Abstract
Native T1 mapping is used to assess myocardial tissue characteristics without gadolinium contrast agents. The focal T1 high-intensity region can indicate myocardial alterations. This study aimed to identify the association between the native T1 mapping including the native T1 high region and left ventricular ejection fraction (LVEF) recovery in patients with dilated cardiomyopathy (DCM). Patients with newly diagnosed DCM (LVEF of < 45%) who underwent cardiac magnetic resonance imaging with native T1 mapping were included in the analysis. Native T1 high region was defined as a signal intensity of > 5 SD in the remote myocardium. Recovered EF was defined as a follow-up LVEF of ≥ 45% and an LVEF increase of ≥ 10% after 2 years from baseline. Seventy-one patients met the inclusion criteria for this study. Forty-four patients (61.9%) achieved recovered EF. Logistic regression analysis showed that the native T1 value (OR: 0.98; 95% CI: 0.96–0.99; P = 0.014) and the native T1 high region (OR: 0.17; 95% CI: 0.05–0.55; P = 0.002), but not late gadolinium enhancement, were independent predictors of recovered EF. Compared with native T1 value alone, combined native T1 high region and native T1 value improved the area under the curve from 0.703 to 0.788 for predicting recovered EF. Myocardial damage, which was quantified using native T1 mapping and the native T1 high region were independently associated with recovered EF in patients with newly diagnosed DCM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dilated cardiomyopathy (DCM) is a myocardial disease commonly diagnosed based on impaired left ventricular ejection fraction (LVEF) and LV dilation [1]. LVEF recovery can be achieved with guideline-directed medical therapy (GDMT). Further, it is associated with favourable outcomes in patients with DCM [2, 3]. However, despite progression in GDMT, a significant number of patients with DCM do not achieve LVEF recovery [4].
Cardiac magnetic resonance (CMR) imaging is suitable for investigating cardiac properties, functions and geometry. Late gadolinium enhancement (LGE)-CMR imaging is a standard technique for evaluating myocardial fibrosis [5]. Moreover, myocardial fibrosis evaluated via LGE-CMR imaging has a significant prognostic value for predicting the incidence of cardiac events and LVEF recovery in patients with DCM [6]. However, the capability of LGE-CMR imaging in evaluating diffuse myocardial fibrosis is limited [7]. In addition, LGE is not applicable to patients with renal dysfunction because of the need for gadolinium-based contrast agents [8]. Biological tissues have a fixed T1 value. The T1 map, which reflects tissue characteristics, can be produced by measuring the T1 value of cardiac tissues pixel-by-pixel. However, LGE can only be utilised to qualitatively assess myocardial fibrosis. The novel T1 mapping technique can be used to quantitatively assess native T1 value and extracellular volume (ECV) fraction [9].
ECV is a surrogate measure of extracellular space and is equivalent to the myocardial volume of gadolinium contrast medium distribution. It is used to assess extracellular space, which is occupied by the extracellular matrix. Therefore, it can reflect diffuse myocardial fibrosis in the absence of protein deposition or oedema [7]. The native T1 value is a pre-contrast T1 value of the myocardium, which reflects its intracellular and extracellular interstitial components [10]. Native T1 mapping can be applied to evaluate myocardial properties without gadolinium contrast agents [11, 12]. A high native T1 value indicates cardiomyocyte oedema or a high interstitial component, which indicates myocardial alterations including fibrosis [9]. A previous study showed that a high native T1 value was a predictor of hospitalisation due to worsening heart failure (HF) and all-cause mortality in patients with DCM [13]. However, the association between native T1 mapping and LVEF recovery in patients with DCM is unclear. Recently, the heterogeneity of native T1 mapping of the myocardium has attracted attention because it can have an additive prognostic value for predicting cardiac events and LV reverse remodelling [14, 15]. Based on these results, not only global native T1 value but also regional differences in native T1 value can be clinically significant. A high native T1 value is associated with myocardial alterations such as fibrosis and inflammation. We hypothesised that the focal high-intensity region of native T1 mapping can reflect regional myocardial alterations. Thus, the current study aimed to investigate the association between native T1 mapping, including the regional intensity area and LVEF recovery in patients with DCM.
Methods
Participants
This single-centre, retrospective, observational study assessed patients with newly diagnosed DCM who underwent CMR imaging at Kitasato University Hospital in Japan between October 2016 and December 2019. DCM was defined as an LVEF of < 45% at baseline echocardiography. Patients with significant coronary artery disease (> 75% luminal stenosis on coronary angiography), cardiac amyloidosis, sarcoidosis, acute myocarditis, metabolic disorders, endocrine dysfunction, neuromuscular diseases, peripartum cardiomyopathy, organic heart valve disease, use of cardiotoxic drugs and alcohol abuse were excluded. The Ethics Committee of Kitasato University Medical approved this study and the use of clinically acquired data. Moreover, the need for a written informed consent was waived.
CMR imaging acquisition
All CMR imaging procedures were performed with a 3.0T scanner (MAGNETOM Skyra, Siemens Healthineers, Erlangen, Germany) using a standard protocol. All images were obtained during breath holding at expiration. The cine images included the acquisition of three long-axis slices (two- and four-chamber) and a stack of short-axis slices covering the whole LV using a balanced steady-state free precession (bSSFP) sequence. Native T1 mapping was performed on a standard LV short-axis slice at the mid-ventricular level using the modified Look-Locker inversion recovery sequence combined with motion correction before contrast injection. The sequence parameters were as follows:
-
For an RR interval of > 700 ms, repetition time (TR)/echo time (TE): 280.6/1.1 ms; matrix: 256 × 169; field of view (FOV): 360 × 307 mm2; flip angle (FA): 35°; bandwidth: 1085 Hz/pixel and slice thickness: 8 mm.
-
For an RR interval of < 700 ms, TR/TE: 263.9/1.0 ms; matrix: 192 × 154; FOV: 360 × 307 mm2: FA: 35°; bandwidth: 1085 Hz/pixel and slice thickness: 8 mm.
LGE images were acquired 10–15 min after the intravenous injection of 0.2 mmol/kg gadolinium using the phase-sensitive inversion recovery bSSFP sequence. The sequence parameters were as follows: TR/TE, 2.7/1.1 ms; matrix, 224 × 180; FOV, 340 × 340 mm2; FA, 55°; bandwidth, 1,175 Hz/pixel; slice thickness, 8 mm and slice gap, 2 mm. Parallel imaging with GeneRalized Autocalibrating Partially Parallel Acquisitions was used for the sequence. The optimal inversion time (TI) was determined with a TI-scout sequence. This pulse sequence was used to determine optimal TI to null the signal intensity of the normal myocardium.
CMR image analysis
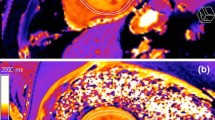
LV volumetric analysis was performed with a commercially available software (cvi42, version 4.1.8, Circle Cardiovascular Imaging, Calgary, Canada). The presence of LGE was defined by an experienced observer. The native T1 values were determined by drawing the region-of-interest (ROI) manually in each segment of the participants on a dedicated workstation with an ROI measuring tool (EV Insite, PSP Corporation, Tokyo, Japan), according to the six regions of the mid-ventricle in the 17-segment model [16]. The ROIs of all participants were drawn in a mid-wall region of the myocardium to minimise partial volume effects at the epicardial and endocardial borders (Fig. 1A) [17]. Similar to the measurement of the LGE area [18], the native T1 high region (Fig. 1B) was defined as a signal intensity of > 5 SD of the remote myocardium and was expressed as a percentage of the LV myocardium (native T1 high region ratio) using a commercially available software (Ziostation2, Ziosoft, Tokyo, Japan) (Fig. 1C).
Evaluation of native T1 values and native T1 high region. A Native T1 values were determined by drawing the region-of-interest in each segment of the six regions in the mid-left ventricle. B The native T1 high region (arrowheads). C A region-of-interest of 0.5−1 cm2 was manually drawn in the visually normal myocardium. The native T1 high region ratio was defined as a signal intensity of > 5 SD in the remote myocardium and was expressed as a percentage of the left ventricular area
Clinical measurement and observation
At baseline, blood pressure, heart rate and laboratory parameters were evaluated upon undergoing CMR imaging and echocardiography was performed. Patients were treated according to the current guidelines.[19] Recovered EF was defined as an LVEF of ≥ 45% and an LVEF increase of ≥ 10% on follow-up echocardiography after 2 years from baseline.[4, 20]. The endpoint was hospitalisation due to worsening HF. The endpoint data were obtained from the patient’s medical records.
Statistical analysis
Data were presented as mean ± standard deviation or as frequency (percentage). The Student’s t-test was used to compare continuous variables and the Mann–Whitney U test was utilised to evaluate non-normally distributed continuous variables. The Pearson’s chi-square test was applied to assessed categorical variables. A two-tailed P value of < 0.05 was considered statistically significant. Multivariate logistic regression analysis was performed to identify variables correlated with recovered EF among all baseline variables. The univariate analysis included potential covariates affecting LVEF recovering, as shown in a previous study [21]. Clinical variables with a P value of < 0.2 in the univariate analysis were examined in the multivariate analysis. The event-free survival curves were drawn using the Kaplan–Meier method and were compared using the log-rank test. Receiver-operating characteristic (ROC) curve analysis was performed to compare the discriminative power of predicting recovered EF between the native T1 value and the native T1 high region. Statistical analyses were performed using JMP version 14 (SAS Institute, Cary, NC, the USA) and R (version 4.1.1, R Project for Statistical Computing).
Results
Patient selection and baseline characteristics
In total, 71 patients met the inclusion criteria of this study. After 2 years from baseline, 44 patients (61.9%) achieved recovered EF (Fig. 2). Table 1 shows the baseline characteristics of the patients. Age, sex, blood pressure, comorbidity, medications, electrocardiogram, laboratory values and echocardiography results did not significantly differ between the non-recovered EF group and the recovered EF group. Table 2 depicts the baseline CMR imaging data. The LV volumes and the presence of LGE on CMR imaging did not significantly differ between the two groups. The non-recovered EF group had a significantly higher native T1 value than the recovered EF group (1329.5 ± 49.8 ms vs. 1296.3 ± 37.1 ms, P = 0.002). The non-recovered EF group was more likely to present with a native T1 high region than the recovered EF group (77.8% vs. 38.4%, P = 0.001). Furthermore, the non-recovered EF group had a significantly higher native T1 high region ratio than the recovered EF group (23.5 ± 16.5% vs. 8.8 ± 12.0%, P < 0.001).
In total, 20 (28.2%) patients presented with native T1 high regions despite the absence of LGE (Fig. 3A). In patients with LGE, the non-recovered EF group with the native T1 high region was significantly more frequently observed than those without (P = 0.002). In patients without LGE, the non-recovered EF group with the native T1 high region also tended to be more frequently observed than those without (P = 0.138) (Fig. 3B).
CMR imaging findings associated with recovered EF and prognosis
According to the results of the univariate analysis, mineralocorticoid receptor antagonist, complete left bundle branch block, LGE, native T1 value and native T1 high region were included in the multivariate model. Two multivariate models, one containing the native T1 value and one containing the native T1 high region, were constructed. In model 1, the native T1 value (odds ratio [OR]: 0.98; 95% confidential interval [CI]: 0.96–0.99; P = 0.014) was considered an independent factor associated with recovered EF. In model 2, the presence of the native T1 high region (OR: 0.17; 95% CI: 0.05–0.55; P = 0.002) was identified as an independent factor associated with recovered EF (Table 3). Based on the Kaplan–Meier curve, the non-recovered EF group had a significantly higher risk of hospitalisation due to HF than the recovered EF group (Fig. 4). Seven of the complete left bundle branch block patients underwent cardiac resynchronization therapy insertion, with no significant difference between the two groups [the non-recovered EF group: 3 (11.1%) vs. the recovered EF group: 4 (9.1%); P = 0.782].
Figure 5 depicts the ROC curves of the native T1 value and the native T1 high region for predicting recovered EF. Compared with native T1 value alone, combined native T1 high region and native T1 value improved the area under the curve from 0.703 to 0.788 for predicting recovered EF.
Discussion
Major findings
The current study showed the clinical significance of native T1 mapping in patients with newly diagnosed DCM. There were no significant differences in LV volumes and the presence of LGE between patients with recovered EF and those without. However, patients without recovered EF had a higher native T1 value than those with recovered EF. Furthermore, both the native T1 value and the presence of the native T1 high region were independently associated with recovered EF. The native T1 high region had an incremental prognostic value for predicting recovered EF. Thus, the native T1 high region and the native T1 value might be important markers for predicting recovered EF in patients with DCM.
High native T1 value and LVEF recovery
A high native T1 value indicates oedema (increased tissue water content caused by different factors including inflammation) and high interstitial components (e.g. fibrosis and amyloid deposition) [9]. In the current study, the non-recovered EF group had a significantly higher native T1 value than the recovered EF group. Hence, fibrosis progression was correlated with the presence or absence of LVEF improvement. These results are consistent with those of two previous studies, which reported that patients without LVEF recovery had a significantly higher native T1 value and ECV than those with LVEF recovery.[14, 22] In contrast, another study found that ECV and T2 values but not native T1 values were associated with LV reverse remodelling [23]. This discrepancy might be explained by differences in the definition of LVEF recovery and the study cohort. For example, this study only included 58% of patients with newly diagnosed DCM. However, in the current study, all patients were newly diagnosed with DCM. This difference might affect differences in the prognostic factors of LVEF recovery because the HF duration is a key factor of LVEF recovery [24].
Both native T1 and ECV fractions are correlated with histological collagen volume fractions. ECV quantifies the interstitial uptake of gadolinium contrast agent relative to the plasma. Native T1 mapping can be an effective alternative option to ECV measurement if a shorter scan time and non-contrast material requirements are considered [12]. Thus, native T1 mapping can be a more convenient method for identifying patients with or without LVEF recovery after GDMT.
Native T1 high region and LGE
LGE is the gold standard method for assessing focal myocardial damage representative of fibrosis [25]. LGE is associated with poor LVEF recovery in patients with DCM [6]. Conversely, similar to the current research, some studies showed that LGE was not a predictor of LVEF recovery [22, 26]. The reason for this discrepancy is unclear. However, the differences in cohorts and the number of events might be a cause.
In the current study, the native T1 high region was associated with LVEF recovery. Two previous studies revealed that the native T1 value of the segments with LGE was higher than that of the segments without LGE in patients with DCM [27, 28]. However, the association between T1 values per segment and the fraction of segments with LGE were modest [27]. In our research, the native T1 high region was observed in the segments without LGE. Therefore, the native T1 high region reflects focal myocardial alterations. However, it is not necessarily consistent with LGE. This discrepancy might be attributed to the fact that LGE may primarily indicate myocardial fibrosis and a high native T1 represents oedema and high interstitial components [9]. Moreover, Dass et al. showed that T1 mapping and LGE measurement were partly overlapping. Nevertheless, there were distinct myocardial pathologies [27]. Furthermore, T1 mapping facilitates direct myocardial signal quantification on a standardised scale. The advantages of T1 mapping can allow a better characterisation of myocardial tissue compared with LGE [25]. Therefore, the native T1 high region is more effective in identifying focal myocardial damage than LGE.
In a previous study, the native T1 value significantly decreased after GDMT. This finding indicates reduced collagen volume fraction and serum myocardial collagen accumulation index in patients with DCM after GDMT [23]. The current research did not assess changes in the native T1 value and the native T1 high region over time. Hence, further studies on this topic should be performed.
Clinical implications
Native T1 mapping can be performed on all patients eligible for CMR imaging because it does not require gadolinium contrast agents. In addition, the native T1 high region had an additive predictive value for predicting LVEF recovery. In relation to this reason, it might be helpful to focus on the native T1 value and the native T1 high region in determining appropriate treatment strategies in patients with newly diagnosed DCM.
Study limitations
The current study had several limitations that must be acknowledged. First, this was a single-centre study with a limited number of patients. This could have resulted in patient selection bias and a lower statistical power. Second, only patients undergoing CMR imaging were included in the analysis, which could have posed a risk of bias. Third, the statistical power was limited because of the small number of events. Fourth, T1 mapping images of LV were acquired only at the mid-ventricular level. Therefore, the whole LV myocardium could not be evaluated.
Conclusion
The quantitative value of native T1 mapping and the presence of a high-signal intensity region were independent predictors of LVEF improvement in patients with newly diagnosed DCM. Combined native T1 value and native T1 high region was more accurate in predicting LVEF improvement than native T1 value alone. Hence, T1 mapping might be useful in identifying therapeutic options for patients with DCM.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
References
Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P et al (2008) Classification of the cardiomyopathies: a position statement from the european society of cardiology working group on myocardial and pericardial diseases. Eur Heart J 29(2):270–276
Merlo M, Cannatá A, Vitagliano A, Zambon E, Lardieri G, Sinagra G (2016) Clinical management of dilated cardiomyopathy: current knowledge and future perspectives. Expert Rev Cardiovasc Ther 14(2):137–140
Wilcox JE, Fang JC, Margulies KB, Mann DL (2020) Heart failure with recovered left ventricular ejection Fraction: JACC scientific expert panel. J Am Coll Cardiol 76(6):719–734
Lupón J, Díez-López C, de Antonio M, Domingo M, Zamora E, Moliner P et al (2017) Recovered heart failure with reduced ejection fraction and outcomes: a prospective study. Eur J Heart Fail 19(12):1615–1623
Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S et al (2013) Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309(9):896–908
Becker MAJ, Cornel JH, van de Ven PM, van Rossum AC, Allaart CP, Germans T (2018) The Prognostic Value of late gadolinium-enhanced Cardiac magnetic resonance imaging in nonischemic dilated cardiomyopathy: a review and Meta-analysis. JACC Cardiovasc Imaging 11(9):1274–1284
Everett RJ, Stirrat CG, Semple SIR, Newby DE, Dweck MR, Mirsadraee S (2016) Assessment of myocardial fibrosis with T1 mapping MRI. Clin Radiol 71(8):768–778
Broome DR (2008) Nephrogenic systemic fibrosis associated with gadolinium based contrast agents: a summary of the medical literature reporting. Eur J Radiol 66(2):230–234
Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P et al (2017) Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2 and extracellular volume: a consensus statement by the society for cardiovascular magnetic resonance (SCMR) endorsed by the European association for cardiovascular imagin. J Cardiovasc Magn Reson 19(1):1–24
Iles L, Pfluger H, Phrommintikul A, Cherayath J, Aksit P, Gupta SN et al (2008) Evaluation of diffuse myocardial fibrosis in heart failure with cardiac magnetic resonance contrast-enhanced T1 mapping. J Am Coll Cardiol 52(19):1574–1580
Taylor AJ, Salerno M, Dharmakumar R, Jerosch-Herold M (2016) T1 mapping basic techniques and clinical applications. JACC Cardiovasc Imaging 9(1):67–81
Nakamori S, Dohi K, Ishida M, Goto Y, Imanaka-Yoshida K, Omori T et al (2018) Native T1 mapping and extracellular volume mapping for the assessment of diffuse myocardial fibrosis in dilated cardiomyopathy. JACC Cardiovasc Imaging 11(1):48–59
Puntmann VO, Carr-White G, Jabbour A, Yu CY, Gebker R, Kelle S et al (2016) T1-Mapping and outcome in nonischemic cardiomyopathy all-cause mortality and heart failure. JACC Cardiovasc Imaging 9(1):40–50
Kinoshita M, Kato S, Kodama S, Azuma M, Nakayama N, Fukui K et al (2022) Native T1 heterogeneity for predicting reverse remodeling in patients with non-ischemic dilated cardiomyopathy. Heart Vessels. https://doi.org/10.1007/s00380-022-02057-4
Nakamori S, Ngo LH, Rodriguez J, Neisius U, Manning WJ, Nezafat R (2020) T1 mapping tissue heterogeneity provides improved risk stratification for ICDs without needing Gadolinium in patients with dilated cardiomyopathy. JACC Cardiovasc Imaging 13(9):1917–1930
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK et al (2002) Standardized myocardial segmentation and nomenclature for Tomographic Imaging of the heart. Circulation 105(4):539–542
Cui Y, Cao Y, Song J, Dong N, Kong X, Wang J et al (2018) Association between myocardial extracellular volume and strain analysis through cardiovascular magnetic resonance with histological myocardial fibrosis in patients awaiting heart transplantation. J Cardiovasc Magn Reson 20:1–12
Nabeta T, Inomata T, Fujita T, Iida Y, Ikeda Y, Sato T et al (2017) Temporal change of myocardial tissue character is associated with left ventricular reverse remodeling in patients with dilated cardiomyopathy: a cardiovascular magnetic resonance study. J Cardiol 70(2):185–191
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Colvin MM et al (2017) 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA Guideline for the management of Heart failure: a report of the American college of cardiology/American heart association task force on clinical practice guidelines and the heart failure society of Amer. Circulation 136(6):e137–e161
Swat SA, Cohen D, Shah SJ, Lloyd-Jones DM, Baldridge AS, Freed BH et al (2018) Baseline longitudinal strain predicts recovery of left ventricular ejection fraction in hospitalized patients with nonischemic cardiomyopathy. J Am Heart Assoc 7(20):e09841
Aimo A, Gaggin HK, Barison A, Emdin M, Januzzi JL (2019) Imaging, biomarker, and clinical predictors of cardiac remodeling in heart failure with reduced ejection fraction. JACC Hear Fail 7(9):782–794
Inui K, Asai K, Tachi M, Yoshinaga A, Izumi Y, Kubota Y et al (2018) Extracellular volume fraction assessed using cardiovascular magnetic resonance can predict improvement in left ventricular ejection fraction in patients with dilated cardiomyopathy. Heart Vessels 33(10):1195–1203
Xu Y, Li W, Wan K, Liang Y, Jiang X, Wang J et al (2021) Myocardial tissue reverse remodeling after guideline-directed medical therapy in idiopathic dilated cardiomyopathy. Circ Hear Fail 14:59–70
Lupón J, Gavidia-Bovadilla G, Ferrer E, de Antonio M, Perera-Lluna A, López-Ayerbe J et al (2018) Dynamic trajectories of left ventricular ejection Fraction in Heart failure. J Am Coll Cardiol 72(6):591–601
Mewton N, Liu CY, Croisille P, Bluemke D, Lima JAC (2011) Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 57(8):891–903
Tayal U, Prasad SK (2017) Myocardial remodelling and recovery in dilated cardiomyopathy. JRSM Cardiovasc Dis 6:1–7
Dass S, Suttie JJ, Piechnik SK, Ferreira VM, Holloway CJ, Banerjee R et al (2012) Myocardial tissue characterization using magnetic resonance noncontrast T1 mapping in hypertrophic and dilated cardiomyopathy. Circ Cardiovasc Imaging 5(6):726–733
Yanagisawa F, Amano Y, Tachi M, Inui K, Asai K, Kumita S (2019) Non-contrast-enhanced T 1 mapping of dilated cardiomyopathy: comparison between native T 1 values and late gadolinium enhancement. Magn Reson Med Sci 18(1):12–18
Acknowledgements
We thank Hirofumi Hata and Shotaro Komi Department of Radiology, Kitasato University Hospital, for their technical assistance in the analysis of CMR.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
MY: performed the analyses. All authors involved in data acquisition revised the manuscript and participated in scientific discussion during the study. All authors read and approved final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Kitasato University Medical and the use of clinically acquired data.
Consent to participate
Moreover, the need for a written informed consent was waived.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yazaki, M., Nabeta, T., Takigami, Y. et al. Native T1 high region and left ventricular ejection fraction recovery in patients with dilated cardiomyopathy. Int J Cardiovasc Imaging 39, 1785–1793 (2023). https://doi.org/10.1007/s10554-023-02888-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02888-w