Abstract
Background
The association between alcohol intake and incidence of pituitary adenoma has not been reported previously. We examined this association in three large, prospective cohort studies.
Methods
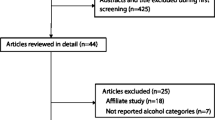
Using data from the Nurses’ Health Study, Nurses’ Health Study II, and Health Professionals Follow-Up Study, we computed multivariable-adjusted hazard ratios (MVHR) and 95% confidence intervals (CI) for pituitary adenoma by levels of alcohol intake using Cox proportional hazards regression.
Results
We identified 292 incident cases of pituitary adenoma (225 among women, 67 among men) among 235,973 participants with 6,548,732 person-years of follow-up. Compared with intake of ≤ 0.5 g/day, cumulative average alcohol intake in all categories was associated with reduced risk of pituitary adenoma (MVHR = 0.60, 95% CI 0.43–0.83 for 0.5–≤ 2 g/day, MVHR = 0.57, 95% CI 0.41–0.79 for > 2.0–≤ 8.0, MVHR = 0.70, 95% CI 0.47–1.04 for > 8.0–≤ 15.0, and MVHR = 0.51, 95% CI 0.32–0.83 for > 15.0 g/day). Significant inverse findings were present in women and were similar but non-significant in men. For specific alcoholic beverages, inverse associations were statistically significant for total wine (MVHR = 0.58, 95% CI 0.43–0.79 comparing 0.5–≤ 2 to ≤ 0.5 g/day), red wine (MVHR = 0.65, 95% CI 0.46–0.92 comparing 0.5–≤ 2 to ≤ 0.5 g/day), and white wine (MVHR = 0.72, 95% CI 0.53–0.97 comparing 0.5–≤ 2 to ≤ 0.5 g/day). Results were consistent using baseline intake, recent intake, and with an 8-year lag.
Conclusion
In three prospective cohorts, compared to almost no consumption, alcohol consumption was associated with reduced risk of pituitary adenoma. Sensitivity analyses suggest that these results are unlikely to be the result of reverse causation or diagnostic bias.
Similar content being viewed by others
Data availability
The data used in this manuscript are available from the corresponding authors upon reasonable request.
References
Melmed S (2020) Pituitary-tumor endocrinopathies. N Engl J Med 382(10):937–950
Cote DJ, Smith TR, Kaiser UB, Laws ER, Stampfer MJ (2021) Body habitus across the lifespan and risk of pituitary adenoma. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgaa987
Gittleman H, Ostrom QT, Farah PD et al (2014) Descriptive epidemiology of pituitary tumors in the United States, 2004–2009. J Neurosurg 121(3):527–535
Schoemaker MJ, Swerdlow AJ (2009) Risk factors for pituitary tumors: a case–control study. Cancer Epidemiol Biomark Prev 18(5):1492–1500
Coulam CB, Annegers JF, Abboud CF, Laws ER Jr, Kurland LT (1979) Pituitary adenoma and oral contraceptives: a case–control study. Fertil Steril 31(1):25–28
Ostrom QT, Adel Fahmideh M, Cote DJ et al (2019) Risk factors for childhood and adult primary brain tumors. Neuro Oncol 21(11):1357–1375
Hirko KA, Chen WY, Willett WC et al (2016) Alcohol consumption and risk of breast cancer by molecular subtype: prospective analysis of the nurses’ health study after 26 years of follow-up. Int J Cancer 138(5):1094–1101
Mostofsky E, Mukamal KJ, Giovannucci EL, Stampfer MJ, Rimm EB (2016) Key findings on alcohol consumption and a variety of health outcomes from the Nurses’ Health Study. Am J Public Health 106(9):1586–1591
Kim MK, Ko MJ, Han JT (2010) Alcohol consumption and mortality from all-cause and cancers among 1.34 million Koreans: the results from the Korea national health insurance corporation’s health examinee cohort in 2000. Cancer Causes Control 21(12):2295–302
Bagnardi V, Blangiardo M, La Vecchia C, Corrao G (2001) A meta-analysis of alcohol drinking and cancer risk. Br J Cancer 85(11):1700–1705
Polsky S, Akturk HK (2017) Alcohol consumption, diabetes risk, and cardiovascular disease within diabetes. Curr Diab Rep 17(12):136
Jimenez M, Chiuve SE, Glynn RJ et al (2012) Alcohol consumption and risk of stroke in women. Stroke 43(4):939–945
Chow WH, Dong LM, Devesa SS (2010) Epidemiology and risk factors for kidney cancer. Nat Rev Urol 7(5):245–257
Moissl AP, Delgado GE, Krämer BK et al (2021) Alcohol consumption and mortality: the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Atherosclerosis 335:119–125
English LK, Ard JD, Bailey RL et al (2021) Evaluation of dietary patterns and all-cause mortality: a systematic review. JAMA Netw Open 4(8):e2122277
Di Castelnuovo A, Costanzo S, Bonaccio M et al (2021) Alcohol intake and total mortality in 142 960 individuals from the MORGAM Project: a population-based study. Addiction. https://doi.org/10.1111/add.15593
Galeone C, Malerba S, Rota M et al (2013) A meta-analysis of alcohol consumption and the risk of brain tumours. Ann Oncol 24(2):514–523
Braganza MZ, Rajaraman P, Park Y et al (2014) Cigarette smoking, alcohol intake, and risk of glioma in the NIH-AARP Diet and Health Study. Br J Cancer 110(1):242–248
Kuan AS, Green J, Kitahara CM et al (2019) Diet and risk of glioma: combined analysis of 3 large prospective studies in the UK and USA. Neuro-Oncology 21(7):944–952
Cote DJ, Samanic CM, Smith TR et al (2021) Alcohol intake and risk of glioma: results from three prospective cohort studies. Eur J Epidemiol 36(9):965–974
Bao Y, Bertoia ML, Lenart EB et al (2016) Origin, methods, and evolution of the three nurses’ health studies. Am J Public Health 106(9):1573–1581
Smith-Warner SA, Spiegelman D, Ritz J et al (2006) Methods for pooling results of epidemiologic studies: the Pooling Project of Prospective Studies of Diet and Cancer. Am J Epidemiol 163(11):1053–1064
Willett WC, Sampson L, Stampfer MJ et al (1985) Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 122(1):51–65
Rimm EB, Giovannucci EL, Stampfer MJ et al (1992) Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 135(10):1114–1126; discussion 1127-1136
Feskanich D, Rimm EB, Giovannucci EL et al (1993) Reproducibility and validity of food intake measurements from a semiquantitative food frequency questionnaire. J Am Diet Assoc 93(7):790–796
Giovannucci E, Colditz G, Stampfer MJ et al (1991) The assessment of alcohol consumption by a simple self-administered questionnaire. Am J Epidemiol 133(8):810–817
Willett WC (1998) Nutritional epidemiology. Oxford University Press, New York
Scangas GA, Laws ER Jr (2014) Pituitary incidentalomas. Pituitary 17(5):486–491
Day PF, Loto MG, Glerean M et al (2016) Incidence and prevalence of clinically relevant pituitary adenomas: retrospective cohort study in a Health Management Organization in Buenos Aires, Argentina. Arch Endocrinol Metab 60(6):554–561
McDowell BD, Wallace RB, Carnahan RM et al (2011) Demographic differences in incidence for pituitary adenoma. Pituitary 14(1):23–30
Ezzat S, Asa SL, Couldwell WT et al (2004) The prevalence of pituitary adenomas: a systematic review. Cancer 101(3):613–619
Freda PU, Beckers AM, Katznelson L et al (2011) Pituitary incidentaloma: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 96(4):894–904
Grant BF, Chou SP, Saha TD et al (2017) Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001–2002 to 2012–2013: results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry 74(9):911–923
Carter LG, D’Orazio JA, Pearson KJ (2014) Resveratrol and cancer: focus on in vivo evidence. Endocr Relat Cancer 21(3):R209–R225
Casper RF, Quesne M, Rogers IM et al (1999) Resveratrol has antagonist activity on the aryl hydrocarbon receptor: implications for prevention of dioxin toxicity. Mol Pharmacol 56(4):784–790
Bilbao Garay I, Daly AF, Egaña Zunzunegi N, Beckers A (2020) Pituitary disease in AIP mutation-positive familial isolated pituitary adenoma (FIPA): a kindred-based overview. J Clin Med 9(6):2003
McCarty MF (2000) The insulin-sensitizing activity of moderate alcohol consumption may promote leanness in women. Med Hypotheses 54(5):794–797
Carvalho AF, Heilig M, Perez A, Probst C, Rehm J (2019) Alcohol use disorders. Lancet 394(10200):781–792
Shafrir AL, Wise LA, Palmer JR et al (2021) Validity of self-reported endometriosis: a comparison across four cohorts. Hum Reprod 36:1268–1278
Colditz GA, Stampfer MJ, Willett WC et al (1987) Reproducibility and validity of self-reported menopausal status in a prospective cohort study. Am J Epidemiol 126(2):319–325
Acknowledgments
We would like to thank the participants and staff of the Nurses’ Health Study, Nurses’ Health Study II, and Health Professionals Follow-Up Study for their valuable contributions as well as the following state cancer registries for their help: AL, AZ, AR, CA, CO, CT, DE, FL, GA, ID, IL, IN, IA, KY, LA, ME, MD, MA, MI, NE, NH, NJ, NY, NC, ND, OH, OK, OR, PA, RI, SC, TN, TX, VA, WA, and WY. The authors assume full responsibility for analyses and interpretation of these data.
Funding
National Institutes of Health (NIH) PO1 CA87969, U01 CA167552, UM1 CA186107, U01 CA176726, UM1 CA167552, F30 CA235791 (DJC), and R37 HD019938 (UBK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state that they have no relevant conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cote, D.J., Smith, T.R., Kaiser, U.B. et al. Alcohol intake and risk of pituitary adenoma. Cancer Causes Control 33, 353–361 (2022). https://doi.org/10.1007/s10552-021-01523-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01523-0