Abstract
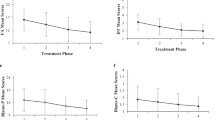
Family accommodation (FA) has been shown to relate to poorer treatment outcomes in pediatric obsessive compulsive disorder (OCD), yet few studies have examined the trajectory of change in FA throughout treatment and its relation to treatment outcomes. This study examined change in FA in relation to change in symptom severity and impairment in 63 youth receiving a family-based intervention for early-onset OCD. FA, symptom severity and functional impairment were assessed at baseline, week 5, week 9, and post-treatment (week 14). Results suggested that changes in FA in the beginning stages of treatment preceded global symptom improvement (but not OCD specific improvement) whereas changes in functional impairment preceded changes in FA. In the latter half of treatment, changes in FA preceded improvement in global and OCD specific symptom severity as well as functional impairment. These findings highlight the importance of reducing FA, especially in the later stages of treatment, in order to optimize treatment outcomes in early-onset OCD.



Similar content being viewed by others
References
Freeman J, Benito K, Herren J et al (2018) Evidence base update of psychosocial treatments for pediatric obsessive-compulsive disorder: evaluating, improving, and transporting what works. J Clin Child Adolesc Psychol 47:669–698. https://doi.org/10.1080/15374416.2018.1496443
Mancebo MC, Boisseau CL, Garnaat SL et al (2014) Long-term course of pediatric obsessive-compulsive disorder: 3 years of prospective follow-up. Compr Psychiatry 55:1498–1504. https://doi.org/10.1016/j.comppsych.2014.04.010
Stewart SE, Hu Y-P, Leung A et al (2017) A multisite study of family functioning impairment in pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 56:241-249.e3. https://doi.org/10.1016/j.jaac.2016.12.012
Ezpeleta L, Keeler G, Alaatin E et al (2001) Epidemiology of psychiatric disability in childhood and adolescence. J Child Psychol Psychiatry 42:901–914. https://doi.org/10.1111/1469-7610.00786
Hofer PD, Wahl K, Meyer AH et al (2018) Obsessive–compulsive disorder and the risk of subsequent mental disorders: a community study of adolescents and young adults. Depress Anxiety 35:339–345. https://doi.org/10.1002/da.22733
Thomsen PH, Mikkelsen HU (1995) Course of obsessive-compulsive disorder in children and adolescents: a prospective follow-up study of 23 Danish cases. J Am Acad Child Adolesc Psychiatry 34:1432–1440. https://doi.org/10.1097/00004583-199511000-00009
Franklin ME, Sapyta J, Freeman JB et al (2011) Cognitive behavior therapy augmentation of pharmacotherapy in pediatric obsessive-compulsive disorder: the Pediatric OCD Treatment Study II (POTS II) randomized controlled trial. JAMA 306:1224–1232. https://doi.org/10.1001/jama.2011.1344
Pediatric OCD Treatment Study (POTS) Team (2004) Cognitive-behavior therapy, sertraline, and their combination for children and adolescents with obsessive-compulsive disorder: the Pediatric OCD Treatment Study (POTS) randomized controlled trial. JAMA 292:1969–1976. https://doi.org/10.1001/jama.292.16.1969
Comer JS, Furr JM, Kerns CE et al (2017) Internet-delivered, family-based treatment for early-onset OCD: a pilot randomized trial. J Consult Clin Psychol 85:178–186. https://doi.org/10.1037/ccp0000155
Freeman J, Sapyta J, Garcia A et al (2014) Family-based treatment of early childhood obsessive-compulsive disorder: the Pediatric Obsessive-Compulsive Disorder Treatment Study for Young Children (POTS Jr)—a randomized clinical trial. JAMA Psychiat 71:689–698. https://doi.org/10.1001/jamapsychiatry.2014.170
Lewin AB, Park JM, Jones AM et al (2014) Family-based exposure and response prevention therapy for preschool-aged children with obsessive-compulsive disorder: a pilot randomized controlled trial. Behav Res Ther 56:30–38. https://doi.org/10.1016/j.brat.2014.02.001
Storch EA, Geffken GR, Merlo LJ, Mann G, Duke D, Munson M et al (2007) Family-based cognitive-behavioral therapy for pediatric obsessive-compulsive disorder: comparison of intensive and weekly approaches. J Am Acad Child Adolesc Psychiatry 46(4):469–478. https://doi.org/10.1097/chi.0b013e31803062e7
Peris TS, Rozenman MS, Sugar CA et al (2017) Targeted family intervention for complex cases of pediatric obsessive-compulsive disorder: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 56:1034–1042. https://doi.org/10.1016/j.jaac.2017.10.008
Freeman J, Garcia A, Benito K et al (2012) The pediatric obsessive compulsive disorder treatment study for young children (POTS Jr): developmental considerations in the rationale, design, and methods. J Obsessive-Compuls Relat Disord 1:294–300. https://doi.org/10.1016/j.jocrd.2012.07.010
Calvocoressi L, Lewis B, Harris M et al (1995) Family accommodation in obsessive-compulsive disorder. Am J Psychiatry 152:441–443. https://doi.org/10.1176/ajp.152.3.441
Flessner CA, Freeman JB, Sapyta J et al (2011) Predictors of parental accommodation in pediatric obsessive-compulsive disorder: findings from the Pediatric Obsessive-Compulsive Disorder Treatment Study (POTS) trial. J Am Acad Child Adolesc Psychiatry 50:716–725. https://doi.org/10.1016/j.jaac.2011.03.019
Lebowitz ER, Scharfstein LA, Jones J (2014) Comparing family accommodation in pediatric obsessive-compulsive disorder, anxiety disorders, and nonanxious children. Depress Anxiety 31:1018–1025. https://doi.org/10.1002/da.22251
Lebowitz ER, Panza KE, Su J, Bloch MH (2012) Family accommodation in obsessive-compulsive disorder. Expert Rev Neurother 12:229–238. https://doi.org/10.1586/ern.11.200
Wu MS, McGuire JF, Martino C et al (2016) A meta-analysis of family accommodation and OCD symptom severity. Clin Psychol Rev 45:34–44. https://doi.org/10.1016/j.cpr.2016.03.003
Garcia AM, Sapyta JJ, Moore PS et al (2010) Predictors and moderators of treatment outcome in the Pediatric Obsessive Compulsive Treatment Study (POTS I). J Am Acad Child Adolesc Psychiatry 49:1024–1033. https://doi.org/10.1016/j.jaac.2010.06.013
Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA (2009) Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. J Consult Clin Psychol 77:355–360. https://doi.org/10.1037/a0012652
Peris TS, Bergman RL, Langley A et al (2008) Correlates of accommodation of pediatric obsessive-compulsive disorder: parent, child, and family characteristics. J Am Acad Child Adolesc Psychiatry 47:1173–1181. https://doi.org/10.1097/CHI.0b013e3181825a91
Storch EA, Larson MJ, Muroff J et al (2010) Predictors of functional impairment in pediatric obsessive-compulsive disorder. J Anxiety Disord 24:275–283. https://doi.org/10.1016/j.janxdis.2009.12.004
Benito KG, Machan J, Freeman JB et al (2018) Measuring fear change within exposures: functionally-defined habituation predicts outcome in three randomized controlled trials for pediatric OCD. J Consult Clin Psychol 86:615–630. https://doi.org/10.1037/ccp0000315
Benito KG, Walther M (2015) Therapeutic process during exposure: habituation model. J Obsessive-Compuls Relat Disord 6:147–157. https://doi.org/10.1016/j.jocrd.2015.01.006
Foa EB, Kozak MJ (1986) Emotional processing of fear: exposure to corrective information. Psychol Bull 99:20–35. https://doi.org/10.1037/0033-2909.99.1.20
Kagan ER, Frank HE, Kendall PC (2017) Accommodation in youth with OCD and anxiety. Clin Psychol Sci Pract 24:78–98. https://doi.org/10.1111/cpsp.12186
Rudy BM, Lewin AB, Geffken GR et al (2014) Predictors of treatment response to intensive cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. Psychiatry Res 220:433–440. https://doi.org/10.1016/j.psychres.2014.08.002
Piacentini J, Bergman RL, Chang S et al (2011) Controlled comparison of family cognitive behavioral therapy and psychoeducation/relaxation training for child obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 50:1149–1161. https://doi.org/10.1016/j.jaac.2011.08.003
Khanna MS, Kendall PC (2009) Exploring the role of parent training in the treatment of childhood anxiety. J Consult Clin Psychol 77:981–986. https://doi.org/10.1037/a0016920
Rudy BM, Zavrou S, Johnco C et al (2017) Parent-led exposure therapy: a pilot study of a brief behavioral treatment for anxiety in young children. J Child Fam Stud 26:2475–2484. https://doi.org/10.1007/s10826-017-0772-y
Storch EA, Wilhelm S, Sprich S et al (2016) Efficacy of augmentation of cognitive behavior therapy with weight-adjusted d-cycloserine vs placebo in pediatric obsessive-compulsive disorder: a randomized clinical trial. JAMA Psychiat 73:779–788. https://doi.org/10.1001/jamapsychiatry.2016.1128
Højgaard DRMA, Hybel KA, Ivarsson T et al (2017) One-year outcome for responders of cognitive-behavioral therapy for pediatric obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 56:940-947.e1. https://doi.org/10.1016/j.jaac.2017.09.002
Guy W (1976) Clinical Global Impressions Scale. PsycTESTS Dataset. https://doi.org/10.1037/t48216-000
Scahill L, Riddle MA, McSwiggin-Hardin M et al (1997) Children’s Yale-Brown obsessive compulsive scale: reliability and validity. J Am Acad Child Adolesc Psychiatry 36:844–852. https://doi.org/10.1097/00004583-199706000-00023
Storch EA, Murphy TK, Adkins JW et al (2006) The children’s Yale-Brown obsessive-compulsive scale: psychometric properties of child- and parent-report formats. J Anxiety Disord 20:1055–1070. https://doi.org/10.1016/j.janxdis.2006.01.006
Yucelen AG, Rodopman-Arman A, Topcuoglu V et al (2006) Interrater reliability and clinical efficacy of children’s Yale-Brown obsessive-compulsive scale in an outpatient setting. Compr Psychiatry 47:48–53. https://doi.org/10.1016/j.comppsych.2005.04.005
Piacentini J, Peris TS, Bergman RL et al (2007) Functional impairment in childhood OCD: development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale-Revised (COIS-R). J Clin Child Adolesc Psychol 36:645–653. https://doi.org/10.1080/15374410701662790
Calvocoressi L, Mazure CM, Kasl SV et al (1999) Family accommodation of obsessive-compulsive symptoms: instrument development and assessment of family ehaviour. J Nerv Ment Dis 187:636–642. https://doi.org/10.1097/00005053-199910000-00008
Lebowitz ER, Scharfstein L, Jones J (2015) Child-report of family accommodation in pediatric anxiety disorders: comparison and integration with mother-report. Child Psychiatry Hum Dev 46:501–511. https://doi.org/10.1007/s10578-014-0491-1
Storch EA, Geffken GR, Merlo LJ et al (2007) Family accommodation in pediatric obsessive-compulsive disorder. J Clin Child Adolesc Psychol 36:207–216. https://doi.org/10.1080/15374410701277929
Hallquist MN, Wiley JF (2018) Mplus Automation: an R package for facilitating large-scale latent variable analyses in Mplus. Struct Equ Model 25:621–638. https://doi.org/10.1080/10705511.2017.1402334
Muthén, L.K., Muthén, B.O. (1998) Mplus User’s Guide, Eighth. Muthén & Muthén, Los Angeles
Feinberg L, Kerns C, Pincus DB, Comer JS (2018) A preliminary examination of the link between maternal experiential avoidance and parental accommodation in anxious and non-anxious children. Child Psychiatry Hum Dev 49:652–658. https://doi.org/10.1007/s10578-018-0781-0
Meyer JM, Clapp JD, Whiteside SP et al (2018) Predictive relationship between parental beliefs and accommodation of pediatric anxiety. Behav Ther 49:580–593. https://doi.org/10.1016/j.beth.2017.11.004
O’Connor EE, Langer DA, Comer JS, Tompson MC (2020) A randomized-controlled examination of the effect of cognitive reappraisal instruction on maternal accommodation of child anxiety symptoms. J Anxiety Disord 74:102260. https://doi.org/10.1016/j.janxdis.2020.102260
Benito KG, Caporino NE, Frank HE et al (2015) Development of the pediatric accommodation scale: reliability and validity of clinician- and parent-report measures. J Anxiety Disord 29:14–24. https://doi.org/10.1016/j.janxdis.2014.10.004
Funding
This research was supported by a grant from the National Institute of Mental Health (R01 MH079217, principal investigator Jennifer Freeman).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Research Involving Human Participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
O’Connor, E.E., Carper, M.M., Schiavone, E. et al. Trajectory of Change in Parental Accommodation and Its Relation to Symptom Severity and Impairment in Pediatric OCD. Child Psychiatry Hum Dev 54, 232–240 (2023). https://doi.org/10.1007/s10578-021-01240-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10578-021-01240-4