Abstract
The main reasons why Amniotic Membrane (AM) is transplanted in Ophthalmology are: to provide a substrate for cellular growth and to provide tectonic support or as a biological bandage and barrier that protects the wound to facilitate an environment for wound healing. The application of AM is well-documented in corneal disorders of various aetiologies [1], however, research within the field has highlighted how it can be used in conjunctival disorders and most recently, in glaucoma and vitreoretinal procedures. This review explores the preservation modalities of AM and summarises the current literature regarding AM transplantation in Glaucoma and Vitreoretinal conditions. AM transplantation in conjunction with trabeculectomy was reported to be used in two different surgical techniques. They differ in relation to the position of the implant: below the scleral flap or over the entire exposed sclera. The results of these studies suggest that AM transplant is a safe procedure that helps in the improvement of the intraocular pressure when associated with trabeculectomies. Moreover, it enhances trabeculectomies success rates when used along with mitomycin C [2]. The use of AM is also described for managing leaking blebs. It is mentioned to be a suitable alternative to conjunctival advancement. Regarding AM transplantation in glaucoma shunt or valve surgeries, the current literature is relatively limited. However, AM has been described as a good tectonic support for shunt procedures [3]. Successful results are described in the literature for surgical treatments using AM plug for vitreoretinal procedures. In particular macular hole closure and rhegmatogenous retinal detachment. In conclusion, AM transplant is a very promising and versatile adjutant therapy. However, further studies are also required for a better understanding and refinement of surgical techniques.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction to amniotic membrane transplantation
Historical development of amniotic membrane transplantation
AM is the innermost layer of the placental sac, which nurtures the baby during pregnancy [4]. The AM was first transplanted in ophthalmology in the 1940’s by De Rotth et al. [5], with only fresh AM being available as a treatment option. However, AM transplantation gained popularity in the 1990’s as a widespread and established treatment once preservation modalities were developed to store and transport tissue.
The use of AM in corneal and ocular surface disease pathologies is already well documented in the literature. So it will not be explored in detail in this paper. AM is known for example, to be helpful in the treatment of dry eye disease [6] and ocular burns [7] among others. AM is transplanted in different forms for ocular surface conditions such as patch, graft [7], extract or extract eye drops [8].
Amniotic membrane structure
Different descriptions of the AM layers are found in the literature. To the best of our knowledge, the AM has been commonly subdivided into 3 layers [9,10,11]: (i) epithelium, a monolayer of cuboidal cells which are metabolically active; (ii) basement membrane (iii) and stroma layer, an avascular layer which itself can be subdivided in three other layers (a compact layer, a fibroblast layer and a spongy layer).
However, a different classification (into 5 layers) has also been found in the literature. Walkden [4] describes the layer structure of the AM as: (i) epithelium, (ii) basement membrane, (iii) stromal extracellular matrix (ECM) - which consists of compact and fibroblast layers. (iv) spongy layer and (v) Chorion.
Methods of preservation
To allow for the ease of access to tissue transplantation, AM preservation methods have been developed to provide the ability to have the therapy thoroughly tested for infectious diseases, transported, and stored prior to use. AM is collected from consenting mothers undergoing elective caesarean section, processed in aseptic conditions, and tested for a range of transmissible diseases prior to preservation [4, 12]. The aim of AM preservation is to keep it as close to the native tissue as possible and to provide an on-demand, accessible therapy.
Cryopreservation
Cryopreservation involves freezing the AM at −80 °C, after the tissue has been washed with a cryoprotectant such as phosphate buffered silane in dimethylsulfoxide [13] or Eagle’s Minimum Essential Medium [14]. This form of preservation accounts for a largest amount of AM products on the market [15].The degradation of the tissue through enzymatic reactions has been reported to be limited at this temperature and the AM is deemed non-viable. Tissue must be kept frozen during transport and storage, meaning it is subject to the challenges associated with cold chain logistics and prior to use it must be thawed. Literature has noted that this thawing process causes a loss in the soluble factors that are presumed to be beneficial for healing [15,16,17,18]. Additional to this, ice crystal formation during the freezing process has been reported to cause issues to the cellular integrity and tissue structure [15].
Freeze-drying (or lyophilisation)
Freeze drying of AM conventionally involves the same initial freezing stages as cryopreservation, as the tissue is frozen to −80 °C and sublimation is used to remove water from the tissue. This sublimation process halts any enzymatic reactions taking place within the cells that can alter the tissue state [19]. This presents a dry stable tissue, which does not require cold chain storage and logistics that can be rehydrated prior to use [20]. However, as the tissue is frozen its structural integrity can be compromised by ice crystal formation [15]. Lyophilised AM can also be stored for long periods of time.
Preservation through heat or air drying
This process involved using heat or air to remove any residual moisture from processed tissue to preserve it [4]. This process prevents any damage from freezing the tissue. Literature has noted that AM preserved by heat or air drying are the thinnest tissues at around 20–30 microns [21]. This technique is relatively uncommon due to the difficulties in standardising the technique.
Low temperature vacuum evaporation
Low temperature vacuum evaporation techniques involve treating the tissue with a sugar protectant, such as trehalose to preserve and stabilise tissue structure, cellular membrane, and proteins [15, 22]. Residual water is delicately removed through cool temperatures paired with specified vacuums to lead to a dried product. The sugar protectants used in the preservation process replace intracellular water to prevent any damage to the AMs cellular matrix [15, 23]. Tissue preserved through low temperature vacuum evaporation can be shipped and stored without any logistical issues allowing it be available worldwide and in warzones [4].
Irradiation methods
Most commonly tissue preparations are treated with antibiotic and antimycotic solution during their preservation processes to remove the remanence of bacteria and fungus, however, some tissue preparations undergo further sterilisation by irradiation such as gamma sterilisation [20] or by using fluids, such as carbon dioxide in a supercritical state [24]. However, there has been reports that terminal sterilisation can compromise tissue integrity [21, 22]. Recent publications by Marsit et al. [25] have reported an antibiotic-based, aseptic decontamination technique that can be used for dried AM.
Amniotic membrane application methods
AM may be transplanted in several ways, dependent on the ophthalmic modality that is being treated [4, 13]. The type of transplantation required depends on the location, size and depth of the wound [4].
Inlay-graft (Graft)
An inlay-graft, also referred to as graft, application of AM is applied epithelial-side-up in the bed of the wound. The tissue acts as a barrier or scaffold, similar to the basement membrane that allows for epithelisation to take place on top of it [12] and therefore, the tissue is permanently incorporated into the ocular surface over time. A single or multi-layer graft may be placed, dependent on the depth of the wound. AM forms hemidesmosomes and desmosomes that provide its ability to incorporate into the ocular stroma [10].
Onlay-graft (Patch)
An onlay-graft, regularly referred to as a patch application of AM acts as a temporary biological bandage that acts as a barrier to protect the wound from external damage or pressure from the eyelids [4]. Patch transplantation is normally used in conditions with superficial damage or extreme inflammatory disorders. The amnion is applied epithelial-side-down against the wound [10]. For conditions that affect the entire mucosal surface, patch transplantation can protect from the formation of symblepharon and ankyloblepharon by providing a barrier between exposed or inflamed tissues [26, 27]. Patch AM transplantations can be replaced during the treatment period to give a renewed benefit and to help to drive ocular surface stabilisation [28].
Sandwich-graft (Sandwich)
The sandwich AM transplantation technique can also be referred to as the combined technique [10]. An inlay-graft is placed into the bed of the wound and an onlay-graft is used to cover it [4, 13, 29]. Sandwich graft technique has the purpose to guide the growth of a new epithelium between the inlay and onlay grafts [30, 31].
Folded AM graft
Eliezer et al. described the use of AM in trabeculectomy using a folded AM graft. A 5x5 mm graft is folded to have the stromal layer facing both superior and inferior sides of the implant. It is than fixated over the sclera with two 10.0 nylon suture [32].
In-office use
Most frequently, AM implant is used in procedures performed in theatres. However, sutureless in-office application has also been reported as a less invasive option for ocular surface diseases. The advantage of this method is that it allows the AM implant to be done faster and in earlier stages of ocular surface conditions, for instance keratitis, corneal ulcers, and chemical burns. Mcguaghy et all describe two different types of in-office AM implant manufactures: ProKera and AmbioDisk. Both are applied under topical antithetic and require saline irrigation of the graft. AmbioDisk is advised to be used with a bandage contact lens covering the AM disc [33].
The benefits of amniotic membrane transplantation
The specific mode of action of AM has not been completely quantified but it is known to be a combination of the barrier function of the tissue from structural benefits, which is complimented by the bioactive proteins within the tissue structure [4, 13, 34]. These properties work synergistically to have a homologous benefit when used as a tissue transplant.
Promotion of epithelisation
AMs ability to promote epithelisation is a dual synergistic effect between structural substrate benefits and the presence of bioactive proteins, which are delivered to the wound [4, 35, 36]. The extracellular matrix of the AM resembles the structure of the cornea and conjunctiva [4]. This allows the tissue to act as a replacement basement membrane in the case where tissue is lost or damage to provide a barrier for wound healing to occur on [30, 37]. AM contains a range of trophic factors, such as epidermal growth factor, neurotrophic substances and keratocyte growth factors that are delivered to the wound following application [35, 36], which have been shown to aid the healing process.
Anti-inflammatory and immunosuppressive action
AM transplantation limits the development and continuation of the inflammatory process through an immunosuppressive mechanism that limits the infiltration of infiltrating immune cells. Shimmura et al. noted that inflammatory cells are trapped with the AM’s stroma, where they undergo apoptosis and therefore, do no cause an inflammatory cascade at the ocular surface [38]. AM has an extracellular matrix within the stroma, this complex is reported to contain heavy chain protease inhibitors of heavy chain 1 of inter-\(\alpha\)-trypsin and hyaluronan/pentraxin3 (HC-HA/PTX3) [39, 40]. The inhibition of HC-HA/PTX3 is known to contribute to the anti-inflammatory, anti-fibrotic and anti-angiogenic mode of action of AM. Finally, pro-inflammatory cytokines, such as interleukin (IL-)-1a, IL-2, IL-8, IL-10 and tumour necrosis factor-beta have their expression inhibited by AM transplantations [41].
Mechanical properties
The AM tends to be between \(20 \,{\rm and} \,500 \,\mu {\rm m}\) [9]. The basement membrane of the AM closely resembles that of the cornea and conjunctiva, regarding its collagen composition [42]. This property means AM can be an effective substrate to replace the missing ocular tissue to provide a basement membrane for epithelisation to take place [10].
Glaucoma
For glaucoma patients with appropriate indication, AM can be transplanted as a secondary adjunct to surgical procedures to replace lost or missing conjunctiva, which can leave the sclera exposed [4]. AM is known to reduce scarring at the time of the filtering surgery; repair any early or late blebs and act as a protective cover in valve procedures [43]. When used in conjunction with any glaucoma surgery, AM transplantation is used to protect and cover any exposed sclera to improve both patient outcomes and the rate of complications [44, 45]. It should be noted that as AM is a human tissue, it can have variable persistence time dependent on the inflammation present at the ocular surface and the method of application. Although literature reports its high tensile strength and ability to be excellent for host-tissue integration [46]. Table 1 summarises some useful papers on glaucoma.
In conjunction with trabeculectomy
For glaucoma surgeries, the use of AM transplantation in conjunction with trabeculectomy procedures is the most documented glaucoma indication [4, 13]. First reported by Fujishima et al. [47] the surgical procedure for AMtransplantation following trabeculectomy is yet to be standardised. Some studies report the placement of the AM below of scleral flap in a ‘inlay-graft’ fashion [48, 49], however, other studies state that the tissue is placed over the wound in an ‘onlay-graft’ fashion to over the entire exposed scleral bed [32, 44, 50]. As a whole, data shows the application of AM epithelial-side-down [2] when placed onto the wound. Although these differences are present, no obvious differences have been noted regarding outcomes dependent on surgical technique. Future research in this area has the potential to define if different surgical methodologies may lead to higher success rates.
In 2015, Wang et al. [51] conducted a meta-analysis on the data of device modified trabeculectomy procedures for glaucoma conditions. This analysis studied 33 papers that met the inclusion criteria, which included 18 studies utilising AM. These studies reported that tissue transplantation is associated with a lower intraocular pressure at 12 months, compared to trabeculectomy alone [51]. Although this review was limited by the loss of follow-up in 11/18 studies, but this collation of data presented the benefits of AM as an adjunct to this procedure.
Following this, Shen et al. [2] ran a meta-analysis of randomised controlled clinical trials that assess the AM assisted trabeculectomy to trabeculectomy alone. Shen et al’s meta-analysis included 174 eyes across 5 studies, the data noted that there was a statistically significant benefit in the intraocular pressure of patients in the AM treatment group at 3 months (\(p < 0.0003\)) and 12 months (\(p = 0.02\)). Whilst the complete success of patients’ procedures in the AM group were also significant at 6 months (\(p = 0.02\)) and 12 months (\(p = 0.003\)) compared to the trabeculectomy alone group. Additional to this, fewer complications were noted in the AM group. However, no benefit observed differences regarding the number of anti-glaucoma medications; hypotony; encapsulated bleb and choroidal detachment. In conclusion, Shen et al. noted that AM transplantation with trabeculectomy is a safe and efficient treatment compared to trabeculectomy alone.
Studies have researched the use of AM transplantation paired with mitomycin-c application when undergoing trabeculectomy to trabeculectomy and mitomycin-c alone. Sheha et al. [48] studied 37 eyes in a two-arm comparative study. Complete success at 6 months was noted 93.6% (15/16) of the study eyes, compared to 9/15 (60%) of the trabeculectomy alone control eyes. The AM treatment group saw statistically significantly improved intraocular pressure compared to the control group at 3-months (\(p = 0.0002\)), 6-months (\(p < 0.0001\)), 9-months (\(p < 0.0001\)) and 12-months(\(p < 0.0001\)). Sheha et al. [48] noted that the use of mitomycin-c and AM combined in a trabeculectomy with mitomycin-c procedure providers lower intraocular pressure, higher success rates and fewer complications.
Most recently, Roque et al. presented a retrospective study of 51 eyes of 45 glaucoma patients, which compared trabeculectomy with mitomycin-c application to patients who had undergone trabeculectomy with mitomycin-c and amniotic membrane. This study showed no significant difference between the two groups, however, it should be noted that this was not a randomised and controlled cohort of patients due to the retrospective nature of the study [52].
During glaucoma procedures, mitomycin-c is used to limit scar formation and to improve the bleb formation following trabeculectomy procedures [53]. However, mitomycin-c can cause the formation of thin-walled blebs, which can lead to over-filtration, hypotony and can form serious complications such as: bleb leaks; bleb infections and endophthalmitis [53]. Therefore, AM has a potential to improve the success rate and lower the complications rate of trabeculectomies with mitomycin-c even further [2].
Published clinical data supports the use of AM in conjunction with trabeculectomy procedures, and this also may be supported using mitomycin-c in the procedure too. However, further research is required tos define the most beneficial surgical technique of above or below the scleral flap, as placement as an onlay-graft or inlay-graft.
Trabeculectomy surgeries is known to rely on the availability of mitomicin-C. At the end of 2019, the world experienced an international shortage of this vital medication for glaucoma surgeons [54, 55]. Taking this into account, studies regarding the AM as a possible substitute for mitomycin-C has an extreme importance to be considered.
Leaking bleb fixture
For patients undergoing AM transplantation to manage a leaking bleb, the tissue is placed over the bare sclera, often epithelial-side-down [56]. The AM is supported by the corneoscleral limbus with the opposite side being undermined under the healthy conjunctival tissue and secured in place at both areas [56]. The aim of this treatment is to reduce inflammation, vascularisation and allow for the intraocular pressure of the patient to allow for stabilisation.
A meta-analysis was published by Bochmann et al., in 2012 [57] that noted the variations of treatments for managing late trabeculectomy bleb leaks. Within the Bochmann et al. analysis, one randomised controlled study of 30 eyes of 30 patients by Budenz et al. [58] matched the inclusion criteria and was included in the analysis. The study arms compared patients treated with conjunctival advancement to those who underwent AM transplantation. The primary outcome of the study was the sealing of the bleb leak confirmed by a negative Seidel’s test after 1 month, 1 year and 5 years. In the 19.5 ± 6.9 months follow-up period, the cumulative survival rate of the bleb reconstruction was 81% at 6 months and 74% at 1 year for the amniotic membrane group. However, it was at 100% for conjunctival advancement for the follow-up period. Recurrence of the bleb was seen in seven of the AM cases, with two persistent leaks and three that required repeat surgery. However, intra-ocular pressure, visual acuity and the number of glaucoma medications prescribed were comparable between the two groups.
The long-term outcomes (\(73 \pm 7\) months) of the patient cohort included in the Budenz et al. study were evaluated by Rauscher et al. [59]. During this analysis, it was noted that there was no significant difference in patients’ intraocular pressure, final visual acuities, or difference in the number of glaucoma medications. Bleb vascularity was significantly lower in the AM group (\(p = 0.2\)) when comparing failed bleb repair, 7/30 of the AM group failed with 4/30 of the conjunctival advancement group failing (\(p = 0.44\)), showing no statistically significant difference. Rauscher et al. concluded that although prone to early potential failure, AM may be a suitable alternative to conjunctival advancement in the long-term.
Since the release of Bochmann et al’s meta-analysis, Sethi et al. [60] published a retrospective case series on patients who underwent sub-conjunctival AM draping to repair leaking cystic blebs. Of the 17 eyes of 16 patients included in the study at a follow-up of \(21.4 \pm 7.3\) months, a success rate of 88% (15/17 eyes) was noted, patients saw a stabilisation of the intraocular pressure from \(5.7 \pm 2.8\) mmHg to \(13.1 \pm 3.4\) mmHg and LogMAR visual acuity improved from \(0.7 \pm 0.8\) preoperatively to \(0.1 \pm 0.1\) LogMAR units (\(p < 0.030\)).
The data regarding the use of AM transplantation as an adjuvant to manage leaking blebs is relatively mixed. Although the technique is viewed as being safe, there are more effective treatment methods available, such as conjunctival advancement. Therefore, this technique may be most viable in patients with a lack of conjunctival tissue, where alternative treatment options are required. Otherwise, further research is required to refine the surgical technique to evaluate if there is a potential for the improvement of AM use in the management of leaking blebs.
Glaucoma valve or shunt implantation
A glaucoma shunt tube or valve will be covered using a range of transplantation materials. This includes: pericardium, donor corneal tissue, sclera, collagen matrixes or AM. The aim of covering the implantation is to avoid erosion, which can cause implantation exposure [61, 62]. Ainsworth et al. in 2006 [63] first noted the application of AM to manage exposed tubes following a glaucoma tube shunt surgery in a small case series of 3 patients. In one of these cases, they described a technique using a double AM graft to cover the tube from the glaucoma drainage device (GDD). The GDD tube is first covered by a full thickness scleral patch, sutured with four 9.0 nylon stitches. Then the first AM graft is placed with epithelial side up. The size of this graft is described to be larger than the above conjunctival defect. The conjunctiva is placed above the first AM implant, noticing that between the conjunctiva edges, a gap is kept. Four 10.0 nylon sutures fixate the conjunctiva to the underlying epsclera/AM draft. In sequence the second AM patch is applied over the epithelial defect. This second AM patch is larger than the epithelial defect and is placed with epithelial side down. Finally, four 6.0 nylon sutures are done at the margins of the second AM patch to keep it in the right position.
The use specifically in ahmed glaucoma valve procedure was noted by Amini et al. in 2010 [64]. The largest study in this area has been conducted by Yazdani et al. in 2016 [53], a randomised, double-masked 3 arm clinical trial of 75 eyes of 75 patients. The patient arms included ahmed glaucoma valve (AGV) alone compared to AGV with mitomycin-c compared to AGV with AM transplantation. Patients in the AM arm had their AGV wrapped with tissue prior to implantation with the aim to reduce fibrosis and postoperative vascularisation. Regarding intraocular pressure, at 12-weeks no statistically significant difference was noted (\(p = 0.13\)) between all three arms. Similar to this, there was no difference in the number of glaucoma medications taken by patients in any of the arms (\(p = 0.22\)). This study is limited by the short follow-up time of 12 months. A longer-term study is required to further assess the benefit of this treatment. Both AM and mitomycin-c have been shown to be safe methods of treatment, however, in this study, neither were associated with improved outcomes within the 12-month follow-up period.
In regard to glaucoma shunt addition, Sheha et al. in 2011 [3] conducted a retrospective case series of 44 eyes who underwent the implantation of a glaucoma drainage device with an AM graft. The patients had a follow-up of \(22 \pm 3\) months. Of the cohort, 93% (41/44) of eyes had a successful procedure. The incidence of tube exposure was 2.3%, which is comparable to alternative substrate materials that are applied in these conditions. Sheha et al. [3] concluded that AM presented good tectonic support and allows for the clinician to have direct visualisation of the implanted shunt through the conjunctiva and tissue graft. Some cases have reported the use of a double layer AM transplantation when protecting a shunt tube to provide additional durability and support, if the AM transplantation were to begin to degrade [65].
The current body of literature with AM transplantation in glaucoma shunt or valve surgeries is relatively limited and offers the opportunity to be further explored to fully provide data regarding its long-term effectiveness for recipients. The most common reported surgical methodology for applying the AM in shunt procedures is during the primary procedure [66, 46], however, there is additional reports where AM has been transplanted following an exposed shunt tube, which may or may not have been covered with other transplant materials (i.e. scleral flap or pericardium) [67].
Vitreoretinal procedures
The potential to utilise AM transplantation in retinal and vitreous procedures is a new, novel and developing area of research. AM has traditionally only been utilised for treatment for conditions of the ocular surface, but its wound healing function is now being placed in vitreoretinal procedures. AM has been proved a helpful tool in treatment of large macular tears, high myopic retinal detachment associated with macula hole, paravascular tears, serous macular detachment associated with optic pits, complicated retinal detachment and advanced age related macular degeneration (AMD) [68]. Table 2 summarises several important vitreoretinal papers.
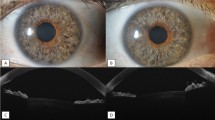
Macular hole closure
Recent publications have noted the use of amniotic membrane transplant in conjunction with vitrectomy for the treatment of macular holes [69,70,71]. Studies in vivo and in vitro have shown that AM transplantation can promote the regeneration of retinal tissue when placed under the fovea [72,73,74]. It has been noted that measuring the macular hole through ocular surface tomography, allows for the healthcare professional to alter the size of the AM graft specific to the defect [75].
Caporossi et al. report that in their experience, AM plugs are more precisely trimmed when using cutaneous punch. It is important to use an accurate size plug to achieve the best result. If the plug is smaller than the macular hole diameter, it will not develop the macular hole closure. Larger plugs may crinkle and stop the healing process.
The AM plug is implanted into the eye following the vitrectomy.
A 23-gauge trocar can be used if the plug size is smaller than 3 mm. However, if it is larger than 3 mm, a 20-gauge sclerotomy is indicated. In other to reduce the plug corrugation, a DSAEK- like technique has been described by Caporossi et al. This method uses a plastic support that holds the plug at the entrance of the trocar where it can be grabbed with a vitreoretinal forceps [68].
The AM plug is inserted under the neuroretinal margins of the hole [76] with the chorion layer facing the Retinal Pigment Epithelium (RPE) [68].
Garcin et al. in 2021 [69] noted how during a follow-up of 1-year that 10 eyes of 10 patients had shown to have successfully closed macular holes, which were previously refractory to the standard of care. Additional to this, Caporossi et al. in 2020 [77] studied the treatment of 16 eyes of 16 patients with high myopic macular holes of an axial length >30 mm. All patients were treated with an AM plug after undergoing a pars plana vitrectomy. Optical coherence tomography showed that 93.75% (15/16) of patients healed after two weeks, with the following patient having complete healing after a repeat application of the AM plug. The mean best correct visual acuity improved from 20/200 to 20/100 at the 6-month follow-up period. No adverse events were experienced during the treatment period [77]. Similar results have been noted in multiple studies, that showed an improvement in best correct visual acuity and complete healing of the macular hole at the 6-month period.
Caporossi et al. in 2021 [78] published a prospective, comparative study of 20 eyes of 20 patients all diagnosed with macular holes, which were failing to close. All macular holes were treated with an AM plug, with 10 eyes receiving transplantation with 20% sulphur hexafluoride tamponade and 10 eyes receiving transplantation with an air tamponade. Results showed that both groups had an improvement in their BCVA, and all macular holes closed at the 12-month follow-up appointment. However, this case reported that the use of air provided similar outcomes to the use of gas, an innovative technique.
The preliminary data regarding the use of human AM plugs to drive the healing of macular holes, which are recurrent or refractory to the standard of care is positive. Highlighting good healing rates within this group of patients. However, much of the data is only from select research groups and therefore, more expansive and comparative, randomised data is required to provide a complete conclusion. The potential to use air tamponade rather than gas tamponade presents another practice changing technique, which could benefit this group of patients.
Retinal detachment
Whilst conducting research on macular hole closure, Rizzo et al. in 2019 [71] noted the use of AM transplant in patients with retinal breaks. Within the case series of 14 eyes of 14 patients, with 6 patients had retinal detachment (1 rhegmatogenous retinal detachment and 5 retinal detachment recurrences). All patients underwent transconjunctival pars plana vitrectomy with an AM plug being placed under the retinal tear. The BCVA for the cohort was \(2.33 \pm 0.51\) logMAR pre-operatively and improved to \(1.2 \pm 0.62\) logMAR post-operatively at the 3-month follow-up. No adverse events were experienced for any patients. The retina was shown to adhere over the AM plug in the retinal break site at 1-week post-surgery when using optical coherence tomography analysis [71].
Similar to Rizzo et al. in 2019 study multiple papers have supported the use of AM plugs in conjunction with vitrectomy for the treatment of retinal detachment [70, 79, 80]. Abouhussein et al. in 2020 [79] reported 14 eyes of 14 patients all diagnosed with rhegmatogenous retinal detachment co-existing with a macular hole. All the patients were treated with a human AM plug and had their condition improved from a BCVA of \(1.87 \pm 0.31\) logMAR pre-operatively to \(0.67 \pm 0.17\) logMAR post-operatively at the 6-month follow-up [79]. All the patients noted complete retinal attachment and macular hole closure at the 6-month follow-up appointment. This shows that all patients were effectively treated.
Innovation within this area is extremely new and upcoming and further research of larger patient numbers and randomised data is required to truly evaluate the benefit of AM transplantation in these conditions. However, it presents the growing scope regarding AM use and its capacity to be used in various ophthalmic modalities.
Optic disc pit associated macular detachment
Optic disc pit may cause serous retinal detachment. The application of AM plugs has been a promising ally in this sight threatening condition. An AM plug placed inside the pit helps to improve the re-absorption of the intraretinal fluid. Enhancement of vision has been described at the 6th month after the procedure. This is a faster result when compared with scleral autograft procedures, that has been reported to achieve improvement approximately 1 year later [68].
Age related macular degeneration (AMD)
AM has been studied as a possible treatment for Geographic macula atrophy seen in late AMD patients. Caporossi et al. describe insertion of AM sheet in the macular area in eyes with AMD and macula atrophy. The implant is positioned with the chorion layer facing the RPE, and is performed after a previous surgical provoked retinal detachment. Visual improvement has been described from 20/2000 to 20/320, \(p = 0.0084\).
Risks of amniotic membrane use
During manufacture, precautions are taken during the donor selection and testing stages to protect any transplantation recipients, there is a minimal risk regarding the transplantation of human allogenic tissue as the risk of transmissible disease cannot be completely removed. AM is traditionally harvested by elective caesarean section to minimise the potential for transmission of disease or infectious agents during the delivery of the placental tissues [4]. All donors are tested for a range of transmissible diseases, such as HIV, Hepatitis, HTLV and more dependent on the country of collection and manufacturing body [13]. Processing of the AM can also be country dependent and a 6 month quarantine period is sometimes employed to reduce the risk of infection. After 6 months HIV tests are repeated to cover the immunological window period [13].
However, the risk of contamination cannot be completely removed, due to the low risk of the presence of infective agents, such as Variant Creutzfeldt-Jakob Disease (vCJD) and other emerging virus’, prions, or pathogens. Currently, there is no validated method for testing CJD infectivity of tissue donors that is routinely available for use [81].
Conclusion
AM transplantation is a popular treatment methodology in ophthalmic care due to its immunosuppressive, anti-fibrotic and wound healing properties that are driven by the tissues potential to provide an environment or substrate for healing, dependent on the application method. Traditionally, AM transplantation has showed to be most utilised in corneal specialities, however, further research and development has highlighted its beneficial use as an adjunctive treatment in Glaucoma surgeries. However, the method of application of amniotic membrane in trabeculetomy is yet to be standardised.
For VR conditions, the data is only just emerging and although there is the lack a fully randomised clinical trials, it presents and exciting and innovative area of research and highlights the interest and beneficial perception of AM in ocular conditions of various specialities and aetiologies. AM transplantation has a large scope to be useful for long-term patient outcomes in conditions outside of corneal indications. Data is consistently emerging in these markets to provide well-rounded understanding of its benefits.
References
Röck T, Bartz-Schmidt K, Landenberger J, Bramkamp M, Röck D (2018) Amniotic membrane transplantation in reconstructive and regenerative ophthalmology. Ann Transplant 23:160–165
Shen T-Y et al. (2020) Effectiveness and safety of trabeculectomy along with amniotic membrane transplantation on glaucoma: a systematic review. J Ophthalmol 3949735-3949735
Sheha H, Anand A, Tello C (2011) Use of amniotic membrane graft in glaucoma shunt surgery. Investig Ophthalmol Vis Sci 52(14):2636–2636
Walkden A (2020) Amniotic membrane transplantation in ophthalmology: an upyeard perspective. Clin Ophthalmol 14:2057–2072
Malhotra C, Jain A (2014) Human amniotic membrane transplantation: different modalities of its use in ophthalmology. World J Transplant 4(2):111–121
McDonald MB et al (2018) Treatment outcomes in the dry eye amniotic membrane (dream) study. Clin Ophthalmol Auckland NZ 12:677
Parmar DP, Bhole PK, Patel PN, Jadeja JN (2021) Amniotic membrane transplant in acute ocular surface burns in western India: a tertiary eye care center study. Indian J Ophthalmol 69(1):58
Murri MS et al (2018) Amniotic membrane extract and eye drops: a review of literature and clinical application. Clin Ophthalmol Auckland NZ 12:1105
Rao T, Chandrasekharam V (1981) Use of dry human and bovine amnion as a biological dressing. Arch Surg 116(7):891–896
Jirsova K, Jones G (2017) Amniotic membrane in ophthalmology: properties, preparation, storage and indications for grafting-a review. Cell Tissue Bank 18(2):193–204
Lacorzana J (2020) Amniotic membrane, clinical applications and tissue engineering. Review of its ophthalmic use. Arch Soc Esp Oftalmol 95(1):15–23
Sangwan V, Burman S, Tejwani S, Mahesh S, Murthy R (2007) Amniotic membrane transplantation: a review of current indications in the management of ophthalmic disorders. Indian J Ophthalmol 55(4)
Dua H, Gomes J, King A, Maharajan V (2004) The amniotic membrane in ophthalmology. Surv Ophthalmol 49(1):51–77
Kim J, Tseng S (1995) Transplantation of preserved human amniotic membrane for surface reconstruction in severely damaged rabbit corneas. Cornea 14(5):473–84
Allen C et al (2013) Augmented dried versus cryopreserved amniotic membrane as an ocular surface dressing. PLoS One 8(10):78441
Gicquel J et al (2009) Epidermal growth factor variations in amniotic membrane used for ex vivo tissue constructs. Tissue Eng Part A 15(8):1919–1927
Hopkinson A, McIntosh R, Shanmuganathan V, Tighe P, Dua H (2006) Proteomic analysis of amniotic membrane prepared for human transplantation: characterization of proteins and clinical implications. J Proteome Res 5(9):2226–35
Hopkinson A, McIntosh R, Tighe P, James D, Dua H (2006) Amniotic membrane for ocular surface reconstruction: donor variations and the effect of handling on tgf-beta content. Invest Ophthalmol Vis Sci 47(10):4316–22
Rodríguez-Ares M et al (2009) Effects of lyophilization on human amniotic membrane. Acta Ophthalmol 87(4):396–403
Nakamura T et al (2004) Sterilized, freeze-dried amniotic membrane: a useful substrate for ocular surface reconstruction. Invest Ophthalmol Vis Sci 45(1):93–9
Versen-Höynck F, Syring C, Bachmann S, Möller D (2004) The influence of different preservation and sterilisation steps on the histological properties of amnion allografts-light and scanning electron microscopic studies. Cell Tissue Bank 5(1):45–56
Riau A, Beuerman R, Lim L, Mehta J (2010) Preservation, sterilization and de-epithelialization of human amniotic membrane for use in ocular surface reconstruction. Biomaterials 31(2):216–25
Wolkers W, Tablin F, Crowe J (2002) From anhydrobiosis to freeze-drying of eukaryotic cells. Comp Biochem Physiol A Mol Integr Physiol 131(3):535–43
Wehmeyer J, Natesan S, Christy R (2015) Development of a sterile amniotic membrane tissue graft using supercritical carbon dioxide. Tissue Eng Part C Methods 21(7):649–59
Marsit N et al (2019) Validation and assessment of an antibiotic-based, aseptic decontamination manufacturing protocol for therapeutic, vacuum-dried human amniotic membrane. Sci Rep 9(1):12854–12854
Ma K, Thanos A, Chodosh J, Shah A, Mantagos I (2016) A novel technique for amniotic membrane transplantation in patients with acute stevens-johnson syndrome. Ocul Surf 14(1):31–6
Shanbhag S, Hall L, Chodosh J, Saeed H (2020) Long-term outcomes of amniotic membrane treatment in acute stevens-johnson syndrome/toxic epidermal necrolysis. Ocul Surf 18(3):517–522
Maqsood S et al (2021) Management of persistent corneal epithelial defects with human amniotic membrane-derived dry matrix. Clin Ophthalmol 15:2231–2238
Schuerch K, Baeriswyl A, Frueh B, Tappeiner C (2020) Efficacy of amniotic membrane transplantation for the treatment of corneal ulcers. Cornea 39(4):479–483
Meller D, Pauklin M, Thomasen H, Westekemper H, Steuhl K-P (2011) Amniotic membrane transplantation in the human eye. Dtsch Arztebl Int 108(14):243–248
Baradaran-Rafii A, Aghayan H, Arjmand B, Mohammad-Ali J (2008) Amniotic membrane transplantation. J Ophthalmic Vis Res 2
Eliezer R et al. (2006) Use of amniotic membrane in trabeculectomy for the treatment of glaucoma: a pilot study, vol. 69 , Arq Bras Oftalmol
Mcgaughy A, Gupta KP (2015) In-office use of amniotic membrane. Ophthalmic Pearls Cornea. https://www.aao.org/eyenet/article/in-office-use-of-amniotic-membrane
Adinolfi M et al (1982) Expression of hla antigens, beta 2-microglobulin and enzymes by human amniotic epithelial cells. Nature 295(5847):325–7
Rinastiti M, Harijadi SLA, Sosroseno W (2006) Histological evaluation of rabbit gingival wound healing transplanted with human amniotic membrane. Int J Oral Maxillofac Surg 35(3):247–51
Niknejad H et al (2008) Properties of the amniotic membrane for potential use in tissue engineering. Eur Cell Mater 15:88–99
Meller D, Pires R, Tseng S (2002) Ex vivo preservation and expansion of human limbal epithelial stem cells on amniotic membrane cultures. Br J Ophthalmol 86(4):463–71
Shimmura S, Shimazaki J, Ohashi Y, Tsubota K (2001) Antiinflammatory effects of amniotic membrane transplantation in ocular surface disorders. Cornea 20(4):408–13
He H et al (2017) Inhibition of proliferation and epithelial mesenchymal transition in retinal pigment epithelial cells by heavy chain-hyaluronan/pentraxin 3. Sci Rep 7(1):43736
Shay E, He H, Sakurai S, Tseng S (2011) Inhibition of angiogenesis by hc.ha, a complex of hyaluronan and the heavy chain of inter-\(\alpha\)-inhibitor, purified from human amniotic membrane. Invest Ophthalmol Vis Sci 52(5):2669–78
Solomon A et al (2001) Suppression of interleukin 1alpha and interleukin 1beta in human limbal epithelial cells cultured on the amniotic membrane stromal matrix. Br J Ophthalmol 85(4):444–9
Fukuda K, Chikama T, Nakamura M, Nishida T (1999) Differential distribution of subchains of the basement membrane components type iv collagen and laminin among the amniotic membrane, cornea, and conjunctiva. Cornea 18(1):73–9
Rahman I, Said D, Maharajan V, Dua H (2009) Amniotic membrane in ophthalmology: indications and limitations. Eye 23(10):1954–1961
Yadava U et al (2017) Simultaneous use of amniotic membrane and mitomycin c in trabeculectomy for primary glaucoma. Indian J Ophthalmol 65(11):1151–1155
Stavrakas P et al (2012) The use of amniotic membrane in trabeculectomy for the treatment of primary open-angle glaucoma: a prospective study. Clin Ophthalmol 6:205–212
Sheha H, Tello C, Al-Aswad LA, Sayed MS, Lee RK (2019) Outcomes of the shunt tube exposure prevention study. Ophthalmol Glaucoma 2(6):392–401. https://doi.org/10.1016/j.ogla.2019.08.003
Fujishima H, Shimazaki J, Shinozaki N, Tsubota K (1998) Trabeculectomy with the use of amniotic membrane for uncontrollable glaucoma. Ophthalmic Surg Lasers 29(5):428–31
Sheha H, Kheirkhah A, Taha H (2008) Amniotic membrane transplantation in trabeculectomy with mitomycin c for refractory glaucoma. J Glaucoma 17(4):303–7
Ji Q-S et al (2013) Comparison of trabeculectomy and trabeculectomy with amniotic membrane transplantation in the same patient with bilateral glaucoma. Int J Ophthalmol 6(4):448–451
Mahdy R, Nada W, Almasalamy S, Anany H, Almasary A (2010) A freeze-dried (lyophilized) amniotic membrane transplantation with mitomycin c and trabeculectomy for pediatric glaucoma. Cutan Ocul Toxicol 29(3):164–70
Wang X, Khan R, Coleman A (2015) Device-modified trabeculectomy for glaucoma. Cochrane Database Syst Rev 12(12):010472–010472
Roque J et al (2021) Use of amniotic membrane in MMC-augmented trabeculectomy: a retrospective comparative study. Clin Ophthalmol 15:4527–4533. https://doi.org/10.2147/opth.s342593
Yazdani S, Mahboobipour H, Pakravan M, Doozandeh A, Ghahari E (2016) Adjunctive mitomycin c or amniotic membrane transplantation for ahmed glaucoma valve implantation: a randomized clinical trial. J Glaucoma 25(5):415–21
Ophthalmologists TRC (2020) Mitomycin shortage resolution. https://www.rcophth.ac.uk/news-views/mitomycin-shortage-resolution/
Obeda Kailani DL, Quijano C (1999) How will mitomycin c shortages affect glaucoma surgery?. https://theophthalmologist.com/subspecialties/drug-drought
Nagai-Kusuhara A, Nakamura M, Fujioka M, Negi A (2008) Long-term results of amniotic membrane transplantation-assisted bleb revision for leaking blebs. Graefes Arch Clin Exp Ophthalmol 246(4):567–71
Bochmann F, Azuara-Blanco A (2012) Interventions for late trabeculectomy bleb leak. Cochrane Database Syst Rev. 9:Cd006769
Budenz D, Barton K, Tseng S (2000) Amniotic membrane transplantation for repair of leaking glaucoma filtering blebs. Am J Ophthalmol 130(5):580–8
Rauscher F, Barton K, Budenz D, Feuer W, Tseng S (2007) Long-term outcomes of amniotic membrane transplantation for repair of leaking glaucoma filtering blebs. Am J Ophthalmol 143(6):1052–4
Sethi P, Patel R, Goldhardt R, Ayyala R (2016) Conjunctival advancement with subconjunctival amniotic membrane draping technique for leaking cystic blebs. J Glaucoma 25(2):188–92
Tanito M, Sano I, Ikeda Y, Fujihara E (2018) Patch grafting using an ologen collagen matrix to manage tubal exposure in glaucoma tube shunt surgery. Case Rep Ophthalmol 9(1):9–16. https://doi.org/10.1159/000485549
Wigton E et al (2014) Outcomes of shunt tube coverage with glycerol preserved cornea versus pericardium. J Glaucoma 23(4):258–261. https://doi.org/10.1097/ijg.0b013e31826a96e8
Ainsworth G, Rotchford A, Dua H, King A (2006) A novel use of amniotic membrane in the management of tube exposure following glaucoma tube shunt surgery. Br J Ophthalmol 90(4):417–419
Amini H, Kiarudi M, Moghimi S, Fakhraie G, Amini N (2010) Ahmed glaucoma valve with adjunctive amniotic membrane for refractory glaucoma. J Ophthalmic Vis Res 5(3):158–161
Ulas B (2021) Novel use of double-layer amniotic membrane technique in tube erosion of pediatric case. Beyoglu Eye J. https://doi.org/10.14744/bej.2021.05900
Anand A et al (2011) Use of amniotic membrane graft in glaucoma shunt surgery. Ophthalmic Surg Lasers Imaging Retina 42(3):184–189. https://doi.org/10.3928/15428877-20110426-01
Ainsworth G (2006) A novel use of amniotic membrane in the management of tube exposure following glaucoma tube shunt surgery. Br J Ophthalmol 90(4):417–419. https://doi.org/10.1136/bjo.2005.084905
Caporossi T et al (2020) Applications of the amniotic membrane in vitreoretinal surgery. J Clin Med 9(8):2675. https://doi.org/10.3390/jcm9082675
Garcin T, Gain P, Thuret G (2021) Epiretinal large disc of blue-stained lyophilized amniotic membrane to treat complex macular holes: a 1-year follow-up. Acta Ophthalmol
Caporossi T, Tartaro R, De Angelis L, Pacini B, Rizzo S (2019) A human amniotic membrane plug to repair retinal detachment associated with large macular tear. Acta Ophthalmol 97(8):821–823
Rizzo S et al (2019) A human amniotic membrane plug to promote retinal breaks repair and recurrent macular hole closure. Retina 39(Suppl 1):95–103
Capeáns C et al (2003) Amniotic membrane as support for human retinal pigment epithelium (rpe) cell growth. Acta Ophthalmol Scand 81(3):271–7
Diniz B et al (2013) Subretinal implantation of retinal pigment epithelial cells derived from human embryonic stem cells: improved survival when implanted as a monolayer. Invest Ophthalmol Vis Sci 54(7):5087–96
Ohno-Matsui K et al (2005) The effects of amniotic membrane on retinal pigment epithelial cell differentiation. Mol Vis 11:1–10
Caporossi T et al (2020) Human amniotic membrane plug to promote failed macular hole closure. Sci Rep 10(1):18264
Ventre L, Marolo P, Reibaldi M (2020) A human amniotic membrane plug to treat persistent macular hole. Case Rep Ophthalmol 11(2):442–447
Caporossi T et al (2020) Human amniotic membrane to close recurrent, high myopic macular holes in pathologic myopia with axial lenght of \(\ge\)30 mm. Retina 40(10):1946–1954
Caporossi T et al (2021) Sulfur hexafluoride endotamponade versus air endotamponade: a prospective comparative study. Retina 41(4):735–743
Abouhussein M, Elbaha S, Aboushousha M (2020) Human amniotic membrane plug for macular holes coexisting with rhegmatogenous retinal detachment. Clin Ophthalmol 14:2411–2416
Caporossi T, De Angelis L, Pacini B, Rizzo S (2020) Amniotic membrane for retinal detachment due to paravascular retinal breaks over patchy chorioretinal atrophy in pathologic myopia. Eur J Ophthalmol 30(2):392–395
Armitage W, Tullo A, Ironside J (2009) Risk of creutzfeldt-jakob disease transmission by ocular surgery and tissue transplantation. Eye 23(10)
Acknowledgements
Acknowledgement to Ms Tonicha Spencer for helping with literature review.
Funding
The authors would like to declare that NuVision Biotherapies Ltd. has kindly funded the publication fees of this review paper.
Author information
Authors and Affiliations
Contributions
All three authors contributed equally to the paper. All three authors have written sections in this paper and contributed to the literature review. The Latex manuscript was prepared by VN. All authors reviewed the paper.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sharma, R., Nappi, V. & Empeslidis, T. The developments in amniotic membrane transplantation in glaucoma and vitreoretinal procedures. Int Ophthalmol 43, 1771–1783 (2023). https://doi.org/10.1007/s10792-022-02570-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02570-5