Abstract
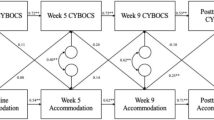
Family accommodation (FA) involves the actions taken by family members, particularly parents, to accommodate a child´s obsessive–compulsive disorder (OCD) symptoms, reducing distress or impairment. This behavior may maintain compulsive and avoidant behavior, preventing corrective learning or habituation. This study aims to investigate the prevalence and factors influencing FA in a large Scandinavian sample of children with OCD. We assessed 238 children using standardized diagnostic interviews, OCD symptom severity assessments and questionnaires evaluating functional impairment and internalizing and externalizing symptoms. FA was measured using the Family Accommodation Scale, a 12-item clinician-rated interview. Our results confirmed a high frequency of accommodation, with approximately 70% of primary caregivers reporting some accommodation daily and 98% at least once per week. FA was associated with increased OCD symptom severity, contamination/cleaning symptoms, internalizing and externalizing behavior, and functional impairment. Linear regression analysis showed that high levels of FA are specifically associated with lower age, higher OCD symptom severity, parent-reported impairment, internalizing, and externalizing symptoms. A path analysis revealed that FA partially mediated the relationship between OCD severity, externalizing symptoms, and child’s age, highlighting the role of FA in the progression of OCD and related symptoms. The findings emphasize the importance of evaluating FA before initiating treatment and specifically addressing it during the therapeutic process.

Similar content being viewed by others
Data Availability
Ethical committees do not accept the transfer of data outside of EEA.
References
Achenbach TM (1994) Child Behavior Checklist and related instruments. In: Maruish ME (eds) The Use of Psychological Testing for Treatment Planning and Outcome Assessment. Lawrence Erlbaum Associates, Hillsdale, NJ
Achenbach TM, Rescorla LA (2001) Manual for the ASEBA School-Age Forms & Profiles. University of Vermont, Research Center for Children, Youth, and Families, Burlington, VT
Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D (2010) Family accommodation in obsessive-compulsive disorder: Relation to symptom dimensions, clinical and family characteristics. Psychiatry Res 179:204–211
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Publishing, Arlington
Barbeau K, Boileau K, Sarr F, Smith K (2019) Path analysis in Mplus: a tutorial using a conceptual model of psychological and behavioral antecedents of bulimic symptoms in young adults. Quant Methods Psychol 15:38–53
Bipeta R, Yerramilli SSRR, Pingali S, Karredla AR, Ali MO (2013) A cross-sectional study of insight and family accommodation in pediatric obsessive-compulsive disorder. Child Adolesc Psychiatry Ment Health 7:20
Calvocoressi L, Mazure CM, Kasl SV, Skolnick J, Fisk D, Vegso SJ, Van Noppen BL, Price LH (1999) Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family behavior. J Nerv Mental Dis 187:636–642
Caporino NE, Morgan J, Beckstead J, Phares V, Murphy TK, Storch EA (2012) A structural equation analysis of family accommodation in pediatric obsessive-compulsive disorder. J Abnorm Child Psychol 40:133–143
Douglass HM, Moffitt TE, Dar R, McGee R, Silva P (1995) Obsessive-compulsive disorder in a birth cohort of 18-year-olds: prevalence and predictors. J Am Acad Child Adolesc Psychiatry 34:1424–1431
Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, Sceery W, Shaffer D (1988) Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry 27:764–771
Flessner CA, Freeman JB, Sapyta J, Garcia A, Franklin ME, March JS, Foa E (2011) Predictors of parental accommodation in pediatric obsessive-compulsive disorder: findings from the Pediatric Obsessive-Compulsive Disorder Treatment Study (POTS) trial. J Am Acad Child Adolesc Psychiatry 50:716–725
Francazio SK, Flessner CA, Boisseau CL, Sibrava NJ, Mancebo MC, Eisen JL, Rasmussen SA (2016) Parental accommodation predicts symptom severity at long-term follow-up in children with obsessive-compulsive disorder: a preliminary investigation. J Child Fam Stud 25:2562–2570
Garcia AM, Sapyta JJ, Moore PS, Freeman JB, Franklin ME, March JS, Foa EB (2010) Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I). J Am Acad Child and Adolesc Psychiatry 49:1024–1033
Geffken GR, Storch EA, Duke DC, Monaco L, Lewin AB, Goodman WK (2006) Hope and coping in family members of patients with obsessive-compulsive disorder. J Anxiety Disord 20:614–629
Geller D, March J (2012) Practice parameter for the assessment and treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 51:98–113
Gorenstein G, Gorenstein C, de Oliveira MC, Asbahr F, Shavitt R (2015) Child-focused treatment of pediatric OCD affects parental behavior and family environment. Psychiatry Res 229:161–166
Griffiths DL, Farrell LJ, Waters AM, White SW (2017) Clinical correlates of obsessive compulsive disorder and comorbid autism spectrum disorder in youth. J Obsessive-Compuls Relat Dis 14:90–98
Guzick AG, Geller DA, Small BJ, Murphy TK, Wilhelm S, Storch EA (2021) Irritability in children and adolescents with OCD. Behav Ther 52:883–896
Heyman I, Fombonne E, Simmons H, Ford T, Meltzer H, Goodman R (2003) Prevalence of obsessive-compulsive disorder in the British nationwide survey of child mental health. Int Rev Psychiatry 15:178–184
Hojgaard DRMA, Mortensen EL, Ivarsson T, Hybel K, Skarphedinsson G, Nissen JB, Valderhaug R, Dahl K, Weidle B, Torp NC, Grados M, Lewin AB, Melin KH, Storch EA, Wolters LH, Murphy TK, Sonuga-Barke EJS, Thomsen PH (2017) Structure and clinical correlates of obsessive-compulsive symptoms in a large sample of children and adolescents: a factor analytic study across five nations. Eur Child Adolesc Psychiatry 26:281–291
Ivarsson T, Melin K, Wallin L (2008) Categorical and dimensional aspects of co-morbidity in obsessive-compulsive disorder (OCD). Eur Child Adolesc Psychiatry 17:20–31
Ivarsson T, Skarphedinsson G, Kornør H, Axelsdottir B, Biedilæ S, Heyman I, Asbahr F, Thomsen PH, Fineberg N, March J, Accreditation TFOTCIFOCD (2015) The place of and evidence for serotonin reuptake inhibitors (SRIs) for obsessive compulsive disorder (OCD) in children and adolescents: views based on a systematic review and meta-analysis. Psychiatry Res 227:93–103
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988
Kraemer HC, Morgan GA, Leech NL, Gliner JA, Vaske JJ, Harmon RJ (2003) Measures of clinical significance. J Am Acad Child Adolesc Psychiatry 42:1524–1529
Kragh K, Husby M, Melin K, Weidle B, Torp NC, Højgaard DRMA, Hybel KA, Nissen JB, Thomsen PH, Skarphedinsson G (2019) Convergent and divergent validity of the schedule for affective disorders and schizophrenia for school-age children - present and lifetime version diagnoses in a sample of children and adolescents with obsessive-compulsive disorder. Nord J Psychiatry 73(2):111–117
Krebs G, Bolhuis K, Heyman I, Mataix-Cols D, Turner C, Stringaris A (2013) Temper outbursts in paediatric obsessive-compulsive disorder and their association with depressed mood and treatment outcome. J Child Psychol Psychiatry 54:313–322
Lauth B, Arnkelsson GB, Magnusson P, Skarphedinsson G, Ferrari P, Petursson H (2010) Validity of K-SADS-PL (schedule for affective disorders and schizophrenia for school-age children-present and lifetime version) depression diagnoses in an adolescent clinical population. Nord J Psychiatry 64:409–420
Lavell CH, Farrell LJ, Waters AM, Cadman J (2016) Predictors of treatment response to group cognitive behavioural therapy for pediatric obsessive-compulsive disorder. Psychiatry Res 245:186–193
Lebowitz ER, Panza KE, Su J, Bloch MH (2012) Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother 12:229–238
Lebowitz ER, Omer H, Leckman JF (2011) Coercive and disruptive behaviors in pediatric obsessive-compulsive disorder. Depress Anxiety 28:899–905
Lebowitz ER, Storch EA, MacLeod J, Leckman JF (2015) Clinical and family correlates of coercive-disruptive behavior in children and adolescents with obsessive-compulsive disorder. J Child Fam Stud 24:2589–2597
Lebowitz ER, Shimshoni Y (2018) The SPACE program, a parent-based treatment for childhood and adolescent OCD: the case of Jasmine. Bull Menninger Clin 82:266–287
Lewin AB, Bergman RL, Peris TS, Chang S, McCracken JT, Piacentini J (2010) Correlates of insight among youth with obsessive-compulsive disorder. J Child Psychol Psychiatry 51:603–611
McGuire JF, Small BJ, Lewin AB, Murphy TK, De Nadai AS, Phares V, Geffken G, Storch EA (2013) Dysregulation in pediatric obsessive compulsive disorder. Psychiatry Res 209:589–595
Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA (2009) Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. J Consult Clin Psychol 77:355–360
Monzani B, Vidal-Ribas P, Turner C, Krebs G, Stokes C, Heyman I, Mataix-Cols D, Stringaris A (2020) The role of paternal accommodation of paediatric OCD symptoms: patterns and implications for treatment outcomes. J Abnorm Child Psychol 48:1313–1323
Muthén LK, Muthén BO (2018) Mplus user’s guide. Muthén & Muthén, Los Angeles: CA
National Institute for Health and Clinical Excellence (2005) Obsessive compulsive disorder (OCD) and body dysmorphic disorder (BDD).
O’Connor EE, Carper MM, Schiavone E, Franklin M, Sapyta J, Garcia AM, Freeman JB (2023) Trajectory of change in parental accommodation and its relation to symptom severity and impairment in pediatric OCD. Child Psychiatry Hum Dev 54:232–240
Ost L-G, Riise EN, Wergeland GJ, Hansen B, Kvale G (2016) Cognitive behavioral and pharmacological treatments of OCD in children: a systematic review and meta-analysis. J Anxiety Disord 43:58–69
Patterson GR (2002) The early development of coercive family process. In: (ed) Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. American Psychological Association, Washington
Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J (2008) Correlates of accommodation of pediatric obsessive-compulsive disorder: parent, child, and family characteristics. J Am Acad Child Adolesc Psychiatry 47:1173–1181
Piacentini J, Bergman RL, Chang S, Langley A, Peris T, Wood JJ, McCracken J (2011) Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 50:1149–1161
Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M (2007) sFunctional impairment in childhood OCD: development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale-Revised (COIS-R). J Clin Child Adolesc Psychol 36:645–653
Pinto A, Van Noppen B, Calvocoressi L (2013) Development and preliminary psychometric evaluation of a self-rated version of the family accommodation scale for obsessive-compulsive disorder. J Obsessive Compuls Relat Disord 2:457–465
Pontillo M, Demaria F, Tata MC, Averna R, Gargiullo P, Pucciarini ML, Santonastaso O, Boldrini T, Tozzi AE, Vicari S (2020) Clinical significance of family accommodation and parental psychological distress in a sample of children and adolescents with obsessive-compulsive disorder aged 8–17 years old. Ital J Pediatr 46:167
POTS Study Team (2004) Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA 292:1969–1976
Riise EN, Kvale G, Öst LG, Skjold SH, Hansen B (2019) Does family accommodation predict outcome of concentrated exposure and response prevention for adolescents. Child Psychiatry Hum Dev 50:975–986
Rosa-Alcázar Á, Rosa-Alcázar AI, Parada-Navas JL, Olivares-Olivares PJ, Rosa-Alcázar E (2021) Predictors of parental accommodation and response treatment in young children with obsessive-compulsive disorder. Front Psychiatry 12:737062
Rudy BM, Lewin AB, Geffken GR, Murphy TK, Storch EA (2014) Predictors of treatment response to intensive cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. Psychiatry Res 220:433–440
Russell AJ, Jassi A, Fullana MA, Mack H, Johnston K, Heyman I, Murphy DG, Mataix-Cols D (2013) Cognitive behavior therapy for comorbid obsessive-compulsive disorder in high-functioning autism spectrum disorders: a randomized controlled trial. Depress Anxiety 30:697–708
Scahill L, Riddle MA, McSwiggin-Hardin M, Ort SI, King RA, Goodman WK, Cicchetti D, Leckman JF (1997) Children’s Yale-brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852
Selles RR, Hojgaard DRMA, Ivarsson T, Thomsen PH, McBride N, Storch EA, Geller D, Wilhelm S, Farrell LJ, Waters AM, Mathieu S, Lebowitz E, Elgie M, Soreni N, Stewart SE (2018) Symptom insight in pediatric obsessive-compulsive disorder: outcomes of an international aggregated cross-sectional sample. J Am Acad Child Adolesc Psychiatry 57:615-619.e5
Sharma E, Sharma LP, Balachander S, Lin B, Manohar H, Khanna P, Lu C, Garg K, Thomas TL, Au ACL, Selles RR, Højgaard DRMA, Skarphedinsson G, Stewart SE (2021) Comorbidities in obsessive-compulsive disorder across the lifespan: a systematic review and meta-analysis. Front Psychiatry 12:703701
Skarphedinsson G, Hanssen-Bauer K, Kornør H, Heiervang ER, Landrø NI, Axelsdottir B, Biedilæ S, Ivarsson T (2015) Standard individual cognitive behaviour therapy for paediatric obsessive-compulsive disorder: a systematic review of effect estimates across comparisons. Nord J Psychiatry 69:81–92
Skarphedinsson G, Weidle B, Thomsen PH, Dahl K, Torp NC, Nissen JB, Melin KH, Hybel K, Valderhaug R, Wentzel-Larsen T, Compton SN, Ivarsson T (2015) Continued cognitive-behavior therapy versus sertraline for children and adolescents with obsessive-compulsive disorder that were non-responders to cognitive-behavior therapy: a randomized controlled trial. Eur Child Adolesc Psychiatry 24:591–602
Skarphedinsson G, Melin KH, Valderhaug R, Wentzel-Larsen T, Højgaard DRMA, Thomsen PH, Ivarsson T (2015) Evaluation of the factor structure of the child obsessive-compulsive impact scale—revised (COIS-R) in Scandinavia with confirmatory factor analysis. J Obsess-Compuls Relat Disorders 7:65–72
Skoog G, Skoog I (1999) A 40-year follow-up of patients with obsessive-compulsive disorder [see commetns]. Arch Gen Psychiatry 56:121–127
Socialstyrelsen (2017) Nationella riktlinjer för vård vid depression och ångestsyndrom: Stöd för styrning och ledning [The Swedish National Clinical Guidelines for anxiety- and affective disorders: Support for management and administration]. Socialstyrelsen, Stockholm
Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, Faraone SV (2004) Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr Scand 110:4–13
Stewart SE, Beresin C, Haddad S, Egan Stack D, Fama J, Jenike M (2008) Predictors of family accommodation in obsessive-compulsive disorder. Ann Clin Psychiatry 20:65–70
Storch EA, De Nadai AS, Jacob ML, Lewin AB, Muroff J, Eisen J, Abramowitz JS, Geller DA, Murphy TK (2014) Phenomenology and correlates of insight in pediatric obsessive-compulsive disorder. Compr Psychiatry 55:613–620
Storch EA, Lewin AB, Geffken GR, Morgan JR, Murphy TK (2010) The role of comorbid disruptive behavior in the clinical expression of pediatric obsessive-compulsive disorder. Behav Res Ther 48:1204–1210
Storch EA, Lewin AB, Larson MJ, Geffken GR, Murphy TK, Geller DA (2012) Depression in youth with obsessive-compulsive disorder: clinical phenomenology and correlates. Psychiatry Res 196:83–89
Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, Larson MJ, Fernandez M, Grabill K (2007) Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol 36:207–216
Storch EA, Jones AM, Lack CW, Ale CM, Sulkowski ML, Lewin AB, De Nadai AS, Murphy TK (2012) Rage attacks in pediatric obsessive-compulsive disorder: phenomenology and clinical correlates. J Am Acad Child Adolesc Psychiatry 51:582–592
Storch EA, Lehmkuhl H, Pence SL, Geffken GR, Ricketts E, Storch JF, Murphy TK (2009) Parental experiences of having a child with obsessive-compulsive disorder: associations with clinical characteristics and caregiver adjustment. J Child Fam Stud 18:249–258
Storch EA, Milsom VA, Merlo LJ, Larson M, Geffken GR, Jacob ML, Murphy TK, Goodman WK (2008) Insight in pediatric obsessive-compulsive disorder: associations with clinical presentation. Psychiatry Res 160:212–220
Thompson-Hollands J, Kerns CE, Pincus DB, Comer JS (2014) Parental accommodation of child anxiety and related symptoms: range, impact, and correlates. J Anxiety Disord 28:765–773
Thomsen PH, Torp NC, Dahl K, Christensen K, Englyst I, Melin KH, Nissen JB, Hybel KA, Valderhaug R, Weidle B, Skarphedinsson G, von Bahr PL, Ivarsson T (2013) The nordic long-term OCD treatment study (NordLOTS): rationale, design, and methods. Child Adolesc Psychiatry Ment Health 7:41
Torp NC, Dahl K, Skarphedinsson G, Compton S, Thomsen PH, Weidle B, Hybel K, Valderhaug R, Melin K, Nissen JB, Ivarsson T (2015) Predictors associated with improved cognitive-behavioral therapy outcome in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 54:200-207.e1
Torp NC, Dahl K, Skarphedinsson G, Thomsen PH, Valderhaug R, Weidle B, Melin KH, Hybel K, Nissen JB, Lenhard F, Wentzel-Larsen T, Franklin ME, Ivarsson T (2015) Effectiveness of cognitive behavior treatment for pediatric obsessive-compulsive disorder: acute outcomes from the Nordic Long-term OCD Treatment Study (NordLOTS). Behav Res Ther 64:15–23
Watson P, Clarkin J, Lomax C (2021) What are the predictors of family accommodation of obsessive-compulsive behaviours in adults and youth with obsessive-compulsive disorder and their relatives? A systematic review. J Obsess-Compuls and Relat Dis 31:100681
Weidle B, Jozefiak T, Ivarsson T, Thomsen PH (2014) Quality of life in children with OCD with and without comorbidity. Health Qual Life Outcomes 12:152
Wu MS, Geller DA, Schneider SC, Small BJ, Murphy TK, Wilhelm S, Storch EA (2019) Comorbid psychopathology and the clinical profile of family accommodation in pediatric OCD. Child Psychiatry & Human Develop 50(5):717–726
Wu MS, Lewin AB, Murphy TK, Geffken GR, Storch EA (2014) Phenomenological considerations of family accommodation: related clinical characteristics and family factors in pediatric obsessive–compulsive disorder. J Obsess-Compuls Relat Dis 3:228–235
Wu MS, McGuire JF, Martino C, Phares V, Selles RR, Storch EA (2016) A meta-analysis of family accommodation and OCD symptom severity. Clin Psychol Rev 45:34–44
Zaboski BA, Gilbert A, Hamblin R, Andrews J, Ramos A, Nadeau JM, Storch EA (2019) Quality of life in children and adolescents with obsessive-compulsive disorder: the pediatric quality of life enjoyment and satisfaction questionnaire (PQ-LES-Q). Bull Menninger Clin 83:377–397
Funding
The Stiftelsen Clas Groschinskys Minnesfond Agreement concerning the research and education of doctors in Region Västra Götaland, TrygFonden, The Lundbeck Foundation, Central Region Denmark’s Research Fund, The Danish Council for Strategic Research, the Center for Child and Adolescent Mental Health, Eastern and Southern Norway (RBUP), the Norwegian Research Council, and the Norwegian Extra Foundation supported the research presented in this article through project grants. The funding source had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
All authors (GS, NCT, BW, SJ, TI, KH, JBN, PHT, DRMAH) contributed to the conception and design of the study or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content, approving the final version for publication, and agreement to be accountable for that all aspects of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
All authors have reported no biomedical financial interests or potential conflicts of interest.
Ethical approval
The trial was approved by the Norwegian, Swedish and Danish Committees for Medical and Health Research Ethics and the Medical Products Agencies.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Skarphedinsson, G., Torp, N.C., Weidle, B. et al. Family Accommodation in Pediatric Obsessive–Compulsive Disorder: Investigating Prevalence and Clinical Correlates in the NordLOTS Study. Child Psychiatry Hum Dev (2023). https://doi.org/10.1007/s10578-023-01602-0
Accepted:
Published:
DOI: https://doi.org/10.1007/s10578-023-01602-0