Abstract
Background
Maladaptive and adaptive emotion regulation are putative risk and protective factors for depression and anxiety, but most prior research does not differentiate within-person effects from between-person individual differences. The current study does so during the early part of the Covid-19 pandemic when internalizing symptoms were high.
Methods
A sample of emerging adult undergraduate students (N = 154) completed online questionnaires bi-weekly on depression, anxiety, and emotion regulation across eight weeks during the early days of the Covid-19 pandemic (April 2nd to June 27th, 2020).
Results
Depression demonstrated significantly positive between-person correlations with overall maladaptive emotion regulation, catastrophizing, and self-blame, and negative correlations with overall adaptive emotion regulation and reappraisal. Anxiety demonstrated significantly positive between-person correlations with overall maladaptive emotion regulation, rumination, and catastrophizing, and a negative correlation with reappraisal. After controlling for these between-person associations, however, there were generally no within-person associations between emotion regulation and internalizing symptoms.
Conclusions
Emotion regulation and internalizing symptoms might be temporally stable individual differences that cooccur with one another as opposed to having a more dynamic relation. Alternatively, these dynamic mechanisms might operate over much shorter or longer periods compared to the two-week time lag in the current study.
Similar content being viewed by others
Introduction
Emerging adulthood, spanning ages 18 to 29, is a developmental period of increased risks for the development and maintenance of internalizing symptoms (Arnett et al., 2014). Among emerging adults in the U.S., the lifetime prevalence of major depressive disorder is approximately 15%, and the lifetime prevalence of any anxiety disorder is around 30% (Kessler et al., 2005). Internalizing symptoms can cause significant distress and dysfunction in various domains of daily living, such as increased somatic symptoms, poor academic performance, and impaired social functioning (Beiter et al., 2015; Jamnik & DiLalla, 2019). As longitudinal studies indicated that there has been an increased prevalence of moderate to severe depression and anxiety symptoms in emerging adults during the Covid-19 pandemic in comparison to before (Ettman et al., 2020; Fruehwirth et al., 2021), it is especially important to understand pathways of risk and resilience factors for internalizing symptoms.
Emotion regulation is the application of cognitive and behavioral strategies that modulate emotional responses. Emotion regulation strategies can be characterized as maladaptive when they are associated with negative outcomes (i.e., higher frequency of negative life events and higher levels of depression and anxiety symptoms), and adaptive when they are associated with positive outcomes (i.e., experiencing negative life events less frequently and reporting lower depression and anxiety symptoms; Garnefski et al., 2001). Meta-analytic reviews indicate that the use of maladaptive emotion regulation strategies can be vulnerability markers of depression and anxiety, whereas adaptive emotion regulation strategies function as protective factors against them (Aldao et al., 2010; Schäfer et al., 2017). One maladaptive response to negative emotion is rumination, defined as thinking about feelings and thoughts associated with the negative event (Watkins & Roberts, 2020). Rumination is considered maladaptive because it has been associated with more negative life events and higher depression and anxiety symptoms (Watkins & Roberts, 2020). However, most longitudinal studies regarding the role of emotion regulation on internalizing symptoms focus on rumination but not other emotion regulation strategies. Therefore, the current longitudinal study seeks to examine specific emotion regulation strategies as vulnerability and resilience factors for internalizing symptoms during the ongoing pandemic among emerging adults.
Although it is well established that emotion regulation strategies and internalizing symptoms are associated with one another, prior research has not generally used statistical methods that correctly differentiate between-person effects (i.e., stable individual differences in internalizing symptoms which covary with stable individual differences in emotion regulation profiles), within-person effects (i.e., changes in emotion regulation strategies lead to changes in symptoms over time), or a combination of both (Hamaker & Kuiper, 2015). This distinction is critical, as many theories posit a causal role for emotion regulation in changing symptoms within-persons (Joormann & Vanderlind, 2014; Joormann et al., 2010; Lazarus & Folkman, 1984), but there are few direct tests of within-person changes. Some longitudinal studies have attempted to examine within-person changes by controlling internalizing symptoms at baseline (e.g., Broderick & Korteland, 2016; Hatzenbuehler et al., 2008; Hong, 2007; Whisman et al., 2020). Although including baseline measures accounts for autoregressive effects (i.e., how baseline internalizing symptoms predict internalizing symptoms at follow-up), such tests assume no individual differences in how internalizing symptoms may vary over time and can lead to inaccurate conclusions regarding within-person changes (Hamaker & Kuiper, 2015). In other words, including baseline measures corrects for the temporal stability in internalizing symptoms over the duration of study periods, but it does not adequately control for the trait-like stability for which individuals might have different trajectories in internalizing symptom severity. An alternative statistical model, the random intercept cross‐lagged panel model (RI‐CLPM), has been developed to separate between-person from within-person effects (Hamaker & Kuiper, 2015). Thus, our study also used the RI-CLPM to decompose the time-invariant between-person associations between emotion regulation and internalizing symptoms from the time-variant within-person effects to better test theories about risk and protective mechanisms.
Maladaptive Emotion Regulation as a Risk Factor
Maladaptive emotion regulation, specifically rumination, catastrophizing, and self-blame, can represent risk factors of internalizing symptoms. Rumination refers to repetitively focusing on negative events and feelings, and such fixation on past or current distress can prolong the length of time negative emotional processing reside in working memory (Garnefski et al., 2001; Joormann et al., 2010). Similarly, catastrophizing is the over-emphasizing of the consequences associated with negative experiences and can exaggerate the salience of negative emotional processing in working memory (Garnefski et al., 2001; Joormann et al., 2010). Self-blame, the tendency to view stressful and negative events as having internal causes, is associated with self-attribution bias and produces emotional difficulties characterized by having dysfunctional negative views of the self, world, and future (Garnefski et al., 2001; Rubenstein et al., 2016). Rumination, catastrophizing, and self-blame can all in theory lead to imbalanced engagement in negative over positive experiences, increaseing negative affect, and therefore act as transdiagnostic risk factors for depression and anxiety (Everaert & Joormann, 2019; Joormann & Vanderlind, 2014; Laird, 1974).
It is well-established that these maladaptive emotion regulation strategies are associated with increased internalizing symptoms. Both cross-sectional (Garnefski et al., 2002, 2003, 2004; Kraaij, Garnefski, de Wilde, et al., 2003; Kraaij et al., 2008a; Martin & Dahlen, 2005) and longitudinal studies (Broderick & Korteland, 2016; Butler & Nolen-Hoeksema, 1994a; Calmes & Roberts, 2007; Grabe et al., 2016; Hatzenbuehler et al., 2008; Hong, 2007; McLaughlin et al., 2011a; Nolen-Hoeksema, 2000; Sarin et al., 2005; Whisman et al., 2020) indicate between-person associations between rumination and higher depression and anxiety symptoms. Longitudinal studies that controlled for baseline internalizing symptoms with study periods ranging from two weeks to four years provide evidence that rumination is associated with worsened depression (Broderick & Korteland, 2016; Butler & Nolen-Hoeksema, 1994b; Hatzenbuehler et al., 2008; Hong, 2007; Sarin et al., 2005; Whisman et al., 2020) and anxiety symptoms (Calmes & Roberts, 2007; Hatzenbuehler et al., 2008; Sarin et al., 2005) over time.
Cross-sectional studies have showed the between-person effects between catastrophizing and higher depression and anxiety symptoms (Dehghanizadeh et al., 2017; Garnefski et al., 2002, 2003, 2004; Kraaij et al., 2003a, b; Kraaij, Garnefski, de Wilde, et al., 2003; Kraaij et al., 2008a; Martin & Dahlen, 2005; Min et al., 2013; Sullivan et al., 1995). Longitudinal studies over the course of two (Kraaij et al., 2008b) and two and half years (Kraaij et al., 2002) have established the between-person effects of catastrophizing on subsequent depression but not subsequent anxiety, although these studies did not control for baseline depression.
Finally, self-blame is linked to higher depression and anxiety symptoms between-persons, both concurrently (Anderson et al., 1994; Domaradzka & Fajkowska, 2018; Garnefski et al., 2002, 2003, 2004; Kraaij, Garnefski, de Wilde, et al., 2003; Martin & Dahlen, 2005; Min et al., 2013; Orgeta & Orrell, 2014) and prospectively over two years (Kraaij et al., 2008b).
In conclusion, rumination, catastrophizing, and self-blame are transdiagnostic risk factors for depression and anxiety. Based on the average effect sizes calculated from this prior research (Anderson et al., 1994; Calmes & Roberts, 2007; Dehghanizadeh et al., 2017; Garnefski et al., 2002, 2003, 2004; Grabe et al., 2016; Hatzenbuehler et al., 2008; Hong, 2007; Kraaij et al., 2002, 2008b; Kraaij, Garnefski, de Wilde, et al., 2003; Martin & Dahlen, 2005; Min et al., 2013; Nolen-Hoeksema, 2000; Wang et al., 2014), these maladaptive strategies have similar associations with depression (β = 0.224) and anxiety (β = 0.217).
Adaptive Emotion Regulation as a Resilience Factor
In general, adaptive emotion regulation can be divided into two categories: problem-focused and emotion-focused strategies. Problem-focused strategies exert control over the stressor, whereas emotion-focused strategies manage the negative emotional experiences associated with the stressor (Lazarus & Folkman, 1984). Problem-focused strategies typically involve planning, more specifically proposing problem-solving options, weighing the pros and cons of various options, and deciding on a final plan to solve the problem (Lazarus & Folkman, 1984). Therefore, problem-focused strategies are linked to lowered risks of depression and anxiety symptoms (Priester & Clum, 1993). Reappraisal is an emotion-focused strategy that aims to give benign interpretations to stressful events and reframe negative materials with positive meaning and personal growth (Garnefski et al., 2001). Acceptance, defined as accepting and resigning oneself to what has happened, is another emotion-focused strategy that is associated with high self-esteem, optimism, and low negative affect (Carver et al., 1989; Cheung & Ng, 2019; Garnefski et al., 2001). Reappraisal and acceptance might be able to manage the negative thoughts and emotions associated with the stressor, counterbalance the negative effects of rumination and catastrophizing, and therefore function as transdiagnostic resilience factors for depression and anxiety (Joormann et al., 2010).
Frequent use of adaptive emotion regulation is linked to lower internalizing symptoms. There are between-person associations between planning and lower depression and anxiety symptoms both concurrently (Carver et al., 1989; Min et al., 2013; Siu & Shek, 2010) and prospectively over eight to 16 days (Priester & Clum, 1993) and over one year (Vollrath et al., 1996). One study that controlled for baseline anxiety demonstrated the effects of planning on decreased anxiety symptoms over one year (Vollrath et al., 1996).
Likewise, cross-sectional studies indicate the between-person association of reappraisal with lower depression and anxiety symptoms (Carver et al., 1989; Garnefski et al., 2002, 2003, 2004; Kraaij et al., 2008a; Kraaij et al., 2003a, b; Martin & Dahlen, 2005; Xu et al., 2020). Longitudinal studies controlling for baseline symptom levels demonstrate that reappraisal contributes to decreases in depression symptoms over one month (Wang et al., 2014) and two and half years (Kraaij et al., 2002) and decreases in anxiety symptoms over one month (Krafft et al., 2019) and nine years (Hittner et al., 2019).
However, there are inconsistent findings regarding the association between acceptance and internalizing symptoms. Longitudinal studies that controlled for baseline internalizing symptom levels found the effects of acceptance on decreased symptom levels of depression and anxiety over one month (Wang et al., 2014) and over one and half years (Cheung & Ng, 2019). However, one longitudinal study (Kraaij et al., 2002) and many cross-sectional studies found that acceptance is related to higher depression and anxiety symptoms between-persons (Garnefski et al., 2002; Kraaij et al., 2003a, b; Martin & Dahlen, 2005).
To summarize, research supports reappraisal and planning as transdiagnostic protective factors against depression and anxiety. The average effect sizes calculated from this prior research (Cheung & Ng, 2019; Garnefski et al., 2002, 2003, 2004; Kraaij et al., 2002; Kraaij, Garnefski, de Wilde, et al., 2003; Martin & Dahlen, 2005; Min et al., 2013; Orgeta & Orrell, 2014, 2014; Siu & Shek, 2010; Vollrath et al., 1996; Wang et al., 2014; Xu et al., 2020) suggest these two strategies have similar associations with depression (β = -0.164) and anxiety (β = -0.155). However, findings are mixed regarding the association between acceptance and internalizing symptoms.
The Present Study
Pre-Covid research has supported maladaptive emotion regulation as a vulnerability marker and adaptive emotion regulation as a protective factor for depression and anxiety. Maladaptive and adaptive emotion regulation strategies are associated with internalizing psychopathology in both adolescence (Broderick & Korteland, 2016; Garnefski et al., 2003; Grabe et al., 2016; Hatzenbuehler et al., 2008; Kraaij, Garnefski, de Wilde, et al., 2003; McLaughlin et al., 2011a) and adulthood (Anderson et al., 1994; Butler & Nolen-Hoeksema, 1994b; Calmes & Roberts, 2007; Carver et al., 1989; Cheung & Ng, 2019; Dehghanizadeh et al., 2017; Domaradzka & Fajkowska, 2018, 2018; Garnefski et al., 2002, 2004, 2004; Hittner et al., 2019, 2019; Hong, 2007; Kraaij et al., 2002, 2008b; Krafft et al., 2019; Martin & Dahlen, 2005; Min et al., 2013; Nolen-Hoeksema, 2000; Orgeta & Orrell, 2014; Priester & Clum, 1993; Sarin et al., 2005; Siu & Shek, 2010; Sullivan et al., 1995; Whisman et al., 2020; Xu et al., 2020). While most studies examined community samples (Anderson et al., 1994; Broderick & Korteland, 2016; Butler & Nolen-Hoeksema, 1994b; Calmes & Roberts, 2007; Carver et al., 1989; Cheung & Ng, 2019; Dehghanizadeh et al., 2017; Domaradzka & Fajkowska, 2018, 2018; Garnefski et al., 2002, 2003, 2004, 2004; Grabe et al., 2016; Hatzenbuehler et al., 2008; Hittner et al., 2019, 2019; Hong, 2007; Kraaij et al., 2002; Kraaij, Garnefski, de Wilde, et al., 2003; Krafft et al., 2019; Martin & Dahlen, 2005; McLaughlin et al., 2011b; Nolen-Hoeksema, 2000; Orgeta & Orrell, 2014; Priester & Clum, 1993; Sarin et al., 2005; Siu & Shek, 2010; Sullivan et al., 1995; Whisman et al., 2020; Xu et al., 2020), a few were conducted among psychiatric outpatients (Min et al., 2013; Vollrath et al., 1996) and other clinical populations (Kraaij et al., 2008b; Kraaij et al., 2003a, b; Wang et al., 2014).
However, there are key gaps in understanding these links between emotion regulation and internalizing psychopathology. First, past research supported that individual differences in the severity of depression and anxiety symptoms were associated with frequency of use of rumination, catastrophizing, self-blame, planning, reappraisal, and acceptance as their emotion regulation strategies (between-person effects). However, for many emotion regulation strategies, the key theoretical models in which changes in emotion regulation predict changes in severity of depression and anxiety symptoms over time (within-person effects) have not yet been adequately tested, because many longitudinal studies did not control for baseline measures. Even studies that did control for baseline measures generally have not used methods that adequately separate between-person from within-person variance (Hamaker & Kuiper, 2015). These studies could still establish prospective between-person associations but fail to test any changes within-persons. Second, most longitudinal studies that controlled for baseline internalizing symptom levels have examined the predictive effects of rumination, but not other emotion regulation strategies, on subsequent changes in depression (Broderick & Korteland, 2016; Butler & Nolen-Hoeksema, 1994b; Hatzenbuehler et al., 2008; Hong, 2007; Sarin et al., 2005, 2005; Whisman et al., 2020) and anxiety symptoms (Calmes & Roberts, 2007; Hatzenbuehler et al., 2008; Sarin et al., 2005) over time. As frequent use of catastrophizing and self-blame, as well as infrequent use of planning, reappraisal, and acceptance are all associated with increased negative emotional processing and general distress which are important vulnerability markers to causally affect internalizing symptoms (Joormann & Vanderlind, 2014; Joormann et al., 2010; Lazarus & Folkman, 1984), more longitudinal studies that appropriately separate between from within-person effects are needed to examine whether each of these strategies predict changes in depression and anxiety over time.
Therefore, it remains unclear whether the association between emotion regulation and internalizing symptoms arises from time-invariant between-person differences, time-variant within-person differences, or both. Within-person effects would support theories that changes in emotion regulation lead to changes in internalizing symptoms over time (Joormann & Vanderlind, 2014; Joormann et al., 2010; Lazarus & Folkman, 1984),. Alternatively, if there are only between-person associations, it could indicate that emotion regulation and internalizing symptoms either have reached an equilibrium where they help maintain stable levels of one another, or that they are associated because they have a common cause (i.e., shared environmental and/or genetic risk or protective factorsGoretti et al., 2010; Zobeir & Jafar, 2016). The current study used random intercept cross‐lagged panel models (RI‐CLPM) to decompose between-person and within-person effects of emotion regulation on internalizing symptoms.
The current study was conducted in a sample of emerging adult undergraduate students (n = 154) who completed online questionnaires of emotion regulation, depression, and anxiety bi-weekly across eight weeks during the early days of the Covid-19 pandemic in the United States (April 2nd to June 27th, 2020). The Covid-19 pandemic provides a unique opportunity to investigate the association between emotion regulation and internalizing symptoms during stressful times and is informative to other situations involving novel, unpredictable and uncontrollable stressors. A longitudinal study that compared mental health outcomes in a sub-sample of the current study (n = 54) demonstrated increased depression, anxiety, and catastrophizing, and decreased self-blame, planning, and reappraisal during the beginning of the pandemic (April 2020) in comparison to before the pandemic (Taylor et al., in press). Therefore, the pandemic may have exacerbated internalizing symptoms and altered the trajectories of maladaptive and adaptive emotion regulation in our sample. Relatedly, it remains unclear whether the mechanisms through which different emotion regulation strategies contribute to internalizing symptoms remain the same during the pandemic. The aim of the current study was thus to understand emotion regulation strategies as between-person and within-person risk and resilience factors for depression and anxiety among emerging adults during the Covid-19 pandemic.
First, we hypothesized between-person effects that participants with frequent use of maladaptive emotion regulation would report higher depression and anxiety symptoms, and participants with frequent use of adaptive emotion regulation would have lower depression and anxiety symptoms. Second, we hypothesized within-person effects that maladaptive emotion regulation would predict increases in depression and anxiety from the previous time-point, and adaptive emotion regulation would predict decreases in depression and anxiety from the previous time-point. Even though the RI-CLPM tests bidirectional within-person effects, we did not hypothesize any effects of earlier internalizing symptoms on later emotion regulation as previous longitudinal studies failed to find prospective relation between depression or anxiety symptoms and later emotion regulation (McLaughlin et al., 2011a; Niu & Snyder, 2022).
We also repeated these analyses with each emotion regulation strategy and hypothesize that depression and anxiety would be predicted by high rumination, catastrophizing, and self-blame, as well as low planning, reappraisal, and acceptance. We predicted 1) between-person effects would be stronger than within-person effects given that studies that examined internalizing symptoms and used RI‐CLPM generally found larger effect sizes for between-person compared to within-person effects (Etherson et al., 2022; Masselink et al., 2018), 2) maladaptive emotion regulation would have stronger effects than adaptive emotion regulation, because previous meta-analyses indicated that frequent use of maladaptive emotion regulation strategies is a stronger predictor of internalizing symptoms compared to infrequent use of adaptive emotion regulation strategies (Aldao et al., 2010; Schäfer et al., 2017), and 3) there would be similar effects for depression and anxiety. These hypotheses and the analysis plan were pre-registered prior to data analysis.Footnote 1,Footnote 2
Methods
Participants
A total of 154 participants were recruited in the study. Participants were 18–23 years old emerging adults (M = 20.05, SD = 1.28) who were full-time undergraduate students at Brandeis University and were fluent in English. The majority of the sample identified as women (77.3% women, 19.5% men, and 3.2% non-binary) and White (64.9% White, 27.9% Asian, 6.5% Black, 1.9% Native Hawaiian/Pacific Islander, 1.3% American Indian/Native Alaskan, and 3.9% other; 9.1% Hispanic/Latino). Participants were recruited via posts in Brandeis Facebook groups.
Procedure
A web-based study using Qualtrics was conducted for eight weeks, from April 2nd to June 27th, 2020. Emotion regulation, depression, and anxiety were measured bi-weekly at five time-points, including week 0 (T1, range April 2nd to April 26th, median April 2nd), week 2 (T2, range April 16th to May 11th, median April 17th), week 4 (T3, range April 30th to May 28th, median May 1st), week 6 (T4, range May 14th to June 22nd, median May 15th), and week 8 (T5, range May 28th to June 27th, median May 30th). Procedures were approved by the Brandeis University Institutional Review Board, and participants gave written informed consent and were compensated for their time.
Measures
Emotion Regulation
The Cognitive Emotion Regulation Questionnaire-Short (CERQ-S, Garnefski & Kraaij, 2006) was used to identify how often coping strategies are used after having experienced negative or unpleasant events, rated from 1 [almost never] to 5 [almost always]. The CERQ-S has good internal consistency, construct validity, and external validity (Garnefski & Kraaij, 2006). It consists of six conceptually distinct subscales, including three maladaptive strategies, namely Rumination (e.g., “I often think about how I feel about what I have experienced”), Catastrophizing (e.g., “I continually think how horrible the situation has been”), and Self-blame (e.g., “I feel that I am the one who is responsible for what has happened”); as well as three adaptive strategies, including Reappraisal (e.g., “I think I can learn something from the situation”), Planning (e.g., “I think about a plan of what I can do best”), and Acceptance (e.g., “I think that I have to accept that this has happened”). Each subscale contains two corresponding items, and scores of the corresponding subscales produce a composite score for maladaptive emotion regulation and adaptive emotion regulation, with each ranging from 6 to 30. Participants reported on how often they used each emotion regulation strategy after having experienced negative or unpleasant events from the beginning of the Covid-19 pandemic to the start of the study at T1, and reported on their prior two weeks at T2-T5. Cronbach’s Alpha (α) across T1-T5 ranged from 0.75-0.83 for maladaptive emotion regulation and 0.74-0.79 for adaptive emotion regulation.
Depression Symptoms
The Patient-Reported Outcomes Measurement Information System® (PROMIS®) Emotional Distress: Depression Short Form (American Psychiatric Association, 2013) is an eight-item questionnaire for depression symptoms (e.g., “I felt worthless”, “I felt that I had nothing to look forward to”, rated from 1 [never] to 5 [always], sum score range 8–40). None to slight depression corresponds to scores of 16 and less, mild corresponds to 17 to 22, moderate corresponds to 23 to 32, and severe corresponds to 33 and over. It shows good internal consistency and convergent validity (Pilkonis et al., 2011). Participants reported on their worst two weeks from the beginning of the Covid-19 pandemic to the start of the study at T1, and provided information regarding the past two weeks at T2-T5. α across T1-T5 ranged from 0.89 to 0.90.
Anxiety Symptoms
The PROMIS® Emotional Distress: Anxiety Short Form (American Psychiatric Association, 2013) is a seven-item questionnaire measure for anxiety symptoms (e.g., “I felt fearful” and “I felt anxious”, rated from 1 [never] to 5 [always], sum score range 7–35). None to slight anxiety corresponds to scores of 15 and less, mild corresponds to 16 to 19, moderate corresponds to 20 to 27, and severe corresponds to 28 and over. It shows good internal consistency and convergent validity (Pilkonis et al., 2011). Participants reported on their worst two weeks from the beginning of the Covid-19 pandemic to the start of the study at T1, and provided information regarding the past two weeks at T2–T5. α across T1–T5 ranged from 0.89 to 0.92.
Analysis Methods
The following procedures were carried out using Mplus (Muthén & Muthén, 2017). Four cases had data points that were more than three SDs away from the median on at least one measure: one case on overall adaptive emotion regulation at T3 and T4, one case on overall adaptive emotion regulation at T2 and T3, one case on overall adaptive emotion regulation at T3, and one case on overall maladaptive emotion regulation at T5. These data points were identified as outliers and excluded from analyses. We used the MLR estimator that uses all available information when there are missing data and is robust to normality given skewed distributions of some variables (see Table S1).
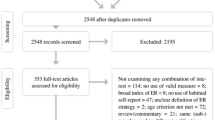
We used random intercept cross‐lagged panel models (RI‐CLPM) to decompose between-person effects that were time-invariant and within-person effects that were time-variant (Hamaker & Kuiper, 2015). As demonstrated in Fig. 1, the correlations between latent random intercepts assessed between-person associations between internalizing symptoms and emotion regulation profiles that were stable over the two-month study period (path b). The within-person effects captured how change in emotion regulation and change in internalizing symptoms are associated with one another (i.e., bidirectional within-person effects) with cross-lagged paths of mean-centered variables at each time-point (paths c1–c4) after controlling for auto-regressive effects (paths ae1–ae4 and paths ai1–ai4). However, we only had hypotheses regarding the within-person effects of emotion regulation on internalizing symptoms. We also tested residual correlations between emotion regulation and internalizing symptoms at each time point (paths r1-r5).
Diagram of Random Intercept Cross-Lagged Panel Model (RI-CLPM). Note. ISit, observed internalizing symptoms of unit i at occasion t. ERit, observed emotion regulation of unit i at occasion t. B, between-person effects. W, within-person effects. ae1–ae4, autoregressive effects of emotion regulation from a previous time-point to the next time-point. ai1–ai4, autoregressive effects of internalizing symptoms from a previous time-point to the next time-point. b, between-person correlations between emotion regulation and internalizing symptoms. c1–c4, cross-lagged effects of emotion regulation from a previous time-point on internalizing symptoms at the next time-point. r1–r5, residual correlations between emotion regulation and internalizing symptoms at each time-point. Gender was coded as a binary variable. Bidirectional arrows indicate correlations. Unidirectional arrows indicate regressions
In all analyses, we included gender as a covariate for between-person effects (path b) where we coded gender as a binary variable (− 1 = male, 1 = female). Non-binary participants were omitted from gender comparison analyses due to the small sample size (n = 5). To determine if we should constrain autoregressive effects (paths ae1-ae4 and paths ai1-ai4), cross-lagged effects (paths c1-c4), and residual correlations (paths r1–r5) to be equal across different lags, we conducted chi-square (χ2) comparisons between the fully freed models and models with each of the three parameters constrained. We freed parameters if constraining them resulted in significant chi-square difference tests than the fully freed model.
The between and within-person effects of the predictors (i.e., maladaptive emotion regulation and adaptive emotion regulation) on outcomes (i.e., depression and anxiety) were examined in 16 separate RI-CLPM models. The main analyses used the composite score of maladaptive and adaptive emotion regulation because the composite score would provide more robust measures. Specifically, model 1 tested the effects of maladaptive emotion regulation on depression. Model 2 tested the effects of maladaptive emotion regulation on anxiety. Model 3 tested the effects of adaptive emotion regulation on depression. Model 4 tested the effects of adaptive emotion regulation on anxiety. Additional analyses tested the specificity to each of the six emotion regulation subscales in terms of its link to depression and anxiety, resulting in additional 12 RI-CLPM models. In all 16 models, we tested whether the effect sizes for between-person correlations (path b) and within-person cross-lagged effects (paths c1–c4) were different between depression and anxiety using a Wald test. We also conducted Wald tests to compare overall maladaptive emotion regulation and overall adaptive emotion regulation, and to compare between-person correlations (path b) and within-person cross-lagged effects (paths c1–c4).Footnote 3
The threshold for statistical significance was set to p < 0.05, two-tailed. The two-stage sharpened method (Benjamini et al., 2006) was used to control the false discovery rate (FDR). We adjusted FDR in between-person correlations (path b), cross-lagged effects (paths c1–c4), auto-regressive effects (paths ae1–ae4 and paths ai1–ai4), and residual correlations (paths r1–r5) in each of the 16 RI-CLPM models, as well as in Wald tests comparing effect sizes of depression and anxiety, comparing overall maladaptive and adaptive emotion regulation, and comparing between-person and within-person effects. Correlations with covariates were not corrected since they were not testing hypothesized effects, and effects that were constrained equal cross paths were only corrected once since they were only estimated once. We report p-values from unstandardized results given that equality constraints apply to unstandardized estimates, but also provide standardized coefficients as measures of effect sizes.
Results
Descriptive Statistics
Of the 154 participants who completed all T1 assessments, five were omitted from modeling due to nonbinary gender status. Of the 149 participants, 88.6% completed T2 (n = 132), 82.6% completed T3 (n = 123), 77.2% completed T4 (n = 115), and 86.6% completed T5 (n = 129); 71.1% (n = 106) completed assessments of depression, anxiety, and maladaptive and adaptive emotion regulation at all time-points. Descriptive statistics of key study variables were reported in Table S1. Non-completers (M = 6.57, SD = 2.64) had significantly lower T1 acceptance compared to completers (M = 7.54, SD = 1.80, t(63.57) = − 2.28, p = 0.026). There were no significant differences between completers and non-completers in other T1 variables (Table S2). Table S3 shows bivariate correlations between study variables.
Model Fit
Model fit for models with constrained vs. unconstrained autoregressive effects, cross-lagged effects, and residuals between correlations of mean-centered variables across time-points were compared with Satorra-Bentler scaled chi-square difference tests, as required when using the MLR estimator. For the depression models with overall maladaptive, overall adaptive emotion regulation, self-blame, and reappraisal, model fit was hurt by constraining autoregressive effects across paths. For the depression model with acceptance, model fit was hurt by constraining residual correlations. For the anxiety model with planning, constraining model fit was hurt by constraining cross-lagged effects. For the anxiety model with reappraisal, model fit was hurt by constraining autoregressive effects and residual correlations. Thus, for these models, the indicated parameters were freed for the final models. For all other models, model fit was not hurt by constraining any parameters, so fully constrained models were used. See Supplemental Materials for details. Good model fit criteria for the final selected models were RMSEA ≤ 0.06, CFI ≥ 0.97, and SRMR ≤ 0.08, and acceptable criteria were RMSEA ≤ 0.08, CFI ≥ 0.95, and SRMR ≤ 0.10 (An et al., 2017; Cangur & Ercan, 2015). All final models had good to acceptable fit.
Main Analyses
Figures 2, 3, 4, 5 and Tables S4–S7 summarize the main analyses using the composite score of maladaptive and adaptive emotion regulation to predict depression and anxiety. There were significantly positive between-person correlations between maladaptive emotion regulation and both depression (r = 0.504, p < 0.001) and anxiety (r = 0.433, p < 0.001). Adaptive emotion regulation had a significant negative between-person correlation with depression (r = − 0.307, p = 0.032), but not anxiety (r = − 0.286, p = 0.110). None of the other within-person cross-lagged effects for either emotion regulation on internalizing symptoms or internalizing symptoms on emotion regulation were significant (ps > 0.8). However, there were significant positive correlations between residuals of mean-centered maladaptive emotion regulation and both depression (r = 0.131, p < 0.001) and anxiety (r = 0.150, p < 0.001). Women had significantly higher depression (r = 0.274, p < 0.001), anxiety (r = 0.284, p = 0.001), and maladaptive emotion regulation (r = 0.201, p = 0.033) compared to men.
Standardized Model Results for Maladaptive Emotion Regulation on Depression. Note. Dit, observed depression symptoms of unit i at occasion t. MEit, observed maladaptive emotion regulation of unit i at occasion t. B, between-person effects. W, within-person effects. Gender was coded as a binary variable (− 1 = male, 1 = female). Bidirectional arrows indicate correlations. Unidirectional arrows indicate regressions
Standardized Model Results for Adaptive Emotion Regulation on Depression. Note. Dit, observed depression symptoms of unit i at occasion t. AEit, observed adaptive emotion regulation of unit i at occasion t. B, between-person effects. W, within-person effects. Gender was coded as a binary variable (− 1 = male, 1 = female). Bidirectional arrows indicate correlations. Unidirectional arrows indicate regressions
Standardized Model Results for Maladaptive Emotion Regulation on Anxiety. Note. Ait, observed anxiety symptoms of unit i at occasion t. MEit, observed maladaptive emotion regulation of unit i at occasion t. B, between-person effects. W, within-person effects. Gender was coded as a binary variable (− 1 = male, 1 = female). Bidirectional arrows indicate correlations. Unidirectional arrows indicate regressions
Standardized Model Results for Adaptive Emotion Regulation on Anxiety. Note. Ait, observed anxiety symptoms of unit i at occasion t. AEit, observed adaptive emotion regulation of unit i at occasion t. B, between-person effects. W, within-person effects. Gender was coded as a binary variable (− 1 = male, 1 = female). Bidirectional arrows indicate correlations. Unidirectional arrows indicate regressions
Additional Analyses
Tables S8–S19 summarize the results of additional analyses testing the specificity of each emotion regulation subscale in terms of predicting depression and anxiety. Depression demonstrated significantly positive between-person correlations with catastrophizing (r = 0.507, p < 0.001) and self-blame (r = 0.429, p = 0.006), and a negative between-person correlation with reappraisal (r = − 0.302, p = 0.016). Anxiety demonstrated significantly positive between-person correlations with rumination (r = 0.370, p = 0.017) and catastrophizing (r = 0.559, p < 0.001), and a negative between-person correlation with reappraisal (r = − 0.356, p = 0.007). There were no significant between-person correlations between gender and any of the emotion regulation subscales (ps > 0.9). The only significant within-person cross-lagged effect was that T3 planning predicted higher T4 anxiety, controlling for T3 anxiety (β = 0.316, p = 0.035). There were significant positive correlations between residuals of mean-centered anxiety and both rumination (r = 0.104, p = 0.013) and self-blame (r = 0.148, p < 0.001). None of the other effects were significantly different between depression and anxiety (ps > 0.9).
Wald Test Statistics
For the main analyses using the composite score of maladaptive and adaptive emotion regulation to predict depression and anxiety, none of the effects were significantly different between depression and anxiety (ps > 0.6, Table S20). When we compared the absolute values of effect sizes for maladaptive emotion regulation and adaptive emotion regulation, none of the effects were significantly different (ps > 0.8, Table S21). The effect sizes for between-person correlations were statistically larger than within-person cross-lagged effects for maladaptive emotion regulation on depression [rBetween = 7.822, βwithin = 0.054, X2(1) = 23.074, p < 0.001], maladaptive emotion regulation on anxiety [rBetween = 5.491, βwithin = − 0.047, X2(1) = 13.241, p < 0.001], adaptive emotion regulation on depression [rBetween = − 4.748, βwithin = 0.072, X2(1) = 8.982, p = 0.002], and adaptive emotion regulation on anxiety [rBetween = − 3.216, βwithin = 0.109, X2(1) = 4.774, p = 0.018].
For additional analyses testing the specificity of each emotion regulation subscale in terms of predicting depression and anxiety, the between-person correlation between self-blame and depression (rDepression = 2.758) was statistically larger than the correlation between self-blame and anxiety [rAnxiety = 0.509, X2(1) = 7.759, p = 0.020]. In addition, the within-person cross-lagged effects of planning on anxiety were freed across paths and were statistically different from the effects of planning on depression (βdepression = 0.178) for T1 to T2 [βanxiety = − 0.250, X2(1) = 9.32, p = 0.011], T3 to T4 [βanxiety = 0.703, X2(1) = 14.07, p < 0.001], and T4 to T5 [βanxiety = − 0.402, X2(1) = 17.12, p < 0.001]. None of the other effects were significantly different between depression and anxiety (ps > 0.7, Table S20).
The effect sizes for between-person correlations were statistically different from within-person cross-lagged effects for rumination on depression [rBetween = 1.607, βwithin = 0.114, X2(1) = 4.331, p = 0.021], rumination on anxiety [rBetween = 1.876, βwithin = 0.124, X2(1) = 6.228, p = 0.010], catastrophizing on depression [rBetween = 3.469, βwithin = − 0.065, X2(1) = 22.862, p < 0.001], catastrophizing on anxiety [rBetween = 3.105, βwithin = − 0.183, X2(1) = 27.506, p < 0.001], self-blame on depression [rBetween = 2.758, βwithin = 0.063, X2(1) = 11.143, p < 0.001], planning on depression [rBetween = − 1.774, βwithin = 0.178, X2(1) = 10.351, p = 0.001], reappraisal on depression [rBetween=− 2.428, βwithin = 0.075, X2(1) = 10.720, p = 0.001], and reappraisal on anxiety [rBetween = − 2.104, βwithin = 0.322, X2(1) = 13.820, p < 0.001]. The within-person cross-lagged effects of planning on anxiety were freed across paths and were significantly different from the between-person effects [rBetween = − 0.752] from T2 to T3 [βwithin = 0.194, X2(1) = 2.830, p = 0.049] and from T3 to T4 [βwithin = 0.703, X2(1) = 5.934, p = 0.010]. None of the other between-person effects were significantly different from within-person effects (ps > 0.2, Table S22).
Discussion
In the current study, individual differences in internalizing symptoms and emotion regulation were associated in expected ways. Specifically, participants with higher depression symptoms had higher overall maladaptive emotion regulation, catastrophizing, and self-blame, and lower overall adaptive emotion regulation and reappraisal. Participants with higher anxiety symptoms had higher overall maladaptive emotion regulation, rumination, and catastrophizing, as well as lower reappraisal. In contrast, after accounting for these between-person individual differences, fluctuations in symptoms and in emotion regulation generally did not predict one another over time within-persons, although there were concurrent associations.
Within-Person Effects of Maladaptive and Adaptive Emotion Regulation
In line with previous studies that used RI‐CLPM in their analyses (Etherson et al., 2022; Masselink et al., 2018), we found weaker effects for within-person compared to between-person associations across various maladaptive and adaptive emotion regulation strategies in relation to depression and anxiety. Changes in overall maladaptive and adaptive emotion regulation, or the specific components of rumination, catastrophizing, self-blame, reappraisal, and acceptance, and changes in depression or anxiety symptoms do not predict one another over any two-week intervals. These findings are consistent with previous research indicating that depression and anxiety symptoms at baseline were not associated with subsequent adjustments in emotion regulation strategies (McLaughlin et al., 2011a; Niu & Snyder, 2022). However, these findings differ from prior longitudinal studies that controlled for baseline internalizing symptoms and found associations between rumination and worsened depression and anxiety symptoms (Broderick & Korteland, 2016; Butler & Nolen-Hoeksema, 1994b; Hatzenbuehler et al., 2008; Hong, 2007; Sarin et al., 2005; Whisman et al., 2020), reappraisal and improved depression symptoms (Kraaij et al., 2002; Wang et al., 2014), and acceptance and improved depression and anxiety symptoms (Cheung & Ng, 2019; Wang et al., 2014). Crucially, however, these studies did not decompose time-invariant between-person effects from time-variant within-person effects (i.e., between-person effects might be potential confounders for within-person effects) and therefore might lead to erroneous conclusions regarding within-person causal effects (Hamaker & Kuiper, 2015). Thus, the associations found in previous studies might be due to between-person individual differences as opposed to more dynamic relations between emotion regulation and internalizing symptoms.
The Covid-19 pandemic was a source of a range of novel, unpredictable, and uncontrollable stressors, such as financial and health concerns and social estrangement. The pandemic has been associated with exacerbated depression and anxiety symptoms and magnified uses of maladaptive emotion regulation strategies (Fancourt et al., 2021; Marelli et al., 2020; Pilch et al., 2021), therefore it might be expected that changes in emotion regulation in response to these new stressors would lead to within-person changes in internalizing symptom severity. Although we did not find such within-person effects in the current study, maladaptive emotion regulation and internalizing symptoms had concurrent (time-point specific) associations even after accounting for the temporally-stable individual differences, suggesting there might be within-person associations that were not captured by the cross-lagged effects. This result was potentially because causal mechanisms under which emotion regulation influences internalizing symptoms may operate on different time-frames than the two-week interval during the beginning of the Covid-19 pandemic.
Specifically, changes in emotion regulation might lead to changes in symptom severity at either shorter or longer time scales than the two-week interval in the current study. On the one hand, because emotion regulation profiles and internalizing symptoms can be relatively stable in the short term, change in emotion regulation might only contribute to change in internalizing symptoms in the long term. For example, prior longitudinal research with longer study periods (seven months to four years) might have better captured the time scale over which rumination predicted increased depression symptoms (Broderick & Korteland, 2016; Folk et al., 2014; Hatzenbuehler et al., 2008; McLaughlin et al., 2011b). On the other end of the spectrum, it is possible that the within-person effects of emotion regulation on internalizing symptoms may operate over much shorter periods. For example, daily diary (Li et al., 2017; White & Shih, 2012) and ecological momentary assessment (EMA) studies (Vanderlind et al., 2021; Zuzama et al., 2020) indicate that rumination might increase depression symptoms on the next day or even next hours. However, it is important to note that none of these studies included random intercepts to account for individual differences and accurately test within-person changes, and thus it remains unknown if within-person casual mechanisms occur over these other time scales. Still, these findings suggest that causal links between emotion regulation and internalizing symptom could occur in either long-term changes or daily fluctuations. This is one possible cause, though certainly not the only one, for the finding in the current study that at time-points over two weeks when participants had higher maladaptive emotion regulation compared to their average level they also had higher internalizing symptoms compared to their average level.
In the current study, only one cross-lagged path was significant, and this effect was in an unexpected direction. Increases in planning predicted increases in anxiety from T3 to T4, contrary to a prior study finding that planning is associated with improved anxiety symptoms over time (Vollrath et al., 1996). These results should be interpreted with caution given that this effect was specific to just one time lag. However, it is worth mentioning that T3 and T4 (median: May 1st to May 15th, 2020) were collected around the end of the spring semester. Thus, one possibility is that participants who did a lot of planning for the summer and then realized that things would not work as they planned because of the pandemic might have felt more anxious than those who did not plan ahead.
Between-Person Effects of Maladaptive Emotion Regulation
In contrast to the lack of within-person effects, maladaptive emotion regulation was robustly associated with internalizing symptoms between-persons. Consistent with our hypotheses, overall maladaptive emotion regulation was significantly and similarly associated with both depression and anxiety symptoms. There are likely multiple drivers of the association between temporally stable individual differences in using maladaptive emotion regulation and depression and anxiety symptoms. First, it is possible that maladaptive emotion regulation and internalizing symptoms do mutually influence one another, but in a way that leads to stability rather than change across the time scale assessed in the current study (a point we return to later). For example, maladaptive emotion regulation may increase internalizing symptoms via reduced cognitive control to disengage from negative materials and vice versa, producing a positive feedback loop (Joormann & Vanderlind, 2014; Joormann et al., 2010). If this feedback loop operates at a faster time scale (e.g., hours, days) than the current study (weeks), these effects would not be seen in the cross-lagged effects and instead contribute to temporal stable associations. Another possibility is that there are no causal relations between maladaptive emotion regulation and internalizing symptoms, but rather that these between-person associations are due to common causes of both maladaptive emotion regulation and internalizing psychopathology, such as cognitive impairments in working memory and sustained attention (Goretti et al., 2010; Zobeir & Jafar, 2016).
Considering individual maladaptive emotion regulation components, catastrophizing was also significantly and equally associated with both depression and anxiety symptoms, consistent with previous findings that the effect sizes of catastrophizing on symptoms were similar for depression and anxiety (Dehghanizadeh et al., 2017; Garnefski et al., 2002; Martin & Dahlen, 2005; Min et al., 2013). Rumination was also associated with higher anxiety symptoms. Although the effect sizes were similar in anxiety and depression, the association between depression and rumination was not significant, which contradicts prior research demonstrating rumination to be more strongly associated with depression than other emotion regulation strategies (Dehghanizadeh et al., 2017; Garnefski et al., 2003, 2004; Kraaij et al., 2002; Kraaij, Garnefski, de Wilde, et al., 2003). One possible explanation is that the rumination items in the current study (Garnefski & Kraaij, 2006) (e.g., “I often think about how I feel about what I have experienced”) were more related to ruminative reflection that is intentional and contemplative, rather than ruminative brooding that is passive, judgmental, and more strongly linked to depression (Treynor et al., 2003; Whitmer & Gotlib, 2011). Finally, self-blame was associated with depression symptoms. The effects of self-blame were significantly stronger for depression than anxiety, and the association between self-blame and anxiety did not reach significance, contrary to prior findings (Garnefski et al., 2002; Martin & Dahlen, 2005; Orgeta & Orrell, 2014). This is possibly because individuals who use self-blame as an emotion regulation strategy tend to interpret negative events as having internal causes, and such attributional style is a vulnerability marker for depression symptoms (Rubenstein et al., 2016; Tilghman-Osborne et al., 2008).
Between-Person Effects of Adaptive Emotion Regulation
Inconsistent with prior evidence that maladaptive emotion regulation is more strongly associated with internalizing symptoms than adaptive emotion regulation (e.g., Aldao et al., 2010), we found similar effect sizes for higher overall maladaptive emotion regulation and lower overall adaptive emotion regulation on internalizing symptoms for both between-person associations and within-person effects. It was not surprising that we found similar within-person effect sizes for maladaptive and adaptive emotion regulation because the vast majority of within-subject effects were non-significant. However, there were fewer significant between-person associations between symptoms and specific adaptive emotion regulation strategies compared to specific maladaptive emotion regulation strategies in the current study. This is potentially because there are more strategy-specific variances in adaptive than maladaptive emotion regulation, as demonstrated by weaker bivariate correlations among individual adaptive strategies than those for maladaptive strategies (Table S2). As a result, composite scores might be more beneficial for adaptive emotion regulation in providing a robust measure than for maladaptive emotion regulation, leading to similar effect sizes between overall maladaptive and adaptive emotion regulation.
Overall adaptive emotion regulation was associated with lower depression but not anxiety, even though these associations were not significantly different between depression and anxiety. Consistent with previous findings that reappraisal predicts lower depression and anxiety symptoms (Garnefski et al., 2002; Martin & Dahlen, 2005), reappraisal was similarly associated with lower depression and anxiety symptoms. Adaptive emotion regulation (specifically reappraisal) and the lack of internalizing symptoms may reinforce the stability of one another during the two-month study period, potentially via hopeful cognitions that provide positive motivational states (Peh et al., 2017; Sari et al., 2021). Another possibility is that, just like maladaptive emotion regulation, adaptive emotion regulation (specifically reappraisal) and low internalizing symptoms might be associated because they share a common cause, such as cognitive flexibility that enables better adjustments during stressful situations (Dryman & Heimberg, 2018; Esmail Soltani et al., 2013), rather than because they are causally related.
Contrary to previous findings on the association between planning and lower internalizing symptoms (Carver et al., 1989; Min et al., 2013; Priester & Clum, 1993; Siu & Shek, 2010; Vollrath et al., 1996), participants in our study who frequently used planning as an emotion regulation strategy did not have lower depression or anxiety symptoms. In addition, despite the past research indicating both positive (Cheung & Ng, 2019; Wang et al., 2014) and negative associations (Garnefski et al., 2002; Kraaij et al., 2002, 2003a, b; Martin & Dahlen, 2005) between acceptance and internalizing symptoms, we found no association between acceptance and depression or acceptance and anxiety. This result is potentially because the adaptiveness of planning and acceptance might depend on the perceived controllability of the stressor. According to the situation-fit hypothesis, it is more effective to use planning to directly modify controllable stressors and reduce negative consequences, while acceptance may be a form of passive resignation to avoid more active problem-solving processes (Compas et al., 1993; Lazarus & Folkman, 1984). In contrast, planning can result in distress and frustration when the stressor is not amenable to change, whereas acceptance provides active self-affirmation when nothing constructive could be done but the negative emotions need to be managed (Compas et al., 1993; Lazarus & Folkman, 1984). Since participants in the current study experienced both pandemic-related stressors that they had little control over (e.g., health and financial stressors) and those they had more control over (e.g., academic adjustment to online courses), the adaptiveness of these planning and acceptance may have varied across uncontrollable and controllable stressors, leading to overall null associations. Future research testing associations between planning or acceptance in response to individual stressors and internalizing symptoms would be needed to test this possibility.
Limitations and Future Directions
The current study has several limitations. First, our two-week time lag might not be the optimal time scale to reflect the within-person effects of emotion regulation on internalizing symptoms. More longitudinal studies are needed to test change processes across multiple time scales. Second, the current study only used self-report measures. Future studies with behavioral assessment of emotion regulation and structured clinical interviews of internalizing symptoms would be valuable to address potential self-report biases. Third, our sample was limited to undergraduate students at Brandeis University with the majority being women. Even after including gender as a covariate, our results may not be generalizable to other emerging adult populations. Future research would benefit from recruiting samples of emerging adults from various communities. The general null within-person findings could also be attributed to our non-clinical sample.
Next, this study examined these processes at the beginning of the CovidCovid-19 pandemic. Although this was an important period of increased internalizing psychopathology (Ettman et al., 2020; Fruehwirth et al., 2021; Niu & Snyder, 2022), it is possible that risk and protective processes during this period differed from other periods. For example, the type and intensity of stress during this period may have rendered some emotion regulation strategies more or less adaptative or available during this period. Future studies should investigate how different types of stressors may interactively affect the risk and protective mechanisms of specific emotion regulation strategies for internalizing symptoms. Lastly, the current study did not consider the influences of interpersonal emotion regulation on internalizing symptoms. Interpersonal emotion regulation is a process when individuals interact and communicate with others to either receive or provide social support in order to regulate emotional responses of themselves or others (Hofmann, 2014). Because socialization decreased as a result of quarantine and restriction measures during the pandemic, an interesting future direction of this work is to examine how specific social contexts may influence links between emotion regulation and internalizing symptoms, such as the amount of virtual versus in-person social interaction, the strategies to seek social support, and the frequency of positive versus negative communication.
Conclusions
Our findings supported the vulnerability and protective factors of maladaptive and adaptive emotion regulation on depression and anxiety symptoms in the context of the Covid-19 pandemic among emerging adults. This is one of the first studies to disentangle the time-invariant between-person effects from the time-variant within-person effects. We found that the risk and protective mechanisms of emotion regulation on internalizing symptoms might be through a temporally stable cooccurrence as opposed to a more dynamic relation, at least on this time scale.
Data Availability
Pre-registration, data, and syntax/analysis output files are available at https://osf.io/8qkfp/.
Notes
Pre-registration, data, and syntax/analysis output files are available at https://osf.io/8qkfp/.
The first additional analysis (comparing between-person and within-person effects) and second additional analysis (comparing maladaptive and adaptive emotion regulation) were not pre-registered but were added during the review process per a reviewer’s request.
We additionally preregistered testing stress controllability as a moderator for the effects of planning, reappraisal, and acceptance on depression and anxiety. However, we later learned that analyses with continuous moderators of within-person effects have not been developed for RI-CLPM models in MPlus (Orth et al., 2022). Therefore, we were unable to conduct this planned analysis.
References
Aldao, A., Nolen-Hoeksema, S., & Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. https://doi.org/10.1016/j.cpr.2009.11.004
An, M., Kusurkar, R. A., Li, L., Xiao, Y., Zheng, C., Hu, J., & Chen, M. (2017). Measurement invariance of the strength of motivation for medical school: A multi-group confirmatory factor analysis. BMC Medical Education, 17(1), 116. https://doi.org/10.1186/s12909-017-0958-4
Anderson, C. A., Miller, R. S., Riger, A. L., Dill, J. C., & Sedikides, C. (1994). Behavioral and characterological attributional styles as predictors of depression and loneliness: Review, refinement, and test. Journal of Personality and Social Psychology, 66(3), 549–558. https://doi.org/10.1037//0022-3514.66.3.549
Arlington, V. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association.
Arnett, J., Žukauskienė, R., & Sugimura, K. (2014). The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. The Lancet Psychiatry, 1, 569–576. https://doi.org/10.1016/S2215-0366(14)00080-7
Beiter, R., Nash, R., McCrady, M., Rhoades, D., Linscomb, M., Clarahan, M., & Sammut, S. (2015). The prevalence and correlates of depression, anxiety, and stress in a sample of college students. Journal of Affective Disorders, 173, 90–96. https://doi.org/10.1016/j.jad.2014.10.054
Benjamini, Y., Krieger, A. M., & Yekutieli, D. (2006). Adaptive linear step-up procedures that control the false discovery rate. Biometrika, 93(3), 491–507. https://doi.org/10.1093/biomet/93.3.491
Broderick, P. C., & Korteland, C. (2016). A prospective study of rumination and depression in early adolescence. Clinical Child Psychology and Psychiatry. https://doi.org/10.1177/1359104504043920
Butler, L. D., & Nolen-Hoeksema, S. (1994). Gender differences in responses to depressed mood in a college sample. Sex Roles: A Journal of Research, 30(5–6), 331–346. https://doi.org/10.1007/BF01420597
Calmes, C. A., & Roberts, J. E. (2007). Repetitive thought and emotional distress: Rumination and worry as prospective predictors of depressive and anxious symptomatology. Cognitive Therapy and Research, 31(3), 343–356. https://doi.org/10.1007/s10608-006-9026-9
Cangur, S., & Ercan, I. (2015). Comparison of model fit indices used in structural equation modeling under multivariate normality. Journal of Modern Applied Statistical Methods. https://doi.org/10.22237/jmasm/1430453580
Carver, C. S., Scheier, M. F., & Weintraub, J. K. (1989). Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology, 56(2), 267–283. https://doi.org/10.1037/0022-3514.56.2.267
Cheung, R. Y. M., & Ng, M. C. Y. (2019). Mindfulness and symptoms of depression and anxiety: The underlying roles of awareness, acceptance, impulse control, and emotion regulation. Mindfulness, 10(6), 1124–1135. https://doi.org/10.1007/s12671-018-1069-y
Compas, B. E., Orosan, P. G., & Grant, K. E. (1993). Adolescent stress and coping: Implications for psychopathology during adolescence. Journal of Adolescence, 16(3), 331–349. https://doi.org/10.1006/jado.1993.1028
Dehghanizadeh, Z., Gharcheh, S., Asghari, K., Shabani, H., & Eydi - Baygi, M. (2017). Relationship of Negative Strategies of Emotion Regulation with Anxiety and Depression in the Students of Shiraz University of Medical Sciences, Shiraz, Iran. Annals of Military and Health Sciences Research, 15(3), Article 3. https://doi.org/10.5812/amh.63315
Domaradzka, E., & Fajkowska, M. (2018). Cognitive emotion regulation strategies in anxiety and depression understood as types of personality. Frontiers in Psychology, 9, 856. https://doi.org/10.3389/fpsyg.2018.00856
Dryman, M. T., & Heimberg, R. G. (2018). Emotion regulation in social anxiety and depression: A systematic review of expressive suppression and cognitive reappraisal. Clinical Psychology Review, 65, 17–42. https://doi.org/10.1016/j.cpr.2018.07.004
Etherson, M. E., Smith, M. M., Hill, A. P., & Flett, G. L. (2022). Feelings of not mattering and depressive symptoms from a temporal perspective: A comparison of the cross-lagged panel model and random-intercept cross-lagged panel model. Journal of Psychoeducational Assessment, 40(1), 60–76. https://doi.org/10.1177/07342829211049686
Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9), e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Everaert, J., & Joormann, J. (2019). Emotion regulation difficulties related to depression and anxiety: A network approach to model relations among symptoms, positive reappraisal, and repetitive negative thinking. Clinical Psychological Science, 7(6), 1304–1318. https://doi.org/10.1177/2167702619859342
Fancourt, D., Steptoe, A., & Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry, 8(2), 141–149. https://doi.org/10.1016/S2215-0366(20)30482-X
Folk, J., Zeman, J., Poon, J., & Dallaire, D. (2014). A longitudinal examination of emotion regulation: Pathways to anxiety and depressive symptoms in Urban minority youth. Child and Adolescent Mental Health. https://doi.org/10.1111/camh.12058
Fruehwirth, J. C., Biswas, S., & Perreira, K. M. (2021). The Covid-19 pandemic and mental health of first-year college students: Examining the effect of Covid-19 stressors using longitudinal data. PLoS ONE, 16(3), e0247999. https://doi.org/10.1371/journal.pone.0247999
Garnefski, N., Boon, S., & Kraaij, V. (2003). Relationships between cognitive strategies of adolescents and depressive symptomatology across different types of life event. Journal of Youth and Adolescence, 32(6), 401–408. https://doi.org/10.1023/A:1025994200559
Garnefski, N., & Kraaij, V. (2006). Cognitive emotion regulation questionnaire—Development of a short 18-item version (CERQ-short). Personality and Individual Differences, 41(6), 1045–1053. https://doi.org/10.1016/j.paid.2006.04.010
Garnefski, N., Kraaij, V., & Spinhoven, P. (2001). Negative life events, cognitive emotion regulation and emotional problems. Personality and Individual Differences, 30(8), 1311–1327. https://doi.org/10.1016/S0191-8869(00)00113-6
Garnefski, N., Legerstee, J., Kraaij, V. V., Van Den Kommer, T., & Teerds, J. (2002). Cognitive coping strategies and symptoms of depression and anxiety: A comparison between adolescents and adults. Journal of Adolescence, 25(6), 603–611. https://doi.org/10.1006/jado.2002.0507
Garnefski, N., Teerds, J., Kraaij, V., Legerstee, J., & van den Kommer, T. (2004). Cognitive emotion regulation strategies and depressive symptoms: Differences between males and females. Personality and Individual Differences, 36(2), 267–276. https://doi.org/10.1016/S0191-8869(03)00083-7
Goretti, B., Portaccio, E., Zipoli, V., Razzolini, L., & Amato, M. P. (2010). Coping strategies, cognitive impairment, psychological variables and their relationship with quality of life in multiple sclerosis. Neurological Sciences, 31(2), 227–230. https://doi.org/10.1007/s10072-010-0372-8
Grabe, S., Hyde, J. S., & Lindberg, S. M. (2016). Body objectification and depression in adolescents: The role of gender. Shame, and Rumination: Psychology of Women Quarterly. https://doi.org/10.1111/j.1471-6402.2007.00350.x
Hamaker, E. L., & Kuiper, R. M. (2015). A critique of the cross-lagged panel model. Psychological Methods, 20(1), 102–116. https://doi.org/10.1037/a0038889
Hatzenbuehler, M. L., McLaughlin, K. A., & Nolen-Hoeksema, S. (2008). Emotion regulation and internalizing symptoms in a longitudinal study of sexual minority and heterosexual adolescents. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 49(12), 1270–1278. https://doi.org/10.1111/j.1469-7610.2008.01924.x
Hittner, E. F., Rim, K. L., & Haase, C. M. (2019). Socioeconomic status as a moderator of the link between reappraisal and anxiety: Laboratory-based and longitudinal evidence. Emotion, 19, 1478–1489. https://doi.org/10.1037/emo0000539
Hofmann, S. G. (2014). Interpersonal emotion regulation model of mood and anxiety disorders. Cognitive Therapy and Research, 38(5), 483–492. https://doi.org/10.1007/s10608-014-9620-1
Hong, R. Y. (2007). Worry and rumination: Differential associations with anxious and depressive symptoms and coping behavior. Behaviour Research and Therapy, 45(2), 277–290. https://doi.org/10.1016/j.brat.2006.03.006
Jamnik, M. R., & DiLalla, L. F. (2019). Health outcomes associated with internalizing problems in early childhood and adolescence. Frontiers in Psychology, 10, 60. https://doi.org/10.3389/fpsyg.2019.00060
Joormann, J., & Vanderlind, W. M. (2014). Emotion regulation in depression: The role of biased cognition and reduced cognitive control. Clinical Psychological Science, 2(4), 402–421. https://doi.org/10.1177/2167702614536163
Joormann, J., Yoon, K. L., & Siemer, M. (2010). Cognition and emotion regulation. In Emotion regulation and psychopathology: A transdiagnostic approach to etiology and treatment (pp. 174–203). The Guilford Press.
Kessler, R. C., Berglund, P., Demler, O., Jin, R., Merikangas, K. R., & Walters, E. E. (2005). Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 593–602. https://doi.org/10.1001/archpsyc.62.6.593
Kraaij, V., Garnefski, N., de Wilde, E. J., Dijkstra, A., Gebhardt, W., Maes, S., & ter Doest, L. (2003a). Negative life events and depressive symptoms in late adolescence: Bonding and cognitive coping as vulnerability factors? Journal of Youth and Adolescence, 32(3), 185–193. https://doi.org/10.1023/A:1022543419747
Kraaij, V., Garnefski, N., & Van Gerwen, L. (2003b). Cognitive coping and anxiety symptoms among people who seek help for fear of flying. Aviation, Space, and Environmental Medicine, 74(3), 273–277.
Kraaij, V., Garnefski, N., & Vlietstra, A. (2008). Cognitive coping and depressive symptoms in definitive infertility: A prospective study. Journal of Psychosomatic Obstetrics and Gynaecology, 29(1), 9–16. https://doi.org/10.1080/01674820701505889
Kraaij, V., Pruymboom, E., & Garnefski, N. (2002). Cognitive coping and depressive symptoms in the elderly: A longitudinal study. Aging & Mental Health, 6(3), 275–281. https://doi.org/10.1080/13607860220142387
Krafft, J., Haeger, J. A., & Levin, M. E. (2019). Comparing cognitive fusion and cognitive reappraisal as predictors of college student mental health. Cognitive Behaviour Therapy, 48(3), 241–252. https://doi.org/10.1080/16506073.2018.1513556
Laird, J. D. (1974). Self-attribution of emotion: The effects of expressive behavior on the quality of emotional experience. Journal of Personality and Social Psychology, 29(4), 475–486. https://doi.org/10.1037/h0036125
Lazarus, R. S., & Folkman, S. (1984). Stress, Appraisal, and Coping. Springer Publishing Company.
Li, Y. I., Starr, L. R., & Hershenberg, R. (2017). Responses to positive affect in daily life: Positive rumination and dampening moderate the association between daily events and depressive symptoms. Journal of Psychopathology and Behavioral Assessment, 39(3), 412–425. https://doi.org/10.1007/s10862-017-9593-y
Marelli, S., Castelnuovo, A., Somma, A., Castronovo, V., Mombelli, S., Bottoni, D., Leitner, C., Fossati, A., & Ferini-Strambi, L. (2020). Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology. https://doi.org/10.1007/s00415-020-10056-6
Martin, R. C., & Dahlen, E. R. (2005). Cognitive emotion regulation in the prediction of depression, anxiety, stress, and anger. Personality and Individual Differences, 39(7), 1249–1260. https://doi.org/10.1016/j.paid.2005.06.004
Masselink, M., Van Roekel, E., Hankin, B. L., Keijsers, L., Lodder, G. M. A., Vanhalst, J., Verhagen, M., Young, J. F., & Oldehinkel, A. J. (2018). The longitudinal association between self-esteem and depressive symptoms in adolescents: Separating between-person effects from within-person effects. European Journal of Personality, 32(6), 653–671. https://doi.org/10.1002/per.2179
McLaughlin, K. A., Hatzenbuehler, M. L., Mennin, D. S., & Nolen-Hoeksema, S. (2011). Emotion dysregulation and adolescent psychopathology: A prospective study. Behaviour Research and Therapy, 49(9), 544–554. https://doi.org/10.1016/j.brat.2011.06.003
Min, J.-A., Yu, J. J., Lee, C.-U., & Chae, J.-H. (2013). Cognitive emotion regulation strategies contributing to resilience in patients with depression and/or anxiety disorders. Comprehensive Psychiatry, 54(8), 1190–1197. https://doi.org/10.1016/j.comppsych.2013.05.008
Muthén, L. K., & Muthén, B. O. (2017). Mplus User’s Guide. Eighth Edition. https://www.statmodel.com/download/usersguide/MplusUserGuideVer_8.pdf
Niu, X., & Snyder, H. R. (2022). The role of maladaptive emotion regulation in the bidirectional relation between sleep and depression in college students during the COVID-19 pandemic. Anxiety, Stress, and Coping. https://doi.org/10.1080/10615806.2022.2073441
Nolen-Hoeksema, S. (2000). The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of Abnormal Psychology, 109(3), 504–511.
Orgeta, V., & Orrell, M. (2014). Coping styles for anxiety and depressive symptoms in community-dwelling older adults. Clinical Gerontologist: The Journal of Aging and Mental Health, 37(4), 406–417. https://doi.org/10.1080/07317115.2014.907590
Orth, U., Meier, L., Buehler, J. L., Dapp, L., Krauss, S., Messerli, D., & Robins, R. (2022). Effect size guidelines for cross-lagged effects. Psychological Methods.
Peh, C. X., Liu, J., Bishop, G. D., Chan, H. Y., Chua, S. M., Kua, E. H., & Mahendran, R. (2017). Emotion regulation and emotional distress: The mediating role of hope on reappraisal and anxiety/depression in newly diagnosed cancer patients. Psycho-Oncology, 26(8), 1191–1197. https://doi.org/10.1002/pon.4297
Pilch, I., Wardawy, P., & Probierz, E. (2021). The predictors of adaptive and maladaptive coping behavior during the COVID-19 pandemic: The Protection Motivation Theory and the Big Five personality traits. PLoS ONE, 16(10), 8606. https://doi.org/10.1371/journal.pone.0258606
Pilkonis, P. A., Choi, S. W., Reise, S. P., Stover, A. M., Riley, W. T., & Cella, D. (2011). Item banks for measuring emotional distress from the patient-reported outcomes measurement information system (PROMIS®): Depression, anxiety, and anger. Assessment, 18(3), 263–283. https://doi.org/10.1177/1073191111411667
Priester, M. J., & Clum, G. A. (1993). Perceived problem-solving ability as a predictor of depression, hopelessness, and suicide ideation in a college population. Journal of Counseling Psychology, 40(1), 79–85. https://doi.org/10.1037/0022-0167.40.1.79
Rubenstein, L. M., Freed, R. D., Shapero, B. G., Fauber, R. L., & Alloy, L. B. (2016). Cognitive attributions in depression: Bridging the gap between research and clinical practice. Journal of Psychotherapy Integration, 26(2), 103–115. https://doi.org/10.1037/int0000030
Sari, S. P., Agustin, M., Wijayanti, D. Y., Sarjana, W., Afrikhah, U., & Choe, K. (2021). Mediating effect of hope on the relationship between depression and recovery in Persons with schizophrenia. Frontiers in Psychiatry. https://doi.org/10.3389/fpsyt.2021.627588
Sarin, S., Abela, J., & Auerbach, R. (2005). The response styles theory of depression: A test of specificity and causal mediation. Cognition and Emotion, 19(5), 751–761. https://doi.org/10.1080/02699930441000463
Schäfer, J. Ö., Naumann, E., Holmes, E. A., Tuschen-Caffier, B., & Samson, A. C. (2017). Emotion regulation strategies in depressive and anxiety symptoms in youth: A meta-analytic review. Journal of Youth and Adolescence, 46(2), 261–276. https://doi.org/10.1007/s10964-016-0585-0
Soltani, E., Shareh, H., Bahrainian, S. A., & Farmani, A. (2013). The mediating role of cognitive flexibility in correlation of coping styles and resilience with depression. Pajoohandeh Journal, 18(2), 88–96.
Siu, A. M. H., & Shek, D. T. L. (2010). Social problem solving as a predictor of well-being in adolescents and young adults. Social Indicators Research, 95(3), 393–406. https://doi.org/10.1007/s11205-009-9527-5
Sullivan, M. J. L., Bishop, S. R., & Pivik, J. (1995). The Pain Catastrophizing Scale: Development and validation. Psychological Assessment, 7(4), 524–532. https://doi.org/10.1037/1040-3590.7.4.524
Taylor, M. M., Wicks, J. J., Fassett-Carman, A. N., & Snyder, H. R. (in press). Differences in depression, anxiety, and coping in emerging adults prior to vs. During the COVID-19 pandemic.
Tilghman-Osborne, C., Cole, D. A., Felton, J. W., & Ciesla, J. A. (2008). Relation of guilt, shame, behavioral and characterological self-blame to depressive symptoms in adolescents over time. Journal of Social and Clinical Psychology, 27(8), 809–842. https://doi.org/10.1521/jscp.2008.27.8.809
Treynor, W., Gonzalez, R., & Nolen-Hoeksema, S. (2003). Rumination reconsidered: A psychometric analysis. Cognitive Therapy and Research, 27(3), 247–259. https://doi.org/10.1023/A:1023910315561
Vanderlind, W. M., Everaert, J., & Joormann, J. (2021). Positive emotion in daily life: Emotion regulation and depression. Emotion, No Pagination Specified-No Pagination Specified. https://doi.org/10.1037/emo0000944
Vollrath, M., Alnaes, R., & Torgersen, S. (1996). Differential effects of coping in mental disorders: A prospective study in psychiatric outpatients. Journal of Clinical Psychology, 52(2), 125–135. https://doi.org/10.1002/(SICI)1097-4679(199603)52:2%3c125::AID-JCLP2%3e3.0.CO;2-T
Wang, Y., Yi, J., He, J., Chen, G., Li, L., Yang, Y., & Zhu, X. (2014). Cognitive emotion regulation strategies as predictors of depressive symptoms in women newly diagnosed with breast cancer. Psycho-Oncology, 23(1), 93–99. https://doi.org/10.1002/pon.3376
Watkins, E. R., & Roberts, H. (2020). Reflecting on rumination: Consequences, causes, mechanisms and treatment of rumination. Behaviour Research and Therapy, 127, 103573. https://doi.org/10.1016/j.brat.2020.103573
Whisman, M. A., du Pont, A., & Butterworth, P. (2020). Longitudinal associations between rumination and depressive symptoms in a probability sample of adults. Journal of Affective Disorders, 260, 680–686. https://doi.org/10.1016/j.jad.2019.09.035
White, M. E., & Shih, J. H. (2012). A daily diary study of co-rumination, stressful life events, and depressed mood in late adolescents. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 41(5), 598–610. https://doi.org/10.1080/15374416.2012.706518
Whitmer, A., & Gotlib, I. H. (2011). Brooding and reflection reconsidered: A factor analytic examination of rumination in currently depressed, formerly depressed, and never depressed individuals. Cognitive Therapy and Research, 35(2), 99–107. https://doi.org/10.1007/s10608-011-9361-3
Xu, C., Xu, Y., Xu, S., Zhang, Q., Liu, X., Shao, Y., Xu, X., Peng, L., & Li, M. (2020). Cognitive reappraisal and the association between perceived stress and anxiety symptoms in COVID-19 isolated people. Frontiers in Psychiatry, 11, 858. https://doi.org/10.3389/fpsyt.2020.00858
Zobeir, S., & Jafar, H. (2016).The Effectiveness Of Emotional Working Memory Training In Cognitive Emotion Regulation Strategies Of Adolescents With Post-Traumatic Stress Disorder. 6(23), 113–132.
Zuzama, N., Fiol-Veny, A., Roman-Juan, J., & Balle, M. (2020). Emotion regulation style and daily rumination: potential mediators between affect and both depression and anxiety during adolescence. International Journal of Environmental Research and Public Health, 17(18), E6614. https://doi.org/10.3390/ijerph17186614
Funding
We thank the Theodore and Jane Norman Fund for supporting Faculty Research at Brandeis University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Xinran Niu, Morgan M. Taylor, Jennifer J. Wicks, Alyssa N. Fassett-Carman, Amelia D. Moser, Chiara Neilson, Elena C. Peterson, Roselinde H. Kaiser, and Hannah R. Snyder declare that they have no conflict of interest.
Human and Animal Rights
The study involved survey-based research on human participants. Procedures and all questionnaires were approved by the Brandeis University Institutional Review Board. No animal studies were carried out by the authors for this article.
Informed Consent
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Niu, X., Taylor, M.M., Wicks, J.J. et al. Longitudinal Relations Between Emotion Regulation and Internalizing Symptoms in Emerging Adults During the Covid-19 Pandemic. Cogn Ther Res 47, 350–366 (2023). https://doi.org/10.1007/s10608-023-10366-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10608-023-10366-9