Abstract
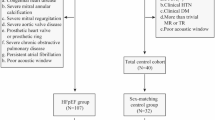
Non-invasive myocardial work (MW) by left ventricular (LV) pressure–strain loops (PSL) is a novel method for assessing myocardial function while adjusting for afterload, yet pediatric data remain lacking. The aims of this study were to investigate the different patterns of LV PSL and non-invasive MW in pediatric patients with hypertrophic (HCM) and dilated cardiomyopathy (DCM) and their association with exercise tolerance. We included 110 pediatric subjects (mean age, 13 ± 4 years, 35 DCM, 40 HCM, and 35 healthy controls). Standard and speckle-tracking echocardiography were performed. LV PSLs were generated, and global work index (GWI), MW efficiency (GWE), constructive work (GCW), and wasted work (GWW) were compared between groups. Regression analysis was used to assess the influence of ventricular function, dimensions, wall thickness, and wall stress on MW and to predict the association between MW and VO2 max as a surrogate of exercise capacity. Patients with DCM had significantly lower GWI compared to controls (GWI 479.6 ± 263.0 vs 1610.1 ± 211.0, P < 0.005). GWE was significantly reduced in DCM (79.3 ± 7.9 vs 95.2 ± 1.3, P < 0.005) due to significantly reduced GCW and increased GWW. HCM patients had significant reduction in GWI and GWE from normal (1237.7 ± 449.1 vs 1610.1 ± 211.0, P = 0.001 and 89.6 ± 4.9 vs 95.2 ± 1.3, P < 0.005, respectively), although less severe than with DCM. In a multivariate regression analysis, GWE had the highest association with VO2 max in both cohorts (DCM: β = 0.68, P = 0.001, HCM: β = 0.71, P = 0.007). Non-invasively assessed myocardial work and LV PSLs provide novel insights into the mechanisms of dysfunction in pediatric patients with cardiomyopathy with good prediction of clinical status and thus hold promise to further explore myocardial mechanistic with clinical relevance in different disease entities.





Similar content being viewed by others
Abbreviations
- BSA:
-
Body surface area
- CPET:
-
Cardiopulmonary exercise test
- DCM:
-
Dilated cardiomyopathy
- EDV:
-
End-diastolic volume
- EF:
-
Ejection fraction
- ESL:
-
Early systolic lengthening
- ESWS:
-
End-systolic wall stress
- FS:
-
Fraction shortening
- GCW:
-
Global constructive work
- GLS:
-
Global longitudinal strain
- GWE:
-
Global work efficiency
- GWI:
-
Global work index
- GWW:
-
Global wasted work
- HCM:
-
Hypertrophic cardiomyopathy
- ICC:
-
Intra-class correlation coefficient
- IVSD:
-
End-diastolic septal wall thickness
- IVSs:
-
End-systolic septal wall thickness
- LV:
-
Left ventricle
- LVIDd:
-
Left ventricular end-diastolic diameter
- LVIDs:
-
Left ventricular end-systolic diameter
- LVM:
-
Left ventricular mass
- LVMI:
-
Left ventricular mass indexed to body surface area
- LVPWd:
-
Left ventricular posterior wall thickness in diastole
- LVPWs:
-
Left ventricular posterior wall thickness in systole
- MV:
-
Mitral valve
- MVO2:
-
Myocardial oxygen consumption
- PSL:
-
Pressure–strain loops
- PSS:
-
Post-systolic shortening
- PVL:
-
Pressure–volume loops
- SBP:
-
Systolic blood pressure
- VO2 max:
-
Maximal oxygen uptake
References
Quinones MA, Gaasch WH, Alexander JK (1976) Influence of acute changes in preload, afterload, contractile state and heart rate on ejection and isovolumic indices of myocardial contractility in man. Circulation 53(2):293–302. https://doi.org/10.1161/01.cir.53.2.293
Klautz RJ, Teitel DF, Steendijk P, van Bel F, Baan J (1995) Interaction between afterload and contractility in the newborn heart: evidence of homeometric autoregulation in the intact circulation. J Am Coll Cardiol 25(6):1428–1435. https://doi.org/10.1016/0735-1097(94)00562-5
Fukuta H, Little WC (2008) The cardiac cycle and the physiologic basis of left ventricular contraction, ejection, relaxation, and filling. Heart Fail Clin 4(1):1–11. https://doi.org/10.1016/j.hfc.2007.10.004
Carabello BA (2002) Evolution of the study of left ventricular function: everything old is new again. Circulation 105(23):2701–2703. https://doi.org/10.1161/01.cir.0000021240.86593.9d
Mele D, Pasanisi G, Capasso F, De Simone A, Morales MA, Poggio D, Capucci A, Tabacchi G, Sallusti L, Ferrari R (2006) Left intraventricular myocardial deformation dyssynchrony identifies responders to cardiac resynchronization therapy in patients with heart failure. Eur Heart J 27(9):1070–1078. https://doi.org/10.1093/eurheartj/ehi814
Yingchoncharoen T, Agarwal S, Popović ZB, Marwick TH (2013) Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr 26(2):185–191. https://doi.org/10.1016/j.echo.2012.10.008
Kuhtz-Buschbeck JP, Drake-Holland A, Noble MIM, Lohff B, Schaefer J (2018) Rediscovery of Otto Frank’s contribution to science. J Mol Cell Cardiol 1(119):96–103. https://doi.org/10.1016/j.yjmcc.2018.04.017 (Erratum in: J Mol Cell Cardiol. 2018;123:58)
Suga H, Hayashi T, Shirahata M (1981) Ventricular systolic pressure-volume area as predictor of cardiac oxygen consumption. Am J Physiol Heart Circ Physiol. https://doi.org/10.1152/ajpheart.1981.240.1.H39
Suga H (1979) Total mechanical energy of a ventricle model and cardiac oxygen consumption. Am J Physiol 236(3):H498-505. https://doi.org/10.1152/ajpheart.1979.236.3.H498
Bastos MB, Burkhoff D, Maly J, Daemen J, den Uil CA, Ameloot K, Lenzen M, Mahfoud F, Zijlstra F, Schreuder JJ, Van Mieghem NM (2020) Invasive left ventricle pressure-volume analysis: overview and practical clinical implications. Eur Heart J 41(12):1286–1297. https://doi.org/10.1093/eurheartj/ehz552
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Remme EW, Haugaa KH, Opdahl A, Fjeld JG, Gjesdal O, Edvardsen T, Smiseth OA (2012) A novel clinical method for quantification of regional left ventricular pressure-strain loop area: a non-invasive index of myocardial work. Eur Heart J 33(6):724–733. https://doi.org/10.1093/eurheartj/ehs016
Van der Bijl P, Kostyukevich M, El Mahdiui M, Hansen G, Samset E, Ajmone Marsan N, Bax JJ, Delgado V (2019) A roadmap to assess myocardial work: from theory to clinical practice. JACC Cardiovasc Imaging 12(12):2549–2554. https://doi.org/10.1016/j.jcmg.2019.05.028
Russell K, Eriksen M, Aaberge L, Wilhelmsen N, Skulstad H, Gjesdal O, Edvardsen T, Smiseth OA (2013) Assessment of wasted myocardial work: a novel method to quantify energy loss due to uncoordinated left ventricular contractions. Am J Physiol Heart Circ Physiol 305(7):H996-1003
Hubert A, Le Rolle V, Leclercq C, Galli E, Samset E, Casset C, Mabo P, Hernandez A, Donal E (2018) Estimation of myocardial work from pressure-strain loops analysis: an experimental evaluation. Eur Heart J Cardiovasc Imaging 19(12):1372–1379. https://doi.org/10.1152/ajpheart.00191.2013
Schrub F, Schnell F, Donal E, Galli E (2020) Myocardial work is a predictor of exercise tolerance in patients with dilated cardiomyopathy and left ventricular dyssynchrony. Int J Cardiovasc Imaging 36(1):45–53. https://doi.org/10.1007/s10554-019-01689-4
Galli E, Vitel E, Schnell F, Le Rolle V, Hubert A, Lederlin M, Donal E (2019) Myocardial constructive work is impaired in hypertrophic cardiomyopathy and predicts left ventricular fibrosis. Echocardiography 36(1):74–82
Ebata R, Fujioka T, Diab SG, Pieles G, Ishii R, Ide H, Sun M, Slorach C, Liu K, Honjo O, Stortz G, Friedberg MK (2021) Asymmetric regional work contributes to right ventricular fibrosis, inefficiency, and dysfunction in pulmonary hypertension versus regurgitation. J Am Soc Echocardiogr 34(5):537-550.e3. https://doi.org/10.1016/j.echo.2020.12.011
Liu FZ, Wang XL, Zhang CQ (2021) Quantitative assessment of left ventricular myocardial work in chronic kidney disease patients by a novel non-invasive pressure-strain loop analysis method. Int J Cardiovasc Imaging 37(5):1567–1575
Spinelli L, Giugliano G, Pisani A, Imbriaco M, Riccio E, Russo C, Cuocolo A, Trimarco B, Esposito G (2021) Does left ventricular function predict cardiac outcome in Anderson-Fabry disease? Int J Cardiovasc Imaging 37(4):1225–1236. https://doi.org/10.1016/j.echo.2020.12.011
Duchenne J, Aalen JM, Cvijic M, Larsen CK, Galli E, Bézy S, Beela AS, Ünlü S, Pagourelias ED, Winter S, Hopp E, Kongsgård E, Donal E, Fehske W, Smiseth OA, Voigt JU (2020) Acute redistribution of regional left ventricular work by cardiac resynchronization therapy determines long-term remodelling. Eur Heart J Cardiovasc Imaging 21(6):619–628. https://doi.org/10.1093/ehjci/jeaa003
Rowin EJ, Maron BJ, Wells S, Burrows A, Firely C, Koethe B, Patel AR, Maron MS (2021) Usefulness of global longitudinal strain to predict heart failure progression in patients with nonobstructive hypertrophic cardiomyopathy. Am J Cardiol 151:86–92. https://doi.org/10.1016/j.amjcard.2021.04.021
Haland TF, Hasselberg NE, Almaas VM, Dejgaard LA, Saberniak J, Leren IS, Berge KE, Haugaa KH, Edvardsen T (2017) The systolic paradox in hypertrophic cardiomyopathy. Open Heart 4(1):e000571. https://doi.org/10.1136/openhrt-2016-000571
Hara Y, Hamada M, Hiwada K (1999) Left ventricular end-systolic wall stress is a potent prognostic variable in patients with dilated cardiomyopathy. Jpn Circ J 63(3):196–200. https://doi.org/10.1253/jcj.63.196
Lopez L, Colan SD, Frommelt PC, Ensing GJ, Kendall K, Younoszai AK et al (2010) Recommendations for quantification methods during the performance of a pediatric echocardiogram: a report from the Pediatric Measurements Writing Group of the American Society of Echocardiography Pediatric and Congenital Heart Disease Council. J Am Soc Echocardiogr 23(5):465–495. https://doi.org/10.1016/j.echo.2010.03.019
Wilson JR, Reichek N, Hirshfeld J (1980) Noninvasive assessment of load reduction in patients with asymptomatic aortic regurgitation. Am J Med 68(5):664–674. https://doi.org/10.1016/j.echo.2010.03.019
Grossman W, Jones D, Mclaurin LP, Grossman W, Jones D, Mclaurin LP (1975) Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Investig 56(1):56–64. https://doi.org/10.1172/JCI108079
Reichek N, Wilson J, St John Sutton M, Plappert TA, Goldberg S, Hirshfeld JW (1982) Noninvasive determination of left ventricular end-systolic stress: validation of the method and initial application. Circulation 65(1):99–108
Voigt JU, Pedrizzetti G, Lysyansky P, Marwick TH, Houle H, Baumann R, Pedri S, Ito Y, Abe Y, Metz S, Song JH, Hamilton J, Sengupta PP, Kolias TJ, d’Hooge J, Aurigemma GP, Thomas JD, Badano LP (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16(1):1–11. https://doi.org/10.1093/ehjci/jeu184
Pradhan S, Mullikin A, Zang H, Ollberding NJ, Stark S, Hill GD, Chin C, Tretter JT (2021) Decreased global myocardial work efficiency correlates with coronary vasculopathy in pediatric heart transplant patients. Pediatr Cardiol. https://doi.org/10.1007/s00246-021-02748-1
Pham TTM, Truong VT, Vu PN, Tran TX, Nguyen NNH, Nguyen LPT, Tu HNT, Palmer C, Tretter JT, Levy P, Mazur W, Pham VN (2021) Echocardiographic reference ranges of non-invasive myocardial work indices in children. Pediatr Cardiol. https://doi.org/10.1007/s00246-021-02695-x
Chan J, Edwards NFA, Khandheria BK, Shiino K, Sabapathy S, Anderson B, Chamberlain R, Scalia GM (2019) A new approach to assess myocardial work by non-invasive left ventricular pressure-strain relations in hypertension and dilated cardiomyopathy. Eur Heart J Cardiovasc Imaging 20(1):31–39
Podroužková H, Meluzín J, Hude P, Krejčí J, Špinarová L, Vítovec J (2012) Post-systolic shortening influences early diastolic tilling in patients with dilated cardiomyopathy. Cor Vasa 54(2):62–67
Brainin P (2021) Myocardial postsystolic shortening and early systolic lengthening: current status and future directions. Diagnostics 11(8):1428. https://doi.org/10.3390/diagnostics11081428
Sogaard P, Egeblad H, Kim WY, Jensen HK, Pedersen AK, Kristensen B, Mortensen PT (2002) Tissue Doppler imaging predicts improved systolic performance and reversed left ventricular remodeling during long-term cardiac resynchronization therapy. J Am Coll Cardiol 40:723–730
Yu CM, Fung JWH, Zhang Q, Chan CK, Chan YS, Lin H, Kum LCC, Kong SL, Zhang Y, Sanderson JE (2004) Tissue Doppler imaging is superior to strain rate imaging and postsystolic shortening on the prediction of reverse remodeling in both ischemic and nonischemic heart failure after cardiac resynchronization therapy. Circulation 110:66–73
Kim IS, Izawa H, Sobue T, Ishihara H, Somura F, Nishizawa T, Nagata K, Iwase M, Yokota M (2002) Prognostic value of mechanical efficiency in ambulatory patients with idiopathic dilated cardiomyopathy in sinus rhythm. J Am Coll Cardiol 39(8):1264–1268. https://doi.org/10.1016/s0735-1097(02)01775-8
Bing RJ, Hammond MM, Handelsman MD, Powers SR, Spencer MD, Eckenhoff MD, Goodale MD, Hafkenschiel MD, Kety MD (1949) The measurement of coronary blood flow, oxygen consumption, and efficiency of the left ventricle in man. Am Heart J 38(1):1–24. https://doi.org/10.1016/0002-8703(49)90788-7
Ishihara H, Yokota M, Sobue T, Saito H (1994) Relation between ventriculoarterial coupling and myocardial energetics in patients with idiopathic dilated cardiomyopathy. J Am Coll Cardiol 23(2):406–416. https://doi.org/10.1016/s0002-8703(96)90434-2
Kanda H, Yokota M, Ishihara H, Nagata K, Kato R, Sobue T (1996) A novel inotropic vasodilator, OPC-18790, reduces myocardial oxygen consumption and improves mechanical efficiency with congestive heart failure. Am Heart J 132(2 Pt 1):361–368. https://doi.org/10.1016/s0002-8703(96)90434-2
Flachskampf FA (2021) Letter to the editor regarding the recent publication of Hiemstra et al., myocardial work in nonobstructive hypertrophic cardiomyopathy: implications for outcome. J Am Soc Echocardiogr 34(2):201. https://doi.org/10.1016/j.echo.2020.10.007
Lytrivi ID, Blume ED, Rhodes J, Dillis S, Gauvreau K, Singh TP (2013) Prognostic value of exercise testing during heart transplant evaluation in children. Circ Heart Fail 6(4):792–799. https://doi.org/10.1016/j.echo.2020.10.007
Guimarães GV, d’Avila VM, Camargo PR, Moreira LF, Lanz JR, Bocchi EA (2008) Prognostic value of cardiopulmonary exercise testing in children with heart failure secondary to idiopathic dilated cardiomyopathy in a non-beta-blocker therapy setting. Eur J Heart Fail 10(6):560–565. https://doi.org/10.1016/j.ejheart.2008.04.009 (Erratum in: Eur J Heart Fail. 2008;10(8):814. Luces, Jose Ramon Lanz [corrected to Lanz, Jose Ramon])
Chen CK, Manlhiot C, Russell JL, Kantor PF, McCrindle BW, Conway J (2017) The utility of cardiopulmonary exercise testing for the prediction of outcomes in ambulatory children with dilated cardiomyopathy. Transplantation 101(10):2455–2460. https://doi.org/10.1097/TP.0000000000001672
Patel MD, Mohan J, Schneider C, Bajpai G, Purevjav E, Canter CE, Towbin J, Bredemeyer A, Lavine KJ (2017) Pediatric and adult dilated cardiomyopathy represent distinct pathological entities. JCI Insight 2(14):e94382. https://doi.org/10.1172/jci.insight.94382
Hiemstra YL, van der Bijl P, El Mahdiui M, Bax JJ, Delgado V, Marsan NA (2020) Myocardial work in nonobstructive hypertrophic cardiomyopathy: implications for outcome. J Am Soc Echocardiogr 33(10):1201–1208. https://doi.org/10.1016/j.echo.2020.05.010
Spirito P, Bellone P, Harris KM, Bernabo P, Bruzzi P, Maron BJ (2000) Magnitude of left ventricular hypertrophy and risk of sudden death in hypertrophic cardiomyopathy. N Engl J Med 342(24):1778–1785
Olivotto I, Gistri R, Petrone P, Pedemonte E, Vargiu D, Cecchi F (2003) Maximum left ventricular thickness and risk of sudden death in patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 41(2):315–321. https://doi.org/10.1016/s0735-1097(02)02713-4
Ho CY, López B, Coelho-Filho OR, Lakdawala NK, Cirino AL, Jarolim P, Kwong R, González A, Colan SD, Seidman JG, Díez J, Seidman CE (2010) Myocardial fibrosis as an early manifestation of hypertrophic cardiomyopathy. N Engl J Med 363(6):552–563. https://doi.org/10.1056/NEJMoa1002659
Coats CJ, Rantell K, Bartnik A, Patel A, Mist B, McKenna WJ, Elliott PM (2015) Cardiopulmonary exercise testing and prognosis in hypertrophic cardiomyopathy. Circ Heart Fail 8(6):1022–1031
Magrì D, Santolamazza C (2017) Cardiopulmonary exercise test in hypertrophic cardiomyopathy. Ann Am Thorac Soc 14(Supplement_1):S102–S109. https://doi.org/10.1513/AnnalsATS.201611-884FR
Lele SS, Thomson HL, Seo H, Belenkie I, McKenna WJ, Frenneaux MP (1995) Exercise capacity in hypertrophic cardiomyopathy. Role of stroke volume limitation, heart rate, and diastolic filling characteristics. Circulation 92(10):2886–2894. https://doi.org/10.1161/01.cir.92.10.2886
Jones S, Elliott PM, Sharma S, McKenna WJ, Whipp BJ (1998) Cardiopulmonary responses to exercise in patients with hypertrophic cardiomyopathy. Heart 80(1):60–67. https://doi.org/10.1136/hrt.80.1.60
Kjaergaard J, Johnson BD, Pellikka PA, Cha SS, Oh JK, Ommen SR (2005) Left atrial index is a predictor of exercise capacity in patients with hypertrophic cardiomyopathy. J Am Soc Echocardiogr 18(12):1373–1380. https://doi.org/10.1016/j.echo.2005.05.020
Roemer S, Jaglan A, Santos D, Umland M, Jain R, Tajik AJ, Khandheria BK (2021) The utility of myocardial work in clinical practice. J Am Soc Echocardiogr 34(8):807–818. https://doi.org/10.1016/j.echo.2021.04.013
Chan J, Edwards NFA, Scalia GM, Khandheria BK (2020) Myocardial work: a new type of strain imaging? J Am Soc Echocardiogr 33(10):1209–1211. https://doi.org/10.1016/j.echo.2020.05.004
Zhao X, Tan RS, Tang HC, Teo SK, Su Y, Wan M, Leng S, Zhang JM, Allen J, Kassab GS, Zhong L (2018) Left ventricular wall stress is sensitive marker of hypertrophic cardiomyopathy with preserved ejection fraction. Front Physiol 28(9):250. https://doi.org/10.3389/fphys.2018.00250
Acknowledgements
We thank the Medical Writing Center at Children’s Mercy Kansas City for editing this manuscript.
Funding
The authors received no financial support for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest of this study.
Ethical Approval
The study was approved by the hospital’s Institutional Review Board.
Informed Consent
Informed consent was obtained from their parents/guardians. Assent was also obtained from children aged 7 and older.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aly, D.M., Nguyen, M., Auerbach, S. et al. Pressure–Strain Loops, a Novel Non-invasive Approach for Assessment of Children with Cardiomyopathy. Pediatr Cardiol 43, 1704–1715 (2022). https://doi.org/10.1007/s00246-022-02902-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02902-3