Abstract
Purpose
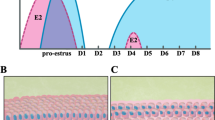
Estrogen is well-known for preparing uterine receptivity. However, its roles in regulating embryo development and implantation are unclear. Our objective was to characterize estrogen receptor 1 (ESR1) in human and mouse embryos and determine the effect of estradiol (E2) supplementation on pre- and peri-implantation blastocyst development.
Methods
Mouse embryos, 8-cell through hatched blastocyst stages, and human embryonic days 5–7 blastocysts were stained for ESR1 and imaged using confocal microscopy. We then treated 8-cell mouse embryos with 8 nM E2 during in vitro culture (IVC) and examined embryo morphokinetics, blastocyst development, and cell allocation into the inner cell mass (ICM) and trophectoderm (TE). Finally, we disrupted ESR1, using ICI 182,780, and evaluated peri-implantation development.
Results
ESR1 exhibits nuclear localization in early blastocysts followed by aggregation, predominantly in the TE of hatching and hatched blastocysts, in human and mouse embryos. During IVC, most E2 was absorbed by the mineral oil, and no effect on embryo development was found. When IVC was performed without an oil overlay, embryos treated with E2 exhibited increased blastocyst development and ICM:TE ratio. Additionally, embryos treated with ICI 182,780 had significantly decreased trophoblast outgrowth during extended embryo culture.
Conclusion
Similar ESR1 localization in mouse and human blastocysts suggests a conserved role in blastocyst development. These mechanisms may be underappreciated due to the use of mineral oil during conventional IVC. This work provides important context for how estrogenic toxicants may impact reproductive health and offers an avenue to further optimize human-assisted reproductive technology (ART) to treat infertility.




Similar content being viewed by others
Data Availability
Data available within the article or its supplementary materials.
References
Vasquez YM, DeMayo FJ. Role of nuclear receptors in blastocyst implantation. Semin Cell Dev Biol. 2013;24(10–12):724–35. https://doi.org/10.1016/j.semcdb.2013.08.004.
Martin L, Finn CA, Carter J. Effects of Progesterone and oestradiol-17β on the luminal epithelium of the mouse uterus. Reproduction. 1970;21(3):461–469. https://rep.bioscientifica.com/view/journals/rep/21/3/jrf_21_3_010.xml
Finn CA, Martin L. Hormone secretion during early pregnancy in the mouse. J Endocrinol. 1969;45(1):57–65. https://doi.org/10.1677/joe.0.0450057.
Ma WG, Song H, Das SK, Paria BC, Dey SK. Estrogen is a critical determinant that specifies the duration of the window of uterine receptivity for implantation. Proc Natl Acad Sci U S A. 2003;100(5):2963–8. https://doi.org/10.1073/pnas.0530162100.
Huet-Hudson YM, Andrews GK, Dey SK. Cell type-specific localization of c-Myc protein in the mouse uterus: modulation by steroid hormones and analysis of the periimplantation period. Endocrinology. 125(3):1683–1690. https://doi.org/10.1210/endo-125-3-1683.
McCormack JT, Greenwald GS. Evidence for a preimplantation rise in oestradiol-17β levels on day 4 of pregnancy in the mouse. Reproduction. 1974;41(2):297–301.
Bhatt H, Brunet LJ, Stewart CL. Uterine expression of leukemia inhibitory factor coincides with the onset of blastocyst implantation. Proc Natl Acad Sci. 1991;88(24):11408–12.
Kumar V, Green S, Sftack G, Berry M, Jinn J, Chambon P. Functional domains of the human estrogen receptor. Cell. 1987;51:941–5.
Kuiper GG, Enmark E, Pelto-Huikko M, Nilsson S, Gustafsson JA. Cloning of a novel estrogen receptor expressed in rat prostate and ovary. Proc Nat Acad Sci U S A. 1996;93:5925–30.
Filardo EJ, Quinn JA, Bland KI, Frackelton AR Jr. Estrogen-induced activation of Erk–1 and Erk–2 requires the G protein-coupled receptor homolog, GPR30, and occurs via trans-activation of the epidermal growth factor receptor through release of HB-EGF. Mol Endocrinol. 2000;14:1649–60.
Prossnitz ER, Arterburn JB, Sklar LA. GPR30: A G protein-coupled receptor for estrogen. Mol Cell Endocrinol. 2007;265–266:138–42. https://doi.org/10.1016/j.mce.2006.12.010.
Hou Q, Gorski J. Estrogen receptor and progesterone receptor genes are expressed differentially in mouse embryos during preimplantation development. Proc Nat Acad Sci U S A. 1993;90(20):9460–4.
Chang KT, Su YT, Tsai YR, Lan KC, Hsuuw YD, Kang HY, Chan WH, Huang FJ. High levels estradiol affect blastocyst implantation and post-implantation development directly in mice. Biomed J. 2021;16:S2319–4170(21)00003–2. https://doi.org/10.1016/j.bj.2021.01.004.
Hou Q, Paria BC, Mui C, Dey SK, Gorski J. Immunolocalization of estrogen receptor protein in the mouse blastocyst during normal and delayed implantation. Proc Natl Acad Sci U S A. 1996;93(6):2376–81. https://doi.org/10.1073/pnas.93.6.2376.
Cheng X, Xu S, Song C, He L, Lian X, Liu Y, Wei J, Pang L, Wang S. Roles of ERα during mouse trophectoderm lineage differentiation: revealed by antagonist and agonist of ERα. Dev Growth Differ. 2016;58(3):327–38. https://doi.org/10.1111/dgd.12276.
Saito K, Furukawa E, Kobayashi M, Fukui E, Yoshizawa M, Matsumoto H. Degradation of estrogen receptor α in activated blastocysts is associated with implantation in the delayed implantation mouse model. Mol Hum Reprod. 2014;20(5):384–91. https://doi.org/10.1093/molehr/gau004.
Dupont S, Krust A, Gansmuller A, Dierich A, Chambon P, Mark M. Effect of single and compound knockouts of estrogen receptors alpha (ER alpha) and beta (ER beta) on mouse reproductive phenotypes. Development. 2000;127(19):4277–91. https://doi.org/10.1242/dev.127.19.4277.
Walker VR, Korach KS. Estrogen receptor knockout mice as a model for endocrine research. ILAR J. 2004;45(4):455–61. https://doi.org/10.1093/ilar.45.4.455.
Gorski J, Hou Q. Embryonic estrogen receptors: do they have a physiological function? Environ Health Perspect. 1995;103 Suppl 7(Suppl 7):69–72. https://doi.org/10.1289/ehp.95103s769.
Paria BC, Lim H, Wang XN, Liehr J, Das SK, Dey SK. Coordination of differential effects of primary estrogen and catecholestrogen on two distinct targets mediates embryo implantation in the mouse. Endocrinology. 1998;139(12):5235–46. https://doi.org/10.1210/endo.139.12.6386.
Paria BC, Chakraborty C, Dey SK. Catechol estrogen formation in the mouse uterus and its role in implantation. Mol Cell Endocrinol 69(1):1990, Pages 25–32, ISSN 0303–7207. https://doi.org/10.1016/0303-7207(90)90085-M.
Hernández N, López-Morató M, Perianes MJ, Sánchez-Mateos S, Casas-Rua V, Domínguez-Arroyo JA, Sánchez-Margallo FM, Álvarez IS. 4-Hydroxyestradiol improves mouse embryo quality, epidermal growth factor-binding capability in vitro and implantation rates. Mol Hum Reprod. 2021;27(2):gaaa075. https://doi.org/10.1093/molehr/gaaa075.
Dickmann Z, Gupta JS, Dey SK. Does “blastocyst estrogen” initiate implantation? Science. 1977;195(4279):687–8. https://doi.org/10.1126/science.841306.
Valbuena D, Martin J, de Pablo JL, Remohí J, Pellicer A, Simón C. Increasing levels of estradiol are deleterious to embryonic implantation because they directly affect the embryo. Fertil Steril. 2001;76(5):962–8. https://doi.org/10.1016/s0015-0282(01)02018-0.
Deglincerti A, Croft GF, Pietila LN, Zernicka-Goetz M, Siggia ED, Brivanlou AH. Self-organization of the in vitro attached human embryo. Nature. 2016;533(7602):251–4. https://doi.org/10.1038/nature17948.
Bedzhov I, Leung CY, Bialecka M, Zernicka-Goetz M. In vitro culture of mouse blastocysts beyond the implantation stages. Nat Protoc. 2014;9(12):2732–9. https://doi.org/10.1038/nprot.2014.186.
Shahbazi MN, Jedrusik A, Vuoristo S, Recher G, Hupalowska A, Bolton V, Fogarty NNM, Campbell A, Devito L, Ilic D, Khalaf Y, Niakan KK, et al. Self-organization of the human embryo in the absence of maternal tissues. Nat Cell Biol. 2016;18(6):700–8. https://doi.org/10.1038/ncb3347.
Logsdon DM, Grimm CK, West RC, Engelhorn HJ, Kile R, Reed LC, Swain JE, Katz-Jaffe M, Schoolcraft WB, Krisher RL, Yuan Y. Maternal physiology and blastocyst morphology are correlated with an inherent difference in peri-implantation human embryo development. Fertil Steril. 2022;30:S0015–0282(22)00137–6. https://doi.org/10.1016/j.fertnstert.2022.02.018.
Institute of Laboratory Animal Resources (ILAR). Guide for the care and use of laboratory animals. [8th] ed. Washington, D.C.: National Academy Press; 2011.
Ermisch AF, Herrick JR, Pasquariello R, Dyer MC, Lyons SM, Broeckling CD, Rajput SK, Schoolcraft WB, Krisher RL. A novel culture medium with reduced nutrient concentrations supports the development and viability of mouse embryos. Sci Rep. 2020;10(1):9263. https://doi.org/10.1038/s41598-020-66019-4.
Herrick JR, Strauss KJ, Schneiderman A, Rawlins M, Stevens J, Schoolcraft WB, et al. The beneficial effects of reduced magnesium during the oocyte-to-embryo transition are conserved in mice, domestic cats and humans. Reprod Fertil Dev. 2015;27:323–31.
Schindelin J, Arganda-Carreras I, Frise E, Kaynig V, Longair M, Pietzsch T, et al. Fiji: an open-source platform for biological-image analysis. Nat Methods. 2012;9:676–82.
Logsdon DM, Ermisch AF, Kile R, Schoolcraft WB, Krisher RL, Yuan Y. Egg cylinder development during in vitro extended embryo culture predicts the post transfer developmental potential of mouse blastocysts. J Assist Reprod Genet. 2020;37(4):747–52. https://doi.org/10.1007/s10815-020-01714-9.
Hayward MA, Mitchell TA, Shapiro DJ. Induction of estrogen receptor and reversal of the nuclear/cytoplasmic receptor ratio during vitellogenin synthesis and withdrawal in Xenopus laevis. J Biol Chem. 1980;255(23):11308–12.
Gao Y, Liu X, Tang B, Li C, Kou Z, Li L, Liu W, Wu Y, Kou X, Li J, Zhao Y, Yin J, Wang H, Chen S, Liao L, Gao S. Protein expression landscape of mouse embryos during pre-implantation development. Cell Rep. 2017;21(13):3957–69. https://doi.org/10.1016/j.celrep.2017.11.111.
Chen F, Ma B, Lin Y, Luo X, Xu T, Zhang Y, Chen F, Li Y, Zhang Y, Luo B, Zhang Q, Xie X. Comparative maternal protein profiling of mouse biparental and uniparental embryos. Gigascience. 2022;11:giac084. https://doi.org/10.1093/gigascience/giac084.
Strömstedt M, Keeney DS, Waterman MR, Paria BC, Conley AJ, Dey SK. Preimplantation mouse blastocysts fail to express CYP genes required for estrogen biosynthesis. Mol Reprod Dev. 1996;43(4):428–36. https://doi.org/10.1002/(SICI)1098-2795(199604)43:4<428::AID-MRD4>3.0.CO;2-R. Yu LL, Qu T, Zhang SM,Yuan DZ, Xu Q, Zhang JH, He.
Dey SK, Dickmann Z. Δ5-32-Hydroxysteroid dehydrogenase activity in rat embryos on days 1 through 7 of pregnancy. Endocrinology. 1974;95(1):321–2. https://doi.org/10.1210/endo-95-1-321.
Hoversland RC, Dey SK, Johnson DC. Aromatase activity in the rabbit blastocyst. J Reprod Fertil. 1982;66(1):259–63. https://doi.org/10.1530/jrf.0.0660259.
Dey SK, Dickmann Z. Estradiol-17β-hydroxysteroid dehydrogenase activity in preimplantation rat embryos. Steroids 24(1):1974, Pages 57–62,ISSN 0039–128X. https://doi.org/10.1016/0039-128X(74)90045-2.
Gene Expression Omnibus (GEO) National Center for Biotechnology Information. Bethesda, MD; 2010 17βHSD in human blastocysts: https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSM456658 CYP19A1 in human blastocysts: https://www.ncbi.nlm.nih.gov/geo/tools/profileGraph.cgi?ID=GDS3959:203475_at. Accessed on 12/29/2022
Petropoulos S, Edsgärd D, Reinius B, Deng Q, Panula SP, Codeluppi S, Plaza Reyes A, Linnarsson S, Sandberg R, Lanner F. Single-cell RNA-seq reveals lineage and X chromosome dynamics in human preimplantation embryos. Cell. 2016;165(4):1012–26. https://doi.org/10.1016/j.cell.2016.03.023. Erratum in: Cell. 2016;167(1):285.
Miller KF, Pursel VG. Absorption of compounds in medium by the oil covering microdrop cultures. Gamete Res. 1987;17(1):57–61. https://doi.org/10.1002/mrd.1120170107.
Yoshinaga K, Adams CE. Delayed implantation in the spayed, progesterone treated adult mouse. J Reprod Fertil. 1966;12(3):593–5. https://doi.org/10.1530/jrf.0.0120593.
Ptak GE, Tacconi E, Czernik M, Toschi P, Modlinski JA, Loi P. Embryonic diapause is conserved across mammals. PLoS One. 2012;7(3):e33027. https://doi.org/10.1371/journal.pone.0033027.
Liu Y, Jones C, Coward K. An investigation of mechanisms underlying mouse blastocyst hatching: a ribonucleic acid sequencing study. F S Sci. 2022;3(1):35–48. https://doi.org/10.1016/j.xfss.2021.12.003.
Segnitz B, Gehring U. Subunit structure of the nonactivated human estrogen receptor. Proc Natl Acad Sci U S A. 1995;92(6):2179–83. https://doi.org/10.1073/pnas.92.6.2179.
Echeverria PC, Picard D. Molecular chaperones, essential partners of steroid hormone receptors for activity and mobility. Biochim Biophys Acta. 2010;1803(6):641–9. https://doi.org/10.1016/j.bbamcr.2009.11.012.
Kushner PJ, Agard DA, Greene GL, Scanlan TS, Shiau AK, Uht RM, Webb P. Estrogen receptor pathways to AP-1. J Steroid Biochem Mol Biol. 2000;74(5):311–7. https://doi.org/10.1016/s0960-0760(00)00108-4.
Moriyama T, Yoneda Y, Oka M, Yamada M. Transportin-2 plays a critical role in nucleocytoplasmic shuttling of oestrogen receptor-α. Sci Rep. 2020;10(1):18640. https://doi.org/10.1038/s41598-020-75631-3.
Zivadinovic D, Watson CS. Membrane estrogen receptor-alpha levels predict estrogen-induced ERK1/2 activation in MCF-7 cells. Breast Cancer Res. 2005;7(1):R130–44. https://doi.org/10.1186/bcr959.
Kahlert S, Nuedling S, van Eickels M, Vetter H, Meyer R, Grohe C. Estrogen receptor alpha rapidly activates the IGF-1 receptor pathway. J Biol Chem. 2000;275(24):18447–53. https://doi.org/10.1074/jbc.M910345199.
Lee JS, Tocheny CE, Shaw LM. The insulin-like growth factor signaling pathway in breast cancer: an elusive therapeutic target. Life (Basel). 2022;12(12):1992. https://doi.org/10.3390/life12121992.
Sampayo RG, Toscani AM, Rubashkin MG, Thi K, Masullo LA, Violi IL, Lakins JN, Cáceres A, Hines WC, Coluccio Leskow F, Stefani FD, Chialvo DR, et al. Fibronectin rescues estrogen receptor α from lysosomal degradation in breast cancer cells. J Cell Biol. 2018;217(8):2777–98. https://doi.org/10.1083/jcb.201703037.
Corson LB, Yamanaka Y, Lai KM, Rossant J. Spatial and temporal patterns of ERK signaling during mouse embryogenesis. Development. 2003;130(19):4527–37. https://doi.org/10.1242/dev.00669.
Saba-El-Leil MK, Vella FD, Vernay B, Voisin L, Chen L, Labrecque N, Ang SL, Meloche S. An essential function of the mitogen-activated protein kinase Erk2 in mouse trophoblast development. EMBO Rep. 2003;4(10):964–8. https://doi.org/10.1038/sj.embor.embor939.
Chang L, Karin M. Mammalian MAP kinase signalling cascades. Nature. 2001;410:37–40. https://doi.org/10.1038/35065000.
Funding
Research was internally funded by the Colorado Center for Reproductive Medicine.
Author information
Authors and Affiliations
Contributions
DML designed and completed all experiments and wrote the manuscript. AC assisted in the experimentation and original experimental design. WBS provided funds and oversaw collection and donation of all human tissues. RLK and YY guided experimental design and assisted in manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Logsdon, D.M., Churchwell, A., Schoolcraft, W.B. et al. Estrogen signaling encourages blastocyst development and implantation potential. J Assist Reprod Genet 40, 1003–1014 (2023). https://doi.org/10.1007/s10815-023-02783-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-023-02783-2