Abstract
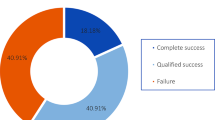
To analyze the intraocular pressure reduction, number of anti-glaucoma medications needed, and post-operative complications of trans-scleral diode laser cyclophotocoagulation (DCPC) in patients with high-risk penetrating keratoplasty (PKP) and secondary refractory glaucoma. Prospective interventional, longitudinal, non-comparative series of cases, including 16 eyes of 15 patient’s post-PKP on maximal anti-glaucoma medical therapy with intraocular pressures above 22 mmHg. All patients received 18 shots, 360° peri-limbal (avoiding the long posterior ciliary nerves and arteries at 3 and 9 o’clock positions) of trans-scleral DCPC (2000 mW, time: 2.0 s/shot). There was a 55.5 % reduction (total of 14.0 mmHg) of the mean pre-operative IOP (31.5 mmHg) after the first diode laser application (p = 0.0020). Re-treatment was required in 31.2 % of eyes over a mean period of 10.7 months. In these five eyes, the mean pre-operative IOP was 40.4 mmHg, which decreased to 15.0 mmHg post-therapy, and a mean IOP reduction of 25.4 mmHg (p = 0.0218). There was a 51.0 % reduction in the mean number of medications used after the first, and a 57.1 % reduction after a second laser application. The incidence of failure (IOP ≥ 22 mmHg or need of additional medical therapy) from initial intervention to loss of follow-up was 1.3 % per person-month. DCPC effectively reduces the intraocular pressure and the number of anti-glaucoma medications with few complications in patients after high-risk PKP and secondary glaucoma. Only, one-third of the eyes needed a second intervention to control the intraocular pressure. Post-DCPC complications were limited to phthisis bulbi and endothelial dysfunction, one eye each. Please check and confirm the author names and initials are correct. Also, kindly confirm the details in the metadata are correct.

Similar content being viewed by others
References
Ayyala RS (2000) Penetrating keratoplasty and glaucoma. Surv Ophthalmol 45:91–105
Wilson SE, Kaufman HE (1990) Graft failure after penetrating keratoplasty. Surv Ophthalmol 34:325–356
Wood TO, West C, Kaufman HE (1972) Control of intraocular pressure in penetrating keratoplasty. Am J Ophthalmol 74:724–728
Al-Mohaimeed M, Al-Shahwan S, Al-Torbak A, Wagoner MD (2007) Escalation of glaucoma therapy after penetrating keratoplasty. Ophthalmology 114:2281–2286
Dada T, Aggarwal A, Minudath KB, Vanathi M, Choudhary S, Gupta V et al (2008) Post-penetrating keratoplasty glaucoma. Indian J Ophthalmol 56:269–277
Sihota R, Sharma N, Panda A, Aggarwal HC, Singh R (1998) Post-penetrating keratoplasty glaucoma: risk factors, management and visual outcome. Aust N Z J Ophthalmol 26:305–309
Karesh JW, Nirankari VS (1983) Factors associated with glaucoma after penetrating keratoplasty. Am J Ophthalmol 96:160–164
Yildirim N, Gursoy H, Sahin A, Ozer A, Colak E (2011) Glaucoma after penetrating keratoplasty: incidence, risk factors, and management. J Ophthalmol 2011:1–6
Oruçoglu F, Blumenthal EZ, Frucht-Pery J, Solomon A (2014) Risk factors and incidence of ocular hypertension after penetrating keratoplasty. J Glaucoma 23:599–605
Leung EW, Medeiros FA, Weinreb RN (2008) Prevalence of ocular surface disease in glaucoma patients. J Glaucoma 17:350–355
Goldberg I, RD F, Aihara M, Lerner FS, Barabino S, Baudouin C, Fetchner RD, Lerner SF, Pflugfelder SC (2010) Ocular surface disease in patients with glaucoma. ALCON, Inc. Jul 21, pp 1–20
García-Fejioo J, Sampaolesi JR (2012) A multicenter evaluation of ocular surface disease prevalence in patients with glaucoma. Clin Ophthalmol 6:441–446
Horsley MB, Kahook MY (2009) Effects of prostaglandin analog therapy on the ocular surface of glaucoma patients. Clin Ophthalmol 3:291–295
O’Brien TP, Springs CL (2008) Addressing ocular surface disease in the glaucoma population. Ophthalmology Times, 1st edn, July 1; 33,13, ProQuest, pp 1–12
Skalicky SE, Goldberg I, McCluskey P (2012) Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol 153:1–9
Gaasterland DE, Pollack IP (1992) Initial experience with a new method of laser transscleral cyclophotocoagulation for ciliary ablation in severe glaucoma. Trans Am Ophthalmol Soc 90:225–226
Vernon SAS, Koppens JMJ, Menon GJG, Negi AKA (2006) Diode laser cycloablation in adult glaucoma: long-term results of a standard protocol and review of current literature. Clin Exp Ophthalmol 34:411–420
Iliev ME, Gerber S (2007) Long-term outcome of trans-scleral diode laser cyclophotocoagulation in refractory glaucoma. Br J Ophthalmol 91:1631–1635
Hennis HL, Stewart WC (1992) Semiconductor diode laser transscleral cyclophotocoagulation in patients with glaucoma. Am J Ophthalmol 113:81–85
Shah P, Lee GA, Kirwan JK, Bunce C, Bloom PA, Ficker LA, Khaw PT (2001) Cyclodiode photocoagulation for refractory glaucoma after penetrating keratoplasty. Ophthalmology 108:1986–1991
Ataullah S, Biswas S, Artes PH, O’Donoghue E, Ridgway AEA, Spencer AF (2002) Long term results of diode laser cycloablation in complex glaucoma using the Zeiss Visulas II system. Br J Ophthalmol 86:39–42
Tzamalis A, Pham D-T, Wirbelauer C (2011) Diode laser cyclophotocoagulation versus cyclocryotherapy in the treatment of refractory glaucoma. Eur J Ophthalmol 21:589–596
Fong AW, Lee GA, O’Rourke P, Thomas R (2011) Management of neovascular glaucoma with transscleral cyclophotocoagulation with diode laser alone versus combination transscleral cyclophotocoagulation with diode laser and intravitreal bevacizumab. Clin Exp Ophthalmol 39:318–323
Hawkins TA, Stewart WC (1993) One-year results of semiconductor transscleral cyclophotocoagulation in patients with glaucoma. Arch Ophthalmol 111:488–491
Espino-Barros-Palau A, Rodríguez-García A (2012) Trans-scleral diode laser cyclophotocoagulation in the management of diabetic neovascular glaucoma. Rev Mex Oftalmol 86:12–19
Brancato R, Leoni G, Trabucchi G, Cappellini A (1991) Histopafhology of continuous wave neodymium: yttrium aluminum garnet and diode laser contact transscleral lesions in rabbit ciliary body. Invest Ophthalmol Vis Sci 32:1586–1592
Peyman GA, Naguib KS, Gaasterland D (1990) Trans-scleral application of a semiconductor diode laser. Lasers Surg Med 10:569–575
Threlkeld AB, Johnson MH (1999) Contact transscleral diode cyclophotocoagulation for refractory glaucoma. J Glaucoma 8:3–7
Yap-Veloso MI, Simmons RB, Echelman DA, Gonzales TK, Veira WJ, Simmons RJ (1998) Intraocular pressure control after contact transscleral diode cyclophotocoagulation in eyes with intractable glaucoma. J Glaucoma 7:319–328
Leng F, Liu P, Li H, Zhang J (2011) Long-term topical antiglaucoma medications cause enhanced Tenon’s capsule fibroblast proliferation and abnormal TGF-β and MMP expressions: potential effects on glaucoma filtering surgery. Curr Eye Res 36:301–309
Iwao K, Inatani M, Ogata-Iwao M, Takihara Y, Tanihara H (2009) Restricted post-trabeculectomy bleb formation by conjunctival scarring. Graefe’s Arch Clin Exp Ophthalmol 247:1095–1101
Lim KS, Allan BD, Lloyd AW, Muir A, Khaw PT (1998) Glaucoma drainage devices; past, present, and future. Br J Ophthalmol 82:1083–1089
Malik R, Ellingham RB, Suleman H, Morgan WH (2006) Refractory glaucoma-tube or diode? Clin Exp Ophthalmol 34:771–777
Hill JC (2002) High risk corneal grafting. Br J Ophthalmol 86:945
Csoter DJ, Jessup CF, Williams KA (2015) Mechanisms of corneal allograft rejection and the development of new therapies. Cornea and external disease. Springer, New York, pp 13–23
Parihar JKS, Vats DP, Maggon R, Mathur V, Singh A, Mishra SK (2009) The efficacy of Ahmed glaucoma valve drainage devices in cases of adult refractory glaucoma in Indian eyes. Indian J Ophthalmol 57:345–350
Association WM (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Olivier MMG (2012) Current options for cyclophotocoagulation. An overview of transscleral diode photocoagulation and endocyclophotocoagulation, Glaucoma Today, Apr 10 (March/April), pp 30–34
Rumelt S (2011) Glaucoma in cases of penetrating keratoplasty, lamellar procedures and keratoprosthesis. In: Rumelt S (ed) Glaucoma basic and clinical concepts (Chap. 30). INTECH, Rijeka, pp 569–590
Gupta P, Sharma A, Ichhpujani P (2014) Post penetrating keratoplasty glaucoma—a review. Nepal J Ophthalmol 6:80–90
McDonnell PJ, Robin JB, Schanzlin DJ, Minckler D, Baerveldt G, Smith RE, Heuer D (1988) Molteno implant for control of glaucoma in eyes after penetrating keratoplasty. Ophthalmology 95:364–369
Chang SHL, Chen Y-C, Li C-Y, Wu S-C (2004) Contact diode laser transscleral cyclophotocoagulation for refractory glaucoma: comparison of two treatment protocols. Can J Ophthalmol 39:511–516
Noureddin BN, Zein W, Haddad C, Ma’luf R, Bashshur Z (2005) Diode laser transcleral cyclophotocoagulation for refractory glaucoma: a 1 year follow-up of patients treated using an aggressive protocol. Eye (London) 20:329–335
Youn J, Cox TA, Herndon LW, Allingham RR (1998) A Clinical comparison of transscleral cyclophotocoagulation with neodymium: YAG and semiconductor diode lasers. Am J Ophthalmol 126:640–647
Rotchford AP, Jayasawal R, Madhusudhan S, Ho S, King AJ, Vernon SA (2010) Transscleral diode laser cycloablation in patients with good vision. Br J Ophthalmol 94:1180–1183
Khan MT, Qazi ZA (2007) Transscleral diode laser cyclophotocoagulation for the treatment of refractory glaucoma. Pak J Ophthalmol 23:204–208
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no propriety or financial interest in any of the laser devices or materials used for this study.
Informed consent
All patients included in the study read and signed an informed consent for laser treatment previously approved by the Ethics and Research Committees of our institution in compliance with the ethical principles of the Declaration of Helsinki.
Rights and permissions
About this article
Cite this article
Rodríguez-García, A., González-González, L.A. & Carlos Alvarez-Guzmán, J. Trans-scleral diode laser cyclophotocoagulation for refractory glaucoma after high-risk penetrating keratoplasty. Int Ophthalmol 36, 373–383 (2016). https://doi.org/10.1007/s10792-015-0130-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-015-0130-2