Abstract
Purpose
The prospective assessment of Clostridium difficile infection (CDI) impact in inflammatory bowel disease (IBD) flare in outpatient setting has been poorly investigated. We aimed to evaluate the prevalence and the associated factors with CDI in IBD outpatients presenting colitis flares as well as the outcomes following treatment.
Methods
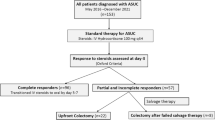
In this prospective cohort study, conducted from October, 2014, to July, 2016, 120 IBD patients (55% presenting colitis flare) and 40 non-IBD controls were assessed for CDI. Multivariate regression analysis was performed to identify predictors of CDI. Outcome analysis was estimated for recurrent CDI, hospitalization, colectomy, and CDI-associated mortality.
Results
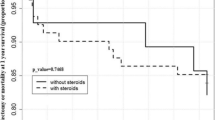
The number of patients with CDI was significantly higher in IBD patients experiencing flares than in both inactive IBD and non-IBD groups (28.8 vs. 5.6 vs. 0%, respectively; p = 0.001). Females (OR = 1.39, 95% CI, 1.13–17.18), younger age (OR = 0.77, 95% CI, 0.65–0.92), steroid treatment (OR = 7.42, 95% CI, 5.17–40.20), and infliximab therapy (OR = 2.97, 95% CI, 1.99–24.63) were found to be independently associated with CDI. There was a dose-related increase in the risks of CDI on patients which had taken prednisone. Those treated with vancomycin had a satisfactory response to therapy, but 21% presented recurrent CDI and 16% were hospitalized. Neither necessity of colectomy nor mortality was noticed in any patient during the investigation.
Conclusions
In IBD outpatients presenting colitis flares, CDI is highly prevalent. Females, younger age, infliximab, and notably steroid therapy were independently associated with CDI. Most patients with CDI experienced mild-to-moderate disease, and prompt treatment with vancomycin was highly effective, which seems to reduce the serious complication risks.

Similar content being viewed by others
References
Surawicz CM (2015) Clostridium difficile infection: risk factors, diagnosis and management. Curr Treat Options Gastroenterol l13:121–129
McDonald LC, Killgore GE, Thompson A et al (2005) An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med 353:2433–2441
Vindigni SM, Surawicz CM (2015) C. difficile infection: changing epidemiology and management paradigms. Clin Transl Gastroenterol 6:e99
Ananthakrishnan AN, McGinley EL, Binion DG (2008) Excess hospitalization burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut 57:205–210
Issa M, Vijayapal A, Graham MB, Beaulieu DB, Otterson MF, Lundeen S, Skaros S, Weber LR, Komorowski RA, Knox JF, Emmons J, Bajaj JS, Binion DG (2007) Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol 5:345–351
Bossuyt P, Verhaegen J, Van Assche G, Rutgeerts P, Vermeire S (2009) Increasing incidence of Clostridium difficile-associated diarrhea in inflammatory bowel disease. J Crohns Colitis 3:4–7
Jodorkovsky D, Young Y, Abreu MT (2010) Clinical outcomes of patients with ulcerative colitis and co-existing Clostridium difficile infection. Dig Dis Sci 55:415–420
Schneeweiss S, Korzenik J, Solomon DH et al (2009) Infliximab and other immunomodulating drugs in patients with inflammatory bowel disease and the risk of serious bacterial infections. Aliment Pharmacol Ther 30:253–264
Rao K, Higgins PD (2016) Epidemiology, diagnosis, and management of Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis 22:1744–1754
Jen MH, Saxena S, Bottle A, Aylin P, Pollok RCG (2011) Increased health burden associated with Clostridium difficile diarrhoea in patients with inflammatory bowel disease. Aliment Pharmacol Ther 33:1322–1331
Reddy SS, Brandt LJ (2013) Clostridium difficile infection and inflammatory bowel disease. J Clin Gastroenterol 47:666–671
Rodemann JF, Dubberke ER, Reske KA, Seo DH, Stone CD (2007) Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol 5:339–344
Kariv R, Navaneethan U, Venkatesh PG, Lopez R, Shen B (2011) Impact of Clostridium difficile infection in patients with ulcerative colitis. J Crohns Colitis 5:34–40
Navaneethan U, Mukewar S, Venkatesh PG, Lopez R, Shen B (2012) Clostridium difficile infection is associated with worse long term outcome in patients with ulcerative colitis. J Crohns Colitis 6:330–336
Ramos-Martínez A, Ortiz-Balbuena J, Curto-García I, Asensio-Vegas Á, Martínez-Ruiz R, Múñez-Rubio E, Cantero-Caballero M, Sánchez-Romero I, González-Partida I, Vera-Mendoza MI (2015) Risk factors for Clostridium difficile diarrhea in patients with inflammatory bowel disease. Rev Esp Enferm Dig 107:4–8
Negrón ME, Rezaie A, Barkema HW, Rioux K, de Buck J, Checkley S, Beck PL, Carroll M, Fedorak RN, Dieleman L, Panaccione R, Ghosh S, Kaplan GG (2016) Ulcerative colitis patients with Clostridium difficile are at increased risk of death, colectomy, and postoperative complications: a population-based inception cohort study. Am J Gastroenterol 111:691–704
Joshi NM, Marks IH, Crowson R, Ball D, Rampton DS (2017) Incidence and outcome of Clostridium difficile infection in hospitalized patients with inflammatory bowel disease in the UK. J Crohns Colitis 11:70–76
Van Assche G, Dignass A, Panes J et al (2010) The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. J Crohns Colitis 4:7–27
Silverberg MS, Satsangi J, Ahmad T, Arnott IDR, Bernstein CN, Brant SR, Caprilli R, Colombel JF, Gasche C, Geboes K, Jewell DP, Karban A, Loftus EV, Peña AS, Riddell RH, Sachar DB, Schreiber S, Steinhart AH, Targan SR, Vermeire S, Warren BF (2005) Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 19(Suppl A):5A–36A
Dignass A, Eliakim R, Magro F, Maaser C, Chowers Y, Geboes K, Mantzaris G, Reinisch W, Colombel JF, Vermeire S, Travis S, Lindsay JO, van Assche G (2012) Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis 6:965–990
Surawicz CM, Brandt LJ, Binion DG et al (2013) uidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 108:478–498
Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, Pepin J, Wilcox MH (2010) Clinical practice guidelines for Clostridium difficile infection in adults: 2010 updated by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Disease Society of America (IDSA). Infect Control Hosp Epidemiol 31:431–455
Binion D (2016) Clostridium difficile infection and inflammatory bowel disease. Gastroenterol Hepatol 12:334–337
Kostic AD, Xavier RJ, Gevers D (2014) The microbiome in inflammatory bowel disease: current status and the future ahead. Gastroenterology 146:1489–1499
Razik R, Rumman A, Bahreini Z, McGeer A, Nguyen GC (2016) Recurrence of Clostridium difficile infection in patients with inflammatory bowel disease: the RECIDIVISM study. Am J Gastroenterol 111:1141–1146
Nguyen GC, Kaplan GG, Harris ML, Brant SR (2008) A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol 103:1443–1450
Gupta A, Khanna S (2014) Community-acquired Clostridium difficile infection: an increasing public health threat. Infect Drug Resist 7:63–72
Kim HB, Wang Y, Sun X (2016) A detrimental role of immunosuppressive drug, dexamethasone, during Clostridium difficile infection in association with a gastrointestinal microbial shift. J Microbiol Biotechnol 26:567–571
Zhang T, Lin QY, Fei JX, Zhang Y, Lin MY, Jiang SH, Wang P, Chen Y (2016) Clostridium difficile infection worsen outcome of hospitalized patients with inflammatory bowel disease. Sci Rep 6:29791
Papamichael K, Mantzaris GJ, Peyrin-Biroulet L (2016) A safety assessment of anti-tumor necrosis factor alpha therapy for treatment of Crohn’s disease. Expert Opin Drug Saf 15:493–501
Lichtenstein GR, Feagan BG, Cohen RD, Salzberg BA, Diamond RH, Price S, Langholff W, Londhe A, Sandborn WJ (2012) Serious infection and mortality in patients with Crohn’s disease: more than 5 years of follow-up in the TREAT registry. Am J Gastroenterol 107:1409–1422
Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, Bousvaros A, Dhanireddy S, Sung L, Keyserling H, Kang I, Infectious Diseases Society of America (2014) IDSA clinical practice guideline for vaccination of the immunocompromised host. Clin Infect Dis 58:e44–e100
Goodhand JR, Alazawi W, Rampton DS (2010) Systematic review: Clostridium difficile and inflammatory bowel disease. Aliment Pharmacol Ther 33:428–441
Kaneko T, Matsuda R, Taguri M, Inamori M, Ogura A, Miyajima E, Tanaka K, Maeda S, Kimura H, Kunisaki R (2011) Clostridium difficile infection in patients with ulcerative colitis: investigations of risk factors and efficacy of antibiotics for steroid refractory patients. Clin Res Hepatol Gastroenterol 35:315–320
Chen Y, Furuya-Kanamori L, Doi SA, Ananthakrishnan AN, Kirk M (2017) Clostridium difficile infection and risk of colectomy in patients with inflammatory bowel disease: a bias-adjusted meta-analysis. Inflamm Bowel Dis 23:200–207
Deshpande A, Pasupuleti V, Thota P, Pant C, Rolston DDK, Hernandez AV, Donskey CJ, Fraser TG (2015) Risk factors for recurrent Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol 36:452–460
Khoruts A, Sadowsky MJ, Hamilton MJ (2015) Development of fecal microbiota transplantation suitable for mainstream medicine. Clin Gastroenterol Hepatol 13:246–250
Khoruts A, Rank KM, Newman KM, Viskocil K, Vaughn BP, Hamilton MJ, Sadowsky MJ (2016) Inflammatory bowel disease affects the outcome of fecal microbiota transplantation for recurrent Clostridium difficile infection. Clin Gastroenterol Hepatol 14:1433–1438
Clayton EM, Rea MC, Shanahan F, Quigley EMM, Kiely B, Hill C, Ross RP (2009) The vexed relationship between Clostridium difficile and inflammatory bowel disease: an assessment of carriage in an outpatient setting among patients in remission. Am J Gastroenterol 104:1162–1169
Longtin Y, Paquet-Bolduc B, Gilca R, Garenc C, Fortin E, Longtin J, Trottier S, Gervais P, Roussy JF, Lévesque S, Ben-David D, Cloutier I, Loo VG (2016) Effect of detecting and isolating Clostridium difficile carriers at hospital admission on the incidence of C. difficile infections: a quasi-experimental controlled study. JAMA Intern Med 176:796–804
Funding source
This work was supported by a clinical research fund from the National Council of Scientific Researches (CNPq), Brazil.
Author information
Authors and Affiliations
Contributions
PGG, LAC, TCRR, PDG, and FHLP: study concept and design, acquisition, analysis and interpretation of data, and manuscript writing. WAC, ICA, and BRMM: manuscript critical revision, study design, and interpretation of data. AZ: statistical analysis, review and interpretation of data, and manuscript critical revision. ACSC, KVBDB, LAC, and ROR: data analysis and interpretation and manuscript critical revision. JMFC: study concept and design, acquisition, analysis and interpretation of data, manuscript writing, and study supervision.
All authors approved the final draft.
Corresponding author
Ethics declarations
The study protocol was defined in accordance with the Declaration of Helsinki and was approved by our Institutional Ethics Committee. All patients signed a freely informed consent form before being admitted to the study.
Financial disclosure
All authors have no financial relationships relevant to this article to disclose.
Conflicts of interest
Julio M F Chebli has received speaker fees from Abbott, Abbvie, Janssen, Takeda.
The remaining authors disclose no conflicts.
Rights and permissions
About this article
Cite this article
Garcia, P.G., Chebli, L.A., da Rocha Ribeiro, T.C. et al. Impact of superimposed Clostridium difficile infection in Crohn’s or ulcerative colitis flares in the outpatient setting. Int J Colorectal Dis 33, 1285–1294 (2018). https://doi.org/10.1007/s00384-018-3105-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3105-8