi.org/10.1016/j.carbpol.2017.02.027
Fedorovich NE, Kuipers E, Gawlitta D, Dhert WJA, Alblas J (2011) Scaffold porosity and oxygenation of printed hydrogel constructs affect functionality of embedded osteogenic progenitors. Tissue Eng Part A 17(19–20):2473–2486. https://doi.org/10.1089/ten.tea.2011.0001
Chang H-I, Wang Y (2011) Cell responses to surface and architecture of tissue engineering scaffolds: Med. Tissue Eng.—Cells Biomater, in: Regen, InTechOpen : p. 569–588. https://doi.org/10.5772/21983
France KJD, Xu F, Hoare T (2018) Structured macroporous hydrogels: Progress, challenges, and opportunities. Adv Healthcare Mater 7(1):1700927. https://doi.org/10.1002/adhm.201700927
Bueno VB, Bentini R, Catalani LH, Petri DFS (2013) Synthesis and swelling behavior of xanthan-based hydrogels. Carbohyd Polym 92(2):1091–1099. https://doi.org/10.1016/j.carbpol.2012.10.062
Ward D (2021) The development of novel hydrogel composites for use in bone tissue engineering Lancaster University (United Kingdom) 28447705. Available from https://www.proquest.com/openview/243ef9ce3d46e77ea09ead3b05db2162/1?pq-origsite=gscholar&cbl=2026366&diss=y
Loh QL, Choong C (2013) Three-dimensional scaffolds for tissue engineering applications: role of porosity and pore size. Tissue Eng Part B Rev 19(6):485–502. https://doi.org/10.1089/ten.teb.2012.0437
Karageorgiou V, Kaplan D (2005) Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26(27):5474–5491. https://doi.org/10.1016/j.biomaterials.2005.02.002
Madden LR, Mortisen DJ, Sussman EM, Ratner BD (2010) Proangiogenic scaffolds as functional templates for cardiac tissue engineering. Proc Natl Acad Sci 107(34):15211–15216. https://doi.org/10.1073/pnas.1006442107
Oliviero O, Ventre M, Netti P (2012) Functional porous hydrogels to study angiogenesis under the effect of controlled release of vascular endothelial growth factor. Acta Biomater 8(9):3294–3301. https://doi.org/10.1016/j.actbio.2012.05.019
Artel A, Mehdizadeh H, Chiu Y-C, Brey EM, Cinar A (2011) An agent-based model for the investigation of neovascularization within porous scaffolds. Tissue Eng Part A 17(17–18):2133–2141. https://doi.org/10.1089/ten.tea.2010.0571
Jang HY, Zhang K, Chon BH, Choi H-J (2015) Enhanced oil recovery performance and viscosity characteristics of polysaccharide xanthan gum solution. J Ind Eng Chem 21:741–745. https://doi.org/10.1016/j.jiec.2014.04.005
Yan S, Wang T, Feng L et al (2014) Injectable in situ self-cross-linking hydrogels based on poly (L-glutamic acid) and alginate for cartilage tissue engineering. Biomacromol 15(12):4495–4508. https://doi.org/10.1021/bm501313t
Tan H, Li H, Rubin JP, Marra KG (2011) Controlled gelation and degradation rates of injectable hyaluronic acid-based hydrogels through a double crosslinking strategy. J Tissue Eng Regen Med 5(10):790–797. https://doi.org/10.1002/term.378
Qu J, Zhao X, Ma XP, Guo B (2017) pH-responsive self-healing injectable hydrogel based on N-carboxyethyl chitosan for hepatocellular carcinoma therapy. Acta Biomater 58:168–180. https://doi.org/10.1016/j.actbio.2017.06.001
Bittner SM, Pearce HA, Hogan KJ et al (2021) Swelling behaviors of 3D printed hydrogel and hydrogel-microcarrier composite scaffolds. Tissue Eng Part A 27(11–12):665–678. https://doi.org/10.1089/ten.tea.2020.0377
Gupta V, Singh AK (2018) Stress relaxation at a gelatin hydrogel–glass interface in direct shear sliding. Mod Phys Lett B 32(02):1750345. https://doi.org/10.1142/S0217984917503456
Caccavo D, Cascone S, Poto S, Lamberti G, Barba AA (2017) Mechanics and transport phenomena in agarose-based hydrogels studied by compression-relaxation tests. Carbohyd Polym 167:136–144. https://doi.org/10.1016/j.carbpol.2017.03.027
Hanna DH, Lotfy VF, Basta AH, Saad GR (2020) Comparative evaluation for controlling release of niacin from protein-and cellulose-chitosan based hydrogels. Int J Biol Macromol 150:228–237. https://doi.org/10.1016/j.ijbiomac.2020.02.056
Vedadghavami A, Minooei F, Mohammadi MH et al (2017) Manufacturing of hydrogel biomaterials with controlled mechanical properties for tissue engineering applications. Acta Biomater 62:42–63. https://doi.org/10.1016/j.actbio.2017.07.028
Liu C, Wu J, Ganet D et al (2020) The characteristics of mussel-inspired nHA/OSA injectable hydrogel and repaired bone defect in rabbit. J Biomed Mater Res B Appl Biomater 108(5):1814–1825. https://doi.org/10.1002/jbm.b.34524
Wilson MA (2015) Structure and rheological properties of self-associating polymer networks San Diego State University. 3721326. Available from https://www.proquest.com/openview/38a7101f2f157a1dea91f7cff7c87cd2/1?pq-origsite=gscholar&cbl=18750
Tommasi G, Perni S, Prokopovich P (2016) An injectable hydrogel as bone graft material with added antimicrobial properties. Tissue Eng Part A 22(11–12):862–872. https://doi.org/10.1089/ten.tea.2016.0014
Giannoni P, Villa F, Cordazzo C et al (2016) Rheological properties, biocompatibility and in vivo performance of new hydrogel-based bone fillers. Biomater Sci 4(11):1691–1703. https://doi.org/10.1039/C6BM00478D
Hu C, Hahn L, Yang M, Altmann A, Stahlhut P, Groll J, Luxenhofer R (2021) Improving printability of a thermoresponsive hydrogel biomaterial ink by nanoclay addition. J Mater Sci 56(1):691–705. https://doi.org/10.1007/s10853-020-05190-5
Chen MH, Wang LL, Chung JJ, Kim Y-H, Atluri P, Burdick JA (2017) Methods to assess shear-thinning hydrogels for application as injectable biomaterials. ACS Biomater Sci Eng 3(12):3146–3160. https://doi.org/10.1021/acsbiomaterials.7b00734
Suna Y, Nan D, Jin H, Qu X (2020) Recent advances of injectable hydrogels for drug delivery and tissue engineering applications. Polym Testing 81:106283. https://doi.org/10.1016/j.polymertesting.2019.106283
Saunders L, Ma PX (2019) Self-healing supramolecular hydrogels for tissue engineering applications. Macromol Biosci 19(1):1800313. https://doi.org/10.1002/mabi.201800313
Wang H, Heilshorn SC (2015) Adaptable hydrogel networks with reversible linkages for tissue engineering. Adv Mater 27(25):3717–3736. https://doi.org/10.1002/adma.201501558
Rosales AM, Anseth KS (2016) The design of reversible hydrogels to capture extracellular matrix dynamics. Nat Rev Mater 1(2):1–15. https://doi.org/10.1038/natrevmats.2015.12
Adzima BJ, Kloxin CJ, Bowman CN (2010) Externally triggered healing of a thermoreversible covalent network via self-limited hysteresis heating. Adv Mater 22(25):2784–2787. https://doi.org/10.1002/adma.200904138
Xia NN, Xiong XM, Rong MZ, Zhang MQ, Kong F (2017) Self-healing of polymer in acidic water toward strength restoration through the synergistic effect of hydrophilic and hydrophobic interactions. ACS Appl Mater Interfaces 9(42):37300–37309. https://doi.org/10.1021/acsami.7b11230
Fairbanks BD, Singh SP, Bowman CN, Anseth KS (2011) Photodegradable, photoadaptable hydrogels via radical-mediated disulfide fragmentation reaction. Macromolecules 44(8):2444–2450. https://doi.org/10.1021/ma200202w
Quan L, Xin Y, Wu X, Ao Q (2022) Mechanism of self-healing hydrogels and application in tissue engineering. Polymers 14(11):2184. https://doi.org/10.3390/polym14112184
Billiau A, Edy VG, Heremans H, Damme JV, Desmyter J, Georgiades JA, Somer PD (1977) Human interferon: mass production in a newly established cell line, MG-63. Antimicrob Agents Chemother 12(1):11–15. https://doi.org/10.1128/AAC.12.1.11
Czekanska EM, Stoddart MJ, Richards RG, Hayes JS (2012) In search of an osteoblast cell model for in vitro research. Eur Cell Mater 24(4):1–17. https://doi.org/10.22203/ecm.v024a01
Jahan K, Manickam G, Tabrizian M, Murshed M (2020) In vitro and in vivo investigation of osteogenic properties of self-contained phosphate-releasing injectable purine-crosslinked chitosan-hydroxyapatite constructs. Sci Rep 10(1):1–17. https://doi.org/10.1038/s41598-020-67886-7
Acknowledgements
This research was financially supported by a grant from Iran National Science Foundation (INSF) (no. 4013250) which is greatly appreciated. The authors would also like to warmly appreciate Dr. Sajedeh Khorshodi, Dr. Reza Karimi, Mr. Amir Hossein Rasooli, and Mr. Yaghoub shavehei from the Amirkabir University of Technology for their scientific consults. Also, the authors declare no potential conflicts of interest.
Author information
Authors and Affiliations
Contributions
MA was involved in experimental design, carrying out measurements and manuscript composition. RI took part in conceptualization, supervision, project administration, validation, funding acquisition, writing—review & editing. MH was involved in conceptualization, supervision, review & editing.
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical approval
Not applicable.
Additional information
Handling Editor: Annela M. Seddon.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aghajanzadeh, M.S., Imani, R. & Nazarpak, M.H. In situ forming aldehyde-modified xanthan/gelatin hydrogel for tissue engineering applications: synthesis, characterization, and optimization. J Mater Sci 58, 14187–14206 (2023). https://doi.org/10.1007/s10853-023-08878-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-023-08878-6