Abstract
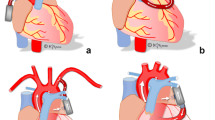
Heart failure with preserved ejection fraction (HFpEF) is a syndrome with an unfavorable prognosis, and the number of the patients continues to grow. Because there is no effective therapy established as a standard, including pharmacological treatments, a movement to develop and evaluate device-based therapies is an important emerging area in the treatment of HFpEF patients. Many devices have set their target to reduce the left atrial pressure or pulmonary capillary wedge pressure because they are strongly related to the symptoms and prognosis of HFpEF, but the methodology to achieve it varies based on the devices. In this review, we summarize and categorize these devices into the following: (1) interatrial shunt devices, (2) left ventricle expander, (3) electrical therapy, (4) left ventricular assist devices, and (5) mechanical circulatory support devices under development. Here, we describe the features and specifications of device-based therapies currently under development and those at more advanced stages of preclinical testing. Advantages and limitations of these technologies, with insights on their safety and feasibility for HFpEF patients, are described.





Similar content being viewed by others
References
Xanthopoulos A, Triposkiadis F, Starling RC (2018) Heart failure with preserved ejection fraction: classification based upon phenotype is essential for diagnosis and treatment. Trends Cardiovasc Med 28(6):392–400. https://doi.org/10.1016/j.tcm.2018.01.001
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62(16):e147-239. https://doi.org/10.1016/j.jacc.2013.05.019
Lewis EF, Lamas GA, O’Meara E, Granger CB, Dunlap ME, McKelvie RS, Probstfield JL, Young JB, Michelson EL, Halling K, Carlsson J, Olofsson B, McMurray JJ, Yusuf S, Swedberg K, Pfeffer MA (2007) Characterization of health-related quality of life in heart failure patients with preserved versus low ejection fraction in CHARM. Eur J Heart Fail 9(1):83–91. https://doi.org/10.1016/j.ejheart.2006.10.012
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37 (27):2129–2200. https://doi.org/10.1093/eurheartj/ehw128
Lam CSP, Voors AA, de Boer RA, Solomon SD, van Veldhuisen DJ (2018) Heart failure with preserved ejection fraction: from mechanisms to therapies. Eur Heart J 39(30):2780–2792. https://doi.org/10.1093/eurheartj/ehy301
Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM (2006) Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 355(3):251–259. https://doi.org/10.1056/NEJMoa052256
van Deursen VM, Urso R, Laroche C, Damman K, Dahlstrom U, Tavazzi L, Maggioni AP, Voors AA (2014) Co-morbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail 16(1):103–111. https://doi.org/10.1002/ejhf.30
De Rosa R, Piscione F, Schranz D, Citro R, Iesu S, Galasso G (2017) Transcatheter implantable devices to monitoring of elevated left atrial pressures in patients with chronic heart failure. Transl Med UniSa 17:19–21
Reddy YNV, Carter RE, Obokata M, Redfield MM, Borlaug BA (2018) A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation 138(9):861–870. https://doi.org/10.1161/circulationaha.118.034646
Issa O, Peguero JG, Podesta C, Diaz D, De La Cruz J, Pirela D, Brenes JC (2017) Left atrial size and heart failure hospitalization in patients with diastolic dysfunction and preserved ejection fraction. J Cardiovasc Echogr 27(1):1–6. https://doi.org/10.4103/2211-4122.199064
Zile MR, Gottdiener JS, Hetzel SJ, McMurray JJ, Komajda M, McKelvie R, Baicu CF, Massie BM, Carson PE (2011) Prevalence and significance of alterations in cardiac structure and function in patients with heart failure and a preserved ejection fraction. Circulation 124(23):2491–2501. https://doi.org/10.1161/circulationaha.110.011031
Reddy YNV, Obokata M, Verbrugge FH, Lin G, Borlaug BA (2020) Atrial dysfunction in patients with heart failure with preserved ejection fraction and atrial fibrillation. J Am Coll Cardiol 76(9):1051–1064. https://doi.org/10.1016/j.jacc.2020.07.009
Linssen GC, Rienstra M, Jaarsma T, Voors AA, van Gelder IC, Hillege HL, van Veldhuisen DJ (2011) Clinical and prognostic effects of atrial fibrillation in heart failure patients with reduced and preserved left ventricular ejection fraction. Eur J Heart Fail 13(10):1111–1120. https://doi.org/10.1093/eurjhf/hfr066
Beltrami M, Palazzuoli A, Padeletti L, Cerbai E, Coiro S, Emdin M, Marcucci R, Morrone D, Cameli M, Savino K, Pedrinelli R, Ambrosio G (2018) The importance of integrated left atrial evaluation: from hypertension to heart failure with preserved ejection fraction. Int J Clin Pract 72 (2). https://doi.org/10.1111/ijcp.13050
Wolsk E, Kaye D, Borlaug BA, Burkhoff D, Kitzman DW, Komtebedde J, Lam CSP, Ponikowski P, Shah SJ, Gustafsson F (2018) Resting and exercise haemodynamics in relation to six-minute walk test in patients with heart failure and preserved ejection fraction. Eur J Heart Fail 20(4):715–722. https://doi.org/10.1002/ejhf.976
Dorfs S, Zeh W, Hochholzer W, Jander N, Kienzle RP, Pieske B, Neumann FJ (2014) Pulmonary capillary wedge pressure during exercise and long-term mortality in patients with suspected heart failure with preserved ejection fraction. Eur Heart J 35(44):3103–3112. https://doi.org/10.1093/eurheartj/ehu315
Burkhoff D, Maurer MS, Joseph SM, Rogers JG, Birati EY, Rame JE, Shah SJ (2015) Left atrial decompression pump for severe heart failure with preserved ejection fraction: theoretical and clinical considerations. JACC Heart Fail 3(4):275–282. https://doi.org/10.1016/j.jchf.2014.10.011
Granegger M, Dave H, Knirsch W, Thamsen B, Schweiger M, Hübler M (2019) A valveless pulsatile pump for the treatment of heart failure with preserved ejection fraction: a simulation study. Cardiovasc Eng Technol 10(1):69–79. https://doi.org/10.1007/s13239-018-00398-8
Fu M, Zhou J, Sun A, Zhang S, Zhang C, Zou Y, Fu M, Ge J (2012) Efficacy of ACE inhibitors in chronic heart failure with preserved ejection fraction–a meta analysis of 7 prospective clinical studies. Int J Cardiol 155(1):33–38. https://doi.org/10.1016/j.ijcard.2011.01.081
Massie BM, Carson PE, McMurray JJ, Komajda M, McKelvie R, Zile MR, Anderson S, Donovan M, Iverson E, Staiger C, Ptaszynska A (2008) Irbesartan in patients with heart failure and preserved ejection fraction. N Engl J Med 359(23):2456–2467. https://doi.org/10.1056/NEJMoa0805450
Liu F, Chen Y, Feng X, Teng Z, Yuan Y, Bin J (2014) Effects of beta-blockers on heart failure with preserved ejection fraction: a meta-analysis. PLoS ONE 9(3):e90555. https://doi.org/10.1371/journal.pone.0090555
Bonsu KO, Arunmanakul P, Chaiyakunapruk N (2018) Pharmacological treatments for heart failure with preserved ejection fraction-a systematic review and indirect comparison. Heart Fail Rev 23(2):147–156. https://doi.org/10.1007/s10741-018-9679-y
McMurray JJ, Packer M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR (2014) Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med 371(11):993–1004. https://doi.org/10.1056/NEJMoa1409077
Solomon SD, McMurray JJV, Anand IS, Ge J, Lam CSP, Maggioni AP, Martinez F, Packer M, Pfeffer MA, Pieske B, Redfield MM, Rouleau JL, van Veldhuisen DJ, Zannad F, Zile MR, Desai AS, Claggett B, Jhund PS, Boytsov SA, Comin-Colet J, Cleland J, Düngen HD, Goncalvesova E, Katova T, Kerr Saraiva JF, Lelonek M, Merkely B, Senni M, Shah SJ, Zhou J, Rizkala AR, Gong J, Shi VC, Lefkowitz MP (2019) Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620. https://doi.org/10.1056/NEJMoa1908655
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, Silverman MG, Zelniker TA, Kuder JF, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Ruff CT, Gause-Nilsson IAM, Fredriksson M, Johansson PA, Langkilde AM, Sabatine MS (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357. https://doi.org/10.1056/NEJMoa1812389
Tanaka H, Soga F, Tatsumi K, Mochizuki Y, Sano H, Toki H, Matsumoto K, Shite J, Takaoka H, Doi T, Hirata KI (2020) Positive effect of dapagliflozin on left ventricular longitudinal function for type 2 diabetic mellitus patients with chronic heart failure. Cardiovasc Diabetol 19(1):6. https://doi.org/10.1186/s12933-019-0985-z
Burlacu A, Simion P, Nistor I, Covic A, Tinica G (2019) Novel percutaneous interventional therapies in heart failure with preserved ejection fraction: an integrative review. Heart Fail Rev 24(5):793–803. https://doi.org/10.1007/s10741-019-09787-0
Gupta A, Bailey SR (2018) Update on devices for diastolic dysfunction: options for a no option condition? Curr Cardiol Rep 20(10):85. https://doi.org/10.1007/s11886-018-1027-2
Kaye DM, Nanayakkara S (2019) Interatrial shunt device for heart failure with preserved ejection fraction. Front Cardiovasc Med 6:143. https://doi.org/10.3389/fcvm.2019.00143
Kaye D, Shah SJ, Borlaug BA, Gustafsson F, Komtebedde J, Kubo S, Magnin C, Maurer MS, Feldman T, Burkhoff D (2014) Effects of an interatrial shunt on rest and exercise hemodynamics: results of a computer simulation in heart failure. J Card Fail 20(3):212–221. https://doi.org/10.1016/j.cardfail.2014.01.005
Søndergaard L, Reddy V, Kaye D, Malek F, Walton A, Mates M, Franzen O, Neuzil P, Ihlemann N, Gustafsson F (2014) Transcatheter treatment of heart failure with preserved or mildly reduced ejection fraction using a novel interatrial implant to lower left atrial pressure. Eur J Heart Fail 16(7):796–801. https://doi.org/10.1002/ejhf.111
Hasenfuß G, Hayward C, Burkhoff D, Silvestry FE, McKenzie S, Gustafsson F, Malek F, Van der Heyden J, Lang I, Petrie MC, Cleland JG, Leon M, Kaye DM (2016) A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, open-label, single-arm, phase 1 trial. Lancet 387(10025):1298–1304. https://doi.org/10.1016/s0140-6736(16)00704-2
Kaye DM, Hasenfuß G, Neuzil P, Post MC, Doughty R, Trochu JN, Kolodziej A, Westenfeld R, Penicka M, Rosenberg M, Walton A, Muller D, Walters D, Hausleiter J, Raake P, Petrie MC, Bergmann M, Jondeau G, Feldman T, Veldhuisen DJ, Ponikowski P, Silvestry FE, Burkhoff D, Hayward C (2016) One-year outcomes after transcatheter insertion of an interatrial shunt device for the management of heart failure with preserved ejection fraction. Circ Heart Fail 9(12):e003662. https://doi.org/10.1161/circheartfailure.116.003662
Feldman T, Mauri L, Kahwash R, Litwin S, Ricciardi MJ, van der Harst P, Penicka M, Fail PS, Kaye DM, Petrie MC, Basuray A, Hummel SL, Forde-McLean R, Nielsen CD, Lilly S, Massaro JM, Burkhoff D, Shah SJ (2018) Transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction (REDUCE LAP-HF I [reduce elevated left atrial pressure in patients with heart failure]): a phase 2, randomized. Sham-controlled trial Circulation 137(4):364–375. https://doi.org/10.1161/circulationaha.117.032094
Wessler J, Kaye D, Gustafsson F, Petrie MC, Hasenfuβ G, Lam CSP, Borlaug BA, Komtebedde J, Feldman T, Shah SJ, Burkhoff D (2018) Impact of baseline hemodynamics on the effects of a transcatheter interatrial shunt device in heart failure with preserved ejection fraction. Circ Heart Fail 11(8):e004540. https://doi.org/10.1161/circheartfailure.117.004540
Kaye DM, Petrie MC, McKenzie S, Hasenfuβ G, Malek F, Post M, Doughty RN, Trochu JN, Gustafsson F, Lang I, Kolodziej A, Westenfeld R, Penicka M, Rosenberg M, Hausleiter J, Raake P, Jondeau G, Bergmann MW, Spelman T, Aytug H, Ponikowski P, Hayward C (2019) Impact of an interatrial shunt device on survival and heart failure hospitalization in patients with preserved ejection fraction. ESC Heart Fail 6(1):62–69. https://doi.org/10.1002/ehf2.12350
Shah SJ, Feldman T, Ricciardi MJ, Kahwash R, Lilly S, Litwin S, Nielsen CD, van der Harst P, Hoendermis E, Penicka M, Bartunek J, Fail PS, Kaye DM, Walton A, Petrie MC, Walker N, Basuray A, Yakubov S, Hummel SL, Chetcuti S, Forde-McLean R, Herrmann HC, Burkhoff D, Massaro JM, Cleland JGF, Mauri L (2018) One-year safety and clinical outcomes of a transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction in the reduce elevated left atrial pressure in patients with heart failure (REDUCE LAP-HF I) Trial: a randomized clinical trial. JAMA Cardiol 3(10):968–977. https://doi.org/10.1001/jamacardio.2018.2936
Hanff TC, Kaye DM, Hayward CS, Post MC, Malek F, Hasenfuβ G, Gustafsson F, Burkhoff D, Shah SJ, Litwin SE, Kahwash R, Hummel SL, Borlaug BA, Solomon SD, Lam CSP, Komtebedde J, Silvestry FE (2019) Assessment of predictors of left atrial volume response to a transcatheter InterAtrial Shunt Device (from the REDUCE LAP-HF Trial). Am J Cardiol 124(12):1912–1917. https://doi.org/10.1016/j.amjcard.2019.09.019
Amat-Santos IJ, Nombela-Franco L, García B, Tobar J, Rodés-Cabau J, San Román JA (2015) The V-Wave Device f for the treatment of heart failure. Initial experience in Europe. Rev Esp Cardiol (Engl Ed) 68(9):808–810. https://doi.org/10.1016/j.rec.2015.04.015
Amat-Santos IJ, Bergeron S, Bernier M, Allende R, Barbosa Ribeiro H, Urena M, Pibarot P, Verheye S, Keren G, Yaacoby M, Nitzan Y, Abraham WT, Rodés-Cabau J (2015) Left atrial decompression through unidirectional left-to-right interatrial shunt for the treatment of left heart failure: first-in-man experience with the V-Wave device. EuroIntervention 10(9):1127–1131. https://doi.org/10.4244/eijy14m05_07
Rodés-Cabau J, Bernier M, Amat-Santos IJ, Ben Gal T, Nombela-Franco L, García Del Blanco B, Kerner A, Bergeron S, Del Trigo M, Pibarot P, Shkurovich S, Eigler N, Abraham WT (2018) Interatrial shunting for heart failure: early and late results from the first-in-human experience with the V-Wave System. JACC Cardiovasc Interv 11(22):2300–2310. https://doi.org/10.1016/j.jcin.2018.07.001
Del Trigo M, Bergeron S, Bernier M, Amat-Santos IJ, Puri R, Campelo-Parada F, Altisent OA, Regueiro A, Eigler N, Rozenfeld E, Pibarot P, Abraham WT, Rodés-Cabau J (2016) Unidirectional left-to-right interatrial shunting for treatment of patients with heart failure with reduced ejection fraction: a safety and proof-of-principle cohort study. Lancet 387(10025):1290–1297. https://doi.org/10.1016/s0140-6736(16)00585-7
Patel MB, Samuel BP, Girgis RE, Parlmer MA, Vettukattil JJ (2015) Implantable atrial flow regulator for severe, irreversible pulmonary arterial hypertension. EuroIntervention 11(6):706–709. https://doi.org/10.4244/eijy15m07_08
Rajeshkumar R, Pavithran S, Sivakumar K, Vettukattil JJ (2017) Atrial septostomy with a predefined diameter using a novel occlutech atrial flow regulator improves symptoms and cardiac index in patients with severe pulmonary arterial hypertension. Catheter Cardiovasc Interv 90(7):1145–1153. https://doi.org/10.1002/ccd.27233
Borggrefe M, Mann DL (2018) Cardiac contractility modulation in 2018. Circulation 138(24):2738–2740. https://doi.org/10.1161/circulationaha.118.036460
Tschöpe C, Van Linthout S, Spillmann F, Klein O, Biewener S, Remppis A, Gutterman D, Linke WA, Pieske B, Hamdani N, Roser M (2016) Cardiac contractility modulation signals improve exercise intolerance and maladaptive regulation of cardiac key proteins for systolic and diastolic function in HFpEF. Int J Cardiol 203:1061–1066. https://doi.org/10.1016/j.ijcard.2015.10.208
Abi-Samra F, Gutterman D (2016) Cardiac contractility modulation: a novel approach for the treatment of heart failure. Heart Fail Rev 21(6):645–660. https://doi.org/10.1007/s10741-016-9571-6
Borggrefe MM, Lawo T, Butter C, Schmidinger H, Lunati M, Pieske B, Misier AR, Curnis A, Böcker D, Remppis A, Kautzner J, Stühlinger M, Leclerq C, Táborsky M, Frigerio M, Parides M, Burkhoff D, Hindricks G (2008) Randomized, double blind study of non-excitatory, cardiac contractility modulation electrical impulses for symptomatic heart failure. Eur Heart J 29(8):1019–1028. https://doi.org/10.1093/eurheartj/ehn020
Kadish A, Nademanee K, Volosin K, Krueger S, Neelagaru S, Raval N, Obel O, Weiner S, Wish M, Carson P, Ellenbogen K, Bourge R, Parides M, Chiacchierini RP, Goldsmith R, Goldstein S, Mika Y, Burkhoff D, Abraham WT (2011) A randomized controlled trial evaluating the safety and efficacy of cardiac contractility modulation in advanced heart failure. Am Heart J 161 (2):329–337.e321–322. https://doi.org/10.1016/j.ahj.2010.10.025
Abraham WT, Kuck KH, Goldsmith RL, Lindenfeld J, Reddy VY, Carson PE, Mann DL, Saville B, Parise H, Chan R, Wiegn P, Hastings JL, Kaplan AJ, Edelmann F, Luthje L, Kahwash R, Tomassoni GF, Gutterman DD, Stagg A, Burkhoff D, Hasenfuß G (2018) A randomized controlled trial to evaluate the safety and efficacy of cardiac contractility modulation. JACC Heart Fail 6(10):874–883. https://doi.org/10.1016/j.jchf.2018.04.010
Borggrefe M, Burkhoff D (2012) Clinical effects of cardiac contractility modulation (CCM) as a treatment for chronic heart failure. Eur J Heart Fail 14(7):703–712. https://doi.org/10.1093/eurjhf/hfs078
Morris DA, Gailani M, Vaz Pérez A, Blaschke F, Dietz R, Haverkamp W, Ozcelik C (2011) Left atrial systolic and diastolic dysfunction in heart failure with normal left ventricular ejection fraction. J Am Soc Echocardiogr 24(6):651–662. https://doi.org/10.1016/j.echo.2011.02.004
Maass AH, Van Gelder IC (2012) Atrial resynchronization therapy: a new concept for treatment of heart failure with preserved ejection fraction and prevention of atrial fibrillation? Eur J Heart Fail 14(3):227–229. https://doi.org/10.1093/eurjhf/hfs014
Liu S, Guan Z, Zheng X, Meng P, Wang Y, Li Y, Zhang Y, Yang J, Jia D, Ma C (2018) Impaired left atrial systolic function and inter-atrial dyssynchrony may contribute to symptoms of heart failure with preserved left ventricular ejection fraction: a comprehensive assessment by echocardiography. Int J Cardiol 257:177–181. https://doi.org/10.1016/j.ijcard.2017.12.042
Daubert C, Leclercq C, Le Breton H, Gras D, Pavin D, Pouvreau Y, Van Verooij P, Bakels N, Mabo P (1997) Permanent left atrial pacing with a specifically designed coronary sinus lead. Pacing Clin Electrophysiol 20(11):2755–2764. https://doi.org/10.1111/j.1540-8159.1997.tb05433.x
Laurent G, Eicher JC, Mathe A, Bertaux G, Barthez O, Debin R, Billard C, Philip JL, Wolf JE (2013) Permanent left atrial pacing therapy may improve symptoms in heart failure patients with preserved ejection fraction and atrial dyssynchrony: a pilot study prior to a national clinical research programme. Eur J Heart Fail 15(1):85–93. https://doi.org/10.1093/eurjhf/hfs150
Ng MM, Sica DA, Frishman WH (2011) Rheos: an implantable carotid sinus stimulation device for the nonpharmacologic treatment of resistant hypertension. Cardiol Rev 19(2):52–57. https://doi.org/10.1097/CRD.0b013e3181f87921
La Rovere MT, Pinna GD, Maestri R, Robbi E, Caporotondi A, Guazzotti G, Sleight P, Febo O (2009) Prognostic implications of baroreflex sensitivity in heart failure patients in the beta-blocking era. J Am Coll Cardiol 53(2):193–199. https://doi.org/10.1016/j.jacc.2008.09.034
Funakoshi K, Hosokawa K, Kishi T, Ide T, Sunagawa K (2014) Striking volume intolerance is induced by mimicking arterial baroreflex failure in normal left ventricular function. J Card Fail 20(1):53–59. https://doi.org/10.1016/j.cardfail.2013.11.007
Abraham WT, Zile MR, Weaver FA, Butter C, Ducharme A, Halbach M, Klug D, Lovett EG, Müller-Ehmsen J, Schafer JE, Senni M, Swarup V, Wachter R, Little WC (2015) Baroreflex activation therapy for the treatment of heart failure with a reduced ejection fraction. JACC Heart Fail 3(6):487–496. https://doi.org/10.1016/j.jchf.2015.02.006
Kirklin JK, Pagani FD, Kormos RL, Stevenson LW, Blume ED, Myers SL, Miller MA, Baldwin JT, Young JB, Naftel DC (2017) Eighth annual INTERMACS report: special focus on framing the impact of adverse events. J Heart Lung Transplant 36(10):1080–1086. https://doi.org/10.1016/j.healun.2017.07.005
Topilsky Y, Pereira NL, Shah DK, Boilson B, Schirger JA, Kushwaha SS, Joyce LD, Park SJ (2011) Left ventricular assist device therapy in patients with restrictive and hypertrophic cardiomyopathy. Circ Heart Fail 4(3):266–275. https://doi.org/10.1161/circheartfailure.110.959288
Wynne E, Bergin JD, Ailawadi G, Kern JA, Kennedy JL (2011) Use of a left ventricular assist device in hypertrophic cardiomyopathy. J Card Surg 26(6):663–665. https://doi.org/10.1111/j.1540-8191.2011.01331.x
Muthiah K, Phan J, Robson D, Macdonald PS, Keogh AM, Kotlyar E, Granger E, Dhital K, Spratt P, Jansz P, Hayward CS (2013) Centrifugal continuous-flow left ventricular assist device in patients with hypertrophic cardiomyopathy: a case series. Asaio j 59(2):183–187. https://doi.org/10.1097/MAT.0b013e318286018d
Lund LH, Matthews J, Aaronson K (2010) Patient selection for left ventricular assist devices. Eur J Heart Fail 12(5):434–443. https://doi.org/10.1093/eurjhf/hfq006
Moscato F, Wirrmann C, Granegger M, Eskandary F, Zimpfer D, Schima H (2013) Use of continuous flow ventricular assist devices in patients with heart failure and a normal ejection fraction: a computer-simulation study. J Thorac Cardiovasc Surg 145(5):1352–1358. https://doi.org/10.1016/j.jtcvs.2012.06.057
Escher A, Choi Y, Callaghan F, Thamsen B, Kertzscher U, Schweiger M, Hübler M, Granegger M (2020) A valveless pulsatile pump for heart failure with preserved ejection fraction: hemo- and fluid dynamic feasibility. Ann Biomed Eng 48(6):1821–1836. https://doi.org/10.1007/s10439-020-02492-2
Giridharan GA, Lederer C, Berthe A, Goubergrits L, Hutzenlaub J, Slaughter MS, Dowling RD, Spence PA, Koenig SC (2011) Flow dynamics of a novel counterpulsation device characterized by CFD and PIV modeling. Med Eng Phys 33(10):1193–1202. https://doi.org/10.1016/j.medengphy.2011.05.008
Morley D, Litwak K, Ferber P, Spence P, Dowling R, Meyns B, Griffith B, Burkhoff D (2007) Hemodynamic effects of partial ventricular support in chronic heart failure: results of simulation validated with in vivo data. J Thorac Cardiovasc Surg 133(1):21–28. https://doi.org/10.1016/j.jtcvs.2006.07.037
Fukamachi K, Horvath DJ, Karimov JH, Kado Y, Miyamoto T, Kuban BD, Starling RC (2020) Left atrial assist device to treat patients with heart failure with preserved ejection fraction: initial in vitro study. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2019.12.110
Santos AB, Kraigher-Krainer E, Gupta DK, Claggett B, Zile MR, Pieske B, Voors AA, Lefkowitz M, Bransford T, Shi V, Packer M, McMurray JJ, Shah AM, Solomon SD (2014) Impaired left atrial function in heart failure with preserved ejection fraction. Eur J Heart Fail 16(10):1096–1103. https://doi.org/10.1002/ejhf.147
Persson H, Lonn E, Edner M, Baruch L, Lang CC, Morton JJ, Ostergren J, McKelvie RS (2007) Diastolic dysfunction in heart failure with preserved systolic function: need for objective evidence: results from the CHARM Echocardiographic Substudy-CHARMES. J Am Coll Cardiol 49(6):687–694. https://doi.org/10.1016/j.jacc.2006.08.062
Zeitler EP, Abraham WT (2020) Novel devices in heart failure: BAT, Atrial Shunts, and Phrenic Nerve Stimulation. JACC Heart Fail 8(4):251–264. https://doi.org/10.1016/j.jchf.2019.11.006
Ter Maaten JM, Damman K, Verhaar MC, Paulus WJ, Duncker DJ, Cheng C, van Heerebeek L, Hillege HL, Lam CS, Navis G, Voors AA (2016) Connecting heart failure with preserved ejection fraction and renal dysfunction: the role of endothelial dysfunction and inflammation. Eur J Heart Fail 18(6):588–598. https://doi.org/10.1002/ejhf.497
Shah SJ, Kitzman DW, Borlaug BA, van Heerebeek L, Zile MR, Kass DA, Paulus WJ (2016) Phenotype-specific treatment of heart failure with preserved ejection fraction: a multiorgan roadmap. Circulation 134(1):73–90. https://doi.org/10.1161/circulationaha.116.021884
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Kiyotaka Fukamachi, Jamshid H. Karimov, and Randall C. Starling are co-inventors of the LAAD. The other coauthors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Miyagi, C., Miyamoto, T., Karimov, J.H. et al. Device-based treatment options for heart failure with preserved ejection fraction. Heart Fail Rev 26, 749–762 (2021). https://doi.org/10.1007/s10741-020-10067-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10741-020-10067-5