Abstract
Purpose
To explore visual dysfunction in Graves’ orbitopathy (GO) objectively by analyzing chromatic visual evoked potentials (cVEP) and evaluate its diagnostic efficiency for dysthyroid optic neuropathy (DON).
Methods
In this cross-sectional study, we analyzed pattern-reversal VEP (pVEP), red–green (R–G) and blue–yellow (B–Y) cVEP in 93 subjects (21 with DON, Group A, 30 with GO, Group B, and 42 healthy controls, Group C) at Wuhan Union Hospital, China.
Results
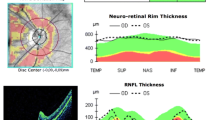
Compared with Group C, the amplitudes of B-Y cVEP were significantly lower in Group B, whereas all amplitudes of cVEP, latencies and amplitudes of pVEP in Group A were significantly impaired. In addition, the pVEP latency at 60 arcmin (60'), pVEP amplitudes and R–G cVEP amplitudes were significantly different between Group A and B. Moreover, 60’cVEP R–G negative–positive (N–P) amplitude was correlated with crowding index (P = 0.001), the average thickness of ganglion cell layer and inner plexiform layer (P = 0.004). Furthermore, combination of 60’cVEP R–G amplitude and 60’pVEP P100 latency had better diagnostic efficiency than each single parameter, with optimal cut-off values of 14.20 μV and 110.65 ms, respectively.
Conclusion
GO may induce electrophysiological changes. The presence of B–Y cVEP anomalies in moderate to severe GO patients may be an early sign of preclinical DON. A decline in 60’cVEP R–G amplitude is associated with apical crowding and thinner inner intra-retinal layers. The combination of 60’cVEP R–G N–P amplitude and 60’pVEP latency can be a useful diagnostic index for DON.




Similar content being viewed by others
Data availability
The datasets used in the current study are available from the corresponding authors on reasonable request.
Code availability
Not applicable.
References
McKeag D, Lane C, Lazarus JH et al (2007) Clinical features of dysthyroid optic neuropathy: a European Group on Graves’ Orbitopathy (EUGOGO) survey. Br J Ophthalmol 91:455–458. https://doi.org/10.1136/bjo.2006.094607
Dolman PJ (2012) Evaluating Graves’ orbitopathy. Best Pract Res Clin Endocrinol Metab 26:229–248. https://doi.org/10.1016/j.beem.2011.11.007
Neigel JM, Rootman J, Belkin RI, Nugent RA, Drance SM, Beattie CW, Spinelli JA (1988) Dysthyroid optic neuropathy. Crowd Orbital Apex Syndr Ophthalmol 95:1515–1521
Wakelkamp I, Baldeschi L, Saeed P, Mourits MP, Prummel MF, Wiersinga WM (2005) Surgical or medical decompression as a first-line treatment of optic neuropathy in Graves’ ophthalmopathy? A randomized controlled trial. Clin Endocrinol 63:323–328. https://doi.org/10.1111/j.1365-2265.2005.02345.x
Liao SL, Chang TC, Lin LLK (2006) Transcaruncular orbital decompression: an alternate procedure for graves ophthalmopathy with compressive optic neuropathy. Am J Ophthalmol 141:810–818. https://doi.org/10.1016/j.ajo.2005.12.010
Garip-Kuebler A, Halfter K, Reznicek L, Klingenstein A, Priglinger S, Hintschich CR (2020) Subclinical dysthyroid optic neuropathy: tritan deficiency as an early sign of dysthyroid optic neuropathy. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2020-316433
Cole BL (2007) Assessment of inherited colour vision defects in clinical practice. Clin Exp Optom 90:157–175. https://doi.org/10.1111/j.1444-0938.2007.00135.x
Farnsworth D (1957) The Farnsworth-Munsell 100 Hue Test Manual (revised ed.). Baltimore: Munsell Color Company
Francois JVG (1961) On acquired deficiency of colour vision, with special reference to its detection and classification by means of the tests of Farnsworth. Vis Res I:201–219
Bassi CJ, Galanis JC, Hoffman J (1993) Comparison of the Farnsworth-Munsell 100-Hue, the Farnsworth D-15, and the L’Anthony D-15 desaturated color tests. Arch Ophthalmol 111:639–641. https://doi.org/10.1001/archopht.1993.01090050073032
Rabin J, Switkes E, Crognale M, Schneck ME, Adams AJ (1994) Visual evoked potentials in three-dimensional color space: Correlates of spatio-chromatic processing. Vis Res 34:2657–2671. https://doi.org/10.1016/0042-6989(94)90222-4
Russell MH, Murray IJ, Metcalfe RA, Kulikowski JJ (1991) The visual defect in multiple sclerosis and optic neuritis. A combined psychophysical and electrophysiological investigation. Brain A J Neurol 114(Pt 6):2419–2435. https://doi.org/10.1093/brain/114.6.2419
Crognale MA, Switkes E, Rabin J, Schneck ME, Haegerstrom-Portnoy G, Adams AJ (1993) Application of the spatiochromatic visual evoked potential to detection of congenital and acquired color-vision deficiencies. J Opt Soc Am A 10:1818–1825. https://doi.org/10.1364/josaa.10.001818
Fuest M, Kieckhoefel J, Mazinani B, Kuerten D, Koutsonas A, Koch E, Walter P, Plange N (2015) Blue-yellow and standard pattern visual evoked potentials in phakic and pseudophakic glaucoma patients and controls. Graefes Arch Clin Exp Ophthalmol 253:2255–2261. https://doi.org/10.1007/s00417-015-3152-6
Pompe MT, Kranjc BS, Brecelj J (2010) Chromatic VEP in children with congenital colour vision deficiency. Ophthalmic Physiol Opt 30:693–698. https://doi.org/10.1111/j.1475-1313.2010.00739.x
Pompe MT, Perovsek D, Sustar M (2020) Chromatic visual evoked potentials indicate early dysfunction of color processing in young patients with demyelinating disease. Doc Ophthalmol 141:157–168. https://doi.org/10.1007/s10633-020-09761-4
Morrone MC, Fiorentini A, Burr DC (1996) Development of the temporal properties of visual evoked potentials to luminance and colour contrast in infants. Vis Res 36:3141–3155. https://doi.org/10.1016/0042-6989(96)00050-8
Crognale MA (2002) Development, maturation, and aging of chromatic visual pathways: VEP results. J Vis. https://doi.org/10.1167/2.6.2
Gregori B, Galie E, Pro S, Clementi A, Accornero N (2006) Luminance and chromatic visual evoked potentials in type I and type II diabetes: relationships with peripheral neuropathy. Neurol Sci 27:323–327. https://doi.org/10.1007/s10072-006-0704-x
Wu F, Yang Y, Li H, Odom JV (2011) Relationship of chromatic visual-evoked potentials and the changes of foveal photoreceptor layer in central serous chorioretinopathy patients. Ophthalmic Physiol Opt 31:381–388. https://doi.org/10.1111/j.1475-1313.2011.00839.x
Korth M, Nguyen NX, Juenemann A, Martus P, Jonas JB (1994) VEP test of the blue-sensitive pathway in glaucoma. Invest Ophthalmol Vis Sci 35:2599–2610
Hendry SHC, Calkins DJ (1998) Neuronal chemistry and functional organization in the primate visual system. Trends Neurosci 21:344–349. https://doi.org/10.1016/s0166-2236(98)01245-4
Bartley GB, Gorman CA (1995) Diagnostic criteria for Graves’ ophthalmopathy. Am J Ophthalmol 119:792–795. https://doi.org/10.1016/s0002-9394(14)72787-4
Goncalves ACP, Silva LN, Gebrim EMMS, Monteiro MLR (2012) Quantification of orbital apex crowding for screening of dysthyroid optic neuropathy using multidetector CT. Am J Neuroradiol 33:1602–1607. https://doi.org/10.3174/ajnr.A3029
Melamud A, Hagstrom S, Traboulsi E (2004) Color vision testing. Ophthalmic Genet 25:159–187. https://doi.org/10.1080/13816810490498341
Odom JV, Bach M, Brigell M, Holder GE, McCulloch DL, Mizota A, Tormene AP, Int Soc Clinical E (2016) ISCEV standard for clinical visual evoked potentials: (2016 update). Doc Ophthalmol 133:1–9. https://doi.org/10.1007/s10633-016-9553-y
Porciatti V, Sartucci F (1999) Normative data for onset VEPs to red-green and blue-yellow chromatic contrast. Clin Neurophysiol 110:772–781. https://doi.org/10.1016/s1388-2457(99)00007-3
Johnson CA, Adams AJ, Casson EJ, Brandt JD (1993) Blue-on-yellow perimetry can predict the development of glaucomatous visual field loss. Arch Ophthalmol 111:645–650. https://doi.org/10.1001/archopht.1993.01090050079034
Mollon JD (1982) What is odd about the short-wavelength mechanism and why is it disproportionately vulnerable to acquired damage. Doc Ophthalmol Proc Series 33:145–149
Hood DC, Greenstein VC (1988) Blue (S) cone pathway vulnerability: a test of a fragile receptor hypothesis. Appl Opt 27:1025–1029. https://doi.org/10.1364/ao.27.001025
Adams AJ (1982) Chromatic and luminosity processing in retinal disease. Am J Optom Physiol Opt 59:954–960
Barrett L, Glatt HJ, Burde RM, Gado MH (1988) Optic nerve dysfunction in thyroid eye disease: CT. Radiology 167:503–507. https://doi.org/10.1148/radiology.167.2.3357962
Nugent RA, Belkin RI, Neigel JM, Rootman J, Robertson WD, Spinelli J, Graeb DA (1990) Graves orbitopathy: correlation of CT and clinical findings. Radiology 177:675–682. https://doi.org/10.1148/radiology.177.3.2243967
Hu WD, Annunziata CC, Chokthaweesak W, Korn BS, Levi L, Granet DB, Kikkawa DO (2010) Radiographic analysis of extraocular muscle volumetric changes in thyroid-related orbitopathy following orbital decompression. Ophthalmic Plast Reconstr Surg 26:1–6. https://doi.org/10.1097/IOP.0b013e3181b80fae
Wu YF, Tu YH, Wu CM, Bao LL, Wang JH, Lu F, Shen MX, Chen Q (2020) Reduced macular inner retinal thickness and microvascular density in the early stage of patients with dysthyroid optic neuropathy. Eye Vis 7:12. https://doi.org/10.1186/s40662-020-00180-9
Park K-A, Kim Y-D, Woo KI, Kee C, Han JC (2016) Optical coherence tomography measurements in compressive optic neuropathy associated with dysthyroid orbitopathy. Graefes Arch Clin Exp Ophthalmol 254:1617–1624. https://doi.org/10.1007/s00417-016-3335-9
Acknowledgements
We thank Prof. Feng Gao (Department of Endocrinology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China), for the guidance in the diagnosis of the patients’ thyroid diseases.
Funding
This work was supported by the National Science Foundation of China (No. 81900912).
Author information
Authors and Affiliations
Contributions
Design of the study (YQ Y, B S, X W, F J); data collection (YQ Y, B S, S C, Y L, R Z, YY Y, J C, X P, X W); statistical analysis (YQ Y, B S); drafting of the manuscript (YQ Y, B S, X W, F J); funding acquisition (X W); supervision (X W, F J). All authors read and approved the manuscript to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare that are relevant to content to this article.
Ethical approval
The present study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Research Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology (approving number: 2021–0246).
Consent for participate
We have obtained consent to publish from the patients to report the data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, Y., Shi, B., Cheng, S. et al. Chromatic visual evoked potentials identify optic nerve dysfunction in patients with Graves’ orbitopathy. Int Ophthalmol 42, 3713–3724 (2022). https://doi.org/10.1007/s10792-022-02369-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-022-02369-4