Abstract
The present study aims to collect data, compare results and assess techniques used for improving corrosion resistance and mechanical properties of biodegradable Mg alloys for fixation elements and orthopedic applications. A general description of biomaterials used for orthopedic implants is performed, including non-bioabsorbable materials. Different methods for reducing the corrosion rate in Mg alloys are researched, and the efficiencies are assessed. After evaluating different techniques, surface modification is found to be the most promising technique to reduce the corrosion rate with an efficiency of 85%. Regarding the Mg alloying agents, Zn is considered as the best candidate to improve the corrosion response and biocompatibility of the Mg.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The acceleration in the aging of the population has resulted in millions of people suffering of bone damage caused by aging and diseases (osteoporosis and necrosis of bone tissue) and accidental injuries, which is why the treatment of bone defects has become the main clinical operation [1,2,3,4]. Therefore, in order to develop biomaterials with characteristics similar to bone, it is necessary to study their chemical composition and mechanical properties.
Human bone is a structure made of fat, an organic phase composed of a structural protein, type I collagen, bone morphogenetic proteins (BMPs), minerals and water [1,2,3,4,5]. Of these elements, the calcium hydroxyapatite (Ca10[PO4]6[OH]2) is the main component of the bone. This mineral is a metabolically active tissue that works as a reservoir for essential electrolytes, such as magnesium and zinc [6]. Hydroxyapatite (HA) crystals are oriented in a periodic matrix in the fibrils with their axis parallel to the collagen fibers. The function of HA crystals and collagen molecules is to provide flexibility, strength and toughness. These two components represent approximately 95% of the dry bone [1, 6]. The bones can be classified as compact bones (cortical bones) and trabecular bones (cancellous bones). Compact bones are nearly solid with only from 3 to 5% spaces for osteocytes, canaliculi, blood vessels and erosion cavities. The pores of the trabecular bones are filled with bone marrow, and the porosity varies between 50 and 90% [5].
From a biological point of view, bone is a complex tissue that continuously undergoes dynamic biological remodeling, in where osteoclasts reabsorb mature bone tissue, while osteoblasts generate new bone to maintain healthy bone homeostasis. This regeneration process gives to the bone the capability to rebuild itself to repair damage. However, when a bone damage exceeds a critical size (approximately greater than 1cm3), bone regeneration is not possible [7, 8]; therefore, external intervention is required to help the bone’s self-healing [5, 8,9,10,11]. To achieve a proper reconstruction and tissue regeneration at the location of the bone defect and to recover the functionality of the region, different researchers have carried out relevant investigations. However, the repair of such a critical bone defect remains to be a challenge due to the complexity of the factors that affect the treatments such as the location and length of the damage or defect, the state of the soft tissue capsule, the mechanical stress and movements of the affected bone, age, metabolic diseases and complications related to the patient's health status [9, 12]. One of the best options for an intervention, according to the authors, is the use of autografts made from the own patient bone avoiding a possible immune rejection. However, the autograft is usually limited in size and quality, which generally carries a risk of complications such as donor site morbidity and prolonged operation time and leads to additional trauma to the bone [5, 9, 13, 14]. Another option is the use of allogeneic bone, but this implants usually lead to immune rejection, disease transmission, and it is associated with an increment in the possibility of suffering a cross-infection and a slower healing process. Consequently, the alternative of use artificial bone implants made of biomaterials, recently, has emerged [5, 9, 10, 15,16,17].
On the other hand, the main aims of an implant are to restore bone functionality and to promote the regeneration of the bone’s tissue. Therefore, it must fulfil the following requirements: (i) good biocompatibility, including histocompatibility and blood compatibility; (ii) to guarantee the surface material is suitable for cell adhesion, proliferation and differentiation; (iii) to contain a network of interconnected pores for cell growth and the transport of nutrients and metabolic waste; (iv) suitable mechanical properties that: allow a positive performance of the implant to the necessities of surrounding tissues, minimize stress shielding and bear anatomical load requirements to avoid mechanical failure [4, 4, 5, 15, 18,19,20,21,22,23].
Material selection is the starting point for designing a successful implant, since chemical composition and microstructural arrangement play an important role in biocompatibility and mechanical properties [23, 24]. In addition, the reaction of the material within the human body is also an important factor to be considered as the release of ions from implants due to corrosion or excessive wear which can trigger inflammation and potentially initiate various complex allergic reactions. These undesired effects cause the destruction of the host's tissues followed also by implant loosening. Similarly, the mismatch between the elastic modulus of the bone and biomaterials leads to stress shielding in the surrounding bones causing bone resorption [5, 21,22,23, 25]. Therefore, researchers have focused on the selection of non-cytotoxic materials with morphology and mechanical properties similar to bone [26].
Regarding mechanical properties of the bone, such as tensile strength, elastic modulus, hardness, toughness and stiffness, they usually vary significantly with the patient’s age, anatomical location and bone quality. The mechanical property of the bone that has attracted the most research interest has been the elastic modulus because of its relevance upon characterizing some bone pathologies and as a key restriction in the design of artificial implants. Designing a bone implant is also important considering the anisotropic properties of the bone; for example, compact bone is stronger and more rigid when loaded longitudinally along the diaphyseal axis than transverse in the radial directions (as shown in Table 1). Compact bone is also stronger in compression than in tension. On the other hand, trabecular bone shows time-dependent behavior, as well as susceptibility to damage under cyclical loading. The mechanical properties of trabecular bone depend not only on porosity, but also on the architectural arrangement of individual trabeculae [5].
In clinical cases, orthopedic fasteners are frequently utilized during the healing process of the bone to provide enough support; however they are required only temporarily until the bone functions have been restored. Once the bone has healed, fasteners are removed, which can be avoided using biomaterials that are degraded naturally inside the human body. Therefore, a key parameter that must be considered for designing a temporary implant using biomaterials is the degradation rate of the material within the human body, where the inorganic ions (e.g., Ca2+, Cl−, OH−, HPO42−, H2PO4−, HCO3− and CO32−) and the organic molecules (e.g., glucose, amino acids and proteins) are the main factors influencing implant degradation [5, 28]. Traditionally, fixation elements for bones, such as screws, nails and plates, are made of 316 L steel or Ti alloy. However, they present a much higher Young’s modulus than natural bone. Therefore, the implant bears most of the load that the bone normally undergoes resulting in a low stress level for the defective bone. Insufficient mechanical stimulation over a prolonged period can cause osteoporosis and other undesirable consequences [15]. In addition, as the orthopedic fasteners are usually structural elements made of materials with good corrosion resistance, once the healing process is finished, the osteosynthesis material is extracted, which requires a second surgical intervention. Nevertheless, bioabsorbable or biodegradable metals can be considered as a new class of promising biomaterials for temporary medical implant applications, which allow the replacement of biological tissues and physiological extracellular components without leaving toxic corrosion products. It is important to point out that corrosion products must not present any toxicity to their surroundings [19]. Thus, biodegradable metals used for implant applications must have an optimal balance between maintaining enough mechanical resistance while the healing process is ongoing and the gradual material degradation [29]. On the one hand, adequate mechanical support in the early stage of the healing process is required in order to obtain good results. On the other hand, it is also desired (to avoid stress shielding) dynamic degradation of the implant in order to decrease the capacity of load support gradually increasing the mechanical stimulation upon the bone progressively. Therefore, a degradation rate higher than the bone remodeling rate can affect the bone regeneration, because of premature loss of mechanical integrity [15, 30, 31].
Currently, a wide variety of new materials have been proposed for designing orthopedic applications, including metallic, ceramic, polymeric and even composite or hybrid materials. Due to their mechanical properties that are similar to bone, machinability and biocompatibility of the degradation products, biodegradable metallic materials have received significant attention in recent investigations. However, the low corrosion resistance of these materials remains a challenge for biomedical applications, which has attracted the attention of numerous studies. Therefore, the present research work performs a review of the state of the art, including the different materials that have been historically used for orthopedic applications and the role of magnesium alloys. Subsequently, we analyze different manufacturing methodologies, as well as surface and structural modifications that are implemented to improve the corrosion resistance of magnesium.
Using the VOSviewer software [32], a keyword co-occurrence plot is made. Figure 1 shows the results of a search carried out in Web of Science database with the keywords "Orthopedic implant" and filtered with the following keywords independently: “titanium,” “stainless steel,” “polymer,” “biodegradable material,” “biodegradable Mg” and “biodegradable composites” from 2000 to 2021. This search yields the most researched terms during the last 21 years, and it allows us to visualize how the development of biomaterials research has evolved. Figure 1 indicates that for materials used for permanent implants, titanium highlights in a dark blue tone, which corresponds to periods around 2016. However, as a biodegradable material, Mg alloys appear on the left side of the graph in a lighter tone, indicating that such alloys have begun to gain relevance from mid-2017. The research interest in the Mg alloys has been focused mainly on corrosion resistance. Therefore, it is possible to demonstrate the research trend toward the development and optimization of biodegradable alloys. For this reason, the search and compilation of data, techniques and fundamentals carried out in this article for the optimization of the properties of biodegradable magnesium alloys for fixation elements and orthopedic applications are justified.
Materials for orthopedic implants
In order to determine and contrast the most promising biomedical materials, which are used for orthopedic applications, an extensive study of the state of the art is carried out to identify the families of materials that are commonly used and investigated for designing and machining fixation elements. The CES Edupack software [33] and the scientific databases (Web of Science, Science Direct and Springer) are used for stablishing eight main classes of materials, viz. titanium-based alloys, Cr–Co alloys, iron-based alloys, zinc-based alloys, magnesium-based alloys, polymers, ceramics and composite materials with a metallic matrix of magnesium. Subsequently, elastic modulus and the respective density are collected and summarized in Fig. 2.
One of the factors to be considered when selecting a material for orthopedic implants is the closeness of the mechanical properties of candidate materials to the target bone properties because the mechanical response of the implant is similar to the bone response preventing stress shielding. In Fig. 2, a comparison of the elastic module of cortical bones and materials frequently used for implant applications is performed. Figure 2 shows that the closest materials to the femur cortical bone, regarding Young’s modulus and density, are the Mg and Zn alloys, composites of Mg matrix and polymers. Additionally, it is observed that materials commonly used for orthopedic applications (such as Ti alloys, stainless steels and Cr-Co alloys) are non-bioabsorbable metals even though their mechanical properties differ considerably in comparison with the bone properties. Bioabsorbable or biodegradable materials can degrade in the human body through electrochemical processes such as corrosion and can be metabolized by cells and tissues without compromising the health of the host [58, 59]. When non-bioabsorbable materials are used for fixation elements, a second surgical intervention is mandatory to remove the fixation material. Therefore, a study of different materials for biomedical applications is carried out classifying them into non-bioabsorbable and bioabsorbable materials.
Non-Bioabsorbable materials for orthopedic applications
Materials with high corrosion resistance used for biomedical applications are polymers such as polymethyl methacrylate (PMMA), polylactic acid (PLA) and polyglycolic acid (PGA) and metals such as CoCr alloys, stainless steels and Ti and its alloys. According to Fig. 2, the polymers have densities and Young's modulus very similar to bone. Regarding metallic materials, which present values of density and Young's modulus much higher than cortical bone (as shown in Fig. 2), they are commercially well accepted for permanent implants. A brief description of their advantages, applications and challenges is given below.
Non-bioabsorbable metal alloys
Currently, metal alloys that are conventionally utilized for orthopedic applications have a high corrosion resistance and biocompatibility [60]; for instance, Ti is an inert and safe material, which is widely used for permanent invasive implants. Ti produces minimum no desired effects on the patient, due to the high resistance to corrosion caused by the formation of a thick and rapidly regenerating oxide layer providing a strong corrosion protection. This metal (Ti) can integrate easily with hard tissues, because bone minerals are formed on the surface promoting the osteoregeneration [39, 61]. Ti also has a lower Young's modulus compared to stainless steels and cobalt alloys [on average 49% less than cobalt–chrome alloys and 53% less than stainless steel (Fig. 2)]. Thus (for all these reasons), use of Ti is presently widespread in its pure state for implants and orthopedic prostheses. Ti alloys are even suitable for allergic patients to metal. They are used for fracture repairs and total hip and knee arthroplasty, due to its high strength per unit mass, low density compared to steel (4.5 g/m3, [62]) and low surface hardness (approximately 70 HB [61]). However, due to their biomechanical incompatibility, high Young's modulus compared to bone (55–110 GPa [61]) and low resistance to wear, Ti alloys are not used as fixation elements [37, 39, 62,63,64]. For orthopedic applications, the most used Ti alloys are Ti6Al4V and Ti grade 4, because they are Ti alloys commercially available with the highest mechanical resistance [65]. However, there are other alloys that are worth mentioning, such as nitinol which is a nickel and titanium alloy. Nitinol has shape memory properties, and it is used in orthopedics to treat cases of ruptured tendons and torn ligaments [66, 67].
Stainless steel is other material that has been successfully used for implants applications; in fact, it was the first material utilized for designing modern orthopedic implants due to its high corrosion resistance and biocompatibility [68]. For medical applications, stainless steel contains molybdenum (2–3% wt), chromium (16–18% wt), manganese (≤ 2% wt), carbon (0.030–0.08% wt), nickel (8–14% wt), phosphorus (0.05% wt), nitrogen (0.10% wt) and sulfur in small proportions (0.03% wt) [69,70,71]. This steel has a high toughness, good manufacturability and low cost compared to other alloys. However, it has low fatigue and wear resistance. Regarding, Young's modulus (approx. 193GPa) is higher than Ti (approx. 96.87 GPa [37]) and the bone (see Table 1). Stainless steel does not promote the formation of natural bonds with bone which can lead to implant failure and can suffer from poor corrosion resistance in physiological fluids causing the release of corrosion products and Ni ions that are harmful to the body [39, 45, 72,73,74]. The most used stainless steel for fixation elements such as plates, bone screws and permanent implants is 316L [39].
Chromium–cobalt are other non-bioabsorbable metal alloys that are widely used for different biomedical applications, such as dental implants, due to their excellent mechanical properties, such as high tensile strength (758.73 ± 25.85 MPa), high wear resistance and hardness (~ 330 HV) [62, 75,76,77]. The chromium–cobalt alloys also exhibit a high corrosion resistance, due to a protective film of chromium oxide that appears on the surface of these alloys [78]. Another suitable orthopedic application for such alloys is arthroplasty devices, especially hip implants, because of their resistance to torque and abrasion [79]. However, the high Young's modulus (approx. 210–220 GPa [80], see Fig. 2) can generate stress shielding, and some allergic reactions can be caused by undesired corrosion products from the cobalt alloys [62]. Also, the release of chromium and cobalt ions may lead to increase the possibility of tumor formation [81, 82].
Non-bioabsorbable polymers
Polymeric materials have been successfully utilized for biomedical applications. They have some advantage such as good biocompatibility, low density and ease of synthesis. Polymethyl methacrylate (PMMA) is one of the most used thermoplastic materials for biomedical applications, due to its good processability, adequate mechanical properties and high biocompatibility. Since mid-twentieth century, PMMA is combined with liquid methyl methacrylate (MMA) to create a bone cement for orthopedic applications [83]. PMMA is a thermosetting polymer; i.e., viscosity of this material is not affected significantly by changes in the temperature; therefore, it is considered nowadays as a main element for manufacturing bone cements for fixation of the stem in hip and total knee replacements surgeries [39].
Polymers are also used for cranial orthopedic applications as an alternative for titanium alloys. Polyester ether ketone (PEEK) provides excellent mechanical properties and long-term biocompatibility, ideal for this type of neurosurgical applications [84]. Ultra-high molecular weight polyethylene (UHMWPE), which was first synthesized in the middle of the twentieth century by Karl Ziegler, has a low coefficient of friction, high impact resistance, good wear resistance, excellent biocompatibility and low cost. Therefore, it has been used for over 50 years in total hip and knee implants [39, 85]. However, although UHMWPE exhibits good wear resistance, the material response when there is contact among components must be improved [85]. Over the years, new manufacturing processes have been proposed to improve the wear resistance of UHMWPE, such as cross-linking, which allows carbon atoms from different polyethylene chains joining together and creating more stable three-dimensional structures with higher tear and wear resistance. The cross-linking process does not affect the density or the ultimate tensile strength of the material [86]. New surface finishes have been engineered to allow fluid build-up to make the polymer more resistant and improve lubrication [87]. Irradiation of UHMWPE with antioxidants, especially with α-tocopherol, improves the fatigue and corrosion resistance, extending the useful life and stability of the implant over time [88]. The main challenge about polymers for biomedical applications has been to improve mechanical properties in order to withstand the loads that human bones usually undergo.
In Table 2, the main differences between non-bioabsorbable metals and polymers are summarized.
Bioabsorbable materials for orthopedic applications
Bioabsorbable or biodegradable materials have been the focus of the recent investigation on implant materials due to their potential use in temporary implants and fixation elements. Using these types of materials for orthopedic implants, it is possible to avoid the need for a second surgical intervention to remove the implant, because the body itself can reabsorb the biodegradable material. Therefore, risks associated with the patient's surgery are reduced, time required for postoperative physical rehabilitation process is diminished, and the cost inherent to the clinical procedures is also lowered. The biodegradable materials in Fig. 2 are alloys and composites of Mg and Zn. Currently, these are the most investigated biomaterials, and the use of these materials in orthopedic applications is expected to increase in the coming years. The alloys and composites of Mg in Fig. 2 have mechanical properties closer to the bone, and they are also suitable for using as fixation and load bearing elements. Therefore, these materials do not damage the bone due to stress shielding.
Bioabsorbable polymeric materials
The first developed and the most used biodegradable materials for commercial implants are polymeric, which are obtained from polyglycolic acids (PGA), polylactic (PLA) and polylactic glycolic acid (PLGA). Biodegradable polymers have been successfully utilized for several biomedical applications including suture threads, drug delivery devices and in the orthopedic industry as pins and screws [57, 60, 92]. Polymers are manufactured through a wide range of methods, such as additive manufacturing, which allows to create custom-made parts economically and with controlled porosity [93, 94]. However, polymeric materials still have some challenges regarding the mechanical properties that must be addressed, which limit the use in orthopedic applications.
Shape memory polymers are promising solution for new surgical and medical devices for special applications like self-fastening stitches and suture less devices, and additionally to temperature changes, shape memory materials can be driven by pH, light and other physical effects. These materials are known for their good biocompatibility and biodegradability and open a new whole universe of smart applications within the body [95].
Polymers like PLA have been used for developing self-fastening elements with shape memory materials. However, these materials are not strong enough to hold weight loading bones. As an alternative to improve the mechanical properties of polymers, Liu et al. [96] developed a triple shape memory polymer, using a highly oriented poly(lactic acid)-b-poly(lactide-co-caprolactone) (PLA-b-PLCL), expecting a decrease in the glass transition temperature, to a range including the body temperature and higher tensile strength and modulus.
Bioabsorbable metallic materials
Biomedical metallic materials that are currently used can be harmful to the human body in the long term due to metallic particles that are released and accumulated by means of degradation and corrosion of the material. Therefore, metallic materials for temporary implants must have excellent biocompatibility and bifunctionality, adequate load capacity, high wear resistance, low density, and a gradual and controlled biodegradation rate that allows once the bone is healed; then, reabsorption of the biodegradable material is completed [60]. Appropriate selection of biodegradable materials reduces the health risks associated with the use of implants and a second surgery to remove the implant after the tissue has healed [97].
Zinc-based metal alloys have good biocompatibility, high bioabsorbability (up to 15 mg/day [98]), ideal corrosion rate in vitro (approximately 0.022 mm/year [99]) and relatively low Young's modulus (80–90 GPa, see Fig. 2). Zinc is essential for the normal operation of human body; for instance, it is indispensable for heart functioning and protects endothelial cells [100]. Zinc alloys do not produce harmful gases during biodegradation, and the corrosion products are biocompatible and harmless [100]. The low melting temperature of these alloys and the low reactivity during melting allow successfully casting components [98, 100]. All these advantages justify the successful use of the zinc alloys as biodegradable implant material. However, zinc alloys implants are limited in size, because they are brittle, have low mechanical properties and show poor ductility under compression loading. In addition, production costs are relatively high for these alloys due to the high purity elements that are required in the fabrication process of the zinc alloys [98, 101].
Magnesium alloys
As zinc, magnesium is an indispensable element for the proper functioning of the body. Human body contains approximately 23 g/kg of magnesium, and the amount of Mg ions (Mg2 +) in the blood is estimated at 0.00070–0.0011 M. Magnesium is nontoxic in concentrations up to 1.05 mM and plays a vital role in inhibiting abnormal nervous excitability. Magnesium also participates in protein synthesis, prevents atherosclerosis and helps to reduce the risk of developing hypertension [65]. Its deficiency could inhibit muscle growth and affect the properties of skeletal muscle [102]. Therefore, magnesium alloys are strong candidates for degradable biomaterials used for temporary implants including in applications such as traumatology, cardiovascular, maxillofacial and dentistry. Currently, these alloys are successfully used for different applications such as components for bone fixation and osteosynthesis, cardiovascular devices such as stents or catheters, even cavity filling materials and as a barrier in dental implants [60, 103,104,105,106,107,108]. Unlike Ti alloys and stainless steel, magnesium reacts with the body's physiological fluids to form soluble and nontoxic products, which are eliminated through urine without generate any health risks. Mechanical properties of most magnesium alloys, viz. Young's modulus (~ 47GPa), UTS (86.8–300 MPa), elongation at break (3–30%) and density (~ 1.74 g/cm3), are close to the properties of human bone as shown in Fig. 2, reducing the possibility of generating stress shielding [45, 109,110,111]. Magnesium alloys have high machinability and can achieve precise final dimensions; therefore, complex components are possible to manufacture with tiny tolerances. Due to the high toughness, magnesium alloys are suitable for using in components for load-bearing applications [112,113,114]. However, these alloys corrode rapidly in aqueous solutions (0.39 mm/year in EBSS [96], 1.39–1.88 mm/year in SBF and 0.25–2.05 mm/year in Hank's solution [115,116,117]). The high corrosion rate of magnesium generates health hazards, such as osteolysis causing degeneration and weakening of the bones and loss of mechanical integrity of the implants. It also produces a high volume of hydrogen gas (H2) (approximately 1 ml/mg of Mg), which promotes formation of gas bubbles in the adjacent tissues raising pH levels of the medium and delaying the healing process [109, 113, 118, 119]. Therefore, controlling the corrosion rate in these alloys is one of the greatest challenges to be faced. It is also indispensable to identify the different mechanisms that can be used for reducing the degradation rate and the hydrogen evolution.
Corrosion behavior of magnesium alloys
Magnesium is one of the most chemically active metals due to its low reduction potential [117, 120]. Table 3 shows the position and potential of Mg in contrast to Zn, Fe and Ag, materials that have been used previously for clinical applications, compared to the standard hydrogen electrode. Therefore, magnesium is widely used as the main element in sacrificial anode coatings to protect other metals from corrosion [121,122,123].
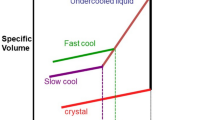
During the corrosion process of metallic implants installed within the human body, various factors affect the corrosion behavior of the material. For magnesium alloys, the most critical factor is the local pH level, which determines the nature and characteristics of the resulting corrosion products. Figure 3 shows the Pourbaix diagram of magnesium in water at a temperature of 25 °C. In this figure, the resulting magnesium products are stablished for different environment pH levels. On one hand, in environments with high pH, viz. pH > 11.5, stable magnesium hydroxide is generated. This base acts as a protective layer on the surface reducing implant corrosion. On the other hand, when the pH around the implant is less than 11.5, Mg(OH)2 is unstable and hydrogen gas is produced, which negatively affects the body and the patient's recovery [124]. Usually, after a surgery the pH surrounding the implant is between 5.3 and 7.4, due to secondary acidosis which is generated by metabolic process and postsurgical reabsorption [104] The low pH level together with the natural chlorine electrolyte of the physiological system accelerates the corrosion of the magnesium, promotes the formation of cracks and small defects in the components and, in combination with the microorganisms in the body’s environment, reduces the oxygen concentrations in the affected zone [104, 125].
PH-potential diagram (Pourbaix) for Mg in water at 25 °C [117]
The chemical reaction that occurs during theorrosion process of magnesium in an aqueous medium is given by [126, 127].
Reaction (1) is obtained as result of the following partial reactions [126,127,128]:
The cathodic reaction releases considerable amount of H2, and the compound reaction drives the passivation of the surface due to the formation of the hydroxide layer Mg(OH)2. However, within the human body, the protective effect of this layer decreases due to the presence of chlorine ions in the body environment surrounding the implant. The magnesium hydroxide reacts with the chlorine and yields water-soluble magnesium chloride, when the concentration exceeds 30 mmol/L. This compound, generated on the surface, deteriorates and significantly reduces the corrosion resistance obtained by means of forming the magnesium hydroxide layer [126, 127].
Parameters such as composition, porosity, grain size and presence of second phases influence the corrosive behavior of magnesium alloys [126]. In particular, grain size is a critical factor that not only influences the corrosion of metals, but also determines mechanical properties such as elastic limit and hardness [129]. Grain boundaries are high-energy regions in the microstructure; therefore, the corrosion rate of metals tends to increase if the grain size is smaller, because the number of grain boundaries increases with the grain refinement [129]. Monocrystalline materials have a low corrosion rate, viz. ∼ 0.5 µm/day in simulated body fluid (SBF) with the packed orientation as the basal plane [129]. For example, Mathieu et al. [130] investigated the correlation between corrosion resistance and microstructure of sem-solid cast magnesium alloys (AZ91D). The results indicate that the casting method influences the corrosive behavior of the alloys by controlling the microstructure of the material. The strength of the semisolid cast alloy was 35% higher than that exhibited by the same high-pressure cast alloy with the same level of impurities. The authors conclude that, regardless of the corrosion evaluation method, the difference in the corrosion resistance of the evaluated specimens should be attributed solely to the microstructural conditions resulting from their manufacturing process.
The galvanic corrosion that occurs between the intermetallic phases and the Mg alloy matrix is a factor that strongly influences the corrosion behavior. The potential difference that forms between the intermetallic phase and the matrix induces the electrons to move from anode to cathode forming galvanic cells. The second anodic phases degrade when they meet a more noble matrix in a galvanic cell; in opposite, the matrix corrodes when the second phase is more noble than the matrix. By increasing the voltage power difference between the intermetallic phase and the matrix, the corrosion rate of the base material increases. Likewise, an increase in the fraction of the second phase provides more active galvanic cells; therefore, the affected area will increase its corrosion rate linearly [129].
The release of hydrogen gas is inherent in the corrosion process of magnesium and one of the most important factors to control when working with this material for clinical applications. The release rate of H2 during Mg corrosion at 37 °C (average body temperature) is 40 ml /cm2/day, and the human body's absorption rate of these ions is 2.25 ml /cm2/day. Excess ions cannot be absorbed, they accumulate as gas bubbles in the tissues, and they can disappear after a while or be eliminated through a puncture which can cause discomfort in the patient [97, 131, 132].
Several studies have been reported on the effect of magnesium corrosion products as corrosion inhibitors and the properties of the oxide films formed: An investigation by Zuo et al. [133] evaluated the behavior of pure magnesium (HP-Mg) in three simulated human fluid media corresponding to SBF, bile and simulated urine. The results show that after immersion of HP-Mg in SBF and bile, no crystalline structures are evident in corrosion products. Paired analysis of EDS and XDR by the authors concludes that resulting precipitates are amorphous calcium/magnesium phosphate and calcium/magnesium carbonate. Additionally, a decrease in the corrosion rate is observed as well as a reduction of corrosion products with amorphous crystalline structure emitted to the human body, which reduces the possibilities of developing problems such as biliary occlusion.
Likewise, S. Feliu (Jr) and I. Llorente [134] evaluated the changes in the chemical composition of the alloys AZ31 and AZ61 in solutions at 0.6 M NaCl. The results show that the magnesium corrosion proceeds with the release of hydrogen bubbles and the release of OH- ions, increasing the pH of the surrounding medium. It is concluded that the relationship between the pH of the medium and the corrosion rate is direct: By increasing the corrosion rate, the pH can take values between 10.5 and 11; on the contrary, with lower corrosion rates, the pH will be less than 10.5. However, strategies have been implemented to minimize the degradation rates of Mg alloys to ensure proper tissue healing without affecting the health of the patient, as shown in the next section.
Mechanisms to control the degradation of magnesium alloys
In the last decades, different strategies have been investigated to control the degradation rate of magnesium alloys, including microstructural and surface modification techniques [118, 135]. The first approach involves the microstructural modification of the magnesium alloy using relatively noble elements such as aluminum [136], zinc [137], manganese[23], calcium [119], lithium [118], yttrium, zirconium, silicon, strontium [64, 138], scandium and rare earth elements, or physical modifications such as mechanical treatments, manufacture of metallic glasses or plastic deformations associated with laminating, stretching, or extrusion processes [118]. Regarding surface modifications, the second approach involves noble coatings to control the corrosion rate of these alloys, and finally, the third approach studies microstructural modifications through the development of magnesium matrix composite materials to optimize mechanical properties and improve corrosion resistance.
Mg alloys
The effects of some of these elements on magnesium are shown in Table 4.
Coating techniques
The second approach proposes the modification of the surface of magnesium alloys to improve their behavior in corrosive environments and provide better mechanical and biological properties [152]. Currently, techniques such as anodization, micro-arc oxidation, ion implantation, chemical conversion coatings, electrophoretic deposition, physical vapor deposition (PVD) and chemical vapor deposition (CVD) are used [118].
Micro-arc oxidation (MAO) or electrolytic plasma oxidation is a technique that applies high potentials that exceed the dielectric breakdown power limit of the growing oxide layer, producing discharges that result in localized plasma reactions under specific conditions of temperature and pressure, which modifies the oxide. This coating is a chemical conversion of the substrate to its oxide and causes its porous growth in all directions of the metal surface, which produces excellent adhesion to the material, provides protection against wear, abrasion and corrosion. In magnesium alloys, the coatings are relatively thick, dense and hard, and it is possible to absorb some elements contained in the solutions improving the chemical and functional properties of the surface, increasing the magnesium corrosion resistance and favoring their use in biomedical applications [113, 153,154,155]. The coatings made by MAO depend on the concentrations and compositions of the electrolytes, the microstructure of the substrate, the electrical parameters and the compositions of the alloy. [153].
Chemical conversion coatings involve the complex interaction of dissolution and precipitation of metallic substrates in saline or acidic aqueous solutions. The surface layer is obtained by immersing the substrates in baths, which specifically, for magnesium alloys, obtain magnesium oxide or magnesium hydroxide and mixtures of other metal-type oxides and hydroxides that result from the ions dissolved in the solution. This type of coating is effective in increasing the corrosion resistance of these alloys [31].
Likewise, electrophoretic deposition (EPD) includes techniques such as cathodic electrodeposition, electropherical coating and anodic electrodeposition. These methods are carried out through the deposition of inorganic phases on the surfaces by an electric field starting from colloidal particles suspended in a charged or liquid medium [31]. EPD is a versatile coating technique and facilitates the use of biomaterials such as hydroxyapatite and hydroxyapatite-polymer coatings, calcium and magnesium silicates and carbon nanotubes. The necessary equipment is simple and provides control over the micro- and macrostructural characteristics and dimensions of the coating, and the mechanical and thermal properties of the materials used in orthopedic applications [154]. This methodology has been used on magnesium alloys previously achieving outstanding results: Kumar et al. coated a Mg–3Zn alloy with hydroxyapatite, achieving a 25-fold improvement in the corrosion resistance of the alloy, the viability of the surface, the electrochemical stability of the substrate and increasing the growth of bone cells on the surface of the alloy [156].
Physical vapor deposition (PVD) requires the atomization of a condensable material through the application of heat, an energy beam or electric arc within a vacuum chamber, causing the vaporized material to condense on the substrate. PVDs allow the depositing of complex or multilayer coatings with specific electrical, physical and magnetic characteristics. However, the pressure of the vacuum chamber is an important variable given its effect on the integrity of the coating; therefore, multilayer processes are more difficult to control [157]. Among the PVD techniques, magnetron sputtering stands out, where the coating is formed by spraying a "target" material into fine particles by the bombardment of argon atoms and the application of a magnetic field around it, and then the particles are deposite on the substrate [158]. Few metals can be treated under this technique due to compatibility with sutrates [140]. In magnesium alloys, titanium [159, 160], ZrO2 [155], ZrN [161], TiN [161], AlN [161] and TiMgAlN [162] have been deposited in order to improve the hydrophilicity of the material, provide uniform layers that increase the surface properties of the material and improve corrosion resistance and protection against wear [163,164,165,166].
Chemical vapor deposition (CVD) achieves high-quality and high-performance coatings. The process consists of exposing the substrate to one or more volatile precursors that react and/or decompose the surface, achieving the required coating. Unwanted volatile by-products are removed by a gas flow [154]. The properties of the deposited films depend on the gas flow rate, the substrate temperature, the energy source and the deposition rate [167]. Among CVD techniques, hydrothermal deposition allows to create a uniform and compact protection layer against corrosion in magnesium alloys with an excellent adhesion strength and viable for use in orthopedic applications. This coating has an adjustable degradation rate by variating the temperature and deposition time during the process [168,169,170]. Solgel deposition, also known as chemical solution deposition, produces high adhesion coatings and requires low surface preparation of the substrate. This process involves the synthesis of materials by a chemical solution that produces hydrolysis and condensation reactions of metal alkoxides that act as precursors of an integrated network of polymers, also called gel, which are deposited on the surface of the material [4, 152]. This technique allows the deposition of ceramic ultrastructure at room temperature [154, 171]. In magnesium alloys, bioactive silica glasses (58S and 68S)[172], hydroxylated nanodiamonds [173], silane/Mg(OH)2 [174], collagen and chitosan [175], and even natural organic inhibitors like quinaldic acid, betaine, dopamine hydrochloride and diazo-collagen and chitosan lidinyl urea [176] have been deposited by solgel systems, achieving thin, uniform, bioactive and flawless coatings that improved the corrosion resistance of magnesium.
Coatings and surface modifications can significantly improve the corrosion resistance, biocompatibility and bioactivity of magnesium [58, 177, 178]. Depending on the type of coating and its characteristics (microstructure, thickness and adhesion strength, physisorption or chemisorption, of the coating material), the morphological, chemical and biological properties of the material surface can be improved [178]. Finally, the surface modification of magnesium is one of the most studied mechanisms to control material degradation due to the cost-effectiveness benefits and provides and the simplicity that most techniques offer compared to other methodologies [178, 179].
Heat treatments and plastic deformation conformation process
Heat treatments, such as aging and solution treatments, as well as hot deformations, generate an improvement on the mechanical properties of casted magnesium alloys, due to the modification of the material grain size [180]. The grain size is an important factor in the mechanical and electrochemical properties of magnesium alloys, through the implementation of heat treatments and plastic deformations in the processing of alloys. Duley et al. investigated the effects of the homogenization treatment in the mechanical properties and microstructure of a molten alloy of Mg–4Zn–0.5Ca–0.16Mn (in wt.%) and compared the results on different annealing times of 12 h, 24 h, 48 h and 72 h. This research suggests that homogenization annealing dissolves the eutectic phases that initiate cracks and produce a slight growth in grain size and that the 24-h specimen gave excellent hardness results and considerable ductility [179, 181].
In a study carried out by A. Gungor and A. Incesu [182], different Mg–Mn–Zn–Ca alloys with different Zn and Ca ratios are evaluated, which are manufactured and homogenized, against the same alloys subjected to a hot rolling process. The results of these investigations show that the hot rolled considerably improves the mechanical properties, while the immersion tests suggest that when the alloys are hot rolled, the grain edges become more vulnerable; micro-cracks are created and are easily corroded; however, all alloys behave within the ideal corrosion rate for an orthopedic implant (< 0.5 mm/year) and the ZXM300-hot rolled was defined as a material suitable for orthopedic applications with a corrosion rate of 0.029 mm/year and very similar mechanical properties to cortical bone.
Apart from the heat treatments, most of the authors add a deformation in the material, M. Kavyani et al. performed a “half equal channel angular pressing (HECAP)” to a Mg–Zn–Ca–Mn alloy and this presented better corrosion behavior, as well as superior mechanical properties, compared to the homogenized and extruded alloy [183]. Implementation of an equal channel angular pressing (ECAP) in pure magnesium has been reported to produce a reduction in grain size and better corrosion resistance [184]. Tong et al. carried out an investigation on the use of ECAP with multiple passes to produce ultrafine grains, and in this way, to improve the creep resistance and ductility, innovative results were obtained, which recognize the ECAP method as a useful alternative to modify the properties mechanics of a magnesium alloy. After four passes through the process, a potential increase in mechanical strength and ductility is seen. Grain size values ~ 9 μm were obtained [185].
N. El-Mahallawy, et al. [186] in their research, they made specimens of Mg-0.24Sn-0.04Mn and Mg–0.24Sn–1.16Zn–0.04Mn, followed by heat treatment and hot extrusion or hot rolling; from this experiment, they obtained data on mechanical and electrochemical properties. By extrusion, there was an increase of 35.4% and 10.4% in the UTS, respectively, and by hot rolling, an increase of 9.1% was observed in the first alloy and a decrease of 8.3% in the UTS. Regarding corrosion resistance, an increase was observed in the first alloy, with results of 0.82 mm/year for the homogenized alloy, 0.71 mm/year for the extruded one and 0.51 mm/year for the hot rolled one, whereas, when adding Zn to the alloy, it presents an improvement in corrosion when extruded from 1.88 to 0.95 mm/year, but when rolled it presents a deterioration of 1.88–2.87 mm/year.
Mg-based composite bioabsorbable materials
Composite biomaterials are presented as a union of a matrix made of a metallic alloy and a reinforcing material. Biodegradable composite materials, for orthopedic applications, both the metal matrix and the reinforcement, must be biodegradable and biocompatible with the human body [187]. Metal alloys for biomaterials are generally reinforced with ceramic particles, including alumina (Al2O3), zirconia (ZrO2), hydroxyapatite (HA) and β-tricalcium phosphate (β-TCP) [26]. Al2O3 is widely used thanks to being chemically inert, when combined with a zinc-based alloy, it increases wear resistance and biocompatibility [178]. By combining HA, a calcium phosphate mineral, with a Mg-based alloy by plasma sintering method, superior mechanical properties and improved corrosion resistance are obtained [47, 52, 55, 56]. Calcium phosphates have a composition like human bone and have excellent biocompatibility and stimulate osseointegration in bone healing processes. When using calcium phosphates in a material, either by coating or by sintering, an improvement in the adhesion and proliferation of the osteoblasts in the substrate has been evidenced, while the mechanical properties of the alloy are increased and the corrosion rate of Mg in the body is decreased [54, 154, 188].
When measuring the experimental density of the biodegradable compounds, it was shown that as the percentage of HA in the metallic alloy increases, the porosity of the material increases, for this reason being 15.13 mm/year that of pure Mg [189]. The implementation of HA in the matrix increases the maximum stress in tension and compression of the material, due to a grain refinement. For low amplitude cyclic stresses, the addition of HA improves the fatigue strength of the implant. For high percentages of HA, the ceramic particles can act as stress concentrators and allow the creation of cracks in the material, which would greatly reduce the useful life of the implant, both due to mechanical failure and cracks that allow the degradation of the material. By simultaneously evaluating corrosion and fatigue, they observe that the behavior of the two types of material is not very different. This is due to the superior corrosion resistance of 2.5%, which does not allow such rapid degradation of the implant, and the greater mechanical resistance of 5%.
Bioceramics have proven to be a promising material for implants and fasteners, due to their excellent biocompatibility and bioactivity; in addition, bioceramics have superior corrosion resistance [190]. By introducing them in the Mg matrix, improvements are obtained in the mechanical properties and resistance to corrosion, producing a passivation layer at the time of degradation, which protects the implant and delays its corrosion.
Table 5 summarizes the effect of the most common bioceramics on the magnesium matrix when used to produce biodegradable composite materials.
Impact of Magnesium modifications on the corrosion rate
Although the strategies previously studied have been effective in reducing the corrosion rate of magnesium alloys, it is necessary to identify which methodology has presented better efficiency in the process. For this, an extensive case study search is carried out in order to gather information about the type of modifications perform on magnesium alloys for biomedical purposes and the respective results of the corrosion parameters. The information is presented in Table 6. Subsequently, the efficiency of the process was determined by Eq. 5, where Icorr−base corresponds to the corrosion potential of the unmodified alloy and Icorr−mod correspond to the corrosion potential after the modification [191, 192]. In the case of alloys without surface modifications or heat treatments, the comparison was made respect to pure magnesium and the results are presented in Fig. 4.
Based on the data presented above, a comparison among the different methodologies to improve the corrosion resistance is carried out in Fig. 4. The efficiency of each technique for improving the corrosion response of the respective alloy is shown in Fig. 4. However, the results that show poor improvement are not considered in Fig. 4. The results in Fig. 4 show that that applying a surface modification an improvement of 85% in the corrosion resistance is possible to achieve (in average), while alloying Mg, implementing heat treatment and manufacturing magnesium matrix composites a similar efficiency (around 65%) can be obtained. In general, these four methodologies improve the corrosion resistance of magnesium. Surface modification is the most used in orthopedic implants, because it allows to establish stable and strong unions between the surface and the immobilized molecule since it promotes to generate ionic or covalent chemical bonds capable of resisting the extreme conditions of the human body during and after implantation [215,216,217,218,219].
Conclusion
Traditional biomaterials used in orthopedic applications (titanium, iron, chrome-cobalt alloys and polymers) are chemically biocompatible and with the ability to support the loads of the bone system. However, some of them in the long-term show cytotoxicity due to the release and accumulation of metallic particles because of the deterioration of the implant, as well as allergic reactions due to the release of metallic ions. In addition to this, if they are used as fixation elements, it is necessary to extract the osteosynthesis material through a second surgical intervention. Magnesium alloys have high potential as a biodegradable material for applications in fasteners or as temporary implants. The biggest challenge they represent is controlling the rate of magnesium degradation in vitro. Therefore, this paper has mainly concentrated on collecting, comparing and summarizing the effects of different methodologies in improving the corrosion resistance of magnesium alloys:
-
Applying a surface modification improve the corrosion resistance 85% in average and alloying Mg, implementing heat treatment and manufacturing magnesium matrix composites provides an efficiency close to 65%.
-
Among the Mg alloying agents, the authors consider that Zn is one of the best candidates since it improves the corrosion rate, improves the biocompatibility of mg and/or represents health risks at low concentrations.
-
For future studies, it is recommended to investigate in detail the types of coatings and compositions of composite materials that present better results and greater advantages for the use of magnesium alloys in biomedical applications and also to evaluate the influence of the manufacturing process on the material's degradability based on the corrosion parameters.
Data and code availability
The data used for the analysis in this document are previously referenced. No code was used for data processing.
References
Bonicelli A, Kranioti EF, Xhemali B et al (2022) Assessing bone maturity: compositional and mechanical properties of rib cortical bone at different ages. Bone 155:116265. https://doi.org/10.1016/J.BONE.2021.116265
Sarhan YM, Fikry A, Youssef AR, Mohamed MA (2022) Serum level of bone morphogenetic protein-7 in relation to entheseal ultrasonography in ankylosing spondylitis patients. Egypt Rheumatol 44:103–108. https://doi.org/10.1016/J.EJR.2021.09.002
de Stefano FA, Elarjani T, Burks JD et al (2021) Dose adjustment associated complications of bone morphogenetic protein: a longitudinal assessment. World Neurosurg 156:e64–e71. https://doi.org/10.1016/J.WNEU.2021.08.142
Oladapo BI, Zahedi SA, Ismail SO, Olawade DB (2021) Recent advances in biopolymeric composite materials: future sustainability of bone-implant. Renew Sustain Energy Rev 150:111505. https://doi.org/10.1016/J.RSER.2021.111505
Wang X, Xu S, Zhou S et al (2016) Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: a review. Biomaterials 83:127–141. https://doi.org/10.1016/J.BIOMATERIALS.2016.01.012
Galusha AL, Howard LJ, Kruger PC et al (2021) Bone mineral composition among long-term parenteral nutrition patients: postmortem assessment of calcium, phosphorus, magnesium, and select trace elements. J Parenter Enter Nutr 45:175–182. https://doi.org/10.1002/JPEN.1818
Bezstarosti H, Metsemakers WJ, van Lieshout EMM et al (2021) Management of critical-sized bone defects in the treatment of fracture-related infection: a systematic review and pooled analysis. Arch Orthop Trauma Surg 141:1215–1230
Cai Z, Wu Z, Wan Y et al (2021) Manipulation of the degradation behavior of calcium phosphate and calcium sulfate bone cement system by the addition of micro-nano calcium phosphate. Ceram Int 47:29213–29224. https://doi.org/10.1016/J.CERAMINT.2021.07.086
Stanovici J, le Nail LR, Brennan MA et al (2016) Bone regeneration strategies with bone marrow stromal cells in orthopaedic surgery. Curr Res Transl Med 64:83–90. https://doi.org/10.1016/J.RETRAM.2016.04.006
de Schickert SL, van den Beucken JJJP, Leeuwenburgh SCG, Jansen JA (2020) Pre-clinical evaluation of biological bone substitute materials for application in highly loaded skeletal sites. Biomolecules 10(6):883. https://doi.org/10.3390/biom10060883
Marzona L, Pavolini B (2009) Play and players in bone fracture healing match. Clin Cases Miner Bone Metab 6:159
Moris V, Loisel F, Cheval D et al (2016) Functional and radiographic evaluation of the treatment of traumatic bone loss of the hand using the masquelet technique. Hand Surg Rehabil 35:114–121. https://doi.org/10.1016/J.HANSUR.2015.11.002
Han JH, Kim HJ, Song JG et al (2015) Is bone grafting necessary in opening wedge high tibial osteotomy? A meta-analysis of radiological outcomes. Knee Surg Relat Res 27:207–220. https://doi.org/10.5792/KSRR.2015.27.4.207
Gamradt SC, Lieberman JR (2003) Bone graft for revision hip arthroplasty: biology and future applications. Clin Orthop Relat Res 417:183–194. https://doi.org/10.1097/01.BLO.0000096814.78689.77
Yang Y, He C, Dianyu E et al (2020) Mg bone implant: Features, developments and perspectives. Mater Des. https://doi.org/10.1016/j.matdes.2019.108259
Heary RF, Schlenk RP, Sacchieri TA et al (2002) Persistent iliac crest donor site pain: independent outcome assessment. Neurosurgery 50:510–517. https://doi.org/10.1097/00006123-200203000-00015
Strong DM (1995) Transmission of the hepatitis-C virus by tissue transplantation. Art J Bone Joint Surg. https://doi.org/10.2106/00004623-199502000-00007
Zhi W, Wang X, Sun D et al (2022) Optimal regenerative repair of large segmental bone defect in a goat model with osteoinductive calcium phosphate bioceramic implants. Bioact Mater 11:240–253. https://doi.org/10.1016/J.BIOACTMAT.2021.09.024
Xu C, Yu S, Wu W et al (2022) Direct ink writing of Fe bone implants with independently adjustable structural porosity and mechanical properties. Addit Manuf 51:102589. https://doi.org/10.1016/J.ADDMA.2021.102589
Gao H, Yang J, Jin X et al (2021) Porous tantalum scaffolds: fabrication, structure, properties, and orthopedic applications. Mater Des 210:110095. https://doi.org/10.1016/J.MATDES.2021.110095
Saini M, Singh Y, Arora P et al (2015) Implant biomaterials: a comprehensive review. World J Clin Cases 3:52. https://doi.org/10.12998/WJCC.V3.I1.52
Manivasagam G, Dhinasekaran D, Rajamanickam A (2010) Biomedical implants: corrosion and its prevention-a review super hydrophilic coatings view project coating on implants for biomedical applications view project biomedical implants: corrosion and its prevention-a review. Recent Pat Corros Sci 2:40–54. https://doi.org/10.2174/1877610801002010040
Manam NS, Harun WSW, Shri DNA et al (2017) Study of corrosion in biocompatible metals for implants: a review. J Alloys Compd 701:698–715. https://doi.org/10.1016/J.JALLCOM.2017.01.196
Sanghvi N, Vora D, Charaya E et al (2021) An approach for material selection for bone staple (an orthopaedic implant) using GRA and Fuzzy logic. Mater Today Proc 44:1300–1306. https://doi.org/10.1016/J.MATPR.2020.11.331
Tahmasebifar A, Kayhan SM, Evis Z et al (2016) Mechanical, electrochemical and biocompatibility evaluation of AZ91D magnesium alloy as a biomaterial. J Alloys Compd 687:906–919. https://doi.org/10.1016/J.JALLCOM.2016.05.256
Kabir H, Munir K, Wen C, Li Y (2021) Recent research and progress of biodegradable zinc alloys and composites for biomedical applications: biomechanical and biocorrosion perspectives. Bioact Mater 6:836–879
Karageorgiou V, Kaplan D (2005) Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26:5474–5491. https://doi.org/10.1016/J.BIOMATERIALS.2005.02.002
Luo Y, Zhang C, Wang J et al (2021) Clinical translation and challenges of biodegradable magnesium-based interference screws in ACL reconstruction. Bioact Mater 6:3231–3243. https://doi.org/10.1016/j.bioactmat.2021.02.032
Md Yusop AH, Al Sakkaf A, Nur H (2021) Modifications on porous absorbable Fe-based scaffolds for bone applications: a review from corrosion and biocompatibility viewpoints. J Biomed Mater Res B Appl Biomater 110:1–27. https://doi.org/10.1002/jbm.b.34893
Shi X, Nommeots-Nomm A, Todd NM et al (2020) Bioactive glass scaffold architectures regulate patterning of bone regeneration in vivo. Appl Mater Today 20:100770. https://doi.org/10.1016/j.apmt.2020.100770
Weng W, Biesiekierski A, Li Y et al (2021) A review of the physiological impact of rare earth elements and their uses in biomedical Mg alloys. Acta Biomater 130:80–97. https://doi.org/10.1016/j.actbio.2021.06.004
Centre for science and technology studies VOSviewer: visualizing scientific landscapes
Edupack CES (2018) Granta design limited
Sing SL, Yeong WY, Wiria FE (2016) Selective laser melting of titanium alloy with 50 wt% tantalum: microstructure and mechanical properties. J Alloys Compd 660:461–470. https://doi.org/10.1016/j.jallcom.2015.11.141
ASTM B265 (2009) Standard specification for titanium and titanium alloy strip, sheet, and plate 1. ASTM international, West Conshohocken, pp 1–10
ASTM F67 (2006) Standard specification for unalloyed titanium, for surgical implant applications. ASTM International, West Conshohocken, pp 1–5
Hi Y, Yamanoglu R (2020) Annals of advanced biomedical sciences β-type Ti alloys for biomedical applications annals of advanced biomedical sciences
Vanmeensel K, Lietaert K, Vrancken B et al (2018) Additively manufactured metals for medical applications. Elsevier Inc, Amsterdam
Jin W, Chu PK (2018) Orthopedic implants. Encycl Biomed Eng 1–3:425–439
Koizumi H, Ishii T, Okazaki T et al (2018) Castability and mechanical properties of Ti–15Mo–5Zr–3Al alloy in dental casting. J Oral Sci 60:285–292. https://doi.org/10.2334/josnusd.17-0280
Rechtin J, Torresani E, Ivanov E, Olevsky E (2018) Fabrication of titanium–niobium–zirconium–tantalium alloy (TNZT) bioimplant components with controllable porosity by spark plasma sintering. Materials. https://doi.org/10.3390/ma11020181
ASM International® (2009) Co-20Cr-15W-10Ni. Materials and coatings for medical devices: cardiovascular ASM materials for medical devices database committee. ASTM International, West Conshohocken, pp 69–73
Atlas Steels Australia (2019) Mechanical properties of 304 grade stainless steel grade, pp 1–3
Li H, Pang S, Liu Y et al (2015) Biodegradable Mg–Zn–Ca–Sr bulk metallic glasses with enhanced corrosion performance for biomedical applications. Mater Des 67:9–19. https://doi.org/10.1016/j.matdes.2014.10.085
Witte F, Hort N, Vogt C et al (2008) Degradable biomaterials based on magnesium corrosion. Curr Opin Solid State Mater Sci 12:63–72. https://doi.org/10.1016/j.cossms.2009.04.001
Dietrich Munz TF (1999) Ceramics: mechanical properties, failure behaviour, materials selection - Dietrich Munz, Theo Fett - Google Libros. In: Springer. https://books.google.com.co/books?hl=es&lr=&id=6I9YTABxdYMC&oi=fnd&pg=PA1&ots=yEVw2Wdq6i&sig=P5kkoMrU5LfDR4uUs95RZ2N5lSI&redir_esc=y#v=onepage&q&f=false. Accessed 25 May 2021
Prakash C, Singh S, Verma K et al (2018) Synthesis and characterization of Mg–Zn–Mn–HA composite by spark plasma sintering process for orthopedic applications. Vacuum 155:578–584. https://doi.org/10.1016/j.vacuum.2018.06.063
Leung L, Chan C, Baek S, Naguib H (2008) Comparison of morphology and mechanical properties of PLGA bioscaffolds. Biomed Mater 3:025. https://doi.org/10.1088/1748-6041/3/2/025006
Kurniawan D, Nor FM, Lee HY, Lim JY (2011) Elastic properties of polycaprolactone at small strains are significantly affected by strain rate and temperature. In: Proceedings of the institution of mechanical engineers, part H: journal of engineering in medicine. SAGE PublicationsSage, London, pp 1015–1020
Perego G, Cella GD, Bastioli C (1996) Effect of molecular weight and crystallinity on poly(lactic acid) mechanical properties. J Appl Polym Sci 59:37–43. https://doi.org/10.1002/(sici)1097-4628(19960103)59:1%3c37::aid-app6%3e3.0.co;2-n
Cui Z, Zhang Y, Cheng Y et al (2019) Microstructure, mechanical, corrosion properties and cytotoxicity of beta-calcium polyphosphate reinforced ZK61 magnesium alloy composite by spark plasma sintering. Mater Sci Eng C 99:1035–1047. https://doi.org/10.1016/j.msec.2019.02.050
Ye X, Chen M, Yang M et al (2010) In vitro corrosion resistance and cytocompatibility of nano-hydroxyapatite reinforced Mg–Zn–Zr composites. J Mater Sci Mater Med 21:1321–1328. https://doi.org/10.1007/s10856-009-3954-3
Wang X, Zhang P, Dong LH et al (2014) Microstructure and characteristics of interpenetrating β-TCP/Mg–Zn–Mn composite fabricated by suction casting. Mater Des 54:995–1001. https://doi.org/10.1016/j.matdes.2013.09.037
Huang Y, Liu D, Anguilano L et al (2015) Fabrication and characterization of a biodegradable Mg–2Zn–0.5Ca/1β-TCP composite. Mater Sci Eng C 54:120–132. https://doi.org/10.1016/j.msec.2015.05.035
Cui Z, Li W, Cheng L et al (2019) Effect of nano-HA content on the mechanical properties, degradation and biocompatible behavior of Mg–Zn/HA composite prepared by spark plasma sintering. Mater Charact 151:620–631. https://doi.org/10.1016/j.matchar.2019.03.048
Jaiswal S, Kumar RM, Gupta P et al (2018) Mechanical, corrosion and biocompatibility behaviour of Mg–3Zn–HA biodegradable composites for orthopaedic fixture accessories. J Mech Behav Biomed Mater 78:442–454. https://doi.org/10.1016/j.jmbbm.2017.11.030
Navarro M, Michiardi A, Castaño O, Planell JA (2008) Biomaterials in orthopaedics. J R Soc Interface 5:1137–1158
Sarian MN, Iqbal N, Sotoudehbagha P et al (2022) Potential bioactive coating system for high-performance absorbable magnesium bone implants. Bioact Mater 12:42–63. https://doi.org/10.1016/J.BIOACTMAT.2021.10.034
Julmi S, Krüger AK, Waselau AC et al (2019) Processing and coating of open-pored absorbable magnesium-based bone implants. Mater Sci Eng C 98:1073–1086. https://doi.org/10.1016/J.MSEC.2018.12.125
Carboneras Chamorro M, Iglesias Urraca C, Onofre Bustamante E et al (2011) Biodegradable metallic materials in the biomedical field. Acta Científica y Tecnológica 19:30–34
Kaur M, Singh K (2019) Review on titanium and titanium based alloys as biomaterials for orthopaedic applications. Mater Sci Eng C 102:844–862. https://doi.org/10.1016/j.msec.2019.04.064
Chen Q, Thouas GA (2015) Metallic implant biomaterials. Mater Sci Eng R Rep 87:1–57. https://doi.org/10.1016/j.mser.2014.10.001
Marchetti E, May O, Girard J et al (2019) Biomateriales en cirugía ortopédica. Mater Sci Eng C 102:844–862. https://doi.org/10.1016/s2211-033x(10)70083-9
Chandra G, Pandey A (2020) Preparation strategies for Mg-alloys for biodegradable orthopaedic implants and other biomedical applications: a review. IRBM, Amsterdam
Filipović U, Dahmane RG, Ghannouchi S et al (2020) Bacterial adhesion on orthopedic implants. Adv Colloid Interface Sci 283:1–12. https://doi.org/10.1016/j.cis.2020.102228
Angadi SV, Nayak SH, Ranjith RK et al (2022) Recent advancements in the manufacture of nitinol including its characterization and properties. Mater Today Proc 62:9–17. https://doi.org/10.1016/J.MATPR.2022.01.382
Asserghine A, Medvidović-Kosanović M, Nagy L, Nagy G (2019) In situ monitoring of the transpassivation and repassivation of the passive film on nitinol biomaterial by scanning electrochemical microscopy. Electrochem commun 107:106539. https://doi.org/10.1016/J.ELECOM.2019.106539
Kraus T, Moszner F, Fischerauer S et al (2014) Biodegradable Fe-based alloys for use in osteosynthesis: outcome of an in vivo study after 52 weeks. Acta Biomater 10:3346–3353. https://doi.org/10.1016/j.actbio.2014.04.007
Zhang W, Liu F, Liu L et al (2022) Effect of grain size and distribution on the corrosion behavior of Y2O3 dispersion-strengthened 304 stainless steel. Mater Today Commun 31:103723. https://doi.org/10.1016/J.MTCOMM.2022.103723
Gao Q, Lu Y, Yu Q et al (2022) High-temperature corrosion behavior of austenitic stainless steel in quaternary nitrate molten salt nanofluids for concentrated solar power. Solar Energy Mater Solar Cells 245:111851. https://doi.org/10.1016/J.SOLMAT.2022.111851
ASTM Astm A240–04 . Chromium and Chromium-Nickel Stainless Steel Plate, Sheet, and Strip for Pressure Vessels and for General Applications
Balestriere MA, Schuhladen K, Herrera Seitz K et al (2020) Sol-gel coatings incorporating borosilicate bioactive glass enhance anti corrosive and surface performance of stainless steel implants. J Electroanal Chem. https://doi.org/10.1016/j.jelechem.2020.114735
Ibrahim MZ, Sarhan AAD, Kuo TY et al (2019) Advancement of the artificial amorphous-crystalline structure of laser cladded FeCrMoCB on nickel-free stainless-steel for bone-implants. Mater Chem Phys 227:358–367. https://doi.org/10.1016/J.MATCHEMPHYS.2018.12.104
Liu X, Liu WC, Wang HY et al (2021) Polyelectrolyte multilayer composite coating on 316 L stainless steel for controlled release of dual growth factors accelerating restoration of bone defects. Mater Sci Eng C 126:112187. https://doi.org/10.1016/J.MSEC.2021.112187
Shen Q, Kong X, Chen X (2021) Fabrication of bulk Al-Co-Cr-Fe-Ni high-entropy alloy using combined cable wire arc additive manufacturing (CCW-AAM): microstructure and mechanical properties. J Mater Sci Technol 74:136–142. https://doi.org/10.1016/j.jmst.2020.10.037
Han X, Sawada T, Schille C et al (2018) Comparative analysis of mechanical properties and metal-ceramic bond strength of Co–Cr dental alloy fabricated by different manufacturing processes. Materials 11:1801. https://doi.org/10.3390/ma11101801
Wu L, Zhu H, Gai X, Wang Y (2014) Evaluation of the mechanical properties and porcelain bond strength of cobalt-chromium dental alloy fabricated by selective laser melting. J Prosthet Dent 111:51–55. https://doi.org/10.1016/j.prosdent.2013.09.011
Jiang F, Zhu W, Zhao C et al (2019) A strong, wear- and corrosion-resistant, and antibacterial Co–30 at.% Cr–5 at.% Ag ternary alloy for medical implants. Mater Des 184:108190. https://doi.org/10.1016/j.matdes.2019.108190
Rony L, Lancigu R, Hubert L (2018) Intraosseous metal implants in orthopedics: a review. Morphologie 102:231–242
Antunes LHM, de Lima CRP (2018) Cobalt-chromium alloys—properties and applications. Ref Module Mater Sci Mater Eng. https://doi.org/10.1016/B978-0-12-803581-8.09386-3
Mohammad Moradi S, Zangeneh S, Vardak S, Bahrami R (2022) New Co–Cr–Mo–Nb–Cu alloy for implant applications: properties characterization. J Alloys Compd 925:166387. https://doi.org/10.1016/J.JALLCOM.2022.166387
Zangeneh S, Lashgari HR, Lopez HF, Farahani HK (2017) Microstructural characterization of TIG surface treating in Co–Cr–Mo–C alloy. Mater Charact 132:223–229. https://doi.org/10.1016/J.MATCHAR.2017.08.017
Arora M, Chan EKS, Gupta S, Diwan AD (2013) Polymethylmethacrylate bone cements and additives: a review of the literature. World J Orthop 4:67–74
Asencio-Cortés C, Salgado-López L, Muñoz-Hernandez F et al (2019) Long-term safety and performance of a polymeric clamplike cranial fixation system. World Neurosurg 126:e758–e764. https://doi.org/10.1016/j.wneu.2019.02.146
Turell MB, Bellare A (2004) A study of the nanostructure and tensile properties of ultra-high molecular weight polyethylene. Biomaterials 25:3389–3398. https://doi.org/10.1016/j.biomaterials.2003.10.027
Kurtz S, Manley M (2009) Cross-Linked Polyethylene. Surg Treat Hip Arthritis Reconstr Replace Revis 11:456–467
Ippolito C, Yu S, Lai YJ, Bryant T (2017) Process parameter optimization for hot embossing uniformly textured uhmwpe surfaces for orthopedic bearings. In: Procedia CIRP. Elsevier B.V, pp 163–167
Oral E, Wannomae KK, Hawkins N et al (2004) α-Tocopherol-doped irradiated UHMWPE for high fatigue resistance and low wear. Biomaterials 25:5515–5522. https://doi.org/10.1016/j.biomaterials.2003.12.048
Agarwal R, García AJ (2015) Biomaterial strategies for engineering implants for enhanced osseointegration and bone repair. Adv Drug Deliv Rev 94:53–62. https://doi.org/10.1016/J.ADDR.2015.03.013
Francis AP, Augustus AR, Chandramohan S et al (2023) A review on biomaterials-based scaffold: an emerging tool for bone tissue engineering. Mater Today Commun 34:105124. https://doi.org/10.1016/J.MTCOMM.2022.105124
Gautam G, Kumar S, Kumar K (2022) Processing of biomaterials for bone tissue engineering: state of the art. Mater Today Proc 50:2206–2217. https://doi.org/10.1016/J.MATPR.2021.09.459
Gohil SV, Suhail S, Rose J et al (2017) Polymers and composites for orthopedic applications. In: Bose S, Bandyopadhyay A (eds) Materials and devices for bone disorders. Academic Press, Cambridge, pp 349–403
Pradeepkumar C, Karthikeyan S, Rajini N et al (2021) A contemporary review on additive manufactured biomedical implants. Mater Today Proc. https://doi.org/10.1016/j.matpr.2021.04.184
Cuiffo MA, Snyder J, Elliott AM et al (2017) Impact of the fused deposition (FDM) printing process on polylactic acid (PLA) chemistry and structure. Appl Sci (Switzerland) 7:579. https://doi.org/10.3390/app7060579
Zhao W, Liu L, Zhang F et al (2019) Shape memory polymers and their composites in biomedical applications. Mater Sci Eng, C 97:864–883. https://doi.org/10.1016/J.MSEC.2018.12.054
Liu Y, Cao H, Ye L et al (2020) Long-chain branched poly(lactic acid)- b-poly(lactide- co-caprolactone): structure, viscoelastic behavior, and triple-shape memory effect as smart bone fixation material. Ind Eng Chem Res 59:4524–4532. https://doi.org/10.1021/ACS.IECR.9B06514/ASSET/IMAGES/LARGE/IE9B06514_0004.JPEG
Tsakiris V, Tardei C, Clicinschi FM (2021) Biodegradable Mg alloys for orthopedic implants: a review. J Magn Alloys. https://doi.org/10.1016/j.jma.2021.06.024
Zheng YF, Gu XN, Witte F (2014) Biodegradable metals. Mater Sci Eng R Rep 77:1–34. https://doi.org/10.1016/J.MSER.2014.01.001
Wei B, Legut D, Sun S et al (2021) Synergistic effect of solute and strain on the electrochemical degradation in representative Zn-based and Mg-based alloys. Corros Sci 188:109539. https://doi.org/10.1016/j.corsci.2021.109539
Wątroba M, Bednarczyk W, Kawałko J et al (2019) Design of novel Zn-Ag-Zr alloy with enhanced strength as a potential biodegradable implant material. Mater Des 183:108154. https://doi.org/10.1016/J.MATDES.2019.108154
Tong X, Zhang D, Zhang X et al (2018) Microstructure, mechanical properties, biocompatibility, and in vitro corrosion and degradation behavior of a new Zn–5Ge alloy for biodegradable implant materials. Acta Biomater 82:197–204. https://doi.org/10.1016/j.actbio.2018.10.015
Maradze D, Capel A, Martin N et al (2019) In vitro investigation of cellular effects of magnesium and magnesium-calcium alloy corrosion products on skeletal muscle regeneration. J Mater Sci Technol 35:2503–2512. https://doi.org/10.1016/j.jmst.2019.01.020
Basturk SB, Dancer CEJ, McNally T (2020) In vitro corrosion study of PLA+Mg composites for cardiovascular stent applications. Pharmacol Res. https://doi.org/10.1016/j.jmbbm.2021.104768
Eliaz N (2012) Degradation of implant materials. Degradation of Implant Materials 9781461439:1–516. https://doi.org/10.1007/978-1-4614-3942-4
Zhang ZQ, Yang YX, Li JA et al (2021) Advances in coatings on magnesium alloys for cardiovascular stents: a review. Bioact Mater 6:4729–4757. https://doi.org/10.1016/j.bioactmat.2021.04.044
Liu J, Wang P, Chu CC, Xi T (2017) Arginine-leucine based poly (ester urea urethane) coating for Mg–Zn–Y–Nd alloy in cardiovascular stent applications. Coll Surf B Biointerfaces 159:78–88. https://doi.org/10.1016/j.colsurfb.2017.07.031
Santos-Coquillat A, Esteban-Lucia M, Martinez-Campos E et al (2019) PEO coatings design for Mg–Ca alloy for cardiovascular stent and bone regeneration applications. Mater Sci Eng C 105:110026. https://doi.org/10.1016/j.msec.2019.110026
Zhou WR, Zheng YF, Leeflang MA, Zhou J (2013) Mechanical property, biocorrosion and in vitro biocompatibility evaluations of Mg–Li–(Al)–(RE) alloys for future cardiovascular stent application. Acta Biomater 9:8488–8498. https://doi.org/10.1016/j.actbio.2013.01.032
Munir K, Lin J, Wen C et al (2020) Mechanical, corrosion, and biocompatibility properties of Mg–Zr–Sr–Sc alloys for biodegradable implant applications. Acta Biomater 102:493–507. https://doi.org/10.1016/j.actbio.2019.12.001
Li H, Zheng Y, Qin L (2014) Progress of biodegradable metals. Prog Nat Sci Mater Int 24:414–422. https://doi.org/10.1016/j.pnsc.2014.08.014
Hussein MA, Azeem MA, Kumar AM, Emara NM (2022) Processing and in vitro corrosion analysis of sustainable and economical eggshell reinforced Mg and Mg–Zr matrix composite for biomedical applications. Mater Today Commun 32:103944. https://doi.org/10.1016/J.MTCOMM.2022.103944
Manne B, Thiruvayapati H, Bontha S et al (2018) Surface design of Mg–Zn alloy temporary orthopaedic implants: tailoring wettability and biodegradability using laser surface melting. Surf Coat Technol 347:337–349. https://doi.org/10.1016/j.surfcoat.2018.05.017
Wan P, Tan L, Yang K (2016) Surface modification on biodegradable magnesium alloys as orthopedic implant materials to improve the bio-adaptability: a review. J Mater Sci Technol 32:827–834. https://doi.org/10.1016/j.jmst.2016.05.003
Vennimalai Rajan A, Mathalai Sundaram C, Vembathu Rajesh A (2020) Mechanical and morphological investigation of bio-degradable magnesium AZ31 alloy for an orthopedic application. Mater Today Proc 21:272–277. https://doi.org/10.1016/j.matpr.2019.05.429
Walker J, Shadanbaz S, Kirkland NT et al (2012) Magnesium alloys: Predicting in vivo corrosion with in vitro immersion testing. J Biomed Mater Res 100B:1134–1141. https://doi.org/10.1002/jbm.b.32680
Feyerabend F, Willumeit-rilmer R, Biese O Van Der, et al (2015) Influence of testing environment on the degradation behavior of magnesium alloys for bioabsorbable implants, pp 3–10
Shaw BA (2003) Corrosion Resistance of Magnesium Alloys. 13:
Li LY, Cui LY, Zeng RC et al (2018) Advances in functionalized polymer coatings on biodegradable magnesium alloys: a review. Acta Biomater 79:23–36
Fan XL, Li CY, Wang YB et al (2020) Corrosion resistance of an amino acid-bioinspired calcium phosphate coating on magnesium alloy AZ31. J Mater Sci Technol 49:224–235. https://doi.org/10.1016/j.jmst.2020.01.046
Feliu S, Maffiotte C, Samaniego A et al (2011) Effect of naturally formed oxide films and other variables in the early stages of Mg-alloy corrosion in NaCl solution. Electrochim Acta 56:4554–4565. https://doi.org/10.1016/j.electacta.2011.02.077
Song GL, Dudney NJ, Li J et al (2014) The possibility of forming a sacrificial anode coating for Mg. Corros Sci 87:11–14. https://doi.org/10.1016/j.corsci.2014.07.007
Sadawy M, Saad S, ABDEL-KARIM R, (2020) Effect of Zn/Mg ratio on cathodic protection of carbon steel using Al−Zn−Mg sacrificial anodes. Trans Nonferrous Metals Soc China 30:2067–2078. https://doi.org/10.1016/S1003-6326(20)65361-4. (English edition)
Yu BL, Uan JY (2006) Sacrificial Mg film anode for cathodic protection of die cast Mg–9 wt.%Al–1 wt.%Zn alloy in NaCl aqueous solution. Scr Mater 54:1253–1257. https://doi.org/10.1016/j.scriptamat.2005.12.031
Ng WF, Chiu KY, Cheng FT (2010) Effect of pH on the in vitro corrosion rate of magnesium degradable implant material. Mater Sci Eng C 30:898–903. https://doi.org/10.1016/J.MSEC.2010.04.003
Witte F, Fischer J, Nellesen J et al (2006) In vitro and in vivo corrosion measurements of magnesium alloys. Biomaterials 27:1013–1018. https://doi.org/10.1016/j.biomaterials.2005.07.037
Hu H, Nie X, Ma Y (2014) Corrosion and surface treatment of magnesium alloys. In: Czerwinski F (ed) Magnesium Alloy—properties in solid and liquid states. Intech Open, Rijeka, p 13
Willumeit R, Fischer J, Feyerabend F et al (2011) Chemical surface alteration of biodegradable magnesium exposed to corrosion media. Acta Biomater 7:2704–2715. https://doi.org/10.1016/j.actbio.2011.03.004
Bornapour M, Celikin M, Pekguleryuz M (2015) Thermal exposure effects on the in vitro degradation and mechanical properties of Mg–Sr and Mg–Ca–Sr biodegradable implant alloys and the role of the microstructure. Mater Sci Eng C 46:16–24. https://doi.org/10.1016/j.msec.2014.10.008
Bahmani A, Arthanari S, Shin KS (2020) Formulation of corrosion rate of magnesium alloys using microstructural parameters. J Magnes Alloy 8:134–149. https://doi.org/10.1016/j.jma.2019.12.001
Mathieu S, Rapin C, Hazan J, Steinmetz P (2002) Corrosion behaviour of high pressure die-cast and semi-solid cast AZ91D alloys. Corros Sci 44:2737–2756. https://doi.org/10.1016/S0010-938X(02)00075-6
Zhang J, Xu C, Jing Y et al (2015) New horizon for high performance Mg-based biomaterial with uniform degradation behavior: formation of stacking faults OPEN. Sci Rep. https://doi.org/10.1038/srep13933
Li C, Lv H, Du Y et al (2022) Biologically modified implantation as therapeutic bioabsorbable materials for bone defect repair. Regen Ther 19:9–23. https://doi.org/10.1016/J.RETH.2021.12.004
Zuo M, Wang W, Wu H et al (2019) In vitro degradation and mineralization of high-purity magnesium in three physiological fluids. Mater Lett 240:279–283. https://doi.org/10.1016/j.matlet.2019.01.001
Feliu S, Llorente I (2015) Corrosion product layers on magnesium alloys AZ31 and AZ61: Surface chemistry and protective ability. Appl Surf Sci 347:736–746. https://doi.org/10.1016/j.apsusc.2015.04.189
Zou YH, Zeng RC, Wang QZ et al (2016) Blood compatibility of zinc–calcium phosphate conversion coating on Mg–1.33Li–0.6Ca alloy. Front Mater Sci 10:281–289. https://doi.org/10.1007/s11706-016-0345-9
Yao QS, Zhang F, Song L et al (2018) Corrosion resistance of a ceria/polymethyltrimethoxysilane modified Mg–Al-layered double hydroxide on AZ31 magnesium alloy. J Alloys Compd 764:913–928. https://doi.org/10.1016/j.jallcom.2018.06.152
Zai W, Zhang X, Su Y et al (2020) Comparison of corrosion resistance and biocompatibility of magnesium phosphate (MgP), zinc phosphate (ZnP) and calcium phosphate (CaP) conversion coatings on Mg alloy. Surf Coat Technol 397:125919. https://doi.org/10.1016/j.surfcoat.2020.125919
Ding Y, Wen C, Hodgson P, Li Y (2014) Effects of alloying elements on the corrosion behavior and biocompatibility of biodegradable magnesium alloys: a review. J Mater Chem B 2:1912–1933. https://doi.org/10.1039/c3tb21746a
Kumar V, Gill KD (2009) Aluminium neurotoxicity: neurobehavioural and oxidative aspects. Arch Toxicol 83:965–978
Verstraeten SV, Aimo L, Oteiza PI (2008) Aluminium and lead: molecular mechanisms of brain toxicity. Arch Toxicol 82:789–802
Zatta P, Lucchini R, Van Rensburg SJ, Taylor A (2003) The role of metals in neurodegenerative processes: aluminum, manganese, and zinc. Brain Res Bull 62:15–28. https://doi.org/10.1016/S0361-9230(03)00182-5
Jin S, Zhang D, Lu X et al (2020) Mechanical properties, biodegradability and cytocompatibility of biodegradable Mg–Zn–Zr–Nd/Y alloys. J Mater Sci Technol 47:190–201. https://doi.org/10.1016/j.jmst.2020.02.017
Hänzi AC, Gerber I, Schinhammer M et al (2010) On the in vitro and in vivo degradation performance and biological response of new biodegradable Mg–Y–Zn alloys. Acta Biomater 6:1824–1833. https://doi.org/10.1016/j.actbio.2009.10.008
Glenske K, Donkiewicz P, Köwitsch A et al (2018) Applications of metals for bone regeneration. Int J Mol Sci 19:826. https://doi.org/10.3390/ijms19030826
Bose S, Fielding G, Tarafder S, Bandyopadhyay A (2013) Understanding of dopant-induced osteogenesis and angiogenesis in calcium phosphate ceramics. Trends Biotechnol 31:594–605
Yao X, Tang J, Zhou Y et al (2020) Surface modification of biomedical Mg–Ca and Mg–Zn–Ca alloys using selective laser melting: corrosion behaviour, microhardness and biocompatibility. J Magnes Alloy. https://doi.org/10.1016/j.jma.2020.08.011
Jung YG, Yang W, Kim YJ et al (2021) Effect of Ca addition on the microstructure and mechanical properties of heat-treated Mg–6.0Zn–1.2Y–0.7Zr alloy. J Magnes Alloy. https://doi.org/10.1016/j.jma.2021.01.010
Ross AC, Taylor CL, Institute of Medicine (US) Committee et al (2011) Dietary reference intakes for calcium and vitamin D. National Academies Press, Washington
Gu X, Zheng Y, Cheng Y et al (2009) In vitro corrosion and biocompatibility of binary magnesium alloys. Biomaterials 30:484–498. https://doi.org/10.1016/j.biomaterials.2008.10.021
Li J, Chen R, Ma Y, Ke W (2013) Effect of Zr modification on solidification behavior and mechanical properties of Mg–Y–RE (WE54) alloy. J Magnes Alloy 1:346–351. https://doi.org/10.1016/j.jma.2013.12.001
Sun M, Wu G, Wang W, Ding W (2009) Effect of Zr on the microstructure, mechanical properties and corrosion resistance of Mg–10Gd–3Y magnesium alloy. Mater Sci Eng A 523:145–151. https://doi.org/10.1016/j.msea.2009.06.002
Catauro M, Bollino F, Veronesi P, Lamanna G (2014) Influence of PCL on mechanical properties and bioactivity of ZrO2-based hybrid coatings synthesized by sol–gel dip coating technique. Mater Sci Eng C 39:344–351. https://doi.org/10.1016/J.MSEC.2014.03.025
Zhang RF, Zhang SF (2009) Formation of micro-arc oxidation coatings on AZ91HP magnesium alloys. Corros Sci 51:2820–2825. https://doi.org/10.1016/j.corsci.2009.08.009
Heimann RB (2020) Magnesium alloys for biomedical application: advanced corrosion control through surface coating. Surf Coat Technol 405:126521. https://doi.org/10.1016/j.surfcoat.2020.126521
Rakoch AG, Monakhova EP, Khabibullina ZV et al (2020) Plasma electrolytic oxidation of AZ31 and AZ91 magnesium alloys: Comparison of coatings formation mechanism. J Magnes Alloy 8:587–600. https://doi.org/10.1016/j.jma.2020.06.002
Manoj Kumar R, Kuntal KK, Singh S et al (2016) Electrophoretic deposition of hydroxyapatite coating on Mg–3Zn alloy for orthopaedic application. Surf Coat Technol 287:82–92. https://doi.org/10.1016/j.surfcoat.2015.12.086
Abela S (2010) Physical vapour deposition of magnesium alloys. In: Surface engineering of light alloys: aluminium, magnesium and titanium alloys. Elsevier Inc., pp 294–322
Zhou A (2012) Methods of MAX-phase synthesis and densification—II. In: Advances in science and technology of Mn+1AXn phases. Elsevier, pp 21–46
Alphonse M, Bupesh Raja VK, Gupta M (2020) Optimization of plasma nitrided, liquid nitrided and PVD TiN coated H13–D2 friction drilling tool on AZ31B magnesium alloy. Mater Today Proc. https://doi.org/10.1016/j.matpr.2020.03.791
Zarka M, Dikici B, Niinomi M et al (2020) A systematic study of β-type Ti-based PVD coatings on magnesium for biomedical application. Vacuum 183:109850. https://doi.org/10.1016/j.vacuum.2020.109850
Altun H, Sen S (2007) The effect of PVD coatings on the wear behaviour of magnesium alloys. Mater Charact 58:917–921. https://doi.org/10.1016/j.matchar.2006.09.007
Hoche H, Schmidt J, Groß S et al (2011) PVD coating and substrate pretreatment concepts for corrosion and wear protection of magnesium alloys. Surf Coat Technol 205:S145–S150. https://doi.org/10.1016/j.surfcoat.2010.12.040
Wu G, Zeng X, Yuan G (2008) Growth and corrosion of aluminum PVD-coating on AZ31 magnesium alloy. Mater Lett 62:4325–4327. https://doi.org/10.1016/j.matlet.2008.07.014
Song GL, Haddad D (2011) The topography of magnetron sputter-deposited Mg–Ti alloy thin films. Mater Chem Phys 125:548–552. https://doi.org/10.1016/j.matchemphys.2010.10.018
Kania A, Pilarczyk W, Szindler MM (2020) Structure and corrosion behavior of TiO2 thin films deposited onto Mg-based alloy using magnetron sputtering and sol–gel. Thin Solid Films 701:137945. https://doi.org/10.1016/j.tsf.2020.137945
Sivapragash M, Kumaradhas P, Vettivel SC, Retnam BSJ (2018) Optimization of PVD process parameter for coating AZ91D magnesium alloy by Taguchi grey approach. J Magnes Alloy 6:171–179. https://doi.org/10.1016/j.jma.2018.02.004
Jeong H, Cho J (2017) Characterization of interfacial layers grown between magnesium substrates and SiOx films deposited by plasma-enhanced CVD. Surf Coat Technol 332:105–111. https://doi.org/10.1016/j.surfcoat.2017.07.088
Kaabi Falahieh Asl S, Nemeth S, Tan MJ (2015) Improved corrosion protection of magnesium by hydrothermally deposited biodegradable calcium phosphate coating. Mater Chem Phys 161:185–193. https://doi.org/10.1016/j.matchemphys.2015.05.035
Kaabi Falahieh Asl S, Nemeth S, Tan MJ (2016) Novel biodegradable calcium phosphate/polymer composite coating with adjustable mechanical properties formed by hydrothermal process for corrosion protection of magnesium substrate. J Biomed Mater Res B Appl Biomater 104:1643–1657. https://doi.org/10.1002/jbm.b.33505
Kavitha RJ, Ravichandran K, Sankara Narayanan TSN (2018) Deposition of strontium phosphate coatings on magnesium by hydrothermal treatment: characteristics, corrosion resistance and bioactivity. J Alloys Compd 745:725–743. https://doi.org/10.1016/j.jallcom.2018.02.200
Hernández-Barrios CA, Saavedra JA, Higuera SL et al (2020) Effect of cerium on the physicochemical and anticorrosive features of TEOS-GPTMS sol–gel coatings deposited on the AZ31 magnesium alloy. Surf Interfaces 21:100671. https://doi.org/10.1016/j.surfin.2020.100671
Omar SA, Ballarre J, Castro Y et al (2020) 58S and 68S sol–gel glass-like bioactive coatings for enhancing the implant performance of AZ91D magnesium alloy. Surf Coat Technol 400:126224. https://doi.org/10.1016/j.surfcoat.2020.126224
Nezamdoust S, Seifzadeh D, HABIBI-YANGJEH A, (2020) Nanodiamond incorporated sol−gel coating for corrosion protection of magnesium alloy. Trans Nonferrous Metals Soc China 30:1535–1549. https://doi.org/10.1016/S1003-6326(20)65317-1. (English Edition)
Wang C, Shen J, Zhang X et al (2017) In vitro degradation and cytocompatibility of a silane/Mg(OH)2 composite coating on AZ31 alloy by spin coating. J Alloys Compd 714:186–193. https://doi.org/10.1016/j.jallcom.2017.04.229
Córdoba LC, Marques A, Taryba M et al (2018) Hybrid coatings with collagen and chitosan for improved bioactivity of Mg alloys. Surf Coat Technol 341:103–113. https://doi.org/10.1016/j.surfcoat.2017.08.062
Upadhyay V, Bergseth Z, Kelly B, Battocchi D (2017) Silica-based sol–gel coating on magnesium alloy with green inhibitors. Coatings 7:86. https://doi.org/10.3390/coatings7070086
Razavi M, Fathi M, Savabi O et al (2014) Coating of biodegradable magnesium alloy bone implants using nanostructured diopside (CaMgSi2O6). Appl Surf Sci 288:130–137. https://doi.org/10.1016/J.APSUSC.2013.09.160
Chavan AB, Gawade SS, Bhosale AP (2022) A review on surface coating techniques on Mg based bio-degradable implants. Mater Today Proc. https://doi.org/10.1016/J.MATPR.2022.09.331
Tong P, Sheng Y, Hou R et al (2022) Recent progress on coatings of biomedical magnesium alloy. Smart Mater Med 3:104–116. https://doi.org/10.1016/J.SMAIM.2021.12.007
Ibrahim H, Klarner AD, Poorganji B et al (2017) Microstructural, mechanical and corrosion characteristics of heat-treated Mg–1.2Zn–0.5Ca (wt%) alloy for use as resorbable bone fixation material. J Mech Behav Biomed Mater 69:203–212. https://doi.org/10.1016/j.jmbbm.2017.01.005
Duley P, Sanyal S, Bandyopadhyay TK, Mandal S (2019) Homogenization-induced age-hardening behavior and room temperature mechanical properties of Mg–4Zn–0.5Ca–0.16Mn (wt%) alloy. Mater Des 164:107554. https://doi.org/10.1016/j.matdes.2018.107554
Gungor A, Incesu A (2021) Effects of alloying elements and thermomechanical process on the mechanical and corrosion properties of biodegradable Mg alloys. J Magnes Alloy 9:241–253. https://doi.org/10.1016/j.jma.2020.09.009
Kavyani M, Ebrahimi GR, Ezatpour HR, Jahazi M (2020) Microstructure refinement, mechanical and biocorrosion properties of Mg–Zn–Ca–Mn alloy improved by a new severe plastic deformation process. J Magnes Alloy. https://doi.org/10.1016/j.jma.2020.11.013
Birbilis N, Ralston KD, Virtanen S et al (2010) Grain character influences on corrosion of ECAPed pure magnesium. Corros Eng Sci Technol 45:224–230. https://doi.org/10.1179/147842209X12559428167805
Tong LB, Chu JH, Jiang ZH et al (2019) Ultra-fine grained Mg–Zn–Ca–Mn alloy with simultaneously improved strength and ductility processed by equal channel angular pressing. J Alloys Compd 785:410–421. https://doi.org/10.1016/j.jallcom.2019.01.181
El-Mahallawy N, Palkowski H, Klingner A et al (2020) Effect of 1.0 wt. % Zn addition on the microstructure, mechanical properties, and bio-corrosion behaviour of micro alloyed Mg-0.24Sn-0.04Mn alloy as biodegradable material. Mater Today Commun 24:100999. https://doi.org/10.1016/j.mtcomm.2020.100999
Radha R, Sreekanth D (2017) Insight of magnesium alloys and composites for orthopedic implant applications: a review. J Magnes Alloy 5:286–312. https://doi.org/10.1016/j.jma.2017.08.003
Dorozhkin SV (2014) Calcium orthophosphate coatings on magnesium and its biodegradable alloys. Acta Biomater 10:2919–2934
Ghazizadeh E, Jabbari AH, Sedighi M (2021) In vitro corrosion-fatigue behavior of biodegradable Mg/HA composite in simulated body fluid. J Magnes Alloy. https://doi.org/10.1016/J.JMA.2021.03.027
Shekhawat D, Singh A, Banerjee MK et al (2021) Bioceramic composites for orthopaedic applications: a comprehensive review of mechanical, biological, and microstructural properties. Ceram Int 47:3013–3030
Wang J, Zhao J, Tabish M et al (2022) Long-term corrosion inhibition for AA5052 aluminum alloy by an eco-friendly hybrid inhibitor: synergism inhibition between rosemary extract and Zinc chloride in 0.05 M NaCl solution. J Ind Eng Chem. https://doi.org/10.1016/J.JIEC.2022.12.037
Li W, Su Y, Ma L et al (2021) Sol–gel coating loaded with inhibitor on ZE21B Mg alloy for improving corrosion resistance and endothelialization aiming at potential cardiovascular application. Coll Surf B Biointerfaces 207:111993. https://doi.org/10.1016/J.COLSURFB.2021.111993
Wu H, Xi K, Xiao S et al (2020) Formation of self-layered hydrothermal coating on magnesium aided by titanium ion implantation: Synergistic control of corrosion resistance and cytocompatibility. Surf Coat Technol 401:126251. https://doi.org/10.1016/j.surfcoat.2020.126251
Lin Z, Zhao Y, Chu PK et al (2019) A functionalized TiO2/Mg2TiO4 nano-layer on biodegradable magnesium implant enables superior bone-implant integration and bacterial disinfection. Biomaterials 219:119372. https://doi.org/10.1016/J.BIOMATERIALS.2019.119372
Pei Y, Zhang G, Zhang C et al (2019) Corrosion resistance, anticoagulant and antibacterial properties of surface-functionalized magnesium alloys. Mater Lett 234:323–326. https://doi.org/10.1016/j.matlet.2018.09.140
Zhou W, Hu Z, Wang T et al (2020) Enhanced corrosion resistance and bioactivity of Mg alloy modified by Zn-doped nanowhisker hydroxyapatite coatings. Coll Surf B Biointerfaces 186:110710. https://doi.org/10.1016/j.colsurfb.2019.110710
Zhou H, Li J, Li J et al (2020) Calcium phosphate coating on biomedical WE43 magnesium alloy pretreated with a magnesium phosphate layer for corrosion protection. Surf Coat Technol 401:126248. https://doi.org/10.1016/J.SURFCOAT.2020.126248
Su Y, Lu Y, Su Y et al (2015) Enhancing the corrosion resistance and surface bioactivity of a calcium-phosphate coating on a biodegradable AZ60 magnesium alloy via a simple fluorine post-treatment method. RSC Adv 5:56001–56010. https://doi.org/10.1039/c5ra10315k
Lin X, Tan L, Zhang Q et al (2013) The in vitro degradation process and biocompatibility of a ZK60 magnesium alloy with a forsterite-containing micro-arc oxidation coating. Acta Biomater 9:8631–8642. https://doi.org/10.1016/j.actbio.2012.12.016
Prakash C, Singh S, Gupta MK et al (2018) Synthesis, characterization, corrosion resistance and in-vitro bioactivity behavior of biodegradable Mg–Zn–Mn–(Si–HA) composite for orthopaedic applications. Materials 11:1602. https://doi.org/10.3390/MA11091602
Wang X, Zhang P, Dong LH et al (2014) Microstructure and characteristics of interpenetrating β-TCP/Mg–Zn–Mn composite fabricated by suction casting. Mater Des 1980–2015(54):995–1001. https://doi.org/10.1016/J.MATDES.2013.09.037
Lin DJ, Hung FY, Lui TS, Yeh ML (2015) Heat treatment mechanism and biodegradable characteristics of ZAX1330 Mg alloy. Mater Sci Eng C 51:300–308. https://doi.org/10.1016/j.msec.2015.03.004
Bakhsheshi-Rad HR, Idris MH, Abdul-Kadir MR et al (2014) Mechanical and bio-corrosion properties of quaternary Mg–Ca–Mn–Zn alloys compared with binary Mg–Ca alloys. Mater Des 53:283–292. https://doi.org/10.1016/j.matdes.2013.06.055
Homayun B, Afshar A (2014) Microstructure, mechanical properties, corrosion behavior and cytotoxicity of Mg–Zn–Al–Ca alloys as biodegradable materials. J Alloys Compd 607:1–10. https://doi.org/10.1016/J.JALLCOM.2014.04.059
Yan Y, Kang Y, Li D et al (2017) Improvement of the mechanical properties and corrosion resistance of biodegradable β-Ca3(PO4)2/Mg–Zn composites prepared by powder metallurgy: the adding β-Ca3(PO4)2, hot extrusion and aging treatment. Mater Sci Eng C 74:582–596. https://doi.org/10.1016/J.MSEC.2016.12.132
Yan Y, Cao H, Kang Y et al (2017) Effects of Zn concentration and heat treatment on the microstructure, mechanical properties and corrosion behavior of as-extruded Mg–Zn alloys produced by powder metallurgy. J Alloys Compd 693:1277–1289. https://doi.org/10.1016/J.JALLCOM.2016.10.017
Zarka M, Dikici B, Niinomi M et al (2021) A systematic study of β-type Ti-based PVD coatings on magnesium for biomedical application. Vacuum 183:109850. https://doi.org/10.1016/j.vacuum.2020.109850
Zhou Z, Zheng B, Lang H et al (2020) Corrosion resistance and biocompatibility of polydopamine/hyaluronic acid composite coating on AZ31 magnesium alloy. Surf Interfaces 20:100560. https://doi.org/10.1016/j.surfin.2020.100560
Guo Y, Su Y, Gu R et al (2020) Enhanced corrosion resistance and biocompatibility of biodegradable magnesium alloy modified by calcium phosphate/collagen coating. Surf Coat Technol 401:126318. https://doi.org/10.1016/j.surfcoat.2020.126318
Pan H, Yang H, Tang X et al (2017) Effect of Ca/P ratio on the structural and corrosion properties of biomimetic Ca[sbnd]P coatings on ZK60 magnesium alloy. Mater Sci Eng C 72:676–681. https://doi.org/10.1016/j.msec.2016.11.132
Jiang S, Cai S, Lin Y et al (2019) Effect of alkali/acid pretreatment on the topography and corrosion resistance of as-deposited CaP coating on magnesium alloys. J Alloys Compd 793:202–211. https://doi.org/10.1016/j.jallcom.2019.04.198
Dutta S, Devi KB, Mandal S et al (2019) In vitro corrosion and cytocompatibility studies of hot press sintered magnesium-bioactive glass composite. Materialia (Oxf) 5:100245. https://doi.org/10.1016/J.MTLA.2019.100245
Khalajabadi SZ, Abdul Kadir MR, Izman S, Ebrahimi-Kahrizsangi R (2015) Fabrication, bio-corrosion behavior and mechanical properties of a Mg/HA/MgO nanocomposite for biomedical applications. Mater Des 88:1223–1233. https://doi.org/10.1016/J.MATDES.2015.09.065
Zhao J, Yu K, Chen L et al (2012) Mechanical properties and biodegradable behavior of Mg–6%Zn–Ca 3(PO 4) 2 metal matrix composites in Ringer’s solution. Int J Mater Res 103:723–728. https://doi.org/10.3139/146.110686/MACHINEREADABLECITATION/RIS
Sevilla P, Vining KH, Dotor J et al (2015) Surface immobilization and bioactivity of TGF- b 1 inhibitor peptides for bone implant applications. J Biomed Mater Sci 104:385–394. https://doi.org/10.1002/jbm.b.33374
Fernandez-garcia E, Chen X, Gutierrez-gonzalez CF et al (2015) ScienceDirect Peptide-functionalized zirconia and new zirconia/titanium biocermets for dental applications. J Dent 43:1162–1174. https://doi.org/10.1016/j.jdent.2015.06.002
Sevilla P, Cirera A, Dotor J et al (2018) In vitro cell response on CP–Ti surfaces functionalized with TGF-β1 inhibitory peptides. J Mater Sci Mater Med 29(1):11
Fang K, Song W, Wang L et al (2014) Immobilization of chitosan film containing semaphorin 3A onto a microarc oxidized titanium implant surface via silane reaction to improve MG63 osteogenic differentiation. Int J Nanomedicine 9:4649–4657. https://doi.org/10.2147/IJN.S68895
Mohammadi M, Alibolandi M, Abnous K et al (2020) Comparison of liposomal formulations incorporating BMP-2 peptide to induce bone tissue engineering. Nanomed J 0:225–230. https://doi.org/10.22038/nmj.2020.15575
Funding
Open Access funding provided by Colombia Consortium.
Author information
Authors and Affiliations
Contributions
LDCGP contributed to conceptualization, methodology, formal analysis, investigation, writing—original draft, visualization, writing—review and editing. JCRM contributed to conceptualization, methodology, formal analysis, investigation, writing—original draft, visualization, writing—review and editing. AMFR contributed to conceptualization, investigation, writing—review and editing. HZR contributed to writing—review and editing, visualization and validation. VNPM contributed to conceptualization, formal analysis, writing—review and editing, visualization and supervision. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
No animal or human tissue experiments were carried out in this review.
Additional information
Handling Editor: Catalin Croitoru.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gutiérrez Púa, L.D., Rincón Montenegro, J.C., Fonseca Reyes, A.M. et al. Biomaterials for orthopedic applications and techniques to improve corrosion resistance and mechanical properties for magnesium alloy: a review. J Mater Sci 58, 3879–3908 (2023). https://doi.org/10.1007/s10853-023-08237-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10853-023-08237-5