Abstract
Background
Inflammatory bowel disease (IBD) patients who have Clostridioides difficile infection (CDI) have worse outcomes.
Aims
We aimed to determine whether such outcomes are the result of CDI or whether CDI occurs in patients who have more severe IBD.
Methods
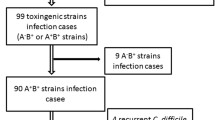
This was a retrospective study of patients hospitalized for ≥ 2 IBD flares from 2010 to 2019. The primary outcome was time to IBD flare between hospitalizations. First, time to flare was compared between patients who were hospitalized for a flare complicated by CDI and subsequently for a CDI-negative flare (cohort A, denoted +/−) versus patients who were hospitalized for two CDI-negative flares (cohort B, −/−). Second, time between flares was compared within the subset of cohort A patients who had three flares (cohort C, −/+/−) before and after CDI.
Results
Time between flares was a median of 4 months (IQR 1–9) among 51 cohort A patients versus 12 months (IQR 6–38) among 51 cohort B patients (log-rank P < 0.01). In contrast, the median time between flares was similar within cohort C before and after CDI (log-rank P = 0.54). At time of the second IBD flare, patients in cohort A (+/−) were more likely to have moderate or severe disease compared to patients in cohort B (−/−).
Conclusions
Patients with prior CDI had shorter time to subsequent IBD flare relative to their CDI-negative counterparts. This is not likely due to CDI itself because there was no difference in time between flares before versus after acquiring CDI. Rather, patients who acquire CDI may have more severe IBD.



Similar content being viewed by others
References
Malik T, Mannon P. Inflammatory bowel diseases: emerging therapies and promising molecular targets. Front Biosci (Schol Ed). 2012;4:1172–1189.
Ananthakrishnan AN. Epidemiology and risk factors for IBD. Nat Rev Gastroenterol Hepatol. 2015;12:205–217.
Azimi T, Nasiri MJ, Chirani AS, Pouriran R, Dabiri H. The role of bacteria in the inflammatory bowel disease development: a narrative review. APMIS. 2018;126:275–283.
Kostic AD, Xavier RJ, Gevers D. The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology. 2014;146:1489–1499.
Jostins L, Ripke S, Weersma RK, et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature. 2012;491:119–124.
Nguyen GC, Kaplan GG, Harris ML, Brant SR. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol. 2008;103:1443–1450.
Surawicz CM, Brandt LJ, Binion DG, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol. 2013;108:478–498. quiz 99.
Larson AM, Fung AM, Fang FC. Evaluation of tcdB real-time PCR in a three-step diagnostic algorithm for detection of toxigenic Clostridium difficile. J Clin Microbiol. 2010;48:124–130.
Brignola C, Campieri M, Bazzocchi G, Farruggia P, Tragnone A, Lanfranchi GA. A laboratory index for predicting relapse in asymptomatic patients with Crohn’s disease. Gastroenterology. 1986;91:1490–1494.
D’Haens G, Baert F, van Assche G, et al. Early combined immunosuppression or conventional management in patients with newly diagnosed Crohn’s disease: an open randomised trial. Lancet. 2008;371:660–667.
Sahmoud T, Hoctin-Boes G, Modigliani R, et al. Identifying patients with a high risk of relapse in quiescent Crohn’s disease. The GETAID Group. The Groupe d’Etudes Therapeutiques des Affections Inflammatoires Digestives. Gut.. 1995;37:811–818.
Henriksen M, Jahnsen J, Lygren I, et al. Clinical course in Crohn’s disease: results of a five-year population-based follow-up study (the IBSEN study). Scand J Gastroenterol. 2007;42:602–610.
Peyrin-Biroulet L, Panes J, Sandborn WJ, et al. Defining disease severity in inflammatory bowel diseases: current and future directions. Clin Gastroenterol Hepatol. 2016;14:348–54.e17.
Kutty PK, Woods CW, Sena AC, et al. Risk factors for and estimated incidence of community-associated Clostridium difficile infection, North Carolina, USA. Emerg Infect Dis. 2010;16:197–204.
Bossuyt P, Verhaegen J, Van Assche G, Rutgeerts P, Vermeire S. Increasing incidence of Clostridium difficile-associated diarrhea in inflammatory bowel disease. J Crohns Colitis. 2009;3:4–7.
Rodemann JF, Dubberke ER, Reske KA, Seo DH, Stone CD. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5:339–344.
Schneeweiss S, Korzenik J, Solomon DH, Canning C, Lee J, Bressler B. Infliximab and other immunomodulating drugs in patients with inflammatory bowel disease and the risk of serious bacterial infections. Aliment Pharmacol Ther. 2009;30:253–264.
Kariv R, Navaneethan U, Venkatesh PG, Lopez R, Shen B. Impact of Clostridium difficile infection in patients with ulcerative colitis. J Crohns Colitis. 2011;5:34–40.
Ananthakrishnan AN, McGinley EL, Binion DG. Excess hospitalisation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut. 2008;57:205–210.
Issa M, Vijayapal A, Graham MB, et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007;5:345–351.
Berg AM, Kelly CP, Farraye FA. Clostridium difficile infection in the inflammatory bowel disease patient. Inflamm Bowel Dis. 2013;19:194–204.
Khanna S, Pardi DS. IBD: poor outcomes after Clostridium difficile infection in IBD. Nat Rev Gastroenterol Hepatol. 2012;9:307–308.
Jodorkovsky D, Young Y, Abreu MT. Clinical outcomes of patients with ulcerative colitis and co-existing Clostridium difficile infection. Dig Dis Sci. 2010;55:415–420. https://doi.org/10.1007/s10620-009-0749-9.
Yanai H, Nguyen GC, Yun L, et al. Practice of gastroenterologists in treating flaring inflammatory bowel disease patients with Clostridium difficile: antibiotics alone or combined antibiotics/immunomodulators? Inflamm Bowel Dis. 2011;17:1540–1546.
Ben-Horin S, Margalit M, Bossuyt P, et al. Combination immunomodulator and antibiotic treatment in patients with inflammatory bowel disease and Clostridium difficile infection. Clin Gastroenterol Hepatol. 2009;7:981–987.
Lukin DJ, Lawlor G, Hudesman DP, et al. Escalation of immunosuppressive therapy for inflammatory bowel disease is not associated with adverse outcomes after infection with Clostridium difficile. Inflamm Bowel Dis. 2019;25:775–781.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Varma, S., Faye, A.S., Kannan, A. et al. Patients with More Severe IBD Get Clostridioides difficile Rather than Clostridioides difficile Increasing the Severity of IBD. Dig Dis Sci 66, 3113–3123 (2021). https://doi.org/10.1007/s10620-020-06504-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-020-06504-y