Abstract
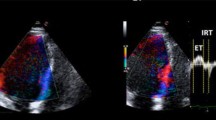
Identifying hypertensive patients who are at higher risk and thus to assess early echocardiographic markers of LV dysfunction in this population. Our comparative cross-section study included 100 patients divided into two groups; Group1: Hypertensive with preserved ejection fraction (EF) (n = 50) & Group 2: Normotensive (Control) (n = 50). Who underwent 2D Echo imaging with analysis of multible parameters of LV systolic and diastolic function including: left atrial volume index (LAVI), LV mass index, relative wall thickness, LV systolic function (EF%), diastolic function (trans-mitral pulsed and tissue Doppler study of E, A, e′-wave velocities& E/A, E/e′ ratios), Global myocardial longitudinal strain (GLS) by speckle tracking echocardiography (STE) and the early diastolic driving force (DF) which calculated as (DF = mass × acceleration; DF = 0.004E2/DT). We reported significant differences between the two groups in LV mass, LA volume and DF, which were all elevated in the hypertensive group, as well as reduced GLS magnitude. We also reported that a GLS cutoff of > − 18.1% was able to accurately “predict subclinical LV systolic dysfunction”. Finally, DF showed a moderate correlation (r = 0.33, which was established with statistical confidence) with E/e′ ratio, and a DF cutoff of ≥ 0.25 N was able to accurately “predict subclinical diastolic dysfunction”. GLS cutoff > − 18.1% could be used for early prediction of LV systolic dysfunction in hypertensive. The early diastolic DF cutoff ≥ 0.25 N could be a useful tool for early prediction of LV diastolic dysfunction in hypertensive. These sensitive parameters could be used for early diagnosis and proper management for better outcomes.






Similar content being viewed by others
Data availability
Our comparative cross-section study data used to support the findings of this study are available from the corresponding author upon request.
References
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJL (2002) The comparative risk assessment collaborating group “Selected major risk factors and global and regional burden of disease”. Lancet 360(9343):1347–1360. https://doi.org/10.1016/S0140-6736(02)11403-6
Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F (2000) Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension 35(2):580–586. https://doi.org/10.1161/01.HYP.35.2.580Hypertension
Ibrahim MM, Damasceno A (2012) Hypertension in developing countries. Lancet 380(9841):611–619. https://doi.org/10.1016/S0140-6736(12)60861-7
Ammar KA, Jacobsen SJ, Mahoney DW (2007) Prevalence and prognostic significance of heart failure stages: application of the American College of Cardiology/American Heart Association heart failure staging criteria in the community. Circulation 115(12):1563–1570. https://doi.org/10.1161/CIRCULATIONAHA.106.666818Circulation
Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, Nesser HJ, Khandheria B, Narula J, Sengupta PP (2010) Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 23(4):351–369. https://doi.org/10.1016/j.echo.2010.02.015
Alam M, Wardell J, Andersson E, Samad BA, Nordlander R (1999) Characteristics of mitral and tricuspid annular velocities determined by pulsed-wave Doppler tissue imaging in healthy subjects. J Am Soc Echocardiogr 12:618–628. https://doi.org/10.1053/je.1999.v12.a99246
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ (2005) Chamber quantification writing group; American Society of Echocardiography’s guidelines and standards committee; European Association of Echocardiography. J Am Soc Echocardiogr 18(12):1440–1463. https://doi.org/10.1016/j.echo.2005.10.005
Ammar A, Tavli T, Wong M (1993) Early diastolic driving force: a new index for separating relaxation from compliance abnormalities. New Egypt J Med 9:436–442. https://doi.org/10.1159/000177133
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur J Echocardiogr 17:1321–1360. https://doi.org/10.1093/ehjci/jew082
Troughton RW, Prior DL, Frampton CM, Nash PJ, Pereira JJ, Martin M, Fogarty A, Morehead AJ, Starling RC, Young JB, Thomas JD (2005) Usefulness of tissue Doppler and color M-mode indexes of left ventricular diastolic function in predicting outcomes in systolic left ventricular heart failure (from the ADEPT study). Am J Cardiol 96(2):257–262. https://doi.org/10.1016/j.amjcard.2005.03.055
Kasner M, Westermann D, Steendijk P, Gaub R, Wilkenshoff U, Weitmann K, Hoffmann W, Poller W, Schultheiss H, Pauschinger M, Tschöpe C (2007) Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation 11:637–647
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 10:165–193. https://doi.org/10.1093/ejechocard/jep007
Yingchoncharoen T, Agarwal S, Popović ZB, Marwick TH (2013) Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr 26:185–191. https://doi.org/10.1016/j.echo.2012.10.008Get
Weidemann F, Niemann M, Ertl G, Störk S (2010) The different faces of echocardiographic left ventricular hypertrophy: clues to the etiology. J Am Soc Echocardiogr 23(8):793–801. https://doi.org/10.1016/j.echo.2010.05.020
Drukteinis JS, Roman MJ, Fabsitz RR, Lee ET, Best LG, Russell M, Devereux RB (2007) Cardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults. Circulation 115:221–227. https://doi.org/10.1161/CIRCULATIONAHA.106.668921
Gonçalves S, Cortez-Dias N, Nunes A, Belo A, Zimbarra Cabrita I, Sousa C, Pinto FJ (2014) Left ventricular systolic dysfunction detected by speckle tracking in hypertensive patients with preserved ejection fraction. Rev Port Cardiol 33(1):27–37. https://doi.org/10.1016/j.repce.2013.07.013
Zhu H, Yan W, Ge D, Treiber FA, Harshfield GA, Kapuku G, Snieder H, Dong Y (2007) Cardiovascular characteristics in American youth with prehypertension. Am J Hypertens 20(10):1051–1057. https://doi.org/10.1016/j.amjhyper.2007.05.009
Lee SE, Youn JC, Lee HS, Park S, Lee SH, Cho IJ, Shim CY, Hong GR, Choi D, Kang SM (2015) Left atrial volume index is an independent predictor of hypertensive response to exercise in patients with hypertension. Hypertens Res 38(2):137–142. https://doi.org/10.1038/hr.2014.146
Cioffi G, Mureddu GF, Stefenelli C, Simone G (2004) Relationship between left ventricular geometry and left atrial size and function in patients with systemic hypertension. J Hypertens 22:1589–1596. https://doi.org/10.1097/01.hjh.0000125454.28861.76
Jenkins C, Bricknell K, Chan J, Hanekom L, Marwick T (2007) Comparison of two- and three-dimensional echocardiography with sequential magnetic resonance imaging for evaluating left ventricular volume and ejection fraction over time in patients with healed myocardial infarction. Am J Cardiol 99:300–306. https://doi.org/10.1016/j.amjcard.2006.08.026Get
Borlaug BA, Lam CS, Roger VL, Rodeheffer RJ, Redfield MM (2009) Contractility and ventricular systolic stiffening in hypertensive heart disease insights into the pathogenesis of heart failure with preserved ejection fraction. J Am Coll Cardiol 54:410–418. https://doi.org/10.1016/j.jacc.2009.05.013
Petrie MC, Caruana L, Berry C, McMurray JJ (2002) “Diastolic heart failure” or heart failure caused by subtle left ventricular systolic dysfunction? Heart 87:29–31. https://doi.org/10.1136/heart.87.1.29
Narayanan A, Aurigemma GP, Chinali M, Hill JC, Meyer TE, Tighe DA (2009) Cardiac mechanics in mild hypertensive heart disease: a speckle-strain imaging study. Circ Cardiovasc Imaging 2(5):382–390. https://doi.org/10.1136/heart.87.1.29
Heinzel Frank R, Hohendanner Felix, Jin Ge, Sedej Simon, Edelmann Frank (2015) Myocardial hypertrophy and its role in heart failure with preserved ejection fraction. J Appl Physiol 119(10):1233–1242. https://doi.org/10.1152/japplphysiol.00374.2015
Kouzu H, Yuda S, Muranaka A, Doi T, Yamamoto H, Shimoshige S, Hase M, Hashimoto A, Saitoh S, Tsuchihashi K, Miura T, Watanabe N, Shimamoto K (2011) Left ventricular hypertrophy causes different changes in longitudinal, radial, and circumferential mechanics in patients with hypertension: a two-dimensional speckle tracking study. J Am Soc Echocardiogr 24:192–199. https://doi.org/10.1016/j.echo.2010.10.020
Kraigher-Krainer E, Shah AM, Gupta DK, Santos A, Claggett B, Pieske B, Zile MR, Voors AA, Lefkowitz MP, Packer M, McMurray JJ, Solomon SD (2014) Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. J Am Coll Cardiol 63:447–456. https://doi.org/10.1016/j.jacc.2013.09.052
Marwick TH, Leano RL, Brown J, Sun JP, Hoffmann R, Lysyansky P, Becker M, Thomas JD (2009) Myocardial strain measurement with 2-dimensional speckle-tracking echocardiography: definition of normal range. JACC Cardiovasc Imaging 2(1):80–84. https://doi.org/10.1016/j.jcmg.2007.12.007
Takigiku K, Takeuchi M, Izumi C, Yuda S, Sakata K, Ohte N, Tanabe K, Nakatani S, JUSTICE investigators, (2012) Normal range of left ventricular 2-dimensional strain: Japanese Ultrasound Speckle Tracking of the Left Ventricle (JUSTICE) study. Circ J 76(11):2623–2632. https://doi.org/10.1253/circj.CJ-12-0264
Ayoub AM, Keddeas VW, Ali YA, El Okl RA (2016) Subclinical LV dysfunction detection using speckle tracking echocardiography in hypertensive patients with preserved LV ejection fraction. Clin Med Insights Cardiol 10:85–90. https://doi.org/10.4137/CMC.S38407
Negishi K, Lucas S, Negishi T, Hamilton J, Marwick TH (2013) What is the primary source of discordance in strain measurement between vendors: imaging or analysis? Ultrasound Med Biol 39(4):714–720. https://doi.org/10.1016/j.ultrasmedbio.2012.11.021
Patrianakos AP, Zacharaki AA, Kalogerakis A, Solidakis G, Parthenakis FI, Vardas PE (2015) Two-dimensional global and segmental longitudinal strain: are the results from software in different high-end ultrasound systems comparable? Echo Res Pract 2(1):29–39. https://doi.org/10.1530/ERP-14-0070
Funding
The study was performed at Zagazig University Hospitals outpatient clinics with no funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Our research involved human participants
The work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Informed consent
Informed consent was obtained from all participants in our research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shehata, I.E., Eldamanhory, A.S. & Shaker, A. Early predictors of left ventricular dysfunction in hypertensive patients: comparative cross-section study. Int J Cardiovasc Imaging 36, 1031–1040 (2020). https://doi.org/10.1007/s10554-020-01790-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01790-z