Abstract
Considering the variability in individual responses to opioids and the growing concerns about opioid addiction, prescribing opioids for postoperative pain management after spine surgery presents significant challenges. Therefore, this study undertook a novel pharmacogenomics-based in silico investigation of FDA-approved opioid medications. The DrugBank database was employed to identify all FDA-approved opioids. Subsequently, the PharmGKB database was utilized to filter through all variant annotations associated with the relevant genes. In addition, the dpSNP (https://www.ncbi.nlm.nih.gov/snp/), a publicly accessible repository, was used. Additional analyses were conducted using STRING-MODEL (version 12), Cytoscape (version 3.10.1), miRTargetLink.2, and NetworkAnalyst (version 3). The study identified 125 target genes of FDA-approved opioids, encompassing 7019 variant annotations. Of these, 3088 annotations were significant and pertained to 78 genes. During variant annotation assessments (VAA), 672 variants remained after filtration. Further in-depth filtration based on variant functions yielded 302 final filtered variants across 56 genes. The Monoamine GPCRs pathway emerged as the most significant signaling pathway. Protein–protein interaction (PPI) analysis revealed a fully connected network comprising 55 genes. Gene–miRNA Interaction (GMI) analysis of these 55 candidate genes identified miR-16-5p as a pivotal miRNA in this network. Protein–Drug Interaction (PDI) assessment showed that multiple drugs, including Ibuprofen, Nicotine, Tramadol, Haloperidol, Ketamine, l-Glutamic Acid, Caffeine, Citalopram, and Naloxone, had more than one interaction. Furthermore, Protein–Chemical Interaction (PCI) analysis highlighted that ABCB1, BCL2, CYP1A2, KCNH2, PTGS2, and DRD2 were key targets of the proposed chemicals. Notably, 10 chemicals, including carbamylhydrazine, tetrahydropalmatine, Terazosin, beta-methylcholine, rubimaillin, and quinelorane, demonstrated dual interactions with the aforementioned target genes. This comprehensive review offers multiple strong, evidence-based in silico findings regarding opioid prescribing in spine pain management, introducing 55 potential genes. The insights from this report can be applied in exome analysis as a pharmacogenomics (PGx) panel for pain susceptibility, facilitating individualized opioid prescribing through genotyping of related variants. The article also points out that African Americans represent an important group that displays a high catabolism of opioids and suggest the need for a personalized therapeutic approach based on genetic information.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The United States has been grappling with a concerning rise in issues related to prescription misuse, opioid use disorder, and fatal overdoses (El Ibrahimi et al. 2023; Wang et al. 2023). Over two decades, from 1999 to 2020, the country witnessed a staggering toll of over 263,000 lives lost due to overdoses linked to prescription opioids (Aaron 2023). This distressing figure represents a nearly fivefold increase in overdose deaths involving prescription opioids from 1999 to 2020 (Böttcher et al. 2023). The root of this crisis can be traced back to the 1990s, a period when the volume of opioids being prescribed to patients started to escalate (Friedman et al. 2020). Unfortunately, as the prescription quantities of opioids surged, so did the incidents of overdoses and fatalities stemming from these medications. Despite this surge in opioid prescriptions for pain management, there has been no corresponding alteration in the amount of pain reported by the American populace (Piper et al. 2018).
The shift in medical practice has been partially ascribed to misleading information disseminated by pharmaceutical companies, who erroneously downplayed the risk of addiction associated with certain opioid pain relievers (Sarpatwari et al. 2017). This deceit had an effect since the truth regarding the highly addictive potential of these drugs recently became known (Meier 2003, 2018; Posner 2021).
By then, many of these opioids had already been misused, abused, or diverted. Concurrently, the American Pain Society introduced the notion of pain as the “fifth vital sign,” advocating for its evaluation and treatment at par with traditional vital signs such as temperature, blood pressure, respiratory rate, and heart rate (Krauss et al. 2021). This concept gained traction in 2001 with the endorsement by the Joint Commission, placing pain management practices under closer scrutiny (Scher et al. 2018).
2020 saw a grim average of 44 deaths daily due to prescription opioid overdoses, culminating in over 16,000 fatalities (Wilson et al. 2020). Almost a quarter (24%) of all deaths due to overdoses that year were related to prescription opioids; this suggests a 16% increase in prescription opioid-related morbidity between 2019 and 2020. Post-surgical pain management often marks patients' initial exposure to opioids, consequently posing a documented risk for chronic opioid dependence among opioid-naïve individuals. Alarmingly, around 70% of those using prescription opioids acquire them through diversion, frequently via legitimate prescriptions of friends and family (Krauss et al. 2021). Many surgeons, including orthopedic specialists who are ranked as the third-highest opioid prescribers, administer opioids to control postoperative pain. However, miscalculations in assessing the extent of postoperative pain can lead to excessive opioid prescriptions after surgery, inadvertently contributing to the surplus of unused pills that can be diverted (Orosz et al. 2022). The following distinct challenges are common in pain management of spine patients:
Substantial postoperative opioid needs have been associated with spine surgeries, as evidenced by recent studies encompassing various orthopedic and non-orthopedic elective procedures (Wyles et al. 2021).
Data extrapolated from the Global Burden of Disease, Injuries, and Risk Factors Study spanning 1990 to 2017 identifies low back pain as a leading cause of global disability, persistently ranking among the top five worldwide (Wu et al. 2020).
Many patients are prescribed opioids before consulting a spine surgeon, rendering them opioid-experienced, consequently heightening the risk of opioid misuse, abuse, and dependency (Cram et al. 2019).
The population of the United States is living longer, and undergoing more spine surgery. For example, between 2020 and 2040, surgical procedures for Anterior Cervical Discectomy and Fusion (ACDF) are anticipated to grow by 13.3% (from 153,288 to 173,699 procedures), while Posterior Cervical Discectomy and Fusion (PCDF) surgeries are expected to see a 19.3% increase (from 29,620 to 35,335 procedures). The most significant growth for ACDF is forecasted in the 45–54 age bracket (from 42,077 to 49,827) and the 75–84 age bracket (from 8065 to 14,862). For PCDF, the 75–84 age bracket is projected to experience the most substantial rise (from 3710 to 6836). With the demographic shift toward an older population, slight upticks are also predicted in the over-85 age group for ACDF (from 858 to 1847) and PCDF (from 730 to 1573) (Neifert et al. 2020).
Despite the identification of specific predictors that influence patterns of opioid overuse, (Dasgupta et al. 2018) such as prior opioid use, surgery type, patient age, body mass index (BMI), diagnoses of depression or anxiety, length of hospital stay, and pain scores at discharge, there is a notable absence of precise pharmacogenetic parameters in preoperative protocols. The integration of genetic factors into these protocols could be instrumental in preparing patients for postoperative pain and in determining the most effective pain management strategies. Given that opioids are among the top 30 medications with significant pharmacogenetic implications, the prospect of leveraging genetic information to guide perioperative and postoperative pain management is promising, yet its practical application remains limited (Sadhasivam and Chidambaran 2012). In this context, a patient's genetic profile related to opioid susceptibility and responsiveness could potentially replace traditional pain management methods, reducing the risks associated with opioid use and identifying more effective treatment alternatives (Manworren 2015). The most potential annotations related to the candidate genes were extracted, refined, and presented in detail (Gene, RS ID, Function, Related Drug, Genotype-phenotype associations) (Table 1).
One potentially important tool may reside in a validated Genetic Addiction Risk Severity (GARS®) test that measure risk polymorphisms across ten reward genes having heuristic value to predetermine high genetic risk for opioid dependence. It is important to consider the interaction of neurotransmitters and genes that control the release of dopamine in the Brain Reward Cascade (BRC). It is well-known that variations within the BRC, whether genetic or epigenetic, may predispose people to addictive behaviors and alter pain tolerance. The GARS, which is the first test to accurately predict vulnerability to pain, addiction, and other compulsive behaviors, is defined as Reward Deficiency Syndrome (RDS). Moreover, sensitivity to pain may reside in the mesolimbic projection system, where genetic polymorphisms are associated with a predisposition to pain vulnerability or tolerance. Blum’s laboratory statistically validated the GARS test in 74,566 case–control subjects with Alcohol Use Disorder (AUD). This analysis assessed the Hardy–Weinberg Equilibrium (HWE) of each single nucleotide polymorphism (SNP) in controls and cases. If available, the Pearson's χ2 test or Fisher's exact test was utilized for comparing the gender, genotype, and allele distributions. The statistical analyses found the OR, 95% CI for OR, and a post-risk for 8% estimation of the population's alcoholism prevalence showed a significant detection. The OR results indicated significance for COMT, OPRM1, DRD2, DRD3, DRD4, DAT1, and 5HTT at 5% (Blum et al. 2018, 2020, 2021; Blum et al. 2022a, b; Blum et al. 2022a, b; Fried et al. 2020; Moran et al. 2021; Bajaj et al. 2022; Dennen et al. 2022; Gondré-Lewis et al. 2022; Gupta et al. 2022; Vereczkei et al. 2022; Thanos et al. 2023a, b; Thanos et al. 2023a, b). Consequently, this study aimed to explore the most effective pharmacogenomic approach to managing spinal pain in postoperative patients by analyzing potential actionable genetic variants associated with FDA-approved drugs targeting specific receptors, that is, the genes themselves (Table 2).
Methods
This study designed a bioinformatics strategy first and then reviewed the PubMed data for the keywords such as opioids, spine surgery, spine pain, pharmacogenomics, and personalized medicine. These keywords were considered the main focus of publications filtering the papers containing opioid use in spine surgery for example. To reach a precise archive of related researches, some studies were excluded from this review due to the lack of if they failed to highlight how opioids may impact spine pain management. Thus, this investigation is divided into two main categorizations; in sillico computational database analysis investigations and systematic review of the literature. The publically available and accessible dpSNP database was searched (https://www.ncbi.nlm.nih.gov/snp/) for our reference variants.
In Silico Methods
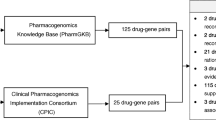
Documenting the DrugBank results of approved drugs having a role in opioid addiction, commonly used drugs such as methadone, morphine, and amphetamine were selected. The database was search for targets associated with these drugs. Following this step, all the targets were merged and duplicated targets were omitted. The in silico analyses carried out in the current study included Variant annotation assessment (VAA) by PharmGKB (https://www.pharmgkb.org/), signaling pathways (Cytoscape ver. 3.10.1), protein–protein interactions (PPI) by STRING-MODEL (https://string-db.org/), Gene–miRNA interactions (GMI) by miRTargetLink2 (https://ccb-compute.cs.uni-saarland.de/mirtargetlink2), and Protein–drug interactions (PDI) and Protein–Chemical Interactions (PCIs) by NetworkAnalyst (https://www.networkanalyst.ca/NetworkAnalyst/). The results of all aforementioned interactions are described in the various sub-sections of the “Results” section.
Results
Protein–Protein Interactions (PPI)
A large network of 126 opioid targets was extracted by STRING MODEL via the DrugBank search. Almost all of the proteins were connected in this network except CCKBR. Hence, further analysis was done with the 125 remaining genes. PPI enrichment p-value was lower than 1.0e−16. The other molecularly-demonstrated fully-connected targets were selected for further analyses (Fig. 1).
Variant Annotation Assessment (VAA)
Due to the importance of pharmacogenomics on spine pain management, the 125 remaining genes from PPIs, were then checked for their variant annotations. In total, 7019 variant annotations were found, among them, 3088 had a significant annotation according to the p-value below 0.05. Furthermore, 47 genes were discarded for having no variant annotations or not significant annotations and 78 candidate genes remained. To be more specific, the genotype associations of variant annotations were then searched for “pain” or “addiction.” Finally, after omitting the unrelated genotype associations and duplicated annotations, 78 genes and 672 variants remained. Additional deep filtrations based on the functions of variants indicated that there were 302 in total including 222 functional and 80 regulatory variants (29 Promoter, 25 Enhancer, 7 CTCF, 14 Splicing, and 5 overlapped functions variants). The intronic, intergenic, ncRNA, and synonymous variants were discarded. These 302 final filtered variants were related to the 56 genes. Another gene was eliminated as a result of the STRING MODEL described in the following, reducing the number of genes to 55.
Signaling Pathway Assessment (SPA)
Cytoscape analysis was carried out to find the signaling pathways which might be helpful for checking the refined gene list (55 genes) and prioritize the genes with higher potential of being drug targets based on the pharmacogenomics approach. Results revealed that 10 genes of out of 55 refined genes were similar with the 34 gene list of Monoamine GPCRs (10 out of 34) as the most related curated pathway with the p-value of 3.78e−13. These 10 genes were: ADRA1A, ADRA2A, ADRB1, CHRM1, DRD2, DRD3, HTR1B, HTR2A, HTR2C, and HTR7 (Fig. 2). The second most significant pathway was based on the nicotine effect on dopaminergic neurons with a p-value of 1.12e−7.
Gene–miRNA Interactions (GMIs)
miRTargetLink2 was applied on the 55 refined genes and adjusted with the strong molecular evidences to reveal the most important genes according to the GMIs. In the center of the concentric model, 13 genes had the maximum shared interactions including ABCB1, OPRM1, SLC6A4, CYP1B1, GP1BA, PPARA, TRL4, KCNH2, PPARG, PTGS2, BCL2, CFTR, and ESR1. Additionally, one miRNA indicated the maximum shared relationships with the aforementioned genes in the center of the concentric model including hsa-miR-16-5p (Fig. 3).
Protein–Drug Interactions (PDIs)
Analyzing 55 final genes by NetworkAnalyst (according to DrugBank ver. 5) adjusted for senior network, Fruchterman–Reingold model of PDIs showed important associated drugs. Drugs with the highest degree of betweenness are Ibuprofen and Nicotine with a degree of 4; Tramadol, Dipivefrin, Haloperidol, Ketamine, and Paliperidone with a degree of 3; and l-Glutamic Acid, Icosapent, Caffeine, Citalopram, Eletriptan, Atomoxetine, Pentobarbital, Indomethacin, Terfenadine, Naloxone, and Alfuzosin with a degree of 2. The other drugs can be found on Fig. 4.
Protein–Chemical Interactions (PCIs)
PCIs carried out by NetworkAnalyst based on data from the Comparative Toxicogenomics Database (CTD). Linear Bi/tripartite model adjusted for Steiner Forest Model which indicated at least one chemical for each of 55 target genes. Notably, some target genes had more than 2 interaction including ABCB1 (17 interactions), BCL2 (11 interactions); CYP1A2, KCNH2, and PTGS2 (4 interactions); and some of them had 2 interactions for example DRD2. Thus, ABCB1 was the most important target of suggested chemicals. Additionally, 10 chemicals were found with two interactions with the mentioned target genes including carbamylhydrazine, tetrahydropalmatine, 4-iodo-2, 5-dimethoxyphenylisopropylamine, 2-amino-3, 4-dimethylimidazo(4, 5-f)quinolone, Terazosin, beta-methylcholine, propiconazole, rubimaillin, quinelorane, and 1,3-dipropyl-8-cyclopentylxanthine (Fig. 5).
Literature Review
According to MeSH (Medical Subject Headings), we searched PubMed using the MeSH guidelines, and selected the titles and subheading of the papers for inclusion criteria (https://pubmed.ncbi.nlm.nih.gov/help/#using-mesh-database). Reviewing the PubMed database by focusing on the related terms including Pharmacogenomics, opioid, spine, and surgery revealed that there are 42 publications with the keywords of ‘Pharmacogenomics’ and ‘Opioids’ from 2011 to 2023; 16 papers with the keyword of pharmaocogenomics, opioid, and ‘surgery’ from 2008 to 2023 and 3 papers containing pharmacogenomics, opioid, and spine from 2014 to 2023; notably, 2 articles by Cottrill reported similar results. Following exact examination of related publications to this review, 12 papers were relevant and are examined in the discussion section. Figure 6 summarized a PRISMA workflow containing the details.
Discussion
Technology advancements have mitigated many problems related to traditional open spine surgery related to large incisions, extended surgery times and excessive blood loss contributing to postoperative pain. Robotic-guided, navigation-guided, enhanced reality-assisted, minimally invasive and endoscopic spine surgery alternatives have been shown to decrease tissue disruption and operative times (Carrau et al. 2013; Snyder 2018; Galetta et al. 2019), potentially resulting in a shorter length of stay and an accelerated overall recovery (McClelland and Goldstein 2017).
In addition to these innovative surgical techniques, implementation of enhanced surgical recovery (ERAS) protocols has modernized the way spine surgery patients prepare for, undergo, and recover from surgery (Carr et al. 2019; Wang et al. 2019). Sufficient pain control can be obtained through the combination of preoperative education on pain management and improving intraoperative non-opioid pain-management strategies. Employing these pain management strategies in an integrated approach may allow to minimize the use of postoperative opioids significantly.
Moreover, by determining certain patient information, such as (I) preoperative opioid vulnerability according to an individual's genome, (II) surgery type, (III) age, (IV) BMI, (V) depression/anxiety detections, (VI) duration of hospital stay, and (VII) pain scores at hospital discharge, are capable of more accurately predicting opioid consumption patterns. Ideally, prescription methods may be tailored according to the requirements of an individual (Dufour et al. 2014; Gao et al. 2021), recognizing that the causes of the opioid crisis are multifaceted, with socioeconomical determinants of health playing an important part (Orosz and Yamout 2023).
Genetic study on opioid analgesic response has concentrated on selecting SNPs in candidate genes (encoding proteins) which are associated with identified opioid pharmacokinetics and pharmacodynamics and those related to alternate pain-related pathways (Lötsch and Geisslinger 2006; Kim et al. 2009). Abundant studies have confirmed differing analgesic responses related to candidate SNPs, remarkably increased postoperative morphine requirements among adults homozygous for μ opioid receptor (MOR) variants which is encoded by OPRM1 A118G, but the findings do not carry across all patient populations (Chou et al. 2006a, b; Chou et al. 2006a, b; Coulbault et al. 2006; Janicki et al. 2006). Current candidate gene approaches give clear evidence of the polygenic nature of postoperative pain and opioid analgesic requirement, but continue to limit findings to known pain pathway elements (Coulbault et al. 2006; Mamie et al. 2013). A remarkable research by Chen et al. hypothesized that brain reward circuitry genes were genetic antecedents of pain sensitivity and critical diagnostic and also, they focused on pharmacogenomic treatment targets for chronic pain conditions. They introduced the concepts of brain reward cascade (BRC) and reward deficiency syndrome (RDS) both playing vital roles in pain management by opioids. A noticeable number of genes including OPRD1, OPRK1, OPRM1, BDNF, DRD genes (D1–5), MAO-A, COMT, PDYN, CYP2D6, CYP2B6, CYP2C19, CYP2C9, ABCB1, PENK, CNR1, UGT2B7, TTC12, ANKK1, NCAM1, ZCRB1, GABA(A), the metabotropic receptors mGluR6 and mGluR8, nuclear receptor NR4A2 and cryptochrome 1 (photolyase-like), Dat1, DBH, CAMKII; GnRH; NT-3 genes; G-protein alpha subunits; alpha2-adrenoceptor; interleukin-2; RGS-R7; Gbeta5, serotonin transporter, Ca2+/cAMP responsive element binding protein; P-glycoprotein, and CREB (Chen et al. 2009) have been implied in BRC and RDS.
Here we systematically reviewed 61 publications and found 12 relevant PubMed-indexed publications which are discussed in the following. By studying five tag SNPs including A118G, IVS2 + G691C, IVS3 + G5953A, IVS3 + A8449G, and TAA + A2109G, Hayashida et al. reported that analgesic necessities following major abdominal surgery are associated with both genotype and haplotype of OPRM1 gene polymorphisms (Hayashida et al. 2008). Fukuda et al. investigated the association of OPRM1 gene polymorphisms (118G and IVS3 + A8449G) with fentanyl susceptibility among patients experiencing painful cosmetic surgery. Their results offered insight into the role of OPRM1 3′ untranslated region (3′-UTR) polymorphisms, together with the A118G SNP, in fentanyl sensibility, and opened up new options for individualized pain management with fentanyl (Fukuda et al. 2009). Cook-Sather et al. conducted the first experimental GWAS in a pediatric day surgery cohort and found no relationships between rs795484 and rs1277441 at the TAOK3 gene with total morphine request in European Caucasian children (Cook-Sather et al. 2014). We investigated the TAOK3 pharmacogenomics associations in PharmGKB and then included this gene with 55 candidate genes from our analyses, but it showed no molecular connection with any members of candidate genes in a PPIs network by STRING-MODEL. Thus, we excluded TAOK3 from our list. Zhang et al. examined the impact of CYP3A5*3 polymorphism and the association between CYP3A5*3 and CYP3A4*1G variants on fentanyl analgesia following gynecological surgery among Chinese patients. They showed that, in Chinese women having gynecological surgery, CYP3A5*3 was not the primary genetic factor that contributed to inter-individual variation in the post-operative analgesic impact of fentanyl; however, a relationship between CYP3A5*3 and CYP3A4*1G variants can profoundly affect postoperative pain (Zhi-Xue et al. 2023). The influence of CYP3A5*3 polymorphism and interaction between CYP3A5*3 and CYP3A4*1G polymorphisms on post-operative fentanyl analgesia was highlighted in Chinese patients (Zhang et al. 2011). Senagore et al.'s study was designed to conduct the first evaluation of the effects of a PGx-guided analgesic option in an Enhanced Recovery Protocol (ERP) after major abdominal surgery (Zhao et al. 2022). They investigated the genes OPRM1, COMT, CYP2C9, CYP2C19, CYP1A2, CYP2D6, CYP3A4, CYP3A5, and ABCB1. According to their statistics, the groups' gender and procedure mixes were comparable, and over half of the PGx group experienced altered analgesia from the conventional ERP. Post-Op Day 1 (POD 1) (3.8 vs. 5.4) to POD 5 (3.0 vs. 4.5) showed substantially lower Overall Benefit of Analgesia Score (OBAS) ratings (p = 0.0.1) for the PGx group. In POD 1 to POD 5, the PGx group's analgesia was additionally better (p = 0.04). They came to the conclusion that 80% of patients had narcotic alterations of the ERP analgesic scheme and 56% of patients had NSAID selection based on pharmacogenetic advice utilizing the multi-gene profile analyzed. Compared to their normal ERP, these adjustments produced good analgesia with a 50% decrease in narcotic intake and a reduced risk of analgesic-related adverse reactions. These findings pointed to potential areas of improvement for ERP deriving from a patient-centered, lower-narcotic analgesic regimen that offers early and long-lasting pain relief with fewer adverse effects associated with opioid use (Senagore et al. 2017). Rocco et al. hypothesized that pharmacogenomic detection of individuals with varying opioid metabolism capability might allow for individualization of post-surgical opioid prescriptions. This study proposed an association between genetically regulated metabolism and opioid needs following surgery. Enhanced CYP2D6 enzymatic activity was linked to higher opioid intake, fewer unused opioids, and worse satisfaction with opioid prescriptions (Rocco et al. 2019). Li et al. identified 27 SNPs from 9 genes, including ABCB1, COMT, ARRB2, DRD2, MC1R, KCNJ6, OPRM1, OPRD1, and UGT2B7, that matched selection criteria and were evaluated with TAOK3. Morphine dose in African American (AA) children and ABCB1 rs1045642 (p = 0.02) and OPRM1 rs1799971 (p = 0.02); KCNJ6 rs2211843 and high pain in AA subjects (p = 0.01) and in congruent European Caucasian pain phenotypes (p = 0.01); and COMT rs740603 for high pain in European Caucasian individuals (p = 0.046). According to Li et al., TAOK3 (rs795484) is still a major contributor to high morphine dosage requirements in European Caucasian people (Li et al. 2019a, b).
Along these lines, Ettienne et al. (2019) importantly, conducted a retrospective cohort study of 113 patients undergoing buprenorphine-based OUD management in Northeast Washington, DC to find if clinical pharmacogenomics testing for CYP3A4 and CYP3A5 would influence treatment consequences. Clinical outcomes were based on presence of withdrawal symptoms, instances of unauthorized substances in urine drug tests (UDTs), and sublingual buprenorphine/naloxone (SBN) dose with standard-of-care (SOC) dosing versus pharmacogenomics (PGx)-based dosing. Their research suggested that patients with at least one copy of the CYP3A4*1B allele exhibit an accelerated rate of metabolism compared to the wild-type allele CYP3A4*1. These findings have translated in novel approaches in the treatment of pain and addiction by the same group (Ettienne et al. 2017). They suggested that pharmacogenomic testing as clinical decision support helped to individualize OUD management. They further suggested that collaboration by key stakeholders is essential to establishing pharmacogenetic testing as standard of care in OUD management.
Matic et al. examined the possible function of OPRM1 and COMT variants in acute, chronic, and experimental thermal pain following adult heart surgery. The subjects were randomly assigned to receive remifentanil or fentanyl throughout the procedure. They discovered that in adult cardiac surgery individuals, the COMT haplotype can partially account for the variation in early postoperative pain (Matic et al. 2020). Merchant et al. demonstrated that the association of CYP2D6 genotype can predict phenotypes with higher oxycodone requirements and adverse effects among children who underwent surgery. They genotyped CYP2D6 alleles by the TaqMan allelic discrimination system in three allelic groups including full enzyme activity [*1 (N/A), *2 (rs16947), *2A (hCV32407252), *35 (rs769258)]; reduced enzyme activity [*9 (rs5030656), *10 (rs1065852), *17 (hCV2222771), *41 (hCV34816116)]; and none enzyme activity [*3 (hCV32407232), *4 (rs3892097), *5 (deleted), *6 (rs5030655), *7 (rs5030867), *8 (rs5030865), *11 (rs5030863), *14 (rs5030865), *15 (hCV32407245), *18 (hCV32407220), *19 (hCV32407233), *20 (hCV72649949), *40 (hCV32407240), *42 (hCV72649935), *44 (hCV32407228)]. Their results revealed that increasing parent oxycodone and oxymorphone might affect clinical outcomes in severe phenotypes, but oxymorphone might have a superior safety profile. They also discovered that CYP2D6 phenotype data accessible in electronic medical records (EMR) strongly affected oral opioid prescribing patterns (Merchant et al. 2022). Prashant and colleagues studied the association of pain perception and fentanyl consumption following major abdominal surgery with CGRP 4218T/C variant. They discovered that this variation influences postoperative pain perception and analgesic intake. Patients who carried the C/C genotype had greater postoperative fentanyl intake and pain ratings, according to the researchers (Prashant et al. 2023).
To the best of our knowledge based on PubMed database, publications related to the pharmacogenomics in spine pain managements are limited to two reports including Chidambaran et al. (2015) and Cottrill et al. (2021) Chidambaran et al. performed a prospective genotype-blinded research on 88 healthy adolescents (aged 11–18 years; 85% Caucasian, 67% female) who had spine fusion surgery for scoliosis. They were observed for 48 h following surgery to assess pain levels, analgesic adjuvant usage, morphine intake, and morphine-induced respiratory depression (MIRD). OPRM1 A118G variant genotyping revealed that 76% of patients were wild type (AA) and 24% were heterozygous/homozygous for the variation (AG/GG). Results showed that the risk of MIRD in patients with AA genotype was significantly higher (p = 0.030) and presence of G allele was also associated with higher pain scores (p = 0.045) (Chidambaran et al. 2015). Cottrill et al. studied genotypes of genes including CYP2D6, CYP1A2, CYP2C9, CYP3A4, CYP3A5, CYP2B6, CYP2C19, and UGT2B7. Haplotypes were then utilized to assess each patient’s relative capability to metabolize commonly used analgesic drugs. These drugs included both non-opioid (for example ibuprofen, diclofenac, mefenamic acid, nabumetone, indomethacin, piroxicam, meloxicam, tenoxicam, lornoxicam, etoricoxib, parecoxib, celecoxib, flurbiprofen, ketoprofen, fenoprofen, hydrocodone, naproxen, and aspirin) and opioid analgesics (including morphine, ethylmorphine, hydromorphone, codeine, dihydrocodeine, methadone, hydrocodone, oxycodone, oxymorphone, alfentanil, fentanyl, sufentanil, meperidine, ketobemidone, dextropropoxyphene, levacetylmethadol, loperamide, buprenorphine, dextromethorphan, tramadol, tapentadol, and tilidine). They constructed the first pharmacogenetic profiles of an outpatient spine cohort and gave preliminary proof that an outpatient analgesic regimen consisting of one medication since they are poor metabolizers. They discovered that almost half of the patients were given one analgesic because they had genetic variants that caused them to be poor metabolizers of the medication. Given the existing opioid epidemic, 13 of the 19 patients (68%) who were taking opioid drugs at the time of examination were excessively fast metabolizers of their prescription opioid analgesic (Cottrill et al. 2021). The current review is the first report with a pharmacogenomics-based strategy of analyzing all FDA-approved drugs (as of 9 November 2023) by targeting protein-coding genes and filtering the structural and regulatory pharmacological actionable variants. Our report, in comparison with the most relevant reports by Chidambaran et al. (2015). and Cottrill et al. (2021), included more genes (128 genes were filtered down to 55 genes), and a comprehensive variant list, and multiple in silico analyses including PPIs, GMIs, PDIs, and PCIs leading to several crucial findings which are highly recommended to be investigated in future studies of opioid prescribing in spine pain managements.
Based on the strong molecular evidences, in silico outcomes represented 55 candidate genes and 302 potential actionable variants. Additionally, results of signaling pathways proposed the Monoamine GPCRs as the most significant signaling pathway of opioid prescribing in spine pain managements, GMIs suggested hsa-miR-16-5p as a prospective miRNA candidate for detection and prognosis, PDIs revealed Ibuprofen and Nicotine, Tramadol, Dipivefrin, Haloperidol, Ketamine, and Paliperidone as the highly-impacted drugs on opioid prescription, and PCI analysis indicated some target genes with more than two interaction including ABCB1, BCL2, CYP1A2, KCNH2, PTGS2, and DRD2. Also, 10 chemicals were found by PCIs which need more functional validations.
Hou et al. revealed that miR-16 plays a key role in the post-transcriptional regulation of the OPRM1 gene. They stated that morphine decreases the expression of miR-16-5p in lymphocytes, which may be reversed by the antagonist naloxone (Hou et al. 2016a, b). Remarkably, miR-16-5p inhibits MOR expression by binding to a position in its 3′ UTR that is situated within 8699 and 8719 nucleotides from the stop codon (Hou et al. 2016a, b). According to Melo et al., miR-16-5p downregulation serves as a post-transcriptional process via which morphine increases MOR receptor concentrations through stabilizing its mRNA. (Melo et al. 2018). In another report by Chen et al., they suggested that by targeting RAB23 and inhibiting p38 MAPK activation in rats, miR-16 relieves chronic inflammatory pain (Chen et al. 2016). Following subcutaneous capsaicin injection, Kusuda et al. discovered that miR-16 expression was raised in the dorsal root ganglion (DRG) but reduced in the dorsal spinal cord (Kusuda et al. 2011). Furthermore, miR-16 was predicted to target BDNF. The BDNF gene was additionally a direct target of the miR-183 and miR-206, both of which were found to be downregulated in neuropathic pain (Lin et al. 2014; Sun et al. 2017) Additionally, their down-regulation was correlated with an increase in the expression of BDNF. In the spinal cord Chronic Compression Injury (CCI) model, it was also demonstrated that miR-183 was downregulated in neurons and microglial cells (Xie et al. 2017). Consequently, in microglia, miRNAs were connected to the BDNF signaling pathway (Dai et al. 2018). According to Li et al., in the spinal cord of CCI rats, interleukin-1β and tumor-necrosis factor-α expression were downregulated with suppression of miR-15a and miR-16. Using bioinformatics, they discovered that a potential target gene for miR-15a and miR-16 is G protein-coupled receptor kinase 2 (GRK2), is a crucial regulator of neuropathic pain and inflammation. According to their final results, the GRK2 gene is targeted by miR-15a/16 expression suppression, which reduces the development of neuropathic pain (Li et al. 2019a, b). Finally, Toyama et al. showed that miR-16-5p is a circulating blood biomarker which is commonly downregulated by both hydromorphone and oxycodone treatment with a p-value of 0.003 (Toyama et al. 2017). Altogether, miR-16-5p can be further studied for a candidate biomarker in post-operative opioid prescribing in spine pain management along with the genotyping of potential variants based on each individual’s genomic vulnerabilities.
Summary
Variants in patients might affect both pharmacokinetic and pharmacodynamic characteristics of the drugs, which define drug metabolism and effectiveness. (Scott et al. 2019). Several drugs, for example opioids have these two factors involved due to drug modifications via the cytochrome P450 (CYP450) system in the liver changing the biological activity of the substance. Prior study has indicated that such variants are rare (Smith 2009), but their incidence in individuals with spine disorders is unclear. Knowing the incidence of these variants may assist patients in achieving better results since identifying inappropriate pharmaceutical analgesic regimens during clinical assessment may help maximize nonoperative treatment. This advancement, in turn, might reduce healthcare expenses while improving patient satisfaction by saving certain patients from the risks related to surgical intervention (Downs et al. 2019; Cottrill et al. 2021).
Conclusion
The current review aimed to investigate the impact of pharmacogenomics in opioid prescribing of postoperative patients who underwent spine surgery to manage the pain severity and reduce the use of opioids. This goal leads to the personalized medicine strategies of opioid use according to the individual’s genotypes dictated to the potential candidate variants. The outcomes of this study indicated 56 highly-impacted genes. Additional in silico analyses showed novel findings in PPIs, GMIs, PDIs, and PCIs which need further functional and clinical validations.
Data Availability
The data that support the findings of this study are available on request from the corresponding author.
References
Aaron D (2023) The fall of FDA review. Yale J Health Policy Law Ethics 95
Bajaj A, Blum K, Bowirrat A, Gupta A, Baron D, Fugel D, Nicholson A, Fitch T, Downs BW, Bagchi D (2022) DNA directed pro-dopamine regulation coupling subluxation repair, H-Wave® and other neurobiologically based modalities to address complexities of chronic pain in a female diagnosed with reward deficiency syndrome (RDS): emergence of Induction of “Dopamine Homeostasis” in the face of the opioid crisis. J Pers Med 12(9):1416. https://doi.org/10.3390/jpm12091416
Blum K, Lott L, Siwicki D, Fried L, Hauser M, Simpatico T, Baron D, Howeedy A, Badgaiyan RD (2018) Genetic addiction risk score (GARS™) as a predictor of substance use disorder: identifying predisposition not diagnosis. Curr Trends Med Diagn Methods. https://doi.org/10.29011/CTMDM-101.100001
Blum K, Bowirrat A, Baron D, Lott L, Ponce J, Brewer R, Siwicki D, Boyett B, Gondre-Lewis M, Smith D (2020) Biotechnical development of genetic addiction risk score (GARS) and selective evidence for inclusion of polymorphic allelic risk in substance use disorder (SUD). J Syst Integr Neurosci. https://doi.org/10.15761/JSIN.1000221
Blum K, Bowirrat A, Lewis MCG, Simpatico TA, Ceccanti M, Steinberg B, Modestino EJ, Thanos PK, Baron D, McLaughlin T (2021) Exploration of epigenetic state hyperdopaminergia (Surfeit) and genetic trait hypodopaminergia (Deficit) during adolescent brain development. Curr Psychopharmacol. https://doi.org/10.2174/2211556010666210215155509
Blum K, Brodie MS, Pandey SC, Cadet JL, Gupta A, Elman I, Thanos PK, Gondre-Lewis MC, Baron D, Kazmi S (2022a) Researching mitigation of alcohol binge drinking in polydrug abuse: KCNK13 and RASGRF2 gene(s) risk polymorphisms coupled with genetic addiction risk severity (GARS) guiding precision pro-dopamine regulation. J Pers Med 12(6):1009. https://doi.org/10.3390/jpm12061009
Blum K, Han D, Gupta A, Baron D, Braverman ER, Dennen CA, Kazmi S, Llanos-Gomez L, Badgaiyan RD, Elman I (2022b) Statistical validation of risk alleles in genetic addiction risk severity (GARS) test: early identification of risk for alcohol use disorder (AUD) in 74,566 case–control subjects. J Pers Med 12(9):1385. https://doi.org/10.3390/jpm12091385
Böttcher L, Chou T, D'Orsogna MR (2023) Forecasting drug overdose mortality by age in the United States at the national and county levels. medRxiv. https://doi.org/10.1101/2023.09.25.23296097
Carr DA, Saigal R, Zhang F, Bransford RJ, Bellabarba C, Dagal A (2019) Enhanced perioperative care and decreased cost and length of stay after elective major spinal surgery. Neurosurg Focus 46(4):E5. https://doi.org/10.3171/2019.1.FOCUS18630
Carrau RL, Prevedello DM, de Lara D, Durmus K, Ozer E (2013) Combined transoral robotic surgery and endoscopic endonasal approach for the resection of extensive malignancies of the skull base. Head Neck 35(11):E351-358. https://doi.org/10.1002/hed.23238
Chen AL-C, Chen TJ, Waite RL, Reinking J, Tung HL, Rhoades P, Downs BW, Braverman E, Braverman D, Kerner M (2009) Hypothesizing that brain reward circuitry genes are genetic antecedents of pain sensitivity and critical diagnostic and pharmacogenomic treatment targets for chronic pain conditions. Med Hypotheses 72(1):14–22. https://doi.org/10.1016/j.mehy.2008.07.059
Chen W, Guo S, Wang S (2016) MicroRNA-16 alleviates inflammatory pain by targeting Ras-related protein 23 (RAB23) and inhibiting p38 MAPK activation. Med Sci Monit Int Med J Exp Clin Res 22:3894. https://doi.org/10.12659/msm.897580
Chidambaran V, Mavi J, Esslinger H, Pilipenko V, Martin L, Zhang K, Sadhasivam S (2015) Association of OPRM1 A118G variant with risk of morphine-induced respiratory depression following spine fusion in adolescents. Pharmacogenomics J 15(3):255–262. https://doi.org/10.1038/tpj.2014.59
Chou W-Y, Wang C-H, Liu P-H, Liu C-C, Tseng C-C, Jawan B (2006a) Human opioid receptor A118G polymorphism affects intravenous patient-controlled analgesia morphine consumption after total abdominal hysterectomy. J Am Soc Anesthesiol 105(2):334–337. https://doi.org/10.1097/00000542-200608000-00016
Chou WY, Yang LC, Lu HF, Ko JY, Wang CH, Lin SH, Lee TH, Concejero A, Hsu CJ (2006b) Association of μ-opioid receptor gene polymorphism (A118G) with variations in morphine consumption for analgesia after total knee arthroplasty. Acta Anaesthesiol Scand 50(7):787–792. https://doi.org/10.1111/j.1399-6576.2006.01058.x
Cook-Sather SD, Li J, Goebel TK, Sussman EM, Rehman MA, Hakonarson H (2014) TAOK3, a novel genome-wide association study locus associated with morphine requirement and postoperative pain in a retrospective pediatric day surgery population. PAIN® 155(9):1773–1783. https://doi.org/10.1016/j.pain.2014.05.032
Cottrill E, Pennington Z, Ahmed AK, Jiang B, Ehresman J, Zhu A, Perdomo-Pantoja A, Lubelski D, Sciubba DM, Witham T (2021) First report of pharmacogenomic profiling in an outpatient spine setting: preliminary results from a pilot study. World Neurosurg 145:e21–e31. https://doi.org/10.1016/j.wneu.2020.09.007
Coulbault L, Beaussier M, Verstuyft C, Weickmans H, Dubert L, Trégouet D, Descot C, Parc Y, Lienhart A, Jaillon P (2006) Environmental and genetic factors associated with morphine response in the postoperative period. Clin Pharmacol Ther 79(4):316–324. https://doi.org/10.1016/j.clpt.2006.01.007
Cram P, Landon BE, Matelski J, Ling V, Perruccio AV, Paterson JM, Rampersaud YR (2019) Utilization and outcomes for spine surgery in the United States and Canada. Spine (phila Pa 1976) 44(19):1371–1380. https://doi.org/10.1097/BRS.0000000000003083
Dai Z, Chu H, Ma J, Yan Y, Zhang X, Liang Y (2018) The regulatory mechanisms and therapeutic potential of microRNAs: from chronic pain to morphine tolerance. Front Mol Neurosci 11:80. https://doi.org/10.3389/fnmol.2018.00080
Dasgupta N, Beletsky L, Ciccarone D (2018) Opioid crisis: no easy fix to its social and economic determinants. Am J Public Health 108(2):182–186. https://doi.org/10.2105/AJPH.2017.304187
Dennen CA, Blum K, Bowirrat A, Thanos PK, Elman I, Ceccanti M, Badgaiyan RD, McLaughlin T, Gupta A, Bajaj A (2022) Genetic addiction risk severity assessment identifies polymorphic reward genes as antecedents to reward deficiency syndrome (RDS) hypodopaminergia’s effect on addictive and non-addictive behaviors in a nuclear family. J Pers Med 12(11):1864. https://doi.org/10.3390/jpm12111864
Downs BW, Blum K, Baron D, Bowirrat A, Lott L, Brewer R, Boyett B, Siwicki D, Roy AK, Podesta A (2019) Death by opioids: are there non-addictive scientific solutions? J Syst Integr Neurosci. https://doi.org/10.15761/JSIN.1000211
Dufour R, Mardekian J, Pasquale MK, Schaaf D, Andrews GA, Patel NC (2014) Understanding predictors of opioid abuse: predictive model development and validation. Am J Pharm Benefits 6(5):208–216
El Ibrahimi S, Hendricks MA, Little K, Ritter GA, Flores D, Loy B, Wright D, Weiner SG (2023) The association between community social vulnerability and prescription opioid availability with individual opioid overdose. Drug Alcohol Depend 252:110991. https://doi.org/10.1016/j.drugalcdep.2023.110991
Ettienne EB, Chapman E, Maneno M, Ofoegbu A, Wilson B, Settles-Reaves B, Clarke M, Dunston G, Rosenblatt K (2017) Pharmacogenomics-guided policy in opioid use disorder (OUD) management: an ethnically-diverse case-based approach. Addict Behav Rep 6:8–14. https://doi.org/10.1016/j.abrep.2017.05.001
Ettienne EB, Ofoegbu A, Maneno MK, Briggs J, Ezeude G, Williams S, Walker C, Chapman E (2019) Pharmacogenomics and opioid use disorder: clinical decision support in an African American cohort. J Natl Med Assoc 111(6):674–681. https://doi.org/10.1016/j.jnma.2019.09.006
Fried L, Modestino EJ, Siwicki D, Lott L, Thanos PK, Baron D, Badgaiyan RD, Ponce JV, Giordano J, Downs WB (2020) Hypodopaminergia and “Precision Behavioral Management” (PBM): it is a generational family affair. Curr Pharm Biotechnol 21(6):528–541. https://doi.org/10.2174/1389201021666191210112108
Friedman SR, Krawczyk N, Perlman DC, Mateu-Gelabert P, Ompad DC, Hamilton L, Nikolopoulos G, Guarino H, Cerdá M (2020) The opioid/overdose crisis as a dialectics of pain, despair, and one-sided struggle. Front Public Health 8:540423. https://doi.org/10.3389/fpubh.2020.540423
Fukuda K, Hayashida M, Ide S, Saita N, Kokita Y, Kasai S, Nishizawa D, Ogai Y, Hasegawa J, Nagashima M (2009) Association between OPRM1 gene polymorphisms and fentanyl sensitivity in patients undergoing painful cosmetic surgery. PAIN® 147(1–3):194–201. https://doi.org/10.1016/j.pain.2009.09.004
Galetta MS, Leider JD, Divi SN, Goyal DKC, Schroeder GD (2019) Robotics in spinal surgery. Ann Transl Med 7(Suppl 5):S165. https://doi.org/10.21037/atm.2019.07.93
Gao W, Leighton C, Chen Y, Jones J, Mistry P (2021) Predicting opioid use disorder and associated risk factors in a Medicaid managed care population. Am J Manag Care. https://doi.org/10.37765/ajmc.2021.88617
Gondré-Lewis MC, Elman I, Alim T, Chapman E, Settles-Reaves B, Galvao C, Gold MS, Baron D, Kazmi S, Gardner E (2022) Frequency of the dopamine receptor D3 (rs6280) vs. opioid receptor µ1 (rs1799971) polymorphic risk alleles in patients with opioid use disorder: a preponderance of dopaminergic mechanisms? Biomedicines 10(4):870. https://doi.org/10.3390/biomedicines10040870
Gupta A, Bowirrat A, Gomez LL, Baron D, Elman I, Giordano J, Jalali R, Badgaiyan RD, Modestino EJ, Gold MS (2022) Hypothesizing in the face of the opioid crisis coupling Genetic Addiction Risk Severity (GARS) testing with electrotherapeutic nonopioid modalities such as H-Wave could attenuate both pain and hedonic addictive behaviors. Int J Environ Res Public Health 19(1):552
Hayashida M, Nagashima M, Satoh Y, Katoh R, Tagami M, Ide S, Kasai S, Nishizawa D, Ogai Y, Hasegawa J (2008) Analgesic requirements after major abdominal surgery are associated with OPRM1 gene polymorphism genotype and haplotype. https://doi.org/10.2217/14622416.9.11.1605
Hou W, Li H, Jiang W, Zhang C, McNutt MA, Li G (2016a) Simian immunodeficiency virus impacts microRNA-16 mediated post-transcriptional regulation of mu opioid receptor in CEM ×174 cells. J Cell Biochem 117(1):84–93. https://doi.org/10.1002/jcb.25251
Hou W, Li H, Jiang W, Zhang C, McNutt MA, Li G (2016b) Simian immunodeficiency virus impacts microRNA-16 mediated post-transcriptional regulation of mu opioid receptor in CEM× 174 cells. J Cell Biochem 117(1):84–93. https://doi.org/10.1002/jcb.25251
Janicki PK, Schuler G, Francis D, Bohr A, Gordin V, Jarzembowski T, Ruiz-Velasco V, Mets B (2006) A genetic association study of the functional A118G polymorphism of the human μ-opioid receptor gene in patients with acute and chronic pain. Anesth Analg 103(4):1011–1017. https://doi.org/10.1213/01.ane.0000231634.20341.88
Kim H, Clark D, Dionne RA (2009) Genetic contributions to clinical pain and analgesia: avoiding pitfalls in genetic research. J Pain 10(7):663–693. https://doi.org/10.1016/j.jpain.2009.04.001
Krauss WE, Habermann EB, Goyal A, Ubl DS, Alvi MA, Whipple DC, Glasgow AE, Gazelka HM, Bydon M (2021) Impact of opioid prescribing guidelines on postoperative opioid prescriptions following elective spine surgery: results from an institutional quality improvement initiative. Neurosurgery 89(3):460–470. https://doi.org/10.1093/neuros/nyab196
Kusuda R, Cadetti F, Ravanelli MI, Sousa TA, Zanon S, De Lucca FL, Lucas G (2011) Differential expression of microRNAs in mouse pain models. Mol Pain. https://doi.org/10.1186/1744-8069-7-17
Li J, Wei Z, Zhang J, Hakonarson H, Cook-Sather SD (2019a) Candidate gene analyses for acute pain and morphine analgesia after pediatric day surgery: African American versus European Caucasian ancestry and dose prediction limits. Pharmacogenomics J 19(6):570–581. https://doi.org/10.1038/s41397-019-0074-4
Li T, Wan Y, Sun L, Tao S, Chen P, Liu C, Wang K, Zhou C, Zhao G (2019b) Inhibition of microRNA-15a/16 expression alleviates neuropathic pain development through upregulation of G protein-coupled receptor kinase 2. Biomol Ther 27(4):414. https://doi.org/10.4062/biomolther.2018.073
Lin CR, Chen KH, Yang CH, Huang HW, Sheen-Chen SM (2014) Intrathecal miR-183 delivery suppresses mechanical allodynia in mononeuropathic rats. Eur J Neurosci 39(10):1682–1689. https://doi.org/10.1111/ejn.12522
Lötsch J, Geisslinger G (2006) Current evidence for a genetic modulation of the response to analgesics. Pain 121(1–2):1–5. https://doi.org/10.1016/j.pain.2006.01.010
Mamie C, Rebsamen MC, Morris MA, Morabia A (2013) First evidence of a polygenic susceptibility to pain in a pediatric cohort. Anesth Analg 116(1):170–177. https://doi.org/10.1213/ANE.0b013e31826f0637
Manworren RC (2015) Multimodal pain management and the future of a personalized medicine approach to pain. AORN J 101(3):307–318. https://doi.org/10.1016/j.aorn.2014.12.009
Matic M, de Hoogd S, de Wildt SN, Tibboel D, Knibbe CA, van Schaik RH (2020) OPRM1 and COMT polymorphisms: implications on postoperative acute, chronic and experimental pain after cardiac surgery. Pharmacogenomics 21(3):181–193. https://doi.org/10.2217/pgs-2019-0141
McClelland S III, Goldstein JA (2017) Minimally invasive versus open spine surgery: what does the best evidence tell us? J Neurosci Rural Pract 8(2):194–198. https://doi.org/10.4103/jnrp.jnrp_472_16
Meier B (2003) Pain killer: a “wonder” drug’s trail of addiction and death. Rodale, Emmaus
Meier B (2018) Pain killer: an empire of deceit and the origin of America’s opioid epidemic. Random House, New York
Melo Z, Ishida C, Goldaraz MDLP, Rojo R, Echavarria R (2018) Novel roles of non-coding RNAs in opioid signaling and cardioprotection. Non-Coding RNA 4(3):22. https://doi.org/10.3390/ncrna4030022
Merchant S, Prows CA, Yang F, Ding L, MacDonald J, Zhang X, Sadhasivam S, Garcia V, Sturm P, Chidambaran V (2022) Association of CYP2D6 genotype predicted phenotypes with oxycodone requirements and side effects in children undergoing surgery. Ann Transl Med. https://doi.org/10.21037/atm-2022-58
Moran M, Blum K, Ponce JV, Lott L, Gondré-Lewis MC, Badgaiyan S, Brewer R, Downs BW, Fynman P, Weingarten A (2021) High genetic addiction risk score (GARS) in chronically prescribed severe chronic opioid probands attending multi-pain clinics: an open clinical pilot trial. Mol Neurobiol 58:3335–3346. https://doi.org/10.1007/s12035-021-02312-1
Neifert SN, Martini ML, Yuk F, McNeill IT, Caridi JM, Steinberger J, Oermann EK (2020) Predicting trends in cervical spinal surgery in the United States from 2020 to 2040. World Neurosurg 141:e175–e181. https://doi.org/10.1016/j.wneu.2020.05.055
Orosz LD, Yamout T (2023) The opioid crisis as it pertains to spine surgery. J Spine Surg 9(1):9–12. https://doi.org/10.21037/jss-22-107
Orosz LD, Thomson AE, Yamout T, Bhatt FR, Allen B, Schuler TC, Roy R, Good CR, Haines CM, Jazini E (2022) Opioid use after elective spine surgery: do spine surgery patients consume less than prescribed today? N Am Spine Soc J 12:100185. https://doi.org/10.1016/j.xnsj.2022.100185
Piper BJ, Shah DT, Simoyan OM, McCall KL, Nichols SD (2018) Trends in medical use of opioids in the US, 2006–2016. Am J Prev Med 54(5):652–660. https://doi.org/10.1016/j.amepre.2018.01.034
Posner G (2021) Pharma: greed, lies, and the poisoning of America. Simon and Schuster, New York
Prashant H, Saxena KN, Kapoor S, Wadhwa B, Kerai S, Gaba P (2023) Correlation of pain perception and fentanyl consumption after major abdominal surgery with CGRP 4218T/C polymorphism: a prospective interventional study. Indian J Anaesth 67(9):796–801. https://doi.org/10.4103/ija.ija_1033_22
Rocco R, Thiels CA, Ubl DS, Moyer AM, Habermann EB, Cassivi SD (2019) Use of pharmacogenetic data to guide individualized opioid prescribing after surgery. Surgery 166(4):476–482. https://doi.org/10.1016/j.surg.2019.04.033
Sadhasivam S, Chidambaran V (2012) Pharmacogenomics of opioids and perioperative pain management. Pharmacogenomics 13(15):1719–1740. https://doi.org/10.2217/pgs.12.152
Sarpatwari A, Sinha MS, Kesselheim AS (2017) The opioid epidemic: fixing a broken pharmaceutical market. Harv Law Policy Rev 11:463
Scher C, Meador L, Van Cleave JH, Reid MC (2018) Moving beyond pain as the fifth vital sign and patient satisfaction scores to improve pain care in the 21st century. Pain Manag Nurs 19(2):125–129. https://doi.org/10.1016/j.pmn.2017.10.010
Scott RH, Fowler TA, Caulfield M (2019) Genomic medicine: time for health-care transformation. Lancet 394(10197):454–456. https://doi.org/10.1016/S0140-6736(19)31796-9
Senagore AJ, Champagne BJ, Dosokey E, Brady J, Steele SR, Reynolds HL, Stein SL, Delaney CP (2017) Pharmacogenetics-guided analgesics in major abdominal surgery: further benefits within an enhanced recovery protocol. Am J Surg 213(3):467–472. https://doi.org/10.1016/j.amjsurg.2016.11.008
Smith HS (2009) Opioid metabolism. Mayo Clinic Proc. https://doi.org/10.1016/S0025-6196(11)60750-7
Snyder LA (2018) Integrating robotics into a minimally invasive transforaminal interbody fusion workflow. Neurosurg Focus 45(VideoSuppl1):V4. https://doi.org/10.3171/2018.7.FocusVid.18111
Sun W, Zhang L, Li R (2017) Overexpression of miR-206 ameliorates chronic constriction injury-induced neuropathic pain in rats via the MEK/ERK pathway by targeting brain-derived neurotrophic factor. Neurosci Lett 646:68–74. https://doi.org/10.1016/j.neulet.2016.12.047
Thanos PK, Hanna C, Mihalkovic A, Hoffman A, Posner A, Butsch J, Blum K, Georger L, Mastrandrea LD, Quattrin T (2023a) Genetic correlates as a predictor of bariatric surgery outcomes after 1 year. Biomedicines 11(10):2644. https://doi.org/10.3390/biomedicines11102644
Thanos PK, Hanna C, Mihalkovic A, Hoffman AB, Posner AR, Busch J, Smith C, Badgaiyan RD, Blum K, Baron D (2023b) The first exploratory personalized medicine approach to improve bariatric surgery outcomes utilizing psychosocial and genetic risk assessments: encouraging clinical research. J Pers Med 13(7):1164. https://doi.org/10.3390/jpm13071164
Toyama K, Kiyosawa N, Watanabe K, Ishizuka H (2017) Identification of circulating miRNAs differentially regulated by opioid treatment. Int J Mol Sci 18(9):1991. https://doi.org/10.3390/ijms18091991
Vereczkei A, Barta C, Magi A, Farkas J, Eisinger A, Király O, Belik A, Griffiths MD, Szekely A, Sasvári-Székely M (2022) FOXN3 and GDNF polymorphisms as common genetic factors of substance use and addictive behaviors. J Pers Med 12(5):690. https://doi.org/10.3390/jpm12050690
Wang MY, Tessitore E, Berrington N, Dailey A (2019) Introduction. Enhanced recovery after surgery (ERAS) in spine. Neurosurg Focus 46(4):E1. https://doi.org/10.3171/2019.1.FOCUS1957
Wang L, Hong PJ, Jiang W, Rehman Y, Hong BY, Couban RJ, Wang C, Hayes CJ, Juurlink DN, Busse JW (2023) Predictors of fatal and nonfatal overdose after prescription of opioids for chronic pain: a systematic review and meta-analysis of observational studies. CMAJ 195(41):E1399–E1411. https://doi.org/10.1503/cmaj.230459
Wilson N, Kariisa M, Seth P, Smith HT, Davis NL (2020) Drug and opioid-involved overdose deaths—United States, 2017–2018. Morb Mortal Wkly Rep 69(11):290–297. https://doi.org/10.15585/mmwr.mm6911a4
Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, Blyth FM, Smith E, Buchbinder R, Hoy D (2020) Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med 8(6):299. https://doi.org/10.21037/atm.2020.02.175
Wyles CC, Thiels CA, Hevesi M, Ubl DS, Gazelka HM, Turner NS III, Trousdale RT, Pagnano MW, Mabry TM, Habermann EB (2021) Patient opioid requirements are often far less than their discharge prescription after orthopaedic surgery: the results of a prospective multicenter survey. J Am Acad Orthop Surg 29(7):e345–e353. https://doi.org/10.5435/JAAOS-D-19-00415
Xie X, Ma L, Xi K, Zhang W, Fan D (2017) MicroRNA-183 suppresses neuropathic pain and expression of AMPA receptors by targeting mTOR/VEGF signaling pathway. Cell Physiol Biochem 41(1):181–192. https://doi.org/10.1159/000455987
Zhang W, Yuan J-J, Kan Q-C, Zhang L-R, Chang Y-Z, Wang Z-Y, Li Z-S (2011) Influence of CYP3A5* 3 polymorphism and interaction between CYP3A5* 3 and CYP3A4* 1G polymorphisms on post-operative fentanyl analgesia in Chinese patients undergoing gynaecological surgery. Eur J Anaesthesiol 28(4):245–250. https://doi.org/10.1097/EJA.0b013e3283438b39
Zhao J, Cai S, Zhang L, Rao Y, Kang X, Feng Z (2022) Progress, challenges, and prospects of research on the effect of gene polymorphisms on adverse reactions to opioids. Pain Ther 11(2):395–409. https://doi.org/10.1007/s40122-022-00374-0
Zhi-Xue L, Ye F, Wen-Yao L, Yan-Ping B, Yin-Chu C, Zai-Wei S, Rong-Sheng Z, Zhen-Yu R (2023) The effect of genetic variation on the sensitivity to opioid analgesics in patients with postoperative pain: an updated meta-analysis. Pain Physician 26(5):E467. ISSN 2150–1149
Acknowledgements
We are thankful of all database developers and bioinformaticians enhancing big data analysis.
Funding
This study was supported by NIH HHS/United States (Grant No. R41 MD012318/MD/NIMHD).
Author information
Authors and Affiliations
Contributions
AS and KUL wrote the main manuscript text and prepared figures. All authors reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Kenneth Blum is the holder of many patents in the USA and abroad related to GARS and KB220. He has licensed his invention non-exclusively to Victory Nutrition International (VNI).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lewandrowski, KU., Sharafshah, A., Elfar, J. et al. A Pharmacogenomics-Based In Silico Investigation of Opioid Prescribing in Post-operative Spine Pain Management and Personalized Therapy. Cell Mol Neurobiol 44, 47 (2024). https://doi.org/10.1007/s10571-024-01466-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10571-024-01466-5